Abstract
Background:
Traction apophysitis of medial epicondyle (MEC) lesions and osteochondritis dissecans (OCD) of the capitellum are common elbow injuries in adolescent baseball players. However, the age-specific prevalence of these pathologies and their influence on elbow pain remain unknown.
Purpose:
To investigate the age-specific prevalence of each MEC lesion and capitellar OCD and to identify the incidence of elbow pain in each condition.
Study Design:
Descriptive epidemiology study.
Methods:
Study participants consisted of 4249 baseball players aged 6 to 17 years. A questionnaire was used to assess history of elbow pain, and morphological changes of the elbow joint were assessed using ultrasonography.
Results:
Regarding MEC lesions, fragmented (FG) and irregular (IR) lesions both reached their greatest respective prevalence at 11 to 12 years of age. After 14 years of age, IR decreased sharply, whereas FG was maintained at approximately 10%. Hypertrophic (HT) lesions increased sharply, reaching over 50% at 16 years of age, while there was a decrease in IR and FG lesions in the same age group. The prevalence of capitellar OCD remained the same (approximately 2%) throughout all ages except for in players aged 7 to 8 years (>7%). Players with MEC lesions had significantly greater prevalence of a history of elbow pain compared with those without (68.0% vs 39.1%) and were at a significantly greater risk for FG lesions (odds ratio [OR], 4.04; 95% CI, 3.16-5.22) compared with IR (OR, 3.22; 95% CI, 2.44-4.27) and HT lesions (OR, 2.03; 95% CI, 1.75-2.36). Players with capitellar OCD also had a significantly greater risk of a history of elbow pain (OR, 2.34; 95% CI, 1.40-4.11).
Conclusion:
Controlling the amount of practice and its intensity according to the condition of each player in the preadolescent and adolescent periods may be important in accelerating bony healing and decreasing preventable elbow pain in adulthood.
Keywords: medial epicondylar apophysitis, osteochondritis dissecans, age-specific prevalence, elbow pain
The elbow is the most common site of injury in adolescent baseball players.10 Grana and Rashkin9 reported that 58% of older adolescent pitchers experience elbow pain or injury at some point during the baseball season, and occurrence of elbow pain tends to increase with age. Recently, a large questionnaire investigation conducted by the Japanese Orthopaedic Association and the Baseball Federation of Japan revealed that 3742 of 10,228 (36.6%) Japanese adolescent baseball players aged 6 to 13 years had experienced shoulder or elbow pain.2 Another large population study conducted by Kida et al18 found that 57% of Japanese junior high and high school baseball players had experienced elbow pain.
Repetitive valgus stress on the elbow during overhead throwing has been considered the main mechanism of elbow injury. In adult baseball players, the demand on the medial ulnar collateral ligament (MUCL) during the acceleration phase is estimated to be 35 N·m, which exceeds the failure strength of the MUCL (32.1 N·m), and approximately 500 N of compressive force is applied to the humeral capitellum.6 Even in youth baseball players, the elbow valgus force has been estimated to be 18 to 28 N·m; such tremendous stress induces age-specific bone and cartilage injuries in skeletally immature elbows.7,26
Little League elbow, which was defined by Brogden in 1960, is one of the most common throwing injuries, occurring in 20% to 40% of school-aged pitchers.5,17,20
Although there is little reported evidence, the combination of repetitive traction stress on the MUCL and contraction of the flexor pronator muscles is considered to be the main etiology of various types of morphological changes of the medial epicondyle (MEC), such as acute bony avulsion, heterogeneous ossification of the MUCL, and various degrees of widening of the medial epicondylar physis in youth baseball players. In 1965, Adams1 reported on the radiographic appearance of the elbows of 80 Little League pitchers in California, 39 (49%) of whom exhibited medial epicondylar apophyseal fragmentation. Woods and Tullos33 classified MEC avulsion into 3 types based on patient age, fragment size, and MUCL integrity, and small fragmentation of MEC (classified as type III) was the most common type of morphology.16
Although the influence of these MEC lesions on elbow pain and performance has been reported, their clinical significance remains unclear. Several studies have reported that fragmentation of the MEC in skeletally mature baseball players may be a poor prognostic factor in conservative treatment of MUCL injury.8,19 On the other hand, Hang et al11 demonstrated that the presence of radiographic abnormalities in symptomatic players has been somewhat variable, and only half of their study population with MEC separation reported a history of soreness. Furthermore, the natural course of such polymorphic MEC lesions has not yet been well investigated.
