Abstract
Background and aims
Some studies have explored the prevalence of pancreatic cystic lesions (PCLs). Only one study based on magnetic resonance imaging (MRI) report examination focused specifically on intraductal papillary mucinous neoplasm (IPMN) in a European general population. The aim of this study was to evaluate the prevalence of IPMN in a population of patients who had MRI for a non-pancreatic disease.
Methods
We conducted a retrospective, single-center study. All consecutive patients placed on the French liver transplant waiting list who had MRI for a non-pancreatic disease before liver transplantation between 2009 and 2013 were included. Only diagnoses consistent with IPMN were retained (cyst(s) clearly communicating with the main pancreatic duct).
Results
Among 315 patients on the national waiting list, 212 patients had an MRI. PCLs with ductal communication were diagnosed in 14 patients (6.6%; six women, eight men, median age 62 years (45–70)). Liver disease was caused by a virus in seven cases, alcohol in three cases, other in four cases (multiple causes possible). Four patients had hepatocellular carcinoma. No patient had clinical or radiological sign of chronic pancreatitis. The median diameter of the largest cystic lesion was 14 mm (7–22). The number of PCLs was one (n = 4), two (n = 2), four (n = 3), five (n = 2), > 5 (n = 3), respectively. There was no worrisome or main pancreatic duct involvement.
Conclusions
Prevalence of pancreatic cystic lesions consistent with the diagnosis of IPMN was 6.6% in French patients waiting for liver transplantation. These results underscore that IPMN can be considered as a public health problem and justify a screening.
Keywords: Prevalence, intraductal papillary mucinous neoplasm, magnetic resonance imaging
Introduction
Prevalence of pancreatic cystic lesions (PCLs) in the general population is within the range of 1.2% to 36.7%.1–5 Intraductal papillary mucinous neoplasms (IPMN) are defined by adenomatous proliferation of pancreatic duct epithelium in the main pancreatic duct (MPD-IPMN), the branch ducts (BD-IPMN), or both. IPMN represents 18% of surgically resected cystic pancreatic neoplasms.6 Fernández-del Castillo et al. found 27% of patients with IPMN among 78 patients with asymptomatic pancreatic cystic lesions diagnosed using computed tomography, transabdominal ultrasound or magnetic resonance imaging (MRI).4
IPMN was considered a rare disease when it was discovered. However, there are increasing data showing that its prevalence might be higher than previously thought in the general population because of a high frequency of an asymptomatic form discovered incidentally.
Few studies have assessed the specific prevalence of IPMN in Europe. Baiocchi et al. found a 4.73% prevalence of IPMN discovered with MRI in the general population.7
The aim of this study was to evaluate the prevalence of IPMN in a population of French patients who had an MRI for a non-pancreatic disease.
Materials and methods
This is a retrospective, single-center study.
Patients
All patients who were on the waiting list for liver transplantation (LT) in our center between May 2009 and July 2013 were identified from a database. Only patients who had preoperative MRI for a non-pancreatic reason were included. MRI was indicated for pre-transplant workup (e.g. biliary anatomy description, characterization of liver tumors).
The following data were recorded for every patient: demographic data (age at diagnosis, gender, body mass index), clinical data (date and indication for LT, previous history of alcohol consumption and tobacco use, previous familial pancreatic cancer history). Patients with known pancreatic disease were excluded.
Imaging evaluation and diagnostic criteria
MRIs were reviewed by an expert radiologist (MPV), who was blinded to the patients’ clinical course.
MRI examinations were performed with 1.5-T superconducting MR systems using a four-channel phased array coil: Gyroscan ACS-NT and Ingenia (Philips Medical System, Best, the Netherlands), and Sigma (GE HealthCare, Milwaukee, WI, USA). The MR protocol included transverse and coronal T2-weighted imaging with a single-shot fast spin-echo sequence, a transverse breath-hold three-dimensional (3D) T1-weighted, fat-suppressed, spoiled gradient-recalled-echo (dynamic gadolinium-enhanced) sequence before and after dynamic injection of 0.1 mmol/kg of body weight of gadolinium chelates with a power injector at a rate of 2–2.5 ml/s. Contrast-enhanced images were acquired in the pancreatic (35–45 s after injection), portal venous (75–80 s after injection) and delayed (180 s after injection) phases. Two-dimensional magnetic resonance cholangiopancreatography (MRCP) T2-thick slice (25 mm MRCP with a radiated set of thick slices (25–30 mm) were acquired on the biliary tree and head and body of the pancreas (including pancreatobiliary junction) (at least six slices).
