Abstract
The Affordable Care Act (ACA) has reformed U.S. health care delivery through insurance coverage expansion, experiments in payment design, and funding for patient-centered clinical and health care delivery research. The impact on cancer care specifically has been far-reaching, with new ACA-related programs that encourage coordinated, patient-centered, cost-effective care. Insurance expansions through private exchanges and Medicaid, along with pre-existing condition clauses, have helped over 20 million Americans gain health care coverage. Accountable care organizations, oncology patient-centered medical homes and the Oncology Care Model—all implemented through the Center for Medicare and Medicaid Innovation—have initiated an accelerating shift toward value-based cancer care. Concurrently, evidence for better cancer outcomes and improved quality of cancer care is starting to accrue in the wake of ACA implementation.
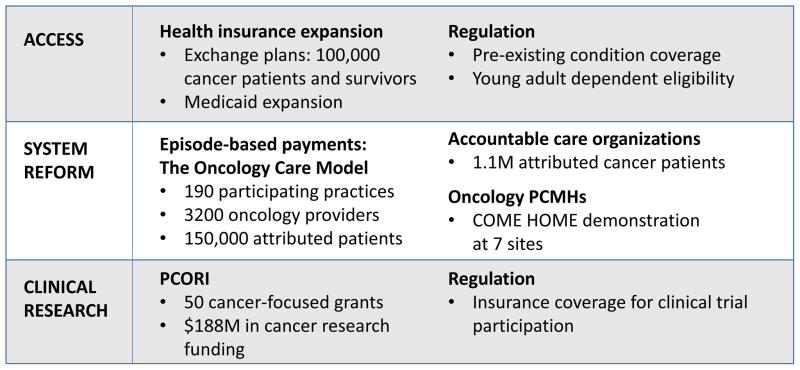
President Barack Obama signed the Patient Protection and Affordable Care Act (ACA) into law on March 23, 2010. Seven years later, 11.5 million Americans have purchased health insurance through exchanges,1 Medicaid has been expanded to approximately 14 million adults,1 and the Center for Medicare and Medicaid Innovation has implemented a staggering number of experiments in health care payment and delivery system reform. As with nearly all areas of U.S. health care delivery, the ACA’s impact on cancer care has been far-reaching. This manuscript will review ACA provisions relating to cancer care delivery (see Figure 1),2,3 with special attention to maturing cancer care outcomes data and the ongoing repercussions of the ACA’s impact on value-based cancer care.
Figure 1.
The Affordable Care Act and cancer care delivery reform
PCMH, patient-centered medical home; PCORI, Patient-Centered Outcomes Research Institute.
Three primary mechanisms have mediated the ACA’s impact on cancer care delivery: health insurance coverage expansion, health care payment and delivery system reform, and support for clinical research. Separate articles in this issue of The Cancer Journal address the relationships between the ACA and various aspects of cancer care, including the impact of Medicaid expansion and provisions relating to cancer screening and end-of-life care. This manuscript focuses on the ACA’s impact on cancer care delivery, driven by provisions relating to insurance expansion, payment and delivery system reform, and support for patient-centered clinical research.
Health Insurance Expansion and Cancer Care
Health insurance coverage expansion is the primary policy target of the ACA, accomplished through a blend of public and private insurance initiatives. Private insurance expansion was accomplished principally through the sale of individual policies on state-level exchanges, and approximately 11.5 million Americans are now insured through this mechanism.1 Additional ACA provisions reinforce private health insurance expansion through regulation of the commercial insurance market. Among the most important of these regulations is a provision prohibiting insurers from denying coverage based on pre-existing health conditions,4 making exchange-based insurance accessible to previously “uninsurable” cancer survivors. Specific figures are unavailable, however estimates from similar populations suggest that more than 100,000 cancer patients and survivors are currently insured through individual exchange-based plans.5 Media reports have highlighted anecdotes of cancer patients who credit their survival to marketplace insurance obtained through the ACA,6 and systematic evidence is beginning to accrue demonstrating improved cancer outcomes associated with private insurance expansion.7
While health insurance coverage is critical for ensuring access to cancer treatment, many exchange-insured cancer patients face narrow coverage networks for hospital-based and outpatient care. In a recent analysis of federal exchange insurance plans, only 41% of plan networks included a National Cancer Institute-designated cancer center.8 Narrow coverage networks for cancer treatment are ultimately symbolic of the compromise between access and cost that permeates the ACA and health care policy-making at large.
