Abstract
Objective
To examine the joint association of birth weight and physical/sedentary activity time with obesity in 12 countries.
Methods
A cross-sectional study of 5,088 children aged 9–11 years was conducted. Birth weight was recalled by parents or guardians. Moderate-to-vigorous physical activity (MVPA) and sedentary behavior were objectively measured using accelerometry.
Results
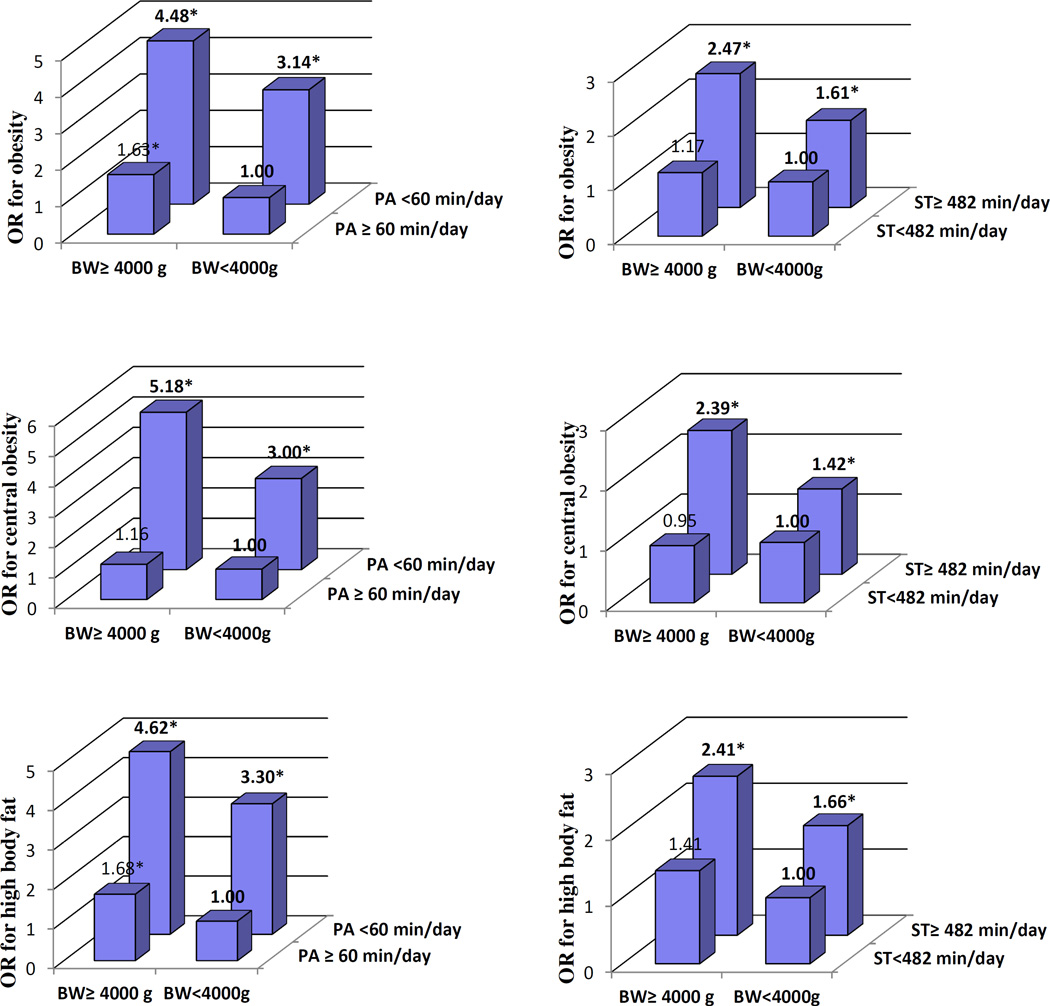
The association of birth weight with the odds of obesity, central obesity and high body fat was significant among children with either low MVPA or high sedentary time but not among children with either high MVPA or low sedentary time. In comparison with children with normal birth weight and high MVPA, children with high birth weight and low MVPA showed 4.48–5.18 fold higher odds of obesity, central obesity, and high body fat; children with normal birth weight and low MVPA showed 3.00–3.30 fold higher odds of obesity, central obesity, and high body fat, and children with high birth weight and high MVPA showed 1.16–1.68 fold higher odds of obesity, central obesity, and high body fat.
Conclusions
High MVPA is more important than high birth weight as a correlate of obesity in children.
Keywords: Birth weight, physical activity, sedentary lifestyle, obesity
Introduction
Obesity is an important lifestyle-related public health problem worldwide (1). The prevalence of childhood obesity has risen dramatically during the past few decades (2). Obesity has negative health impacts in childhood and later in life, as people with obesity experience adverse outcomes including hypertension, early markers of cardiovascular disease, insulin resistance and adverse psychological effects (3).