Osteochondritis dissecans (OCD) of the humeral capitellum, often seen in preadolescent and adolescent baseball players, has been reported to be a critical injury of the elbow joint because it can induce elbow osteoarthritis and subsequent severe elbow dysfunction.3,30 The cause of capitellar OCD is believed to involve ischemia,14 genetic factors,25,29 and microtrauma28; however, the exact etiology remains unclear.4 Several studies have reported the prevalence and clinical characteristics of capitellar OCD,11,13,18,24 but the precise age of onset and relationship to elbow pain are still unknown.
The use of ultrasonography has been reported for the early detection of elbow injuries, especially MEC lesions and capitellar OCD.13,31 The technology is now implemented into medical checkups for youth baseball players in Japan.12,13,18,24 Since ultrasonography is noninvasive, convenient, and a reliable tool for detecting various elbow injuries, it allows the investigation of morphological changes in not only bone but also the surrounding structures with a high degree of accuracy and without any radiation exposure. The purposes of this study were to investigate the age-specific prevalence of both MEC lesions and capitellar OCD and to clarify their clinical implications using large epidemiologic data obtained from medical checkups of youth baseball players.
Methods
Of the 4605 juvenile baseball players aged 6 to 17 years who underwent a medical checkup, 356 were excluded because they had not received ultrasonographic examination on their elbow, leaving 4249 individuals who were ultimately enrolled.
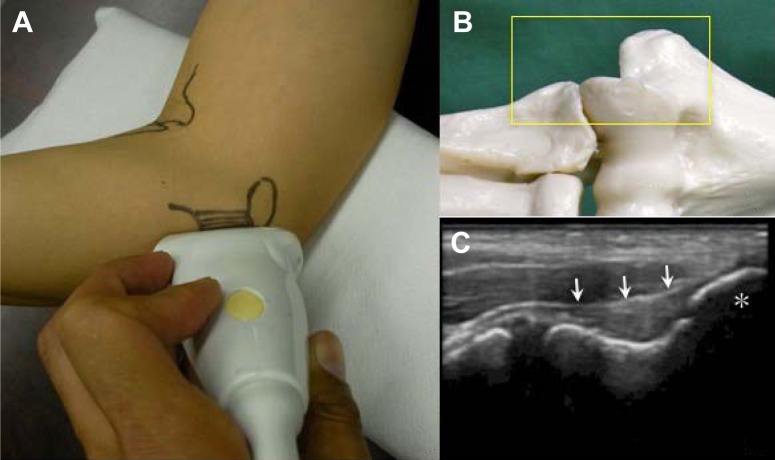
Two methods were employed in the study: a self-completed questionnaire and an ultrasonographic examination. Items on the questionnaire included age, playing position, and history of elbow pain. Elbow pain was assessed using the following question: “Have you ever felt pain or discomfort in your dominant elbow during throwing?” To obtain an accurate answer, we recommended the participants, especially those in the elementary school–aged population, answer the question with the help of their parents. Ultrasonographic examination was performed at the time of medical checkup, which was mainly held in postseason. The medial and lateral aspects of the elbow were assessed by several well-trained orthopaedic surgeons. In principle, ultrasonographic assessment was done on both sides, and the nonthrowing side was considered as a control. The devices used for examination were Mylab125 (Esaote SpA), Titan (Sonosite), Noburus (Hitachi), and Sonimage HS1 (Konica Minolta), with a 10- to 14-MHz high-frequency linear transducer. To assess the medial aspect of the elbow, the elbow was flexed 90°, and the forearm was placed in the supinated position. A linear transducer was placed on the medial aspect of the elbow to obtain an image that included the top of the MEC, the anterior bundle of the MUCL, and the sublime tubercle27 (Figure 1).
Figure 1.
Ultrasonographic examination of the medial elbow. The elbow was flexed 90° and the forearm was placed in the supinated position. (A) A linear transducer was placed on the medial aspect of the elbow to obtain an image that included (B) the top of the medial epicondyle (MEC) (*), the anterior bundle of the medial ulnar collateral ligament (MUCL), and the sublime tubercle. (C) The MUCL (arrow) was identified as a band-like structure that attached to the MEC and sublime tubercle.
