Abstract
Odontogenic tumours are a group of heterogeneous diseases that range from hamartomatous or non-neoplastic tissue proliferations to benign neoplasms to malignant tumours with metastatic potential. They are rare, comprising about <2–3% of all oral and maxillofacial biopsy specimens. The aim of the present study was to determine the clinico-pathological presentation of this heterogeneous group of lesions and review of literature. The present study was conducted in the ENT department of a Government Medical College and Hospital, West Bengal, India, over the period of 5 years from January 2011 to December 2015. It included a total of 15 patients who were clinico-radiologically diagnosed as odontogenic tumours, and were given appropriate treatment. Their diagnostic and management approaches are discussed. Among 15 odontogenic tumours, 13 were benign and two were malignant. Male to female ratio was 2:3. Mandible to maxilla ratio was 1.8:1. The patients were in between 4 and 56 years of age with highest incidence in 3rd decade of life. All patients are doing well till date with a minimum follow-up of 1 year. Incisional biopsy is considered as gold standard for preoperative diagnosis but FNAC can offer clinicians a less invasive alternative. CT is the choice of investigation for study of lesion, analysis of its extension and surgical planning. The challenge to proper management lies in balancing between conservative and radical approach to reduce morbidity and recurrence both. Final diagnosis is made by post-operative histopathological examination.
Keywords: Odontogenic tumours, Jaw, CT scan, Biopsy, Follow-up
Introduction
Odontogenic tumours are a group of heterogeneous diseases that range from hamartomatous or non-neoplastic proliferations to benign neoplasms to malignant tumours with metastatic potential [1, 2]. They are derived from epithelial, ectomesenchymal and/or mesenchymal elements of tooth-forming apparatus. Odontogenic tumours are rare, comprising about <2–3% of all oral and maxillofacial biopsy specimens sent to pathology department [3]. They pose a significant diagnostic and therapeutic challenge. Knowledge of basic clinical features such as age, sex, and location can be extremely valuable in developing differential diagnoses of odontogenic tumours. Available literature of on odontogenic tumors are mostly among Africans and Americans. Very few studies are reported among Asians, especially from the Indian subcontinent [4]. The aim of the present study was to evaluate the clinico-pathological presentation of this heterogeneous group of lesions and review of literature.
Materials and Methods
The present prospective study was conducted in the ENT department of a Government Medical College and Hospital, West Bengal, India, over the period of 5 years from January 2011 to December 2015. It included a total of 15 patients who were clinico-radiologically diagnosed as odontogenic tumours, and were given appropriate treatment. Odontogenic cysts and non-odontogenic tumours like squamous cell carcinomas were excluded from the study. Tumours were grouped under three main headings as per WHO guidelines (2005). A detailed history including age, sex and location of the tumour was taken followed by a thorough clinical examination of the patient. Radiological examination included orthopantomogram (OPG), CT scan or MRI whichever was appropriate for the specific case. Pre-operative cytological or histopathological examination was performed in suitable cases. The treatment modalities were based on clinical, radiological and wherever possible cytological or histopathological diagnosis. All patients with benign tumours were managed by appropriate surgery. Patients with malignant tumours were managed by surgery along with radiotherapy and/or chemotherapy. All patients were followed up regularly for a minimum of 1 year (Figs. 1, 2, 3, 4).
Fig. 1.