Health care payment and delivery system reforms
Insurance coverage expansion has been the most visible aspect of the ACA, however other provisions of the law are explicitly designed to reduce health care costs and improve health system quality. Key ACA provisions related to these goals include the implementation of accountable care organizations (ACOs) through the Medicare Shared Savings Program,9 expanded resources for the development of the patient-centered medical home model (PCMH),10 and a mandate for Medicare to test bundled and episode-based payment initiatives to enhance the quality and value of specialty care.11 Each of these areas has potential to substantially impact cancer care delivery.
Establishment of the Center for Medicare and Medicaid Innovation
The Center for Medicare and Medicaid Innovation (CMMI, also known as the Medicare Innovation Center) was established by the ACA12 and is now the key catalyst of federal health care payment reform. Housed within the Centers for Medicare and Medicaid Services (CMS), CMMI’s legislatively-defined mission is “to test innovative payment and service delivery models to reduce program expenditures…while preserving or enhancing the quality of care”.13 Inherent in the establishment of CMMI is an acknowledgement that designing and evaluating alternatives to fee-for-service payment is difficult work. By establishing CMMI, the ACA created the vehicle for CMS to develop new payment models, retain consultative expertise, and evaluate payment model effectiveness. Since establishment, CMMI has launched dozens of initiatives in service of its payment reform mission. Key initiatives relating to cancer care are described below, including ongoing development of the ACO payment model, funding for health care delivery innovation projects (including the COME HOME demonstration project of an oncology PCMH model), and the large scale-implementation of episode-based payments for cancer care (the Oncology Care Model).
ACOs and Cancer Care
The Medicare Shared Savings Program (MSSP) is the largest payment reform explicitly mandated within the ACA.9 This program follows the accountable care model, where hospitals and physician groups contract together to accept accountability for population-level health care outcomes, including spending. ACOs that reduce per-beneficiary spending, compared with historical targets, can earn “shared savings” payments, incenting cost-effective care. In addition to the MSSP, there are two Medicare demonstrations testing more advanced ACO payment models, Pioneer and Next Generation.
The MSSP is not cancer-focused but its impact is large due to substantial and growing voluntary enrollment (with over 7.7 million assigned beneficiaries as of January 2016).14 Early commentators hypothesized that the diffuse objectives and primary care orientation of the ACO model would limit the impact of the MSSP on costs and outcomes of cancer care.15 An analysis of the Physician Group Practice Demonstration (a forerunner to the MSSP established in 2005) showed annual spending reductions of $721 for cancer patients receiving care in ACOs (3.9% of per-patient spending).16 However, care within an ACO was associated with modest increases, rather than reductions, in spending for chemotherapy and cancer-related procedures. The entirety of the savings achieved among cancer patients was derived from reductions in inpatient hospital spending.16
Limited outcome data are available to judge the impact of the MSSP itself on cancer care, and most reports cover only the first year of the program (2013). In one study of both the Medicare Shared Savings and Pioneer programs, researchers demonstrated that ACO enrollment was associated with modest reductions in health care spending, hospitalizations, and ED visits, among all patients.17 Savings were magnified in a subgroup of patients with multiple chronic conditions, one quarter of whom carried a cancer diagnosis. Reductions in spending for patients with cancer did not appear to differ from spending reductions for patients with other chronic conditions. In another study, researchers evaluated the impact of hospital participation in MSSP on quality outcomes after cancer surgery, finding no significant difference in perioperative mortality, readmissions, or complications for 106 hospitals participating in the MSSP (compared with 2561 control hospitals).18
We conclude that ACOs have thus far had a modest impact in reducing spending for cancer patients, and impacts on quality of cancer care have not been reported. There is consistent evidence from the Physician Group Practice Demonstration, the MSSP, and the Pioneer Program showing modest reductions in total spending and spending for acute inpatient hospitalizations among cancer patients, however the mechanisms driving these reductions are not known. Anecdotally, integration of cancer care providers within ACOs appears to be weak, and initiatives with a more explicit focus on cancer patients may be needed to drive further improvements in cancer care quality and value. Nevertheless, the reach of the ACO model is large and growing; 1.1 million fee-for-service Medicare patients with cancer diagnoses were attributed to ACOs in 2014, representing over 40% of Medicare fee-for-service enrollees with cancer.19 CMS continues to build on the ACO model generally and the MSSP specifically,20 and many cancer patients will continue to receive their care within ACO delivery networks for the foreseeable future.