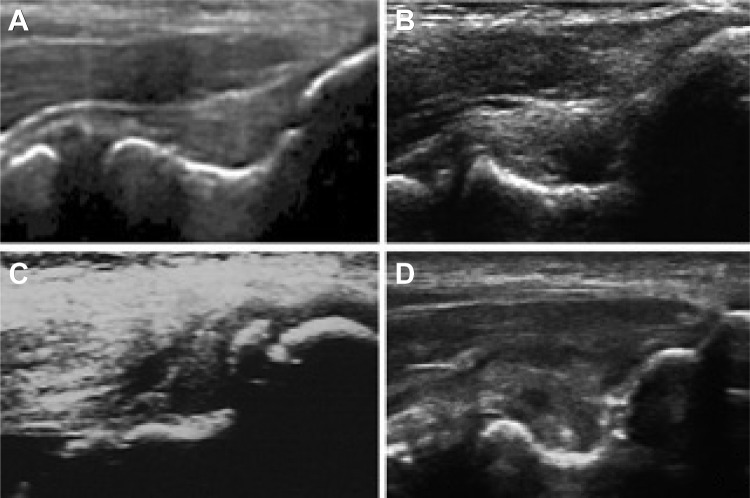
The morphology of the anteroinferior aspect of the MEC, where the MUCL is attached, was classified into 4 types: normal, irregular (IR), fragmented (FG), and hypertrophic (HT)32 (Figure 2).
Figure 2.
Medial epicondyle (MEC) lesion diagnostic criteria. The morphology of the anteroinferior aspect of the MEC, where the medial ulnar collateral ligament is attached, was classified into 4 types: (A) normal, (B) irregular, (C) fragmentated, and (D) hypertrophic.
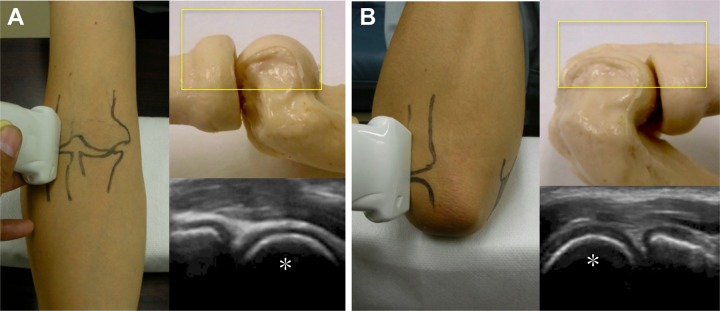
The morphology of the humeral capitellum was also assessed by ultrasonography to determine the presence of OCD. The transducer was first placed on the anterolateral aspect of the elbow in the maximally extended position and then moved to the posterolateral aspect of the elbow in the maximally flexed position18 (Figure 3). A diagnosis of OCD was made based on the irregularity or fragmentation of the subchondral bone of the capitellum24 (Figure 4).
Figure 3.
Ultrasonographic examination of the humeral capitellum. The transducer was first placed on (A) the anterolateral aspect of the elbow in the maximally extended position and then moved to (B) the posterolateral aspect of the elbow in the maximally flexed position. *Humeral capitellum.
Figure 4.
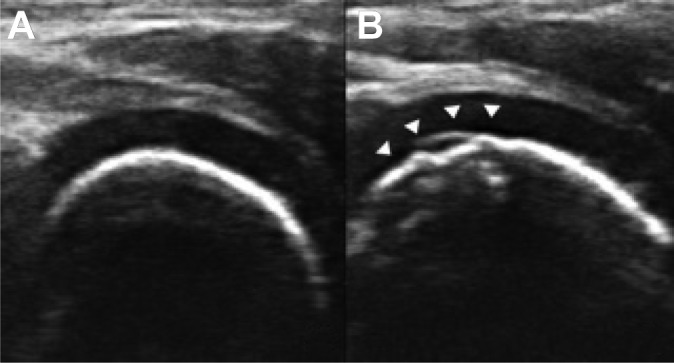
Diagnostic criteria of capitellar osteochondritis dissecans (OCD). (A) No OCD: the subchondral bone is smooth in the normal capitellum. (B) Capitellar OCD was diagnosed by irregularity or fragmentation of the subchondral bone of the capitellum (arrowhead).
The ultrasonographic assessment, patient groupings, and outcome measurements were performed by researchers who were blinded to the patient’s dominant arm and history of pain.
The overall, age-specific, and position-specific prevalence of elbow pain, MEC lesions, and capitellar OCD were investigated. Statistical differences between age and position were assessed using the chi-square test. To investigate the influence of MEC lesions and capitellar OCD on elbow pain, univariate and age- and position-adjusted multivariable analyses were conducted and the odds ratio (OR) was calculated. All tests of statistical significance were 2-tailed, and P values less than .05 were considered statistically significant. All analyses were conducted using JMP version 10.0.2 (SAS Institute Inc).
The Research Ethics Committee of our institute approved the study protocol, and written informed consent was obtained from all participants.
