Abstract
Tonsillectomy is one of the most common surgical procedures performed worldwide. Several techniques have been developed to reduce morbidity and enhance recovery after tonsillectomy. Our study was designed to compare post-operative pain with three different techniques: cold dissection (CD), monopolar–bipolar dissection (MBD) and coblation dissection (CBD). 103 adults were scheduled for elective tonsillectomy from September 2014 to December 2015, and were randomized to CD, MBD and CBD. Post-operative pain was assessed using visual analogue scale (VAS) and Lattinen Test (LT). We did not find significant differences between the groups in the VAS pain scores (p > 0.05), except for the first day, when CBD tonsillectomy showed a higher pain score (p < 0.05). The differences in LT scores between the three techniques were not statistically significant (p > 0.05). Comparison of analgesic consumption between CD, MBD and CBD did not found any significant differences irrespective of the technique used. When first and second week after surgery were compared, differences in analgesics requirements were statistically significant (p < 0.05). Seventeen cases (16.5%) of secondary haemorrhage were reported, but there were no statistical differences in the rate of postoperative bleeding between the three groups (p > 0.05). We conclude that in our study comparison of the three techniques, CD, MBD and CBD, did not show significant differences in the post-tonsillectomy pain scores and bleeding rate.
Keywords: Tonsillectomy, Adult, Pain, Hemorrhage, Technique
Introduction
Tonsillectomy is one of the most commonly performed otolaryngologic operations worldwide. The history of the tonsillectomy dates back to about 100 years, during which various techniques and instruments have evolved to accomplish this operation [1, 2]. Tosillectomy has been described in the literature in 1000 BC in India and then by Celsus and Paul of Aegine in 625 with detailed description of operation with scapel [3]. Although tonsillectomy historically rank as one of the most common surgical procedures performed, these numbers had declined with the advent of antibiotics. When performed with the proper indications, tonsillectomy have been shown to improve the patients quality of life [4]. Indications for tonsillectomy includes recurrent pharyngotonsillitis, chronic tonsillitis, peritonsillar abscess, haemorrhagic tonsillitis, suspicion of malignant diseases, and tonsillar hypertrophy causing obstructive sleep- disorder [5, 6].
Several techniques have been described in the literature to reduce morbidity and enhance recovery after tonsillectomy. The different techniques include cold dissection, cryosurgery, guillotine, monopolar and bipolar diathermy dissection, laser tonsillectomy, ultrasonic removal, bipolar scissors dissection, microdebrider and thermal welding [3, 7]. However, none of them has been accepted universally as the best technique.
Discussion usually focuses on postoperative pain and haemorrhage when comparing different tonsillectomy techniques. Unlike most operative procedures, which are closed primarily, tonsillectomy produces an open wound that heals by secondary intention, so the main problems in this procedure are pain and secondary haemorrhage. The pain is the result of the disruption of mucosa and glossopharyngeal and vagal nerve fiber irritation followed by inflammation and spasm of the pharyngeal muscles that leads to ischemia and a protracted cycle of pain [8]. Cold dissections with knife, scissor or snare have been the traditional instruments for tonsillectomies. During the recent decades, the use of electrosurgery has increased, although it has been associated with increased postoperative pain and risk of haemorrhage, and on the other hand, with less intraoperative blood loss and shorter operative time compared to cold dissection [9, 10]. Direct contact between the tissue and the electrodes generate local temperatures of 400–600 °C, resulting in postoperative pain, odynophagia and associated dehydration. Coblation is a technique which enables ablation of tonsils at much lower temperatures than bipolar diathermy. With this technique, dissociation of isotonic saline between the electrodes of the coblator into sodium ions breaks molecular bands between cells [11]. The temperature during this procedure is approximately 45–85 °C compared to 400–600 °C of electrocautery [6, 11, 12].
This study was designed to compare the postoperative pain of three common techniques to perform tonsillectomy: cold dissection (CD), monopolar–bipolar diathermy dissection (MBD), and coblation dissection (CBD).
Methods
103 adults referred to our hospital for tonsillectomy were recruited to this study. Indications for tonsillectomy in this study were: (1) Recurrent tonsillitis; (2) Tonsillar hypertrophy resulting in snoring but not sleep apnea. Patients with history of bleeding disorder or other major health problems were excluded. Only patients 16 years of age or older were enrolled in this study. Patients were randomized to tonsillectomy with CD, MBD and CBD from September 2014 to December 2015.