Cancer Care Delivery Innovation
In July 2012, CMMI announced the first round of 108 Health Care Innovation Awards.21 Each award tested a health care delivery innovation focused on specific populations and settings, and innovations were meant to deliver better health, improve care, and reduce costs. Cancer was one of seven conditions considered a “priority” because of cost, prevalence, and seriousness, and four cancer-related grants were awarded, focusing on care coordination. Each of these has shown limited improvements in available utilization or quality measures.22
One of these Innovation Awards supported the Community Oncology Medical Home (COME HOME) initiative. COME HOME is an example of an oncology PCMH, a delivery reform that requires practices to meet a set of service-based capabilities including care coordination, patient education, and enhanced patient access.23 These delivery reforms are often accompanied by a fixed monthly case management fee. Early evidence supporting the oncology PCMH came from the experience of Consultants in Medical Oncology and Hematology (CMOH), the first oncology practice to achieve PCMH certification from the NCQA. Sprandio and colleagues credited CMOH’s practice model with dramatic improvements in efficiency and quality of care, including a 68% decrease in emergency department (ED) visits, a 51% decrease in hospitalizations, and a 22% reduction in outpatient visits.24,25 In 2012, the COME HOME program was awarded almost $20 million dollars over three years to test the generalizability of a defined oncology PCMH model. The COME HOME program was implemented at seven community oncology practices across the U.S., featuring enhanced access to providers (by telephone and at same-day outpatient appointments), computerized symptom management pathways, and chemotherapy treatment pathways.22,26 Results of the formal program evaluation showed small but statistically significant reductions in ED visits and 30-day readmission rates. However, total cost of care and all-cause hospitalizations were not significantly different between COME HOME and comparison practices. These results appear to fall short of the program’s stated goals to reduce hospitalizations by 20% and total cost of care by 6%.26 Nevertheless, qualitative evaluation found that the program was well-received by both patients and staff, suggesting favorable quality-of-care outcomes.
The Innovation Awards also included grants to The University of Alabama at Birmingham (UAB) to fund technology and navigator-enabled care coordination and management, to the University of Pennsylvania to fund comprehensive palliative oncology services integrated with home-care services, and to the University of Virginia (UVA) to fund proactive symptom monitoring, team-based palliative care, and symptom palliation through radiation therapy. Each of these showed qualitative improvements in patient experience, with the UAB and UVA programs also reducing hospitalizations and ED visits.22 Round 2 of the Innovation Awards included an award to The University Hospitals Case Medical Center to improve cancer care delivery through early and ongoing palliative care consultation, improved care planning, communication, and patient and caregiver engagement, and care navigation (not yet evaluated).