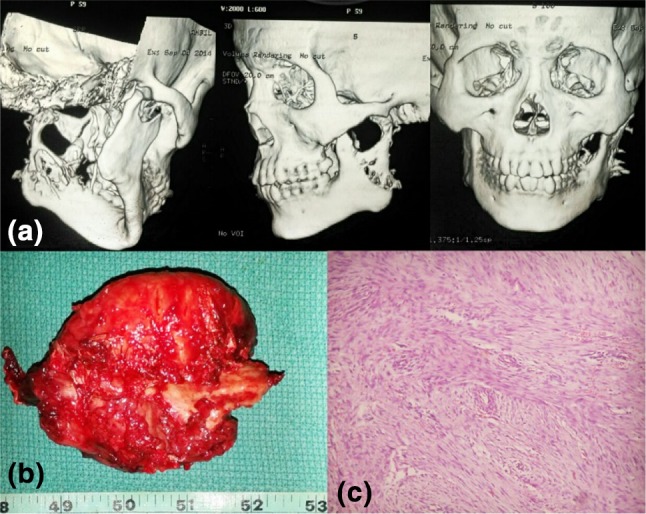
a 3D CT reconstruction of Case no. 4. b Specimen of segmental mandibulectomy. c Post-operative histopathological picture suggesting odontogenic fibromyxoma
Fig. 2.
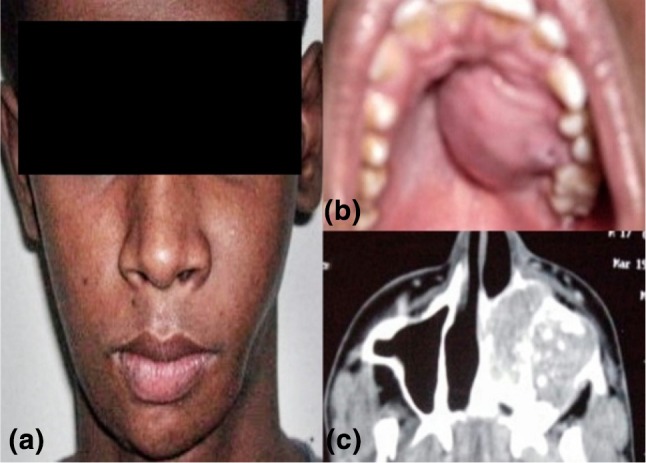
a Profile picture of Case no. 5 with swelling of left cheek. b Intraoral picture of Case no. 5 showing left sided palatal bulge. c CECT of nose and PNS axial section showing expansible mass with calcified matrix arising from left maxillary sinus with extension into left nasal cavity
Fig. 3.

a Profile picture of case no. 11 with swelling over left angle of mandible. b Intra-operative picture of left segmental mandibulectomy. c Post-operative histopathological picture suggesting ameloblastic carcinoma. d Follow-up at 1 month post-op
Fig. 4.

a Profile picture of Case no. 14 with right sided proptosis. b CECT of nose and PNS axial section showing sinonasal mass pushing right eyeball. c Specimen of right medial maxillectomy with removal of the tumour. d Follow-up at 1 month post-op
Results
A total of 15 cases with odontogenic tumours were diagnosed and treated during the 5 years period from January 2011 to December 2015. Of the 15 odontogenic tumours, 13 were benign and two were malignant. Among these, six were in males and nine were females (M:F = 2:3). Nine tumors were encountered in mandible, five in maxilla and one in ethmoid, with an overall mandible to maxilla ratio of 1.8:1. The patients were in between 4 and 56 years of age with highest incidence in 3rd decade of life (Table 1). Clinical, radiological and pre-operative cytological or histological findings are described in Table 2. Treatment and final histopathological diagnosis are discussed in Table 3. All patients are doing well till date with a minimum follow-up of 1 year.
Table 1.
Distribution of patients according to age, sex and site of tumour
| Case number | Age (years) | Sex | Site |
|---|---|---|---|
| 1 | 23 | Female | Right angle of mandible |
| 2 | 27 | Female | Right ramus of mandible |
| 3 | 28 | Female | Right maxilla |
| 4 | 17 | Male | Left angle and ramus of mandible |
| 5 | 18 | Male | Left maxilla |
| 6 | 46 | Female | Left angle of mandible |
| 7 | 32 | Female | Left angle of mandible |
| 8 | 56 | Female | Right side of body of mandible |
| 9 | 26 | Male | Left maxilla |
| 10 | 37 | Male | Right posterior ethmoid |
| 11 | 55 | Male | Left angle of mandible |
| 12 | 34 | Male | Body of mandible |
| 13 | 16 | Female | Left maxilla |
| 14 | 4 | Female | Right maxilla |
| 15 | 21 | Female | Body of mandible |
Table 2.