Childhood obesity is potentially affected by many lifestyle factors, including moderate-to-vigorous physical activity(MVPA) and sedentary behaviors (4). It has been shown that engaging in regular physical activity can reduce the risks of coronary heart disease, stroke, diabetes, and several types of cancer (5). Additionally, physical activity is a key determinant of daily energy expenditure, and thus is fundamental to energy balance and weight control (5). The available evidence from prospective studies suggests that increased physical activity, MVPA, and decreased sedentary behaviour are protective against relative gains in adiposity during childhood and adolescence (6).
Birth weight reflects the product of the growth trajectory during foetal life. Several studies have shown that high birth weight is associated with higher levels of body weight or obesity in childhood (7, 8, 9, 10). However, few studies have assessed the modifying effects of children’s physical activity on the association between birth weight and subsequent obesity in childhood (11, 12, 13) or adulthood (14, 15, 16). The aim of the present study was to examine the cross-sectional joint association of birth weight and objectively determined physical activity/sedentary behavior with the odds of obesity in 9–11 year old children from 12 countries.
Methods
Study design
The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE) is a multinational cross-sectional study conducted at urban and suburban sites in 12 countries (Australia, Brazil, Canada, China, Colombia, Finland, India, Kenya, Portugal, South Africa, United Kingdom and the United States) (17). More details on the study design and methods can be found elsewhere (17). The Institutional Review Board at the Pennington Biomedical Research Center (coordinating center) approved the overarching protocol, and the Institutional/Ethical Review Boards at each participating institution also approved the local protocol. Written informed consent was obtained from parents or legal guardians, and child assent was also obtained as required by local Institutional/Ethical Review Boards before participation in the study.
Participants
A total of 7,372 children aged 9–11 years participated in ISCOLE, of whom 5,088 remained in the present study after excluding those who did not have valid accelerometer (N=1,214), birth weight (N= 698), body mass index (BMI) (N=5), waist circumference (N=3), percentage of body fat (N=55), gestational age (N=118), or other information/data (N=191). Children who were excluded from the present analysis did not differ in age or BMI z-scores, but there were a higher proportion of boys excluded than included in the analysis (32.1% vs 30.0%). Data were collected from September 2011 through December 2013.
Measurements
Demographics and family health history
A demographic and family health history questionnaire was completed by parents or guardians. The questionnaire collected information on child age, sex, birth weight, infant feeding mode, gestational age, maternal history of gestational diabetes, and parent education. High birth weight was defined as birth weight ≥4000g. Maternal history of gestational diabetes was recalled by parents or guardians. The highest parental education completed by the child’s mother was asked, as was the highest level of education completed by the father. These responses were collapsed into three categories: did not complete high school, completed high school or some college, and completed bachelor or postgraduate degree. A derived variable was then created that represented the highest education level obtained by either parent, and if one of the parents’ response to this question was missing, the highest level obtained would be that of the parent who did provide data. The child’s parents were asked whether the child was fed breast milk or not, age when they completely stopped being fed breast milk, age when first fed formula and age when completely stopped drinking formula. These responses were classified into four categories: exclusive breast feeding, mixed feeding, weaned from breast feeding, exclusive formula feeding.
Dietary intake
A food frequency questionnaire (FFQ) that was adapted from the Health Behavior in School-aged Children Survey (HBSC) (18) was administered to all ISCOLE participants. The FFQ asked the participants about their “usual” consumption of 23 food categories, with response categories never, less than once per week, once per week, 2–4 days per week, 5–6 days per week, once a day every day, and more than once a day. Two diet scores which represent an “unhealthy diet pattern” (with positive loadings for fast food, hamburgers, soft drinks, sweets, fried food, etc.) and a “healthy diet pattern” (with positive loadings for vegetables, fruit, whole grains, low-fat milk, etc.) were obtained using principal components analyses (19, 20).
Accelerometry
An ActiGraph GT3X+ accelerometer (ActiGraph, LLC, Pensacola, FL, USA) was used to objectively measure MVPA, sedentary behavior and nocturnal sleeping time. The accelerometer was worn at the waist on an elasticized belt on the right mid-axillary line. Participants were encouraged to wear the accelerometer 24 hours per day (removing only for water-related activities) for at least 7 days (plus an initial familiarization day and the morning of the final day), including 2 weekend days. The minimal amount of accelerometer data that was considered acceptable was 4 days with at least 10 hours of waking wear time per day, including at least one weekend day (17). Several studies have indicated that 4–7 days of accelerometry data provide reliable estimates of usual physical activity(21, 22). Nocturnal sleep duration was estimated from the accelerometer data using a fully automated algorithm for 24-h waist-worn accelerometers that was recently validated for ISCOLE (23). This new algorithm produces more precise estimates of sleep duration than previous algorithms and captures total sleep time from sleep onset to the end of sleep, including all epochs and wakefulness after onset (23). The weekly total sleep time averages were calculated using only days where valid sleep was accumulated (total sleep period time ≥ 160 min) and only for participants with at least 3 nights of valid sleep, including one weekend day (24). After exclusion of total sleep time and awake non-wear time (any sequence of ≥20 consecutive minutes of zero activity counts), MVPA was defined as all activity ≥574 counts per 15 s and total sedentary activity as all movement ≤25 counts per 15 s, which was consistent with the widely used cutoffs from Evenson et al. (25). High (versus low) MVPA was defined as accumulating an average of at least 60 minutes of daily MVPA, similar to the WHO Global recommendations on physical activity for health (5); sedentary behavior was defined as accumulating an average of at least 482 minutes of sedentary time daily, based on a cut-off developed previously in ISCOLE (4).