Episode-based Payment for Cancer Care
CMMI’s most ambitious oncology payment reform initiative to date is the Oncology Care Model (OCM), an episode-based alternative payment model launched in summer of 2016. Voluntary program participants include 3200 oncology practitioners at 190 physician practices, serving over 150,000 beneficiaries (20% of all patients receiving chemotherapy under fee-for-service Medicare).27,28 Participants are primarily community-based medical oncology practices, however, a number of hospital-based practices—including academic cancer centers—are also participating. The OCM is structured around six-month chemotherapy treatment episodes, triggered by a qualifying outpatient chemotherapy claim (inclusive of intravenous and oral chemotherapies, as well as endocrine therapy agents for breast and prostate cancer).
The OCM program design includes two layers of payment incentives: a $160 monthly care coordination payment and performance-based incentive payments (essentially a conditional distribution of shared savings). Participating practices must fulfill requirements including 24/7 patient access to a member of their cancer care team and documentation of a care-management plan that includes 13 criteria proposed by the Institute of Medicine.29 CMS intends that practices will use the monthly care coordination fee to offset the cost of implementing program requirements and coordinating otherwise unreimbursed aspects of cancer care. To earn the additional performance-based incentive payment, practices must reduce total episode spending below a defined target price while meeting quality requirements. Episode target prices vary by cancer diagnosis and other beneficiary characteristics (but not cancer stage, which is not available in Medicare claims). Target prices are derived from historically-based spending projections (“benchmark prices”), less a 4% discount to CMS. A lower discount (2.75%) will be applied for practices electing two-sided risk, however these practices will also face downside risk (and will have to pay Medicare for overspending) when the total cost of care exceeds the episode target cost.
The concept of episode-based payments in cancer care builds on research showing substantial and presumably unwarranted variation in the cost of cancer care across regions and practices.30–32 CMS expects savings in OCM to arise through improved care coordination, decreased hospitalizations and ED visits, and more efficient and evidence-based use of chemotherapy, supportive medications, and imaging.33 These expectations are informed by data from pilot programs involving chemotherapy pathways programs34–36 and novel care management approaches.37 In a notable pilot program that incorporated elements of chemotherapy pathways and episode-based payments, UnitedHealthcare reported a 33% reduction in total spending for 810 patients treated at five participating practices (compared with modeled estimates).38,39 Of note, the success of the OCM is not predicated solely on achieving monetary savings, as patient experiences and quality of care will also be assessed.
Difficulty evaluating quality of care is an important but anticipated challenge associated with implementation and evaluation of the OCM. In order to achieve performance-based payment incentives, practices must demonstrate acceptable quality scores in addition to reductions in total cost of care. However, despite a number of ACA mandates to improve quality measurement, currently available quality measures for cancer care address limited quality domains. Of the 12 measures that feed into the OCM quality scoring system, eight are self-reported process measures.27 The remaining measures assess patient-rated experience of care, ED and inpatient utilization, and hospice enrollment (among decedents). Notably, OCM practices will also complete a patient registry including data on cancer stage and biomarker status, potentially paving the way for future assessment of stage-specific overall survival and other key outcomes of cancer care quality in this Medicare population.
Clinical Cancer Research
Support for clinical research is a small but significant component of the ACA. The Patient Centered Outcomes Research Institute (PCORI) was established by the ACA, and remains the major vehicle for ACA-related research funding. PCORI has carved out a distinct role in sponsoring comparative effectiveness research with intensive patient engagement.40 PCORI’s stated objectives include an increased focus on patient experience in research conduct and design, as well as an explicit emphasis on translation of research findings into clinical settings. PCORI has awarded over $1.6 billion in research funding since 2013, with $188 million allocated across 50 cancer-related projects. While its funding stream is dwarfed by that of the National Cancer Institute, PCORI’s unique deliberative processes have resulted in a correspondingly distinct research portfolio. Examples of PCORI’s ongoing cancer-related research include a pragmatic randomized clinical trial for treatment of cancer-associated thrombosis (comparing low molecular weight heparin with direct oral anticoagulants), a multi-site validation study of an electronic symptom assessment tool for supporting patients during chemotherapy treatment, and a clinical trial to improve appropriate use of colony stimulating factors during chemotherapy.