Distribution of patients according to clinical and radiological features
| Case number | Clinical features | Radiological features | Pre-operative FNAC/HPE |
|---|---|---|---|
| 1 | ~5 × 3 cm2swelling over right angle of mandible for 4 years | Well defined multi-loculated lytic lesion over right angle of mandible with soap bubble appearance | Not done |
| 2 | ~7.5 × 5 cm2 swelling over right ramus of mandible for 9 years | Well defined multi-loculated lytic lesion over right ramus of mandible with soap bubble appearance | HPE—ameloblastoma |
| 3 | Swelling over right cheek and right half of palate for 4 years, right nasal obstruction with intermittent epistaxis for 2 years | ~8 × 6 cm2 expansile bony mass with ground glass appearance involving right maxillary sinus andnasal cavity | Not done |
| 4 | ~8 × 6.5 cm2 swelling over left angle and ramus of mandible for 2 years, pain for 3 months | Well capsulated mass over left ramus of mandible with bony septations | FNAC—inconclusive |
| 5 | ~5 × 4 cm2 swelling over left cheek for 3 years | Expansile mass with calcified matrix involving left maxillary sinus and nasal cavity | Not done |
| 6 | ~4 × 3 cm2 swelling over left angle of mandible for 31/2 years | Well defined multi-loculated lytic lesion over left angle of mandible with soap bubble appearance | Not done |
| 7 | ~6 × 4 cm2 swelling over left angle of mandible for 5 years | Well-defined circular radio-opacity at left body and angle of mandible | Not done |
| 8 | ~9 × 6 cm2 swelling in right lower jaw for last 21/2 years and pain for last 6 months | Expansile osteolytic lesion in the right side of body of mandible | Not done |
| 9 | ~3 × 3 cm2 swelling over left cheek for 11/2 years | Well capsulated mass in left maxilla with bony septations | Not done |
| 10 | Headache for 2 years | Bony mass with ground glass appearance involving right posterior ethmoids | Not done |
| 11 | ~5×4 cm2 swelling over left angle of mandible for 7 years | Multi-loculated lytic lesion over left angle of mandible with ill-defined borders | FNAC—ameloblastoma |
| 12 | ~3 × 2 cm2 swelling over chin for 41/2 years | Well defined multi-loculated lytic lesion over body of mandible with soap bubble appearance | Not done |
| 13 | ~2.5 × 2 cm2 firm swelling over left cheek for 2 years, left sided proptosis for 1 year | Heterogeneously enhancing growth involving left maxillary sinus and left nasal cavity with destruction of medial wall and floor of left maxillary sinus | HPE—malignant round cell tumour IHC—PNET |
| 14 | Right sided nasal obstruction and Epistaxis for 1 year, right cheek swelling and proptosis for 6 months | ~7 × 5 cm2osteolyticmultiloculated lesion in right maxilla | HPE—haemangio-pericytoma |
| 15 | ~4 × 4 cm2 swelling over chin for 6 years | Well defined multi-loculated lytic lesion over body of mandible with soap bubble appearance | Not done |
Table 3.