Anthropometric measurements
A battery of anthropometric measurements was taken according to standardized procedures across all study sites. Height was measured without shoes using a Seca 213 portable stadiometer (Hamburg, Germany), with the participant’s head in the Frankfurt Plane. Waist circumference was measured with a non-elastic tape held midway between the lower rib margin and the iliac crest at the end of a gentle expiration (26). Waist circumference was measured on the bare skin in all countries except in Australia where it was measured over light clothing. The regression equation (y = 0.994x −0.42) developed by McCarthy et al. was applied to the Australian data to correct for the over-the-clothes measurement (27). Each measurement was repeated, and the average was used for analyses (a third measurement was obtained if the first two measurements were greater than 0.5 cm apart, and the average of the two closest measurements was used in analyses).
The participant’s weight and body fat were measured using a portable Tanita SC-240 Body Composition Analyzer (Arlington Heights, IL) after all outer clothing, heavy pocket items and shoes and socks were removed. Two measurements were obtained, and the average was used in analyses (a third measurement was obtained if the first two measurements were more than 0.5 kg or 2.0% apart, for weight and percentage body fat, respectively and the closet two were averaged for analyses). The Tanita SC-240 showed acceptable accuracy for estimating percent body fat when compared with dual-energy X-ray absorptiometry, supporting its use in field studies (28). BMI was calculated by dividing weight in kilograms by the square of height in meters. BMI z-scores were computed using age- and sex-specific reference data from the World Health Organization (29). General obesity was defined as BMI z-scores > +2 SD. Central obesity was defined as waist circumference ≥ 90th percentile of NHANES III reference (30, 31). High body fat was defined as body fat ≥ 90th percentile of NHANES IV reference (32).
Statistical analyses
Variables were compared using t-test for means and χ2 test for proportions between children classified as having normal birth weight and high birth weight. The joint associations of birth weight, time spent in MVPA and sedentary behavior with the risks of obesity, central obesity and high body fat were evaluated using a multi-level (3-level) logistic regression model (SAS version 9.4, PROC GLMMIX) by individual (level 1), nested in school (level 2) and study site (level 3).. Two categories of birth weight (normal and high), MVPA (low and high), and sedentary time (low and high) were used in the analyses. Study sites (level 3) and schools (level 2) nested within study sites were viewed as having random effects. The analyses were adjusted for highest parental education, infant feeding mode, gestational age, child age, sex, unhealthy diet pattern scores, healthy diet pattern scores, and sleeping time. Likelihood ratio test was used to examine the interactions between birth weight and MVPA or sedentary behavior with the odds of obesity, central obesity, and high body fat. The criterion for statistical significance was p<0.05. All statistical analyses were performed using SPSS for Windows, version 21.0 (Statistics 21, SPSS, IBM, USA) or SAS for Windows, version 9.4 (SAS Institute, Cary, NC).
Results
A total of 5088 children (2324 boys and 2764 girls) were included in the present study. The overall prevalence of obesity, central obesity, and high body fat were 12.3%, 9.9%, and 8.3%, respectively. The overall mean birth weight was 3277 g. The mean time spent in MVPA and sedentary behavior was 60.0 and 517 minutes/day, respectively. General characteristics of the study population are presented in Table 1.
Table 1.