Results
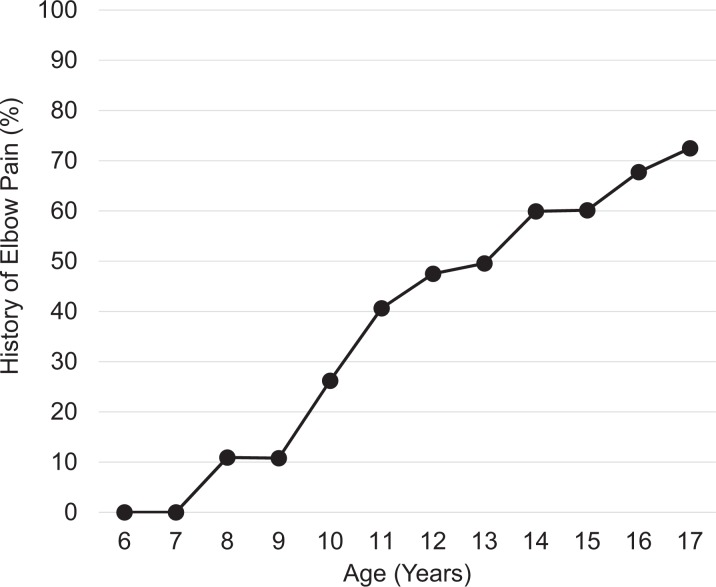
Prevalence of a History of Elbow Pain
Of the 4249 players, 2309 (54.3%) had experienced elbow pain. The prevalence of elbow pain began to increase at age 8 years and dramatically rose beginning at 9 years of age, reaching approximately 50% by the end of 12 years. The prevalence continued to increase and reached 70% at the age of 17 years (Figure 5). As for playing position, history of elbow pain was reported in 67.5% of catchers and 64.8% of pitchers. There was no significant difference between them. Fielders had a significantly lower reported history of elbow pain compared with pitchers and catchers (infielder, 51.8%; outfielder, 44.7%).
Figure 5.
History of elbow pain started to increase at 8 years of age and dramatically rose beginning at 9 years, reaching approximately 50% by the end of 12 years. Seventy percent of players reported a history of elbow pain at the end of high school (age 17 years).
Prevalence of MEC Lesions
The overall prevalence of MEC lesions on the throwing side was 52.9% (2248 patients). Regarding morphology type, HT lesions had the highest prevalence at 36.7%, followed by FG at 9.9% and IR at 6.4%. As for age, the prevalence of FG and IR lesions reached a peak at age 11 to 12 years. After 14 years of age, IR lesions decreased dramatically whereas FG was maintained at approximately 10%. Conversely, the prevalence of HT lesions increased until 16 years of age. The increasing rate of HT lesions was almost the same as that of both FG and IR until 11 years of age; however, it rose sharply, reaching more than 50% at the age of 16 years, while the incidence of IR and FG lesions decreased (Figure 6). As for playing position, pitchers had the highest prevalence of MEC lesions (62.8%), with catchers almost identical at 61.7%; however, fielders had a significantly lower prevalence (infielder, 52.0%; outfielder, 43.0%).
Figure 6.
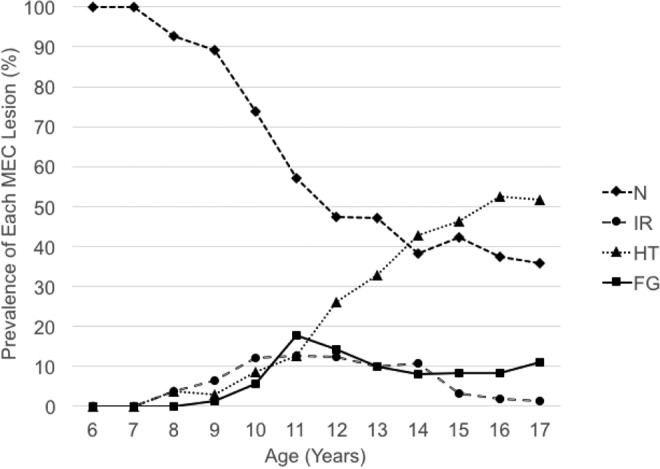
Prevalence of each type of medial epicondyle (MEC) lesion by age. The prevalence of fragmented (FG) and irregular (IR) lesions reached a peak at 11 to 12 years of age. After 14 years of age, IR lesions decreased dramatically whereas FG were maintained at approximately 10%. The prevalence of hypertrophic (HT) lesions increased sharply to 50% at 16 years of age, whereas IR and FG decreased during that time. N, normal.