Distribution of patients according to treatment and post-operative HPE report
| Case number | Treatment | Post-operative HPE |
|---|---|---|
| 1 | Right segmental mandibulectomy | Ameloblastoma |
| 2 | Right segmental mandibulectomy | Ameloblastoma |
| 3 | Right medial maxillectomy | Fibrous dysplasia |
| 4 | Left segmental mandibulectomy | Odontogenic fibromyxoma |
| 5 | Left partial maxillectomy | Cemento-ossifying fibroma |
| 6 | Left segmental mandibulectomy | Ameloblastoma |
| 7 | Left segmental mandibulectomy | Cementoblastoma |
| 8 | Right segmental mandibulectomy | Brown tumour of hyperparathyroidism |
| 9 | Left partial maxillectomy | Odontogenic fibromyxoma |
| 10 | Right ethmoidectomy | Fibrous dysplasia |
| 11 | Left segmental mandibulectomy followed by radiotherapy | Ameloblastic carcinoma |
| 12 | Segmental mandibulectomy | Ameloblastoma |
| 13 | Chemotherapy (ifosphamide, vincristine, etoposide, actinomycin D, doxorubicin) and radiotherapy followed by salvage left total maxillectomy, reconstruction with temporalis muscle rotational flap | PNET |
| 14 | Right partial maxillectomy | Giant cell tumour |
| 15 | Segmental mandibulectomy | Ameloblastoma |
Discussion
Odontogenic tumours are derived from tooth-forming elements. Odontogenesis occurs through a complex process involving enamel organ, dental follicle, and dental papilla. The enamel organ is an epithelial structure, derived from oral ectoderm. The dental follicle and dental papilla are derived from neural crest cells and are therefore ectomesenchymal in nature. Odontogenic tumours demonstrate varying interactions between the odontogenic epithelium and odontogenic ectomesenchyme, and are sub-classified by their tissue of origin [3] These tumours are grouped under three main headings as per WHO guidelines (2005): malignant (odontogenic carcinoma and odontogenic sarcoma), benign (Odontogenic epithelium without odontogenic ectomesenchyme; Odontogenic epithelium with odontogenic ectomesenchyme; Mesenchyme and/or odontogenic ectomesenchyme with or without odontogenic epithelium; Bone-related lesions), and other tumours [5].
Ameloblastoma arising from odontogenic epithelium without odontogenic ectomesenchyme, is the most common tumour of odontogenic origin [6]. Odontogenic fibromyxoma and cementoblastoma, arising from odontogenic ectomesenchyme with or without odontogenic epithelium, are uncommon tumours comprising 3–6% [7] and 1–6.2% [8] of all odontogenic tumours respectively. Cemento-ossifying fibroma, fibrous dysplasia, brown tumour of hyperparathyroidism and giant cell tumour are within the subgroup of bone-related lesions [5]. PNET is a tumour of neuroectodermal origin [5]. Ameloblastic carcinoma is grouped under malignant odontogenic tumour [5].
Odontogenic tumours occur over a wide range of ages with almost equal frequency in men and women [4]. Ameloblastoma occurs within mean age of 20 s and 30 s [9]. Odontogenic fibromyxoma occur in 2nd–4th decades with slight female predilection [7]. The peak incidence of cementoblastoma is between 2nd and 3rd decades of life with caucasian race and male predominance (M:F = 2.1:1) [10]. Greatest number of cases cemento-ossifying fibroma are encountered during 3rd and 4th decades of life with definite female predilection (M:F = 1:5) [11]. Fibrous dysplasia manifests more frequently in childhood [12]. The mean age of presentation of giant cell tumour is 8.2 years, more frequently affecting girls [13]. Brown tumour of hyperparathyroidism is more frequent in women aged over 50 years [14]. Most of the reported cases of PNET of jaw region are less than 20 years of age [15]. The mean age of occurrence of ameloblastic carcinoma is 30 years [16].
Most of the odontogenic tumours occur in the posterior aspect of mandible [17]. In the present series, 40% tumours (6 out of 15) were located at angle of mandible. Among five cases of ameloblastoma, two were at angle of mandible, two were at body of mandible and one at the ramus. Odontogenic fibromyxoma occurred in maxilla and ramus of mandible in one case each. One case each of cemento-ossifying fibroma, giant cell tumour and PNET were found in maxilla. Fibrous dysplasia occurred in maxilla and posterior ethmoid in one case each.