Another ACA provision relating to clinical research is a requirement that commercial insurers cover routine costs associated with participation in cancer clinical trials.4 Specifically, health insurers may not deny participation in a clinical trial, nor can they refuse coverage for routine care that is incidental to trial participation. While the clear intent of this provision is to expand and protect patient access to clinical trials, concerns have been raised regarding lax regulatory oversight and the absence of equivalent protections for Medicaid beneficiaries to access clinical trials.3,41 Lastly, in spite of the clinical trial coverage mandate, the narrow hospital and provider networks that are a feature of many exchange-based health plans may create de facto barriers to research participation.8 For these reasons, the impact of ACA implementation on expanding access to cancer clinical trials appears to be modest.
End of Life Care
The Affordable Care Act has the potential to impact cancer care delivery at the end-of-life through multiple paths. End-of-life care is expensive, with hospitalization being the principle driver of costs in the last months of life.30,42 Better communication between care providers, patients, and caregivers has been shown to both improve outcomes and lower spending by reducing the discordance between physicians and patients regarding prognosis and goals of care.43–45 Recognizing the importance of improving communication regarding preferences for end-of-life care, the OCM requires participating practices to document an explicit discussion of prognosis for all attributable patients. In addition, OCM quality measures emphasize end-of-life care quality by including hospice enrollment rates as a component of the overall quality score. Finally, the data feeds that Medicare provides to OCM participants provide practices with previously unavailable insights about their own end-of-life care patterns, which should allow better self-assessment regarding the adequacy of existing end-of-life care protocols.
Another mode in which the ACA has the potential to impact end-of-life care is through CMMI’s Medicare Care Choices Model (MCCM). Following the “open-access” hospice model, MCCM allows Medicare beneficiaries with qualifying terminal diagnoses to receive hospice-like support services from 140 participating hospice providers while concurrently receiving disease-modifying therapies from office- and hospital-based care providers (under current rules, Medicare beneficiaries are required to forgo “curative” care, including most chemotherapy treatments, in order to receive services under the hospice benefit). The model should allow greater flexibility for cancer patients and their families in deciding between hospice care and cancer-directed therapy, with potential to reduce end-of-life care costs while simultaneously enhancing quality of life in the end-of-life setting.
MACRA and the ACA
While certain aspects of the ACA face the prospect of repeal at the time of this writing, other facets appear more certain to endure. The 2015 Medicare Access and CHIP Reauthorization Act (MACRA) was passed by the U.S. Congress with bipartisan support, and supplants the ACA as further authorizing legislation for many of the payment and delivery system reforms described above, including the OCM. Under MACRA, physician practices that serve Medicare patients must participate in one of two programs in order to earn bonuses and avoid penalty payments. MACRA requirements can be satisfied by qualifying participation in an advanced alternative payment model (APM, including specified ACO contracts, PCMH models, or the OCM) that accepts risk contracts. Alternatively, practices may participate in the Merit-based Incentive Payment System (MIPS) by reporting on quality, resource use, technology capabilities, and quality improvement initiatives. The value-based financial incentives employed under MACRA are substantial in magnitude—with bonuses and penalty payments ranging up to 9% of a practice’s fee-for-service revenue by 2020—in essence providing both carrots (incentives encouraging participation in advanced payment models) and sticks (penalties in the form of reductions in revenue) encouraging a transition to high-value care.
Discussion
Over 20 million Americans have gained health insurance coverage since the passage of the Affordable Care Act. Based on the ACA’s design, many of these newly-insured are young adults, people with low income, and people with pre-existing conditions (including prior cancer diagnosis). Some of these newly-insured will develop cancer, and anecdotal and systematic evidence suggests that these individuals will be diagnosed earlier, will have better access to life-saving and life-prolonging cancer therapies, and will have protection from bankruptcy due to the costs associated with cancer treatment. Assuredly, we hypothesize that the ACA has reduced preventable cancer deaths, though not without cost.