Prevalence of Capitellar OCD
The overall prevalence of capitellar OCD was 2.2% (93 participants). The prevalence remained fairly consistent among all participants except for in 7- and 8-year-olds, in whom the prevalence was more than 7% (Figure 7). As for playing position, catchers had the highest prevalence of OCD (3.4%) followed by pitchers (2.5%). The prevalence for infielders and outfielders was 2.2% and 1.8%, respectively. There was no significant difference in incidence of OCD by position.
Figure 7.
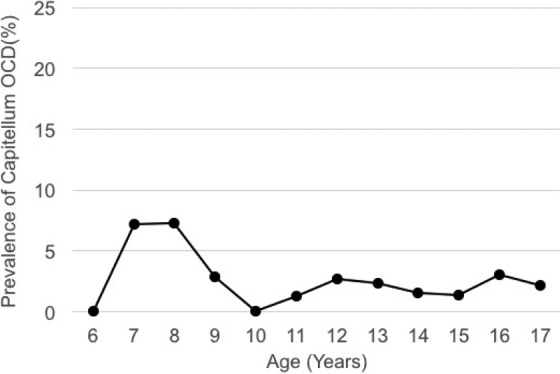
Prevalence of capitellar osteochondritis dissecans (OCD) by age. The prevalence remained at almost the same level at all ages, except for between the ages of 7 and 8 years, where it rose to more than 7%.
Influence of MEC Lesion and Capitellar OCD on Elbow Pain
Patients with MEC lesions more frequently reported a history of elbow pain compared with those without (68.0% vs 39.1%). The highest prevalence was found for FG lesions (74.7%), followed by HT (67.1%) then IR (62.4%) lesions. Patients with capitellar OCD also had a significantly greater reported history of elbow pain compared with those without (77.4% vs 53.8%) (Table 1).
TABLE 1.
Univariate Analysis for the Association Between Position, Age, MEC Lesion, or Capitellar OCD and a History of Elbow Paina
| Total | Elbow Pain (%) | P Value | ||
|---|---|---|---|---|
| Positive | Negative | |||
| Position | <.001 | |||
| Pitcher | 1113 | 721 (64.8) | 392 (35.2) | |
| Catcher | 418 | 282 (67.5) | 136 (32.5) | |
| Infielder | 1385 | 717 (51.8) | 668 (48.2) | |
| Outfielder | 1151 | 514 (44.7) | 637 (55.3) | |
| Unknown | 182 | 75 (41.2) | 107 (58.8) | |
| Age group, y | <.001 | |||
| ≤10 | 486 | 92 (18.9) | 394 (81.1) | |
| 11-12 | 955 | 421 (44.1) | 534 (55.9) | |
| 13-15 | 1182 | 674 (57.0) | 506 (43.0) | |
| 16-17 | 1626 | 1122 (69.0) | 504 (31.0) | |
| MEC lesion | <.001 | |||
| Normal | 2001 | 782 (39.1) | 1219 (60.9) | |
| IR | 271 | 169 (62.4) | 102 (37.6) | |
| HT | 1558 | 1045 (67.1) | 513 (32.9) | |
| FG | 419 | 313 (74.7) | 106 (25.3) | |
| Capitellar OCD | <.001 | |||
| Normal | 4156 | 2237 (53.8) | 1919 (46.2) | |
| OCD | 93 | 72 (77.4) | 21 (22.6) | |
aFG, fragmentated; HT, hypertrophic; IR, irregular; MEC, medial epicondyle; OCD, osteochondritis dissecans.
Of the 93 participants with capitellar OCD, 44 had MEC lesions, and a history of elbow pain was more frequently reported in players with concomitant lesions compared with those without (87.1% and 47.8%, respectively). Age- and position-adjusted multivariable analysis revealed that the presence of MEC lesions led to a greater risk for history of elbow pain, and there was a significantly greater risk for history of pain with the FG lesions (OR, 4.04; 95% CI, 3.16-5.22) compared with IR (OR, 3.22; 95% CI, 2.44-4.27) and HT (OR, 2.03; 95% CI, 1.75-2.36). Capitellar OCD was also associated with a significantly greater risk of a history of elbow pain (OR, 2.34; 95% CI, 1.40-4.11) (Table 2).
TABLE 2.
Age- and Position -Adjusted Odds Ratios for the Association Between Elbow Pain and Each MEC Lesion or Capitellar OCDa
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| Normal | 1 | |
| MEC Lesion | ||
| IR | 3.22 | 2.44-4.27 |
| HT | 2.03 | 1.75-2.36 |
| FG | 4.04 | 3.16-5.22 |
| Capitellar OCD | 2.34 | 1.40-4.11 |
aFG, fragmentation; HT, hypertrophic; IR, irregular; MEC, medial epicondyle; OCD, osteochondritis dissecans.