Many a times, odontogenic tumours are asymptomatic and are incidentally diagnosed by imaging studies [17]. The commonest presenting symptoms are swelling over jaw, dental malocclusion and mal-alignment. Larger and malignant tumours may present with pain, paresthesia or loosening of tooth. On clinical examination, the swelling is usually firm to hard and at times cystic due to perforation of cortex. Signs of nasal obstruction, epistaxis, hyposmia, headache, change in visual acuity, proptosis, impairment of eye movements and trismus are to be searched. Cervical lymphadenopathies are to be looked for while suspecting malignant tumour [17].
The radiological investigations i.e. OPG, CT scan and MRI are adjunct to the armory. For a localized lesion, OPG is good enough to evaluate the extension. For extensive lesion, CT is the choice of investigation for study of the lesions, analysis of their extension and surgical preparation. Moreover, MRI and CT predict whether the tumour is resectable or not, detect distant metastasis and assess the tumour response to treatment. Some of the odontogenic tumours has a characteristic but not diagnostic radiological appearance. Ameloblastoma usually appears as unilocular or multilocular radiolucent area with a honeycomb appearance [9]. Ameloblastic carcinoma mostly presents as ill-defined or irregular margin and osteolytic radiolucency [16]. Odontogenic fibromyxoma may present as bone destroying lesion with ill-defined borders [18]. Cementoblastoma appears as well-defined circular radio-opacity with a radiolucent halo, fused to partly resorbed root(s) of the associated tooth [19]. Cemento-ossifying fibromas are well circumscribed, solitary radiolucencies with scattered radiopaque foci [20]. There are three radiographic patterns of fibrous dysplasia: pategoid, that alternates the radio-dense and radio-transparent areas and give characteristic “ground glass” appearance; sclerotic, homogeneously dense; cystic standard, with spherical or ovoid radiolucent area surrounded by dense limits [21]. GCT has classical osteolytic and multi-loculated appearance [13]. Brown tumour of hyperparathyroidism appears as mono-locular or multi-locular osteolytic lesion with root resorption and loss of lamina dura occasionally [22]. On CT, PNETs usually appear iso-dense or slightly hypo-dense compared to normal muscle and tumour calcifications are uncommon. On MRI, the majority of PNETs are iso-intense or slightly hyper-intense on T1WI and hyper-intense on T2WI. Furthermore, the tumour is often heterogeneously marked following intravenous administration of gadolinium [23].
FNAC can offer the clinician a conservative alternative to the more invasive procedures such as open biopsy. Thinning or destruction of cortical bone permits the use of thin needles for aspiration [24]. Free flowing fresh blood on aspiration alerts the pathologist and precludes biopsy in view of risk of severe hemorrhage. But, the role of FNAC for diagnosis of intra-osseous jaw pathology is limited. FNAC of intra-osseous jaw lesions is often problematic because of their proximity to tooth apices and neurovascular bundles [24]. Obtaining cellular aspirates may be quite difficult in heavily calcified and fibro-osseous lesions, such as cement-ossifying fibroma and fibrous dysplasia. FNAC can broadly diagnose odontogenic tumors, fibro-osseous lesions, giant cell lesions and cystic lesions; however, definitive categorization may not be always possible due to lack of specific cyto-morphological features [24]. Ultrasonography-guided percutaneous core needle biopsy is less invasive compared to open surgical biopsy [25]. It allows precise needle position and avoids vascular damage. Incisional biopsy has been considered as the main diagnostic modality for preoperative presumptive diagnosis of intra-osseous jaw tumours due to difficulty in accessing and lack of well-established cytological features [24].
Irrespective of the histological type, surgical resection is the treatment of choice. In case of benign tumours, there are two options: conservative surgery and radical surgery [26]. Conservative approach includes enucleation or curettage. In the radical surgery, the tumour is resected with 1–2 cm of macroscopically healthy bony margin. But the recurrence rate is much higher in cases of conservative surgery (up to 90%) than radical surgery (up to 25%). In case of malignant tumours, if the tumour is resectable a more radical approach is employed. Lymph node dissection should be considered when there is obvious lymphadenopathy. If margins are close or histopathologically positive then post-operative adjuvant radiotherapy should be given. In case of PNET, surgery along with adjuvant multi agent chemotherapy is used. In locally advanced tumours not amendable to surgical resection or with distant metastasis, radiotherapy and/or chemotherapy is used.