Characteristics of study participants
| Characteristic | Overall (n=5088) |
Normal birth weight (n=4607) |
High birth weight (n=481) |
P value |
|---|---|---|---|---|
| Age, mean (SD) year | 10.4 (0.6) | 10.4 (0.6) | 10.4 (0.5) | 0.12 |
| Male, % | 45.7 | 44.3 | 58.4 | <0.001 |
| Body weight, mean (SD) kg | 37.5 (9.4) | 37.1 (9.3) | 40.6 (9.9) | <0.001 |
| Body height, mean (SD) cm | 142 (7.5) | 142 (7.5) | 145 (7.5) | <0.001 |
| Body mass index, mean (SD) kg/m2 | 18.4 (3.4) | 18.3 (3.4) | 19.1 (3.7) | <0.001 |
| Waist circumference, mean (SD) cm | 64.2 (8.9) | 64.1 (8.8) | 66.1 (9.1) | <0.001 |
| Body Fat, mean (SD) % | 20.8 (7.6) | 20.8 (7.6) | 21.2 (8.1) | 0.31 |
| Birth weight, mean (SD) g | 3277 (581) | 3171 (495) | 4294 (295) | <0.001 |
| Moderate-to-vigorous physical activity, mean (SD) min/day | 60.0 (24.8) | 59.4 (24.7) | 65.0 (25.2) | <0.001 |
| Sedentary, mean (SD) min/day | 517 (68.2) | 517 (68.5) | 513 (65.6) | 0.23 |
| Obesity, %a | 12.3 | 11.8 | 16.8 | 0.001 |
| Central obesity, %b | 9.9 | 9.5 | 13.3 | 0.008 |
| High body fat, %c | 8.3 | 8.0 | 11.0 | 0.02 |
| Parental education, % | 0.84 | |||
| Did not complete high school | 17.7 | 17.8 | 16.8 | |
| Completed high school/some college | 42.7 | 42.7 | 42.6 | |
| Bachelor’s degree or postgraduate degree | 39.6 | 39.5 | 40.5 | |
| Maternal history of gestational diabetes, % | 4.3 | 4.1 | 6.9 | 0.004 |
| Pregnancy term, mean (SD) weeks | 38.6 (2.2) | 38.5 (2.2) | 39.6 (1.6) | <0.001 |
| Infant breast feeding, % | 0.22 | |||
| Exclusive breast feeding | 37.4 | 37.0 | 41.4 | |
| Mixed feeding | 47.0 | 47.2 | 44.5 | |
| Weaned from breast feeding | 1.1 | 1.2 | 0.6 | |
| Exclusive formula feeding | 14.4 | 14.5 | 13.5 | |
| Unhealthy diet pattern score, mean (SD) | −0.11 (0.89) | −0.11 (0.89) | 0.02 (0.97) | 0.061 |
| Healthy diet pattern score, mean (SD) | −0.00 (0.99) | −0.01 (0.99) | 0.02 (0.97) | 0.56 |
| Duration of night sleep, mean (SD) minutes | 528 (53.0) | 528 (52.9) | 529 (54.4) | 0.62 |
Data are means (SD) or number (percentage).
Obesity was defined as BMI z-score >+2 SD for age and gender specific distribution based on from the World Health Organization growth reference.
Central obesity was defined as waist circumference ≥90th percentile for age and gender specific distribution using NHANES III reference.
High body fat was defined as body fat ≥90th percentile for age and gender specific distribution using NHANES IV reference
Among children with low MVPA at 9–11 years old, those born with high birth weight had higher odds for obesity (OR 1.50; 95% CI: 1.03–2.06), central obesity (OR 1.76; 95% CI: 1.23–2.51), and high body fat (OR 1.43; 95% CI: 1.02–2.01) than those born with normal birth weight (Table 2). However, the associations of birth weight with the odds of obesity, central obesity and high body fat were not significant among children with high MVPA at 9–11 years of age. The associations of high birth weight with high odds of obesity, central obesity and high body fat were significant among children with high time spent in sedentary behavior at 9–11 years old but not among those with low sedentary time.
Table 2.
Odds ratios for obesity, central obesity, high body fat by different effects of birth weight, moderate-to-vigorous physical activity and sedentary behavior
| Birth weight | Obesity | Central obesity | High body fat | ||||
|---|---|---|---|---|---|---|---|
| No. | OR (95%CI)a | No. | OR (95%CI)a | No. | OR (95%CI)a | ||
| Mod-to-vig phy act | |||||||
| Low | Normal | 411 | 1.00 | 340 | 1.00 | 306 | 1.00 |
| Low | High | 53 | 1.50 (1.03–2.06) | 49 | 1.76 (1.23–2.51) | 41 | 1.43 (1.02–2.01) |
| High | Normal | 132 | 1.00 | 98 | 1.00 | 64 | 1.00 |
| High | High | 28 | 1.55 (0.97–2.48) | 15 | 1.08 (0.59–1.96) | 12 | 1.60 (0.99–2.60) |
| Sedentary time | |||||||
| High | Normal | 431 | 1.00 | 344 | 1.00 | 293 | 1.00 |
| High | High | 66 | 1.53 (1.12–2.09) | 54 | 1.65 (1.18–2.31) | 42 | 1.43 (1.04–1.96) |
| Low | normal | 112 | 1.00 | 94 | 1.00 | 77 | 1.00 |
| Low | High | 15 | 1.14 (0.63–2.07) | 10 | 0.92 (0.46–1.87) | 11 | 1.36 (0.77–2.41) |
BW, birth weight; high birth weight defined as birth weight ≥4 000g; high moderate-to-vigorous physical activity was defined as accumulating at least 60 minutes of moderate-to-vigorous physical activity daily; high sedentary time defined as accumulating at least 482 minutes of sedentary time daily.
Adjusted for highest parental education, maternal history of gestational diabetes, infant feeding mode, gestational age, and child age, sex, unhealthy diet pattern scores, healthy diet pattern scores, and sleeping times.