Discussion
Characteristics of Medial Epicondyle Apophysitis
Although the morphologies of the MEC in baseball players are quite varied, the fundamental pathologies of MEC lesions are considered to be the traction force via MUCL to the skeletally immature MEC. In a radiological study using high-resolution magnetic resonance imaging, Mamizuka et al21 reported that the MEC in a skeletally immature elbows consists of a secondary ossification center and surrounding epiphyseal cartilage. The MUCL was also observed to be attached to the perichondrium, and various morphological abnormalities were detected not only at the ossification center, cartilage, and perichondrium, but also at the surrounding structures, including the MUCL, in cases of acute and chronic baseball elbow.21 These morphological features in the skeletally immature elbow might be the factors behind the polymorphic pattern of MEC lesions observed in youth baseball players.
It is widely considered that hypertrophy of the MEC demonstrated the appearance of bony healing of an avulsion fracture of the MEC. Harada et al12 reported the results of nonoperative treatment of humeral MEC fragmentation in young baseball players, and they considered hypertrophy of the MEC as a bony union following treatment. They also reported that bony union was achieved in 94% of study participants at 2 years after initial presentation and that delayed bone union was associated with resumption of throwing at maximum strength before bone union had occurred. Matsuura et al22 also reported that bony union was achieved in 18 of 20 players after conservative treatment, and they suggested that the degree of displacement may influence the bony healing rate. According to the results of previous studies, insufficient rest and degree of displacement may disturb the healing process of MEC lesions.
Our results suggest that the prevalence of FG lesions dramatically increases between the ages of 9 and 11 years, reaching about 20%; however, this is decreased by half after the age of 14 years. The prevalence of IR lesions also increases along with FG, but mostly diminishes after 15 years of age. Watanabe et al32 reported that IR lesions indicated minimal injury or a very small avulsion of the epiphyseal ossification center and hemorrhage, and FG indicated a large displaced bony avulsion. Although we did not have any knowledge of previous treatment, our results indicated that small and minimally displaced fragmentations may heal completely. To better understand the pathogenesis and achieve better treatment results, we should take into account the age-specific prevalence of each MEC lesion and its trend demonstrated in this study.
Characteristics of Osteochondritis Dissecans
According to our results, the overall prevalence of capitellar OCD in our study population was 2.0%. There have been several reports that investigated the prevalence of OCD,13,15,18,24 and a large-scale survey using ultrasonography has recently been conducted.18,24 Matsuura et al24 studied 1040 baseball players in their latter years of elementary school and reported that the prevalence of OCD was 2.1%. Kida et al18 investigated 2433 junior high and high school baseball players by ultrasonography, with 3.4% being diagnosed as having OCD. However, no report has yet investigated the age-specific prevalence of capitellar OCD. Furthermore, although previous reports have revealed that capitellar OCD is frequently seen in 11- to 16-year-olds, a clear age of onset has not been well discussed. The unique result in our study was that capitellar OCD prevalence remained at almost the same level (approximately 1% to 3%) throughout each age group, except for a temporary increase in between the ages of 7 and 8 years. Matsuura et al24 classified the morphological variations of the humeral capitellum into 3 grades and suggested that the cystic appearance of the subchondral bone surface (grade 1b) may be a variation of normal development during ossification. Since the apophysis of the humeral capitellum may be immature during the earlier years of elementary school, variation of the normal ossification process, such as the irregularity and cystic appearance of the capitellar subchondral bone, may be identified as OCD. In addition, since the prevalence of capitellar OCD did not increase or decrease in players in the latter years of elementary school, the onset of capitellar OCD may have occurred between the ages of 9 and 12 years and was less likely to develop in mature elbows.
According to our study, univariate and multivariate analyses revealed that MEC lesions and capitellar OCD are linked to a significantly greater risk of a history of elbow pain. As for MEC lesions, those with MEC hypertrophy are at a significantly lower risk for elbow pain compared with fragmentation. Harada et al12 also reported that bone union of the MEC fragmentation was associated with a decreased prevalence of elbow pain. These results of the present study suggested that the fragmentation of the MEC may become a risk factor for elbow pain, and we considered that controlling the amount of practice and its intensity according to the condition of each player in the preadolescent and adolescent periods, especially before 14 years of age, may be important in accelerating bony healing and decreasing preventable elbow pain in adulthood.