Surgical Technique
All procedures were performed under general anaesthesia through endotracheal intubation. The patients were placed in the Rose position and a Crow-Davis mouth gag was inserted into the mouth. The tonsil was taken and medialized with an Allis clamp. CD was performed using scissors to enter the superior peritonsillar space, and blunt dissection was used to remove the tonsil from superior to inferior pole. After tamponade of tonsillar fossa hemostasis was performed by packing or suturing bleeding points with absorbable suture. In MBD group, and incision was made with monopolar cautery at the anterior and superior part of the anterior pillar. Dissection was performed at the peritonsillar cleavage plane with monopolar diathermy, and bleeding points were coagulated with bipolar cautery. Finally, coblation tonsillectomy was made using bipolar radiofrequency through a saline medium by dissecting between the tonsillar capsule and the surrounding pharyngeal muscles. Irrigation and suction was employed at all times, and coagulation of vessels was done with the same instrument.
Most patients were discharged the day after the surgical procedure. As pain medication, we prescribed use dexketoprofen 25 mg three times a day and 2–3 tablets of paracetamol + codeine. The patients could also take metamizol 1 ampoule drunk as rescue therapy if more pain. The amount of the analgesic taken was assessed in each patient.
Postoperative pain was assessed at 1, 3, 7 and 14 postoperative days. The pain was evaluated using visual analogue scale (VAS) on a scale of 0–10, with 0 representing no pain at all and 10 worst possible pain. Postoperative pain was consider mild if EVA ranges between 0.00 and 2.99; moderate when ranges between 3.00 and 6.99, and severe pain when it was greater than 7.00. Lattinen Test (LT), a questionnaire to estimate pain that is employed between Spanish- speaking specialists of pain, was also used to evaluate postoperative pain. This test contains five subscales with a score from 0 to 4 concerning the following items: (1) Pain intensity; (2) Pain frequency; (3) Analgesic consumption; (4) Degree of disability; (5) Sleep hours. Each of the items is added to obtain a total score from 0 to 20. The patients were given a questionnaire for evaluation of postoperative pain including VAS and LT scores.
All episodes of postoperative bleeding were documented and also the interventions required to stop it.
Data Analysis
The three groups were compared for their demographic data, postoperative pain assessed by VAS and LT, and complications. The differences of categorical variables were tested by Fisher´s exact test or chi- square test. For continuous variables, a non-parametric Kruskal–Wallis was used to determine differences of three groups. The results were interpreted within a confidence interval of 95% and a significance level of 0.05.
Results
Demographic Data
There were 103 patients, 44 males (42.7%) and 59 females (57.3%) between 16 and 50 years, with a mean- age of 26.1 ± 7.2 years. Thirty- five patients (16 male, 19 female) with a mean- age of 24.1 ± 6.4 years, ranged between 17 and 49 years, had undergone CD. Forty-one patients (16 male, 25 female) underwent MBD, whose age ranged between 16 and 50 years, with a mean- age of 28.5 ± 7.5 years. In the CBD group, there were 27 patients (12 male, 15 female), with a mean- age of 18.7 ± 7.5 years, ranged between 16 and 43 years.