Overall prognosis is good in cases of benign odontogenic tumours. All are prone to recurrence even with proper management. So long term follow up is essential. Distant metastasis may occur in ameloblastic carcinoma or PNET, even in the absence of recurrence at primary site.
Conclusion
Odontogenic tumours occur over a wide range of ages with almost equal frequency in men and women. Most of them occur in posterior aspect of mandible. Incisional biopsy has been considered as a prime diagnostic modality for preoperative diagnosis but FNAC can offer clinicians a less invasive alternative. CT is the investigation of choice for study of lesion, analysis of its extension and surgical planning. Irrespective of the histological type, surgical resection is the treatment of choice. The challenge to proper management lies in balancing between conservative and radical approach to reduce morbidity and recurrence both. Final diagnosis is made by post-operative histopathological examination. Overall prognosis is good in cases of benign odontogenic tumours.
Compliance with Ethical Standards
Conflict of interest
None.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Philipsen H, Reichart PA. Revision of the 1992-edition of the WHO histological typing of odontogenic tumors. A suggestion. J Oral Pathol. 2002;31:253–258. doi: 10.1034/j.1600-0714.2002.310501.x. [DOI] [PubMed] [Google Scholar]
- 2.Mosqueda-Taylor A. New findings and controversies in odontogenic tumors. Med Oral Patol Oral Cir Bucal. 2008;13:E555–E558. [PubMed] [Google Scholar]
- 3.(2014) Odontogenic and non-odontogenic tumors of the jaws. In: MA Pogrel, KErik Kahnberg, L Andersson (eds) Essentials of oral and maxillofacial surgery. Wiley-Blackwell, Hoboken
- 4.Varkhede A, Tupkari JV, Mandale MS, Sardar M. Odontogenic tumors: a review of 60 cases. J Clin Exp Dent. 2010;2(4):e183–e186. doi: 10.4317/jced.2.e183. [DOI] [Google Scholar]
- 5.Barnes L, Eveson JW, Reichart P, Sidransky D (eds) (2005) World health organization classification of tumours, pathology and genetics of head and neck tumours. IARC Press, Lyon, p 284
- 6.Sciubba JJ, Fantasia JA, Kahn LB, (eds) (1999) Benign odontogenic tumors. In: Atlas of tumor pathology—tumors and cysts of the jaw. AFIP, Washington. p 71–85
- 7.Brannon RB. Central odontogenic fibroma, myxoma (odontogenic myxoma, fibromyxoma), and central odontogenic granular cell tumor. Oral Maxillofac Surg Clin North Am. 2004;16:359–374. doi: 10.1016/j.coms.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Sumer M, Gunduz K, Sumer AP, Gunhan O. Benign cementoblastoma: a case report. Med Oral Patol Oral Cir Bucal. 2006;11:E483–E485. [PubMed] [Google Scholar]
- 9.Iordanidis S, Makos C, Dimitrakopoulos J, Kariki H. Ameloblastoma of the maxilla—case report. Aust Dent J. 1999;44(1):51–55. doi: 10.1111/j.1834-7819.1999.tb00536.x. [DOI] [PubMed] [Google Scholar]
- 10.Lemberg K, Hagström J, Rihtniemi J, Soikkonen K. Benign cementoblastoma in a primary lower molar, a rarity. Dentomaxillofac Radiol. 2007;36:364–366. doi: 10.1259/dmfr/58249657. [DOI] [PubMed] [Google Scholar]
- 11.Kuta AJ, Worley CM, Kaugars GE. Central cementoossifying fibroma of the maxillary sinus: a reviewof six cases. AJNR. 1995;16:1282–1286. [PMC free article] [PubMed] [Google Scholar]