Capitellar OCD can be responsible for not only elbow pain but also severe elbow dysfunction by inducing osteoarthritis; however, it has been reported that healing ability is significantly greater in the early stage of OCD. Matsuura et al23 reported results of conservative treatment, and 90.5% of patients in the early stage of capitellar OCD were healed completely within 15 months. This suggests that early detection and rapid treatment for such injuries are important to minimize the pain and dysfunction of elbow joints. Furthermore, regardless of whether they have elbow pain, regular screening using ultrasonography intended for skeletally immature young athletes might be effective for the early detection of elbow injuries.
Our study has several limitations. First, it might be difficult to assess current elbow conditions because we investigated only those who experience or had experienced elbow pain during their career. Since we did not correlate ultrasonographic abnormalities with “current” or “recent” pain, the exact relationship between current elbow condition and MEC lesion or OCD was unclear. Second, our study only investigated MEC lesions and capitellar OCD using ultrasonography. It is necessary to also investigate other elbow injuries, such as epiphysiolysis of the MEC or olecranon, which are often seen in adolescent baseball players, to evaluate the exact influence of MEC lesions or capitellar OCD on elbow pain. The third limitation is our study design. We demonstrated the incidence of MEC lesions and capitellar OCD by age; however, we did not follow specific lesions over time, so we could not definitively comment on the natural history of these lesions. A cohort study is required to investigate the exact time course of the morphological changes of the elbow joint and to clarify the association between these morphological changes and the likelihood of elbow pain.
Conclusion
The overall prevalence of MEC lesions and capitellar OCD was 47.1% and 2.2%, respectively. The prevalence of MEC lesions increased with age until 16 years, whereas capitellar OCD had a similar prevalence at all ages. The presence of MEC lesion was linked to greater risk of a history of elbow pain and significantly greater risk of fragmented lesions compared with normal and hypertrophic. Capitellar OCD was also associated with a significantly greater risk of a history of elbow pain.
Acknowledgment
The authors thank and acknowledge the following people for their collaboration and assistance with this study: Tomohiko Shigihara, Hiroki Konno, Shuichi Onoda, Kazuhiro Endo, Takuya Shike, Shohei Nonobe, Takanori Kashimura, Yuichi Jumonji, Kazuhide Takada, Mai Kusano, Toshihisa Nishikata, Takehiro Tabe, Kenta Ono, Akihiro Ueno, and Ryo Ueda, belonging to the Fukushima Physical Therapy Association Medical Support Team.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Research Ethics Committee of Fukushima Medical University.
References
- 1. Adams JE. Injury to the throwing arm. A study of traumatic changes in the elbow joints of boy baseball players. Calif Med. 1965;102:127–132. [PMC free article] [PubMed] [Google Scholar]
- 2. Baseball Federation of Japan. http://www.baseballjapan.org/jpn/uploaded_data/bfj_news/doc/0125/undoki2.pdf. Published May 15, 2015. Accessed September 15, 2016.
- 3. Bauer M, Jonsson K, Josefsson PO, Lindén B. Osteochondritis dissecans of the elbow. A long-term follow-up study. Clin Orthop Relat Res. 1992;284:156–160. [PubMed] [Google Scholar]
- 4. Bradley JP, Petrie RS. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med. 2001;20:565–590. [DOI] [PubMed] [Google Scholar]
- 5. Brogdon BG, Crow NE. Little Leaguer’s elbow. AJR Am J Roentgenol. 1960;83:671–675. [PubMed] [Google Scholar]
- 6. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239. [DOI] [PubMed] [Google Scholar]
- 7. Fleisig GS, Barrentine SW, Zheng N, Escamilla RF, Andrews JR. Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech. 1999;32:1371–1375. [DOI] [PubMed] [Google Scholar]
- 8. Furushima K, Urata D, Miyamoto A, Iwabu S, Itoh Y. The disorder of the elbow medial support structure in adult baseball player—about the effect against UCL injury of a medial epicondylar fragment. Jpn J Orthop Sports Med. 2014;34:148–152. [Google Scholar]
- 9. Grana WA, Rashkin A. Pitcher’s elbow in adolescents. Am J Sports Med. 1980;8:333–336. [DOI] [PubMed] [Google Scholar]