Postoperative Pain
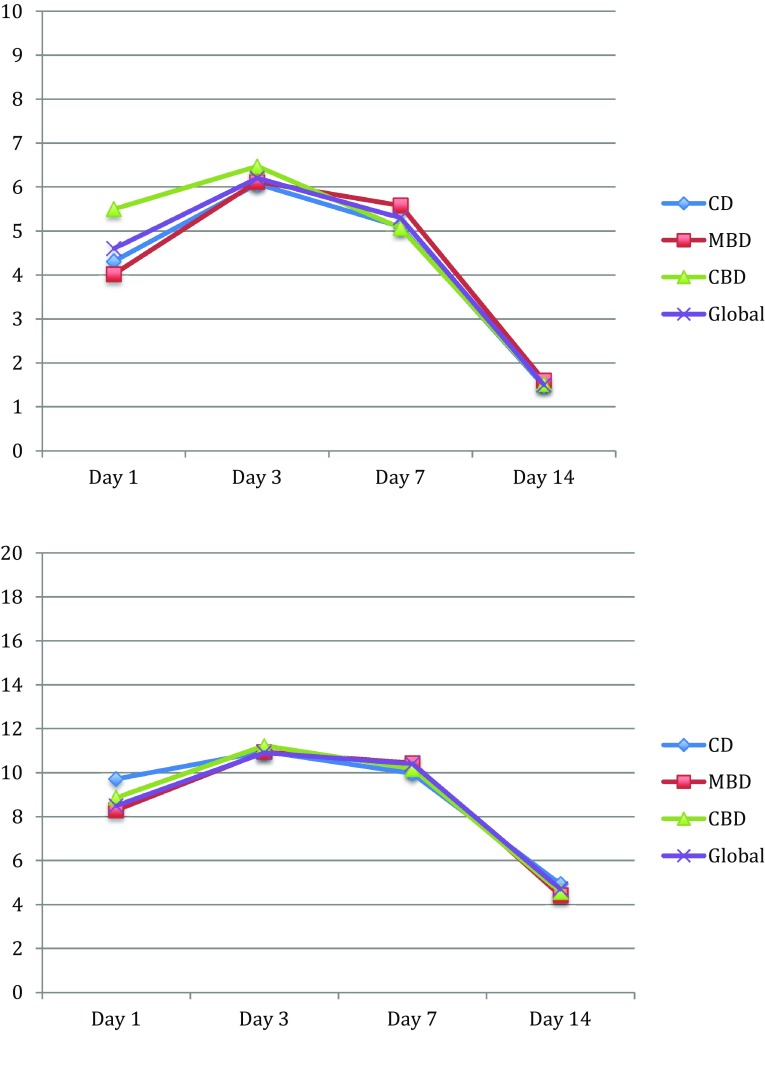
Pain was observed by VAS and LT. The mean postoperative pain score of EVA at first day was 4.6 ± 2 (range 0.5–10); at third day was 6.2 ± 1.8 (range 1.3–10); pain score at seventh day was 5.3 ± 2.8 (range 0.5–10); at fourteenth day was 1.5 ± 0.3 (range 0–5.2). The difference of pain score between days 1, 3, 7, 14 was statistically significance (p < 0.05). Mean postoperative LT score at first day was 8.5 ± 2.3 (range 2–15); mean LT score at third day was 10.9 ± 0.5 (range 4–17); at seventh day 10.4 ± 3.7 (range 2–18); finally, at fourteenth day was 4.7 ± 1 (range 0–14). The difference of mean LT score between days 1, 3, 7, 14 was statistically significance (p < 0.05).
Table 1 shows the median pain scores of EVA for the three groups during the 14- day follow-up. This table shows a significant difference at the assessment points at first day. After that, there was not significance difference between the groups in the pain scores. Table 2 shows the median LT scores for the three groups during the 14- day follow-up. No significance difference was found in LT median scores between the three techniques at days 1, 3, 7, and 14.
Table 1.
Comparison of pain scores by VAS at days 1, 3, 7, 14 between cold dissection, monopolar–bipolar dissection and coblator dissection
| EVA | Cold dissection (n = 35) | Monopolar–bipolar dissection (n = 41) | Coblator dissection (n = 27) | p value | |||
|---|---|---|---|---|---|---|---|
| χ (range) | SD | χ (range) | SD | χ (range) | SD | ||
| Day 1 | 4.31 (0.8–8.2) | 2.13 | 4.02 (0.5–7.6) | 1.99 | 5.5 (2.4–10) | 2.08 | 0.014 |
| Day 3 | 6.07 (2–9.4) | 2.33 | 6.12 (2–9.6) | 2.34 | 6.47 (4–9.2) | 2 | 0.758 |
| Day 7 | 5.1 (0.6–10) | 2.72 | 5.58 (0.5–9.3) | 2.39 | 5.07 (1.9–10) | 2.16 | 0.608 |
| Day 14 | 1.48 (0.2–2.5) | 1.34 | 1.6 (0–5.2) | 1.32 | 1.52 (0.1–3.8) | 1.18 | 0.919 |
Χ, mean; SD, standard deviation
Table 2.