The diagnosis of BD-IPMN was considered by the presence of at least one pancreatic cyst (size > 5 mm) clearly communicating with pancreatic ducts with a non-dilated (<5 mm) main pancreatic duct. MPD involvement was considered as probable if its diameter was ≥5 mm in absence of downstream obstacle.8,9
The radiological data collected were: maximal transversal cyst size, number of cysts, communication with the main pancreatic duct, and maximal diameter of the main pancreatic duct, location of IPMN in different segments of the pancreas (head, neck, body, and tail, multifocal). In patients with multifocal BD-IPMN, data from the largest cyst were considered.
For each patient “worrisome features” (size of IPMN > 3 cm, MPD size between 5 to 9 mm, minor symptoms, pancreatitis, non-enhancing nodules, and/or atypical cells at cytology) and “high-risk stigmata” (jaundice, MPD ≥ 10 mm, enhancing nodules, and/or cytology positive for high-grade dysplasia or adenocarcinoma) as defined in the 2012 International consensus guidelines were searched for10 as well as the presence of a parenchyma solid lesion mimicking an infiltrative adenocarcinoma.11
Statistical analysis
General characteristics were expressed as median and range or percentages. Comparison of general characteristics, clinical features and morphological characteristics were performed using the Kruskal-Wallis test for continuous data and the Chi2 test or the Fisher’s exact test for categorical data. Data were analyzed with the SAS 9.1 statistical software for Windows (SAS Institute Inc, Cary, NC, USA). All statistical tests were two sided. The critical level of statistical significance was set at p < 0.05.
Results
Clinical data
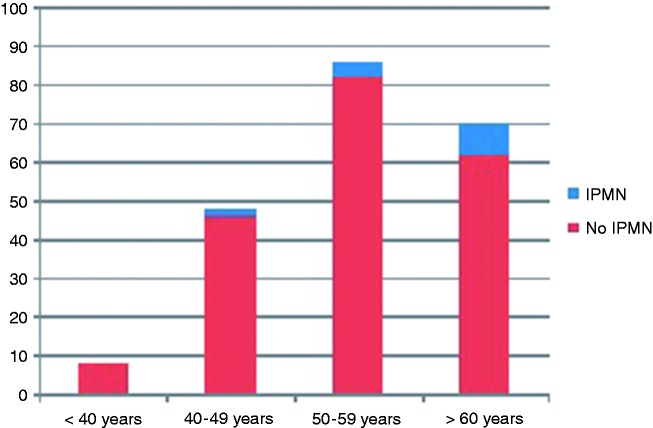
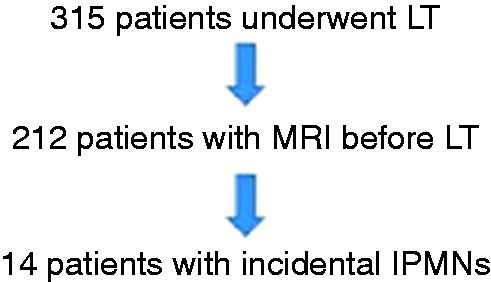
A total of 315 patients who were on the LT list at Beaujon Hospital between May 2009 and July 2013 were screened. Among them, 212 had a preoperative MRI. Pancreatic cystic lesions consistent with the diagnosis of IPMN were present in 14 patients (6.6%) (Figure 1). Distribution of IPMN lesions in the cohort according to the age of the patients is described in Figure 2. Eight patients were older than 60 years (8/70 patients, 11.4%), four patients were between 50 and 59 years of age (4/86 patients, 4.7%), and two patients were between 40 and 49 years of age (2/48 patients, 4.2%), p = 0.19. Prevalence of IPMN for patients older than 60 years was 11.4% (8/70 patients) versus 4.2% for patients younger than 60 years (6/142 patients), p = 0.065. MRCP was performed in 90/198 patients without IPMN (45%) and in 7/14 of those with IPMN (50%, NS).
Figure 1.
Flowchart.
LT: liver transplantation; MRI: magnetic resonance imaging; IPMNs: intraductal papillary mucinous neoplasms.
Figure 2.
Distribution of IPMN lesions in the cohort according to patient age.
IPMN: intraductal papillary mucinous neoplasm.