- 12.Alves AL, Canavarros F, Vilela DS, Granato L, Próspero JD. Displasia fibrosa: relato de três casos. Rev Bras Otorrinolaringol. 2002;68(2):288–292. doi: 10.1590/S0034-72992002000200022. [DOI] [Google Scholar]
- 13.Weber AL, et al. Giant cell tumors of the sphenoid bone in four children: radiological, clinical, and pathological findings. Skull Base Surg. 1997;4:163. doi: 10.1055/s-2008-1058592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitzgerald P. Endocrinology. In: Tierney LM, McPhee SJ, Papadakis MA, editors. Current medical diagnosis & treatment. 39. Stamford: Appleton & Lange; 2000. pp. 1118–1121. [Google Scholar]
- 15.Windfuhr JP. Primitive neuroectodermal tumor of the head and neck: incidence, diagnosis, and management. Ann Otol Rhinol Laryngol. 2004;113:533–543. doi: 10.1177/000348940411300705. [DOI] [PubMed] [Google Scholar]
- 16.Naik V, Kale AD. Ameloblastic carcinoma: a case report. Quintessence Int. 2007;38:873–879. [PubMed] [Google Scholar]
- 17.Azizi T (2013) Diagnosis and management of common oral and maxillofacial lesions. In: Motamedi MHK (ed) A textbook of advanced oral and maxillofacial surgery, vol. 1, ch 5. In Tech Publisher. ISBN 978-953-51-1146-7
- 18.Zhang J, Wang H, He X, Niu Y, Li X. Radiographic examination of 41 cases of odontogenic myxomas on the basis of conventional radiographs. Dentomaxillofac Radiol. 2007;36(3):160–167. doi: 10.1259/dmfr/38484807. [DOI] [PubMed] [Google Scholar]
- 19.Matteson SR. Benign tumors of the jaws. In: White SC, Pharoah MJ, editors. Oral radiology: principles and interpretation. 4. Toronto: Mosby; 2000. pp. 401–402. [Google Scholar]
- 20.Sanchis JM, Peñarrocha M, Balaguer JM, Camacho F. Fibroma cemento-osificante mandibular: presentación de dos casos y revision de la literatura. Med Oral. 2004;9:69–73. [PubMed] [Google Scholar]
- 21.Oliveira RB, Granato L, Korn GP, Marcon MA, Cunha AP. Displasia fibrosa do osso temporal: relato de doiscasos. Rev Bras Otorrinolaringol. 2004;70(5):695–700. doi: 10.1590/S0034-72992004000500019. [DOI] [Google Scholar]
- 22.Alhusban M, Baqain ZH. Mandibular brown tumor as the first manifestation of primary hyperparathyroidism: a case report. Saudi Dent J. 2011;23(2):107–109. doi: 10.1016/j.sdentj.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang WD, Chen YF, Li CX, Zhang L, Xu ZB, Zhang FJ. Computed tomography and magnetic resonance imaging findings of peripheral primitive neuroectodermal tumors of the head and neck. Eur J Radiol. 2011;80:607–611. doi: 10.1016/j.ejrad.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 24.Goyal S, Sharma S, Kotru M, Gupta N. Role of FNAC in the diagnosis of intraosseous jaw lesions. Med Oral Patol Oral Cir Bucal. 2015;20(3):e284–e291. doi: 10.4317/medoral.20274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yeh CH, Yeow KM, Chu SY, et al. Imaging findings in mandibular primitive neuroectodermal tumour: a report of a rare case and review of the literature. Dentomaxillofac Radiol. 2011;40:451–456. doi: 10.1259/dmfr/92169329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akay MC, Zeytinoğlu M, Şimşek B, Aras I (2015) Multidisciplinary management of benign jaw tumors in children. In: Motamedi MHK (ed) A textbook of advanced oral and maxillofacial surgery. vol. 2, Ch14. InTech