The joint association of birth weight and time spent in MVPA/sedentary behavior with the odds of obesity, central obesity and high body fat in children with normal birth weight and high MVPA/low sedentary time as the reference group is shown in Figure 1. In comparison with children with normal birth weight and high MVPA, children with high birth weight and low MVPA showed 4.48–5.18 fold higher odds of obesity, central obesity, and high body fat, children with normal birth weight and low MVPA showed 3.00–3.30 fold higher odds of obesity, central obesity, and high body fat, and children with high birth weight and high MVPA showed 1.16–1.68 fold higher odds of obesity, central obesity, and high body fat, respectively. Similarly, children with high birth weight and high time spent in sedentary behavior showed the highest odds of obesity, central obesity, and high body fat, while children with normal birth weight and high sedentary time had higher odds of obesity, central obesity, and high body fat compared with children with normal birth weight and low time spent in sedentary activity. There were no significant interactions between birth weight and MVPA or sedentary behavior with the odds of obesity, central obesity, and high body fat (all P >0.10).
Figure 1.
Odds ratio for obesity, central obesity, high body fat among children by joint associations of birth weight, moderate-to-vigorous physical activity and sedentary behavior. Adjusted for highest parental education, maternal history of gestational diabetes, and child age, sex, infant feeding mode, gestational age, unhealthy diet pattern scores, healthy diet pattern scores, and sleeping times. *P<0.05.
Table 3 presents results for children with normal birth weight and low MVPA/high sedentary time compared against those with high birth weight and high MVPA/low sedentary time for the odds of obesity, central obesity and high body fat. Children born with high birth weight and high MVPA at 9–11 years old had significantly lower odds of obesity (OR 0.54; 95% CI: 0.34–0.84), central obesity (OR 0.39, 95% CI: 0.22–0.69) and high body fat (OR 0.55, 95% CI: 0.40–0.75) than those who were born with normal birth weight and had low MVPA. The odds of general obesity, central obesity, and high body fat were non-significantly lower among children who were born with high birth weight and reported high sedentary behavior than those who were born with normal birth weight and reported sedentary lifestyle at 9–11 years old.
Table 3.
Odds ratios for obesity, central obesity, high body fat among children with normal birth weight and low MVPA/high sedentary time in comparison with those with high birth weight and high MVPA/low sedentary time
| Category | No. of participates |
Obesity | Central obesity | High body fat | |||
|---|---|---|---|---|---|---|---|
| No. | OR (95%CI) a | No. | OR (95%CI) a | No. | OR (95%CI) a | ||
| Birth weight & MVPA | |||||||
| Normal BW & low MVPA | 2620 | 411 | 1.00 | 340 | 1.00 | 306 | 1.00 |
| High BW & high MVPA | 245 | 28 | 0.54 (0.34–0.84) | 15 | 0.39 (0.22–0.69) | 12 | 0.55 (0.40–0.75) |
| Birth weight & sedentary time | |||||||
| Normal BW & high sedentary time | 3190 | 431 | 1.00 | 344 | 1.00 | 293 | 1.00 |
| High BW & low sedentary time | 158 | 15 | 0.70 (0.40–1.25) | 10 | 0.63 (0.32–1.24) | 11 | 0.81 (0.47–1.39) |
BW, birth weight; MVPA, moderate-to-vigorous physical activity; high birth weight was defined as birth weight ≥4 000g; high moderate-to-vigorous physical activity was defined as accumulating at least 60 minutes of moderate-to-vigorous physical activity daily; high sedentary time was defined as accumulating an average of at least 482 minutes of sedentary time daily
Adjusted for highest parental education, maternal history of gestational diabetes, and child age, sex, infant feeding mode, gestational age, unhealthy diet pattern scores, healthy diet pattern scores, and sleeping times.
Discussion
In this multi-national cross-sectional study, we found that high MVPA is more important than high birth weight in determining obesity in 9–11 years old children. These findings suggest that physical activity is a stronger predictor than birth weight for childhood obesity.
Several studies have indicated that high birth weight is associated with subsequently higher levels of body weight or obesity in childhood (7, 8, 9, 10). Physical inactivity and sedentary behavior are important risk factors for incident type 2 diabetes, coronary heart disease, several types of cancer, and death (5). However, few epidemiological studies have assessed the joint associations of birth weight and physical activity/sedentary behavior with different health outcomes in children (11, 12, 13). A recent study found that among girls with self-reported low MVPA, those born with high birth weight had greater BMI at 12–15 years of age than those born with normal birth weight, and this difference diminished among girls with greater MVPA (13). Among boys, MVPA did not modify the associations between high birth weight and greater BMI (13).The present study indicates that the association of high birth weight with childhood obesity was significant among children with either low MVPA or high sedentary time but was not significant among children with either high MVPA or low sedentary time. However, the present study did not find any sex differences in the joint association of birth weight, MVPA and sedentary behaviours with the risk of childhood obesity. Moreover, we found that children with high birth weight and low MVPA showed the highest (4.48–5.18 fold) odds of obesity, and children with normal birth weight and low MVPA and children with high birth weight and high MVPA showed a high (3.00–3.30 fold and 1.16–1.68 fold) odds of obesity compared with children with normal birth weight and high MVPA.