The cost of health care in America, and cancer care in particular, makes the mission of health care delivery reform an essential one. The ACA has spurred innovations in cancer care payment and delivery through the Medicare Shared Savings Program and other ACO programs, development of the oncology patient-centered medical home model, and the Oncology Care Model. These ACA-initiated programs were based on promising experiments that showed improvements in quality paired with reductions in utilization and spending. The July 2016 implementation of the Oncology Care Model kicked off a critical, high-stakes phase of cancer care delivery reform, and we expect that bipartisan support for this and other payment reforms will allow experimentation and learning to continue. It is likely that more providers will volunteer for advanced payment models over time as MACRA legislation provides additional incentives.
Ultimately, the success of the Affordable Care Act in reforming U.S. cancer care delivery is likely to exceed the sum of its parts. Acting together, the various components of the ACA begin to create the infrastructure for value-driven cancer care. ACO programs and episode-based payments are creating the necessary conditions to bring teams of cancer care providers together in the name of grass-roots delivery reform. Once convened, these clinician-led groups can begin to access and analyze data describing their own performance on quality, cost, and value. Insights from these analyses will reveal many opportunities to improve cancer care in the U.S., and the decentralized approach of payment reform initiatives will allow oncology practices to adopt the reforms most appropriate for their clinical practice setting. Nevertheless, we anticipate that enhanced care coordination, improved communication (especially around end-of-life care preferences), and earlier introduction of concurrent, home-based palliative care will play a large role in many of these efforts. As we build this value-driven system, we must ensure that preserving universal access to life-saving, life-prolonging, and dignity-affirming cancer care remains a guiding principle.
References
- 1.Kaiser Family Foundation. [Accessed January 29, 2017];Interactive Maps: Estimates of Enrollment in ACA Marketplaces and Medicaid Expansion. 2017 at http://kff.org/interactive/interactive-maps-estimates-of-enrollment-in-aca-marketplaces-and-medicaid-expansion/.)
- 2.Albright HW, Moreno M, Feeley TW, et al. The implications of the 2010 Patient Protection and Affordable Care Act and the Health Care and Education Reconciliation Act on cancer care delivery. Cancer. 2011;117:1564–74. doi: 10.1002/cncr.25725. [DOI] [PubMed] [Google Scholar]
- 3.Zhang SQ, Polite BN. Achieving a deeper understanding of the implemented provisions of the Affordable Care Act. Am Soc Clin Oncol Educ Book. 2014:e472–7. doi: 10.14694/EdBook_AM.2014.34.e472. [DOI] [PubMed] [Google Scholar]
- 4.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119 §1201 (2010).
- 5.Kolodziej M, Hoverman JR, Garey JS, et al. Benchmarks for Value in Cancer Care: An Analysis of a Large Commercial Population. J Oncol Pract. 2011;7:301–6. doi: 10.1200/JOP.2011.000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldstein A. The Washington Post. 2017. Jan 14, Cancer survivor who once opposed federal health law challenges Ryan on its repeal. [Google Scholar]
- 7.Robbins AS, Han X, Ward EM, Simard EP, Zheng Z, Jemal A. Association Between the Affordable Care Act Dependent Coverage Expansion and Cervical Cancer Stage and Treatment in Young Women. JAMA. 2015;314:2189–91. doi: 10.1001/jama.2015.10546. [DOI] [PubMed] [Google Scholar]
- 8.Kehl KL, Liao K-P, Krause TM, Giordano SH. Access to Accredited Cancer Hospitals Within Federal Exchange Plans Under the Affordable Care Act. J Clin Oncol. doi: 10.1200/JCO.2016.69.9835. JCO.2016.69.9835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119 §3022 (2010).
- 10.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119 §3502 (2010).
- 11.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119 §3023 (2010).