Comparison of Lattinen test scores at successive evaluations at days 1,3,7 and 14 comparing the three techniques
| Lattinen Test | Cold dissection (n = 35) | Monopolar–bipolar dissection (n = 41) | Coblator dissection (n = 27) | p value | |||
|---|---|---|---|---|---|---|---|
| χ (range) | SD | χ (range) | SD | χ (range) | SD | ||
| Day 1 | 9.71 (3–15) | 2.79 | 8.29 (2–15) | 3.19 | 8.87 (5–12) | 2.88 | 0.122 |
| Day 3 | 10.96 (4–17) | 2.35 | 10.94 (7–16) | 3.2 | 11.22 (4–16) | 2.79 | 0.912 |
| Day 7 | 9.97 (4–17) | 3.62 | 10.43 (6–17) | 3.36 | 10.18 (4–18) | 3.04 | 0.838 |
| Day 14 | 4.93 (1–12) | 2.93 | 4.41 (0–11) | 2.9 | 4.57 (1–14) | 3.25 | 0.749 |
Χ, mean; SD, standard desviation
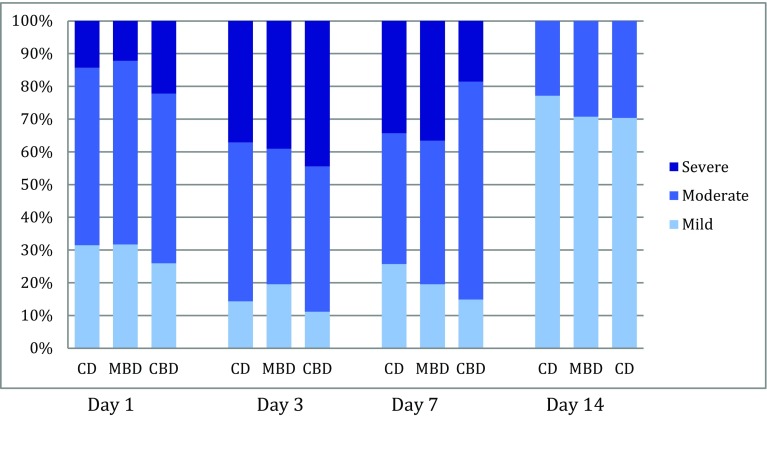
At first day, 30.1% of the patients had mild postoperative pain (EVA ranged between 0.00 and 2.99); in 54.4% pain was moderate (EVA ranged between 3.00 and 6.99); the postoperative pain was severe (EVA greater than 7.00) in 14.5% of the patients. At third day, postoperative pain was mild in 15.5%, moderate in 44.6% and severe in 39.9%. At seventh day, postoperative EVA scores were mild in 28.4%, moderate in 48.5% and severe in 23.1%. Finally, at fourteenth day was mild, moderate and severe in 72.8, 27.2 and 0%, respectively. Figure 1 shows the percentage of patients with mild, moderate or severe pain, according to different techniques, in the 14 days follow up.
Fig. 1.
Percentage of patients with mild (EVA 0.00–2.99), moderate (EVA 3.00–6.99) or severe pain (>7.00), according to different techniques, in the 14 days follow up
Consumption of Analgesics
Globally, mean consumption of analgesics during first week was 14.8 ± 1.8 tablets of dexketoprofen 25 mg; 14.7 ± 3.7 tablets of paracetamol + codeine, and 3.9 ± 1.8 drinked metamizol ampules. At second week, 12.2 tablets of dexketoprofen average were consumed; 10.8 tablets of paracetamol + codeine and 2.8 drink ampoules of metamizol. Table 3 shows mean consumption of analgesics during first and second week according to the different techniques.
Table 3.