The general characteristics of these 212 patients are presented in Table 1. Frequency of IPMN was 4.6% and 16.2% in males and females, respectively (p = 0.01). Patients with IPMN were older, less frequently smokers than those without IPMN. The median age at IPMN diagnosis was 62 years (range: 45–69). The main indication for liver transplantation was viral cirrhosis (seven patients (50%); five with hepatitis C– and two with hepatitis B) and alcoholic cirrhosis (three patients, 22%). Four (29%) of these patients had hepatocellular carcinoma. No patient had familial history of pancreatic cancer. No patient had pancreatic symptoms.
Table 1.
General characteristics of the patients with MRI.
| Patients with IPMN | Patients without IPMN | p | |
|---|---|---|---|
| No. of patients, n (%) | 14 (7%) | 198 (93%) | |
| Age (year, range) | 62 (45-69) | 55 (31-70) | 0.014 |
| Male (n) | 8 (57%) | 167 (84%) | 0.01 |
| Smoking history, n (%) | |||
| Never smoked | 11 (79%) | 85 (43%) | 0.0094 |
| Current smoker | 2 (14%) | 71 (36%) | 0.1 |
| Ex-smoker | 1 (7%) | 42 (21%) | 0.2 |
| BMI (kg/m2) | 28 (19–31) | 26 (18–43) | 0.36 |
| Cirrhosis etiology, n (%) | |||
| Virus | 7 (50%) | 106 (53%) | 0.66 |
| Alcohol | 3 (21%) | 83 (42%) | |
| Others | 4 (29%) | 60 (30%) | |
| Hepatocellular carcinoma | 4 (29%) | 95 (48%) | 0.64 |
MRI: magnetic resonance imaging; IPMN: intraductal papillary mucinous neoplasms; BMI: body mass index.
Morphological data
All patients had BD-IPMN, no patient had MPD-IPMN.
Cyst characteristics are detailed in Table 2. Ten patients had more than one cyst. Cysts were located mainly in the body (eight patients, 57%). The median size of the largest cyst was 14.2 mm (range 7–22). There was no dilatation of the main pancreatic duct, any “worrisome features” or “high-risk stigmata” on MRI, and no parenchyma tumor. No patient had an imaging sign of chronic pancreatitis.
Table 2.
Cyst characteristics.
| Median cyst size, mm (range) | 14 (7–22) |
|---|---|
| Cyst number, n (%) | |
| 1 | 4 (29) |
| 2 | 2 (14.5) |
| 4 | 3 (21) |
| 5 | 2 (14.5) |
| >5 | 3 (21) |
| Cyst location, n (%) | |
| Head | 7 (50) |
| Neck | 3 (21) |
| Body | 8 (57) |
| Tail | 6 (43) |
| Multifocal | 2 (14.5) |
Six patients (43%) had a second MRI during the follow-up. MRI was performed a median time of eight months (range, 8–18) after LT and 13 months (range, 3–17 months) after the first MRI. New pancreatic cysts were diagnosed in two patients without worrisome features or high-risk stigmata. In one patient with four cysts, one cyst increased from 5 mm to 10 mm without worrisome features. In three patients, no change in cyst size was observed. No patients underwent surgery for IPMN or developed pancreatic adenocarcinoma.
Discussion
This study was based on a large cohort of French patients who had an MRI for a non-pancreatic reason (LT work-up). The main finding is that the prevalence of IPMN in this population was 6.6%. Prevalence of IPMN increases with age, 11.4% in patients older than 60 years.
The present study has limitations. This is a single-center, retrospective study and no systematic follow-up was performed after LT. However, all MRI were reviewed by an expert in pancreatic diseases. Although the population was highly selected, the prevalence we found might reflect that of the general population since: (a) MRI was performed for a non-pancreatic disease; (b) there are no data in the literature suggesting that alcohol consumption or virus B and C might be risk or protective factors for IPMN, (c) there are no data suggesting that liver cirrhosis might be associated with an increased or a lowered risk of IPMN. Whether this reflects the true figures in the general population remains to be demonstrated.
Only scarce data are available on the prevalence of IPMN in the general population. Most studies based on imaging procedures reported prevalence of pancreatic cysts from 1.2% to 36.7% without any data about the nature of the cyst lesions.1–5 Among them two were based on MRI. Lee et al. reviewed retrospectively abdominal MRI performed at their institution. Patients were excluded from the study if they had a known or suspected history of pancreatic disease or if they had symptoms related to the pancreas. Prevalence of incidental pancreatic cysts detected was 13.5%.5 Zhang et al. reported a higher rate, around 20%, in 1444 Americans who had a systematic MRI. The frequency of cysts as well as multiple cysts increased with age like in our study.2 In an autopsy study of 300 cases, a prevalence of 24.3% of pancreatic cysts was reported.12 None of these studies reported the proportion of IPMN.