- 12.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119 §3021 (2010).
- 13.Patient Protection and Affordable Care Act, Pub L No. 111–148, 124 Stat 119 §2705 (2010).
- 14.Centers for Medicare and Medicaid Services. [Accessed January 12, 2017];Medicare Care Choices. 2017 at https://innovation.cms.gov/initiatives/Medicare-Care-Choices/.)
- 15.Barkley R. Where does oncology fit in the scheme of accountable care? J Oncol Pract. 2012;8:71–4. doi: 10.1200/JOP.2012.000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colla CH, Lewis VA, Gottlieb DJ, Fisher ES. Cancer spending and accountable care organizations: Evidence from the Physician Group Practice Demonstration. Healthcare. 2013;1:100–7. doi: 10.1016/j.hjdsi.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colla CH, Lewis VA, Kao LS, O’Malley AJ, Chang CH, Fisher ES. Association Between Medicare Accountable Care Organization Implementation and Spending Among Clinically Vulnerable Beneficiaries. JAMA Intern Med. 2016;176:1167–75. doi: 10.1001/jamainternmed.2016.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herrel LA, Norton EC, Hawken SR, Ye Z, Hollenbeck BK, Miller DC. Early impact of Medicare accountable care organizations on cancer surgery outcomes. Cancer. 2016;122:2739–46. doi: 10.1002/cncr.30111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Authors’ analysis of Medicare data.
- 20.Centers for Medicare and Medicaid Services. [Accessed December 28, 2016];Shared Savings Program - News and Updates. 2016 at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/News-and-Updates.html.)
- 21.Centers for Medicare and Medicaid Services. [Accessed February 3, 2017];Health Care Innovation Awards. doi: 10.1111/1475-6773.12622. at https://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards/.) [DOI] [PMC free article] [PubMed]
- 22.Dhopeshwarkar R, Downie S, Freij M, et al. NORC at the University of Chicago. 2016. Mar, Second Annual Report: HCIA Disease-Specific Evaluation. [Google Scholar]
- 23.Page RD, Newcomer LN, Sprandio JD, McAneny BL. The patient-centered medical home in oncology: from concept to reality. Am Soc Clin Oncol Educ Book. 2015:e82–9. doi: 10.14694/EdBook_AM.2015.35.e82. [DOI] [PubMed] [Google Scholar]
- 24.Sprandio JD. Oncology Patient–Centered Medical Home. J Oncol Pract. 2012;8:47s–9s. doi: 10.1200/JOP.2012.000590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sprandio JD, Flounders BP, Lowry M, Tofani S. Data-Driven Transformation to an Oncology Patient–Centered Medical Home. J Oncol Pract. 2013;9:130–2. doi: 10.1200/JOP.2013.001019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sanghavi D, Patel K, Samuels K, et al. Transforming Cancer Care and the Role of Payment Reform: Lessons from the New Mexico Cancer Center. The Brookings Institution; 2014. Aug, [Google Scholar]
- 27.Centers for Medicare and Medicaid Services. [Accessed February 3, 2017];The Oncology Care Model. at https://innovation.cms.gov/initiatives/oncology-care/.)