In the current study, we first showed that the odds of childhood obesity were lower among children born with high birth weight who had high objectively monitored MVPA at 9–11 years compared to those who were born with normal birth weight and had low MVPA at age 9–11 years. This finding has important public health implications because people who have high birth weight might have higher obesity risk later in life but this risk could potentially be reduced if they engage in regular MVPA. These cross-sectional findings are consistent with the hypothesis that MVPA is a crucial component of a healthy lifestyle in prevention of chronic diseases such as obesity.
There are several strengths in our study including the recruitment of a large multi-national sample of children from low to high income countries across several regions of the world, the highly standardized measurement protocol, the use of direct measurements whenever possible, and the rigorous quality control program. In addition, MVPA and sedentary time were objectively measured using a 24-hour, waist worn accelerometer protocol. However, there are several limitations in the present study. First, the cross-sectional study precludes us from making cause-and-effect inferences. Second, birth weight records may have been recalled incorrectly by the parent or guardian. Third, since information on maternal prepregnancy BMI is not available in the present study, we were not able to fully control for the association of this variable on the association of birth weight and childhood physical activity with the risk of childhood obesity. Fourth, we did not collect information on the pubertal development of the participants in our study, which may influence growth and body composition. The degree to which these factors may have biased the results is unknown.
Conclusion
In conclusion, high birth weight was significantly associated with increased odds of childhood obesity, but the higher odds were not found at higher levels of MVPA, and lower levels of sedentary behavior. High MVPA is more important than high birth weight as a correlate of obesity in 9–11 year old children.
What is already known about this subject?
Childhood obesity is potentially affected by many lifestyle factors, including moderate-to-vigorous physical activity (MVPA) and sedentary behaviors.
Several studies have shown that high birth weight is associated with higher levels of body weight or obesity in childhood
What does this study add?
This study examined the cross-sectional joint association of birth weight and objectively determined physical activity/sedentary behavior with the odds of obesity in 9–11 year old children from 12 countries.
We found that high MVPA is more important than high birth weight in determining obesity in 9–11 years old children.
Acknowledgments
We wish to thank the ISCOLE External Advisory Board and the ISCOLE participants and their families who made this study possible. The ISCOLE Research Group includes: Coordinating Center, Pennington Biomedical Research Center: Peter T. Katzmarzyk, PhD (Co-PI), Timothy S. Church, MD, PhD (Co-PI), Denise G. Lambert, RN (Project Manager), Tiago Barreira, PhD, Stephanie Broyles, PhD, Ben Butitta, BS, Catherine Champagne, PhD, RD, Shannon Cocreham, MBA, Kara D. Denstel, MPH, Katy Drazba, MPH, Deirdre Harrington, PhD, William Johnson, PhD, Dione Milauskas, MS, Emily Mire, MS, Allison Tohme, MPH, Ruben Rodarte MS, MBA; Data Management Center, Wake Forest University: Bobby Amoroso, BS, John Luopa, BS, Rebecca Neiberg, MS, Scott Rushing, BS; Australia, University of South Australia: Timothy Olds, PhD (Site Co-PI), Carol Maher, PhD (Site Co-PI), Lucy Lewis, PhD, Katia Ferrar, B Physio (Hon), Effie Georgiadis, BPsych, Rebecca Stanley, BAppSc (OT) Hon; Brazil, Centro de Estudos do Laboratório de Aptidão Física de São Caetano do Sul (CELAFISCS): Victor Keihan Rodrigues Matsudo, MD, PhD (Site PI), Sandra Matsudo, MD, PhD, Timoteo Araujo, MSc, Luis Carlos de Oliveira, MSc, Luis Fabiano, BSc, Diogo Bezerra, BSc, Gerson Ferrari, MSc; Canada, Children’s Hospital of Eastern Ontario Research Institute: Mark S. Tremblay, PhD (Site Co-PI), Jean-Philippe Chaput, PhD (Site Co-PI), Priscilla Bélanger, MA, Mike Borghese, MSc, Charles Boyer, MA, Allana LeBlanc, MSc, Claire Francis, M.Sc., Geneviève Leduc, PhD; China, Tianjin Women’s and Children’s Health Center: Pei Zhao, MD (Site Co-PI), Gang Hu, MD, PhD (Site Co-PI), Chengming Diao, MD, Wei Li, MD, Weiqin Li, MSc, Enqing Liu, MD, Gongshu Liu, MD, Hongyan Liu, MD, Jian Ma, MD, Yijuan Qiao, MD, Huiguang Tian, PhD, Yue Wang, MD, Tao Zhang, MSc, Fuxia Zhang, MD; Colombia, Universidad de los Andes: Olga Sarmiento, MD, PhD (Site PI), Julio Acosta, Yalta Alvira, BS, Maria Paula Diaz, Rocio Gamez, BS, Maria Paula Garcia, Luis Guillermo Gómez, Lisseth Gonzalez, Silvia Gonzalez, RD, Carlos