- 10. Gugenheim JJ, Stanley RF, Woods GW, Tullos HS. Little League survey: the Houston study. Am J Sports Med. 1976;4:189–199. [DOI] [PubMed] [Google Scholar]
- 11. Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med. 2004;32:79–84. [DOI] [PubMed] [Google Scholar]
- 12. Harada M, Takahara M, Hirayama T, Sasaki J, Mura N, Ogino T. Outcome of nonoperative treatment for humeral medial epicondylar fragmentation before epiphyseal closure in young baseball players. Am J Sports Med. 2012;40:1583–1590. [DOI] [PubMed] [Google Scholar]
- 13. Harada M, Takahara M, Sasaki J, Mura N, Ito T, Ogino T. Using sonography for the early detection of elbow injuries among young baseball players. AJR Am J Roentgenol. 2006;187:1436–1441. [DOI] [PubMed] [Google Scholar]
- 14. Haraldsson S. On osteochondrosis deformas juvenilis capituli humeri including investigation of intra-osseous vasculature in distal humerus. Acta Orthop Scand Suppl. 1959;38:1–23. [PubMed] [Google Scholar]
- 15. Iwase T. Elbow osteochondral lesion in young baseball players. Jpn J Pediatr Surg. 1996;28:703–710. [Google Scholar]
- 16. Jonas R, Rudzki JR, George MS, Paletta A., Jr Juvenile and adolescent elbow injuries in sports. Clin Sports Med. 2004;23:581–608. [DOI] [PubMed] [Google Scholar]
- 17. Kerut EK, Kerut DG, Fleisig GS, Andrews JR. Prevention of arm injury in youth baseball pitchers. J La State Med Soc. 2008;160:95–98. [PubMed] [Google Scholar]
- 18. Kida Y, Morihara T, Kotoura Y, et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014;42:1963–1971. [DOI] [PubMed] [Google Scholar]
- 19. Komatsu S, Tsuruta T, Mine H, et al. Follow-up study of medial epicondylar fragmentation of the elbow joint in young baseball players [in Japanese]. J Jpn Soc Clin Sports Med. 2013;21:57–61. [Google Scholar]
- 20. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33:1803–1810. [DOI] [PubMed] [Google Scholar]
- 21. Mamizuka N, Hirano A, Yamazaki M. High-resolution magnetic resonance imaging for elbow injuries in youth baseball player [in Japanese]. Orthop Surg. 2013;64:2–6. [Google Scholar]
- 22. Matsuura T, Kashiwaguchi S, Iketa T, Iwase T. A follow up study of humeral medial epicondyle lesion among young baseball players. Jpn J Orthop Sports Med. 1997;17:263–269. [Google Scholar]
- 23. Matsuura T, Kashiwaguchi S, Iwase T, Takeda Y, Yasui N. Conservative treatment for osteochondrosis of the humeral capitellum. Am J Sports Med. 2008;36:868–872. [DOI] [PubMed] [Google Scholar]
- 24. Matsuura T, Suzue N, Iwame T, Nishio S, Sairyo K. Prevalence of osteochondritis dissecans of the capitellum in young baseball players: results based on ultrasonographic findings. Orthop J Sports Med. 2014;2:2325967114545298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Neilsen NA. Osteochondritis dissecans capituli humeri. Acta Orthop Scand. 1933;4:307–418. [Google Scholar]
- 26. Sabick MB, Torry MR, Lawton RL, Hawkins RJ. Valgus torque in youth baseball pitchers: a biomechanical study. J Shoulder Elbow Surg. 2004;13:349–355. [DOI] [PubMed] [Google Scholar]
- 27. Sasaki J, Takahara M, Ogino T, Kashiwa H, Ishigaki D, Kanauchi Y. Ultrasonographic assessment of the ulnar collateral ligament and medial elbow laxity in college baseball players. J Bone Joint Surg Am. 2002;84-A:525–531. [DOI] [PubMed] [Google Scholar]
- 28. Slocum DB. Classification of elbow injuries from baseball pitching. Tex Med. 1968;64:48–53. [PubMed] [Google Scholar]
- 29. Stougaard J. Familial occurrence of osteochondritis dissecans. J Bone Joint Surg Br. 1964;46:542–543. [PubMed] [Google Scholar]
- 30. Takahara M, Ogino T, Sasaki I, Kato H, Minami A, Kaneda K. Long-term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res. 1999;363:108–115. [PubMed] [Google Scholar]
- 31. Takahara M, Ogino T, Tsuchida H, Takagi M, Kashiwa H, Nambu T. Sonographic assessment of osteochondritis dissecans of the humeral capitellum. AJR Am J Roentgenol. 2000;174:411–415. [DOI] [PubMed] [Google Scholar]
- 32. Watanabe C, Mihata T, Fujisawa Y, Kinoshita M, Yasui K, Kawakami T. Utility of ultrasonographic evaluation for baseball elbow in medical check-ups Jpn J Orthop Sports Med. 2012;32:2–6. [Google Scholar]
- 33. Woods GW, Tullos HS. Elbow instability and medial epicondyle fractures. Am J Sports Med. 1977;5:23–30. [DOI] [PubMed] [Google Scholar]