Baiocchi et al. reviewed all reports of MRCP performed in an academic Italian hospital from 2005 to 2010. They identified all patients diagnosed with IPMN without reviewing MRI slices. The specific prevalence of IPMN was 4.73%. Median age was 69.7 years (range: 38–97).7 All these figures are in accordance with the present results.
A surrogate result of the present study is that there are no data suggesting an increased risk of malignant evolution in this population exposed to immunosuppressive therapy, but our data are too scarce to draw any conclusions. This confirms two recent short studies.13,14 However, the question whether IPMN in immunocompromised patients deserves a closer follow-up remains open.
In conclusion, prevalence of IPMN in a population without pancreatic symptoms is 6.6%. These results underscore that IPMN can be considered a public health problem and justify a screening.
Acknowledgments
Author contributions are as follows: Conception and design: LL, MPV, VR, FM, OH, CF, FD, PR and PL Analysis and interpretation of data: LL, MPV, VR and PL Drafting of the article: LL, MPV, VR and PL Critical revision of the article for important intellectual content: LL, MPV, VR, FM, OH, CF, FD, PR and PL Final approval of the article: LL, MPV, VR and PL
Declaration of conflicting interests
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol 2008; 191: 802–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang XM, Mitchell DG, Dohke M, et al. Pancreatic cysts: Depiction on single-shot fast spin-echo MR images. Radiology 2002; 223: 547–553. [DOI] [PubMed] [Google Scholar]
- 3.Spinelli KS, Frouwiller TE, Daniel RA, et al. Cystic pancreatic neoplasms: Observe or operate. Ann Surg 2004; 239: 651–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernández-del Castillo C, Targarona J, Thayer SP, et al. Incidental pancreatic cysts: Clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg 2003; 138: 427–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee KS, Sekhar A, Rofsky NM, et al. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol 2010; 105: 2079–2084. [DOI] [PubMed] [Google Scholar]
- 6.Kosmahl M, Pauser U, Peters K, et al. Cystic neoplasms of the pancreas and tumor-like lesions with cystic features: A review of 418 cases and a classification proposal. Virchows Arch 2004; 445: 168–178. [DOI] [PubMed] [Google Scholar]
- 7.Baiocchi GL, Portolani N, Grazioli L, et al. Management of pancreatic intraductal papillary mucinous neoplasm in an academic hospital (2005–2010): What follow-up for unoperated patients? Pancreas 2013; 42: 696–700. [DOI] [PubMed] [Google Scholar]
- 8.Irie H, Yoshimitsu K, Aibe H, et al. Natural history of pancreatic intraductal papillary mucinous tumor of branch duct type: Follow-up study by magnetic resonance cholangiopancreatography. J Comput Assist Tomogr 2004; 28: 117–122. [DOI] [PubMed] [Google Scholar]
- 9.Lévy P, Jouannaud V, O’Toole D, et al. Natural history of intraductal papillary mucinous tumors of the pancreas: Actuarial risk of malignancy. Clin Gastroenterol Hepatol 2006; 4: 460–468. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka M, Fernández-del Castillo C, Adsay V, et al. International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 2012; 12: 183–197. [DOI] [PubMed] [Google Scholar]
- 11.Vullierme MP, Giraud-Cohen M, Hammel P, et al. Malignant intraductal papillary mucinous neoplasm of the pancreas: In situ versus invasive carcinoma surgical resectability. Radiology 2007; 245: 483–490. [DOI] [PubMed] [Google Scholar]
- 12.Kimura W, Nagai H, Kuroda A, et al. Analysis of small cystic lesions of the pancreas. Int J Pancreatol 1995; 18: 197–206. [DOI] [PubMed] [Google Scholar]
- 13.Lennon A, Victor D, Zaheer A, et al. Liver transplant patients have a risk of progression similar to that of sporadic patients with branch duct intraductal papillary mucinous neoplasms. Liver Transpl 2014; 20: 1462–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill KR, Pelaez-Luna M, Keaveny A, et al. Branch duct intraductal papillary mucinous neoplasm of the pancreas in solid organ transplant recipients. Am J Gastroenterol 2009; 104: 1256–1261. [DOI] [PubMed] [Google Scholar]