Grijalba, MD, Leidys Gutierrez, David Leal, Nicolas Lemus, Etelvina Mahecha, BS, Maria Paula Mahecha, Rosalba Mahecha, BS, Andrea Ramirez, MD, Paola Rios, MD, Andres Suarez, Camilo Triana; Finland, University of Helsinki: Mikael Fogelholm, ScD (Site-PI), Elli Hovi, BS, Jemina Kivelä, Sari Räsänen, BS, Sanna Roito, BS, Taru Saloheimo, MS, Leena Valta; India, St. Johns Research Institute: Anura Kurpad, MD, PhD (Site Co-PI), Rebecca Kuriyan, PhD (Site Co-PI), Deepa P. Lokesh, BSc, Michelle Stephanie D'Almeida, BSc, Annie Mattilda R, MSc, Lygia Correa, BSc, Vijay D, BSc; Kenya, Kenyatta University: Vincent Onywera, PhD (Site Co-PI), Mark S. Tremblay, PhD (Site Co-PI), Lucy-Joy Wachira, PhD, Stella Muthuri, PhD; Portugal, University of Porto: Jose Maia, PhD (Site PI), Alessandra da Silva Borges, BA, Sofia Oliveira Sá Cachada, Msc, Raquel Nichele de Chaves, MSc, Thayse Natacha Queiroz Ferreira Gomes, PhD, MSc, Sara Isabel Sampaio Pereira, BA, Daniel Monteiro de Vilhena e Santos, PhD, Fernanda Karina dos Santos, MSc, Pedro Gil Rodrigues da Silva, BA, Michele Caroline de Souza, MSc; South Africa, University of Cape Town: Vicki Lambert, PhD (Site PI), Matthew April, BSc (Hons), Monika Uys, BSc (Hons), Nirmala Naidoo, MSc, Nandi Synyanya, Madelaine Carstens, BSc(Hons); United Kingdom, University of Bath: Martyn Standage, PhD (Site PI), Sean Cumming, PhD, Clemens Drenowatz, PhD, Lydia Emm, MSc, Fiona Gillison, PhD, Julia Zakrzewski, PhD; United States, Pennington Biomedical Research Center: Catrine Tudor-Locke, PhD (Site-PI), Ashley Braud, Sheletta Donatto, MS, LDN, RD, Corbin Lemon, BS, Ana Jackson, BA, Ashunti Pearson, MS, Gina Pennington, BS, LDN, RD, Daniel Ragus, BS, Ryan Roubion, John Schuna, Jr., PhD; Derek Wiltz. The ISCOLE External Advisory Board includes Alan Batterham, PhD, Teesside University, Jacqueline Kerr, PhD, University of California, San Diego; Michael Pratt, MD, Centers for Disease Control and Prevention, Angelo Pietrobelli, MD, Verona University Medical School.
Funding/Support: ISCOLE was funded by The Coca-Cola Company. Dr. Hu was supported by grant from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number R01DK100790. The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Footnotes
Conflict of Interest Statement:
The authors reported no other potential conflicts of interest.
References
- 1.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 2.Wu JF. Childhood obesity: a growing global health hazard extending to adulthood. Pediatrics and neonatology. 2013;54:71–72. doi: 10.1016/j.pedneo.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Population-based prevention strategies for childhood obesity: report of a WHO forum and technical meeting. Geneva: World Health Organization; 2010. [Google Scholar]
- 4.Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput J-P, Fogelholm M, et al. Physical Activity, Sedentary Time, and Obesity in an International Sample of Children. Medicine and science in sports and exercise. 2015;47:2062–2069. doi: 10.1249/MSS.0000000000000649. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Global recommendations on physical activity for health. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 6.Must A, Tybor D. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. International journal of obesity. 2005;29:S84–S96. doi: 10.1038/sj.ijo.0803064. [DOI] [PubMed] [Google Scholar]
- 7.Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, Cao XG, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12:525–542. doi: 10.1111/j.1467-789X.2011.00867.x. [DOI] [PubMed] [Google Scholar]
- 8.Schellong K, Schulz S, Harder T, Plagemann A. Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PloS one. 2012;7:e47776. doi: 10.1371/journal.pone.0047776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang X, Liu E, Tian Z, Wang W, Ye T, Liu G, et al. High birth weight and overweight or obesity among Chinese children 3–6 years old. Preventive medicine. 2009;49:172–178. doi: 10.1016/j.ypmed.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Li N, Liu E, Sun S, Guo J, Pan L, Wang P, et al. Birth weight and overweight or obesity risk in children under 3 years in China. American journal of human biology: the official journal of the Human Biology Council. 2014;26:331–336. doi: 10.1002/ajhb.22506. [DOI] [PubMed] [Google Scholar]