- 28.Mortimer L, Strawbridge L, Lukens E, et al. CMS’ Oncology Care Model: Delivering Higher Value Cancer Care. Clin Pharmacol Ther. 2017 doi: 10.1002/cpt.638. [DOI] [PubMed] [Google Scholar]
- 29.Levit L, Balogh E, Nass S, Ganz PA. Delivering high-quality cancer care: charting a new course for a system in crisis. Washington, DC: IOM (Institute of Medicine); 2013. [PubMed] [Google Scholar]
- 30.Brooks GA, Li L, Uno H, Hassett MJ, Landon BE, Schrag D. Acute Hospital Care Is The Chief Driver Of Regional Spending Variation In Medicare Patients With Advanced Cancer. Health Aff (Millwood) 2014;33:1793–800. doi: 10.1377/hlthaff.2014.0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clough JD, Patel K, Riley GF, Rajkumar R, Conway PH, Bach PB. Wide variation in payments for Medicare beneficiary oncology services suggests room for practice-level improvement. Health Aff (Millwood) 2015;34:601–8. doi: 10.1377/hlthaff.2014.0964. [DOI] [PubMed] [Google Scholar]
- 32.Clough JD, Strawbridge LM, LeBlanc TW, Hammill BG, Kamal AH. Association of Practice-Level Hospital Use With End-of-Life Outcomes, Readmission, and Weekend Hospitalization Among Medicare Beneficiaries With Cancer. J Oncol Pract. 2016;12:e933–e43. doi: 10.1200/JOP.2016.013102. [DOI] [PubMed] [Google Scholar]
- 33.Kline RM, Bazell C, Smith E, Schumacher H, Rajkumar R, Conway PH. Centers for Medicare and Medicaid Services: Using an episode-based payment model to improve oncology care. J Oncol Pract. 2015;11:114–6. doi: 10.1200/JOP.2014.002337. [DOI] [PubMed] [Google Scholar]
- 34.Neubauer MA, Hoverman JR, Kolodziej M, et al. Cost effectiveness of evidence-based treatment guidelines for the treatment of non-small-cell lung cancer in the community setting. J Oncol Pract. 2010;6:12–8. doi: 10.1200/JOP.091058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoverman JR, Cartwright TH, Patt DA, et al. Pathways, outcomes, and costs in colon cancer: retrospective evaluations in two distinct databases. J Oncol Pract. 2011;7:52s–9s. doi: 10.1200/JOP.2011.000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kreys ED, Koeller JM. Documenting the benefits and cost savings of a large multistate cancer pathway program from a payer’s perspective. J Oncol Pract. 2013;9:e241–e7. doi: 10.1200/JOP.2012.000871. [DOI] [PubMed] [Google Scholar]
- 37.Hoverman JR, Klein I, Harrison DW, et al. Opening the Black Box: The Impact of an Oncology Management Program Consisting of Level I Pathways and an Outbound Nurse Call System. J Oncol Pract. 2014;10:63–7. doi: 10.1200/JOP.2013.001210. [DOI] [PubMed] [Google Scholar]
- 38.Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M. Changing physician incentives for affordable, quality cancer care: Results of an episode payment model. J Oncol Pract. 2014;10:322–6. doi: 10.1200/JOP.2014.001488. [DOI] [PubMed] [Google Scholar]
- 39.Newcomer LN. Changing physician incentives for cancer care to reward better patient outcomes instead of use of more costly drugs. Health Aff (Millwood) 2012;31:780–5. doi: 10.1377/hlthaff.2012.0002. [DOI] [PubMed] [Google Scholar]
- 40.Selby JV, Lipstein SH. PCORI at 3 Years — Progress, Lessons, and Plans. N Engl J Med. 2014;370:592–5. doi: 10.1056/NEJMp1313061. [DOI] [PubMed] [Google Scholar]
- 41.Martin PJ, Davenport-Ennis N, Petrelli NJ, Stewart FM, Appelbaum FR, AB Responsibility for Costs Associated With Clinical Trials. J Clin Oncol. 2014;32:3357–9. doi: 10.1200/JCO.2014.57.1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chastek B, Harley C, Kallich J, Newcomer L, Paoli CJ, Teitelbaum AH. Health Care Costs for Patients With Cancer at the End of Life. J Oncol Pract. 2012 doi: 10.1200/JOP.2011.000469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mack JW, Cronin A, Taback N, et al. End-of-Life Care Discussions Among Patients With Advanced Cancer: A Cohort Study. Ann Intern Med. 2012;156:204–10. doi: 10.1059/0003-4819-156-3-201202070-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–73. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: Associations with end-of-life conversations. Arch Intern Med. 2009;169:480–8. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]