- 11.Labayen I, Ortega F, Moreno L, Gonzalez-Gross M, Jimenez-Pavon D, Martinez-Gomez D, et al. Physical activity attenuates the negative effect of low birth weight on leptin levels in European adolescents; the HELENA study. Nutrition, Metabolism and Cardiovascular Diseases. 2013;23:344–349. doi: 10.1016/j.numecd.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Ortega FB, Ruiz JR, Hurtig-Wennlöf A, Meirhaeghe A, González-Gross M, Moreno LA, et al. Physical Activity Attenuates the Effect of Low Birth Weight on Insulin Resistance in Adolescents Findings From Two Observational Studies. Diabetes. 2011;60:2295–2299. doi: 10.2337/db10-1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boone-Heinonen J, Markwardt S, Fortmann S, Thornburg K. Overcoming birth weight: can physical activity mitigate birth weight-related differences in adiposity? Pediatric obesity. 2016;11:166–173. doi: 10.1111/ijpo.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laaksonen DE, Lakka H-M, Lynch J, Lakka TA, Niskanen L, Rauramaa R, et al. Cardiorespiratory fitness and vigorous leisure-time physical activity modify the association of small size at birth with the metabolic syndrome. Diabetes care. 2003;26:2156–2164. doi: 10.2337/diacare.26.7.2156. [DOI] [PubMed] [Google Scholar]
- 15.Eriksson JG, Ylihärsilä H, Forsén T, Osmond C, Barker DJ. Exercise protects against glucose intolerance in individuals with a small body size at birth. Preventive medicine. 2004;39:164–167. doi: 10.1016/j.ypmed.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 16.te Velde SJ, Twisk JW, Van Mechelen W, Kemper HC. A birth-weight questionnaire indicated that life style modifies the birth weight and metabolic syndrome relationship at age 36. Journal of clinical epidemiology. 2005;58:1172–1179. doi: 10.1016/j.jclinepi.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M, et al. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health. 2013;13:900. doi: 10.1186/1471-2458-13-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Currie C, Gabhainn SN, Godeau E, Roberts C, Smith R, Currie D, et al. Inequalities in Children's Health: HBSC International Report from the 2005/2006 Survey. Geneva: World Health Organization; 2008. [Google Scholar]
- 19.Saloheimo T, González SG, Erkkola M, Milauskas DM, Meisel JD, Champagne CM, et al. The reliability and validity of a short food frequency questionnaire among 9–11-year olds: a multinational study on three middle-income and high-income countries. International Journal of Obesity Supplements. 2015;5:22–28. doi: 10.1038/ijosup.2015.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dabelea D. The predisposition to obesity and diabetes in offspring of diabetic mothers. Diabetes care. 2007;30:S169–S174. doi: 10.2337/dc07-s211. [DOI] [PubMed] [Google Scholar]
- 21.Tudor-Locke C, Camhi SM, Troiano RP. A Catalog of Rules, Variables, and Definitions Applied to Accelerometer Data in the National Health and Nutrition Examination Survey, 2003–2006. Preventing chronic disease. 2012;9:E113. doi: 10.5888/pcd9.110332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trost SG, Pate RR, Freedson PS, Sallis JF, Taylor WC. Using objective physical activity measures with youth: how many days of monitoring are needed? Medicine and science in sports and exercise. 2000;32:426–431. doi: 10.1097/00005768-200002000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Barreira TV, Schuna JM, Jr, Mire EF, Katzmarzyk PT, Chaput J-P, Leduc G, et al. Identifying Children's Nocturnal Sleep Using 24-h Waist Accelerometry. Medicine and science in sports and exercise. 2015;47:937–943. doi: 10.1249/MSS.0000000000000486. [DOI] [PubMed] [Google Scholar]
- 24.Tudor-Locke C, Barreira TV, Schuna JM, Jr, Mire EF, Katzmarzyk PT. Fully automated waist-worn accelerometer algorithm for detecting children's sleep-period time separate from 24-h physical activity or sedentary behaviors. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2014;39:53–57. doi: 10.1139/apnm-2013-0173. [DOI] [PubMed] [Google Scholar]
- 25.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. Journal of sports sciences. 2008;26:1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation, Geneva, Switzerland. 2011
- 27.McCarthy HD, Ellis SM, Cole TJ. Central overweight and obesity in British youth aged 11–16 years: cross sectional surveys of waist circumference. BMJ (Clinical research ed) 2003;326:624. doi: 10.1136/bmj.326.7390.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barreira TV, Staiano AE, Katzmarzyk PT. Validity assessment of a portable bioimpedance scale to estimate body fat percentage in White and African–American children and adolescents. Pediatric obesity. 2013;8:e29–e32. doi: 10.1111/j.2047-6310.2012.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Onis M, Onyanga AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull WHO. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. The Journal of pediatrics. 2004;145:439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 31.Singh GK. Metabolic syndrome in children and adolescents. Current treatment options in cardiovascular medicine. 2006;8:403–413. [Google Scholar]
- 32.Laurson KR, Eisenmann JC, Welk GJ. Body fat percentile curves for U.S. children and adolescents. American journal of preventive medicine. 2011;41:S87–S92. doi: 10.1016/j.amepre.2011.06.044. [DOI] [PubMed] [Google Scholar]