Mean consumption of analgesics during first and second week according to the different techniques: cold dissection (CD), monopolar–bipolar dissection (MBD) and coblator dissection (CBD)
| Analgesics | CD (n = 35) | MBD (n = 41) | CBD (n = 27) | p value | |
|---|---|---|---|---|---|
| First week | Dexketoprofen | 14.6 ± 1.8 | 14.6 ± 5 | 15.8 ± 3.3 | 0.361 |
| Paracetamol + codeine | 14.6 ± 3.7 | 14.7 ± 4.4 | 14.8 ± 2.9 | 0.979 | |
| Metamizol ampoles | 4.3 ± 1.8 | 4.2 ± 2.3 | 3.5 ± 3.3 | 0.397 | |
| Second week | Dexketoprofen | 11.7 ± 6.2 | 13.8 ± 6.3 | 11.7 ± 6.3 | 0.255 |
| Paracetamol + codeine | 12.6 ± 6.5 | 11.1 ± 4.2 | 13.8 ± 6.2 | 0.147 | |
| Metamizol ampoles | 3.4 ± 3.7 | 2.8 ± 1.9 | 2.7 ± 4.3 | 0.516 |
Haemorrhage and Post-operative Complications
No cases of primary haemorrhage were seen in any group. Seventeen cases (16.5%) of secondary haemorrhage were reported: 4 cases in the CD group (11.4%); 8 patients of MBD group (19.5%); and 5 patients of CBD group (18.5%). There was no statistically difference in the rate of postoperative bleeding between the three groups (p = 0.6). Eleven of these patients were male and six female, so postoperative bleeding was more common among men (25%) than among women (10.1%), with significant differences (p = 0.04).
Five patients were reviewed in operating room for hemostasis (4.8%): four of the latter were male. These patients who needed surgical review were one from CD group, one from MBD group, and three from CBD. In addition, two patients went to the emergency room because of pain, and had to be hospitalized for intravenous analgesic therapy.
Discussion
Tosillectomy is one of the most frequently performed otorhinolaryngological procedures, accounting for about 20% of all operations [2, 3, 7]. The morbidity of this operation may be significant, so surgeons must consider haemorrhage, apnea, pain, fever and poor oral intake as possible effects of the surgery. Ideal tonsillectomy should be quick, painless and associated with no blood loss. However, to date none of the commonly used techniques has been shown to be superior. From the patient´s perspective, the main concern after tonsillectomy is the post-operative pain, so in order to investigate the optimum method for adults, the present study was conducted to evaluate postoperative pain with three different techniques: cold dissection, monopolar–bipolar diathermy dissection, and coblation dissection.
Adult tonsillectomy is often associated with a considerable amount of post-operative pain. Traditional surgical techniques using the scalpel, guillotine, or snare have largely been replaced with techniques utilizing cautery to limit intraoperative blood loss. However, it has been reported that early post-operative pain may be more intense after the mechanical trauma of cold dissection technique, whereas hot methods may have a higher incidence of late post-operative pain [13]. In a systematic review of Leinbach et al. [14] electrodissection caused increased post-operative pain in comparison with cold dissection tonsillectomy. Cardozo et al. [15] also found a significant relationship between bipolar diathermy energy and post- operative pain in adult tonsillectomy. Coblation is a relatively new technique that consists in a radiofrequency bipolar electrical current through a medium of normal saline, resulting in a plasma field of highly ionized particles, which in turn break down intercellular bonds and thus melt tissue at around 70 °C (lower than electrocautery which cut tissues at 400 °C) [8]. Several studies have shown that coblation tonsillectomy caused significantly less pain when compared with conventional techniques [11, 16], and also offers significant advantages such as more rapid return to normal diet and reduction in analgesic requirements [17]. Despite this, in our study we have not found higher pain scores for MBD when compared with CD and CBD. The only significant difference was found at the first day, when curiously coblation tonsillectomy showed a higher pain score. Both EVA and Lattinen Test did not show significant differences between the three techniques. Naturally, the significant differences were found when compared the post-operative pain scores in the different days after surgery. These differences of pain scores between days 1, 3, 7, 14, were statistically significance (p < 0.05), with a higher pain in days 3 and 7 after surgery, regardless of the technique used (see Fig. 2). Tonsillectomy is a surgery that causes a mild or moderate pain in most cases, although few patients complain of severe pain. We found that during first day after surgery, 85.5% of the patients had mild or moderate pain, and only 14.5% a severe pain. By contrast, during third and seventh post-operative days this pain was higher, and we found that in 60.1 and 76.9% of patients the pain was mild or moderate, respectively at days 3 and 7 after surgery, and 39.9 and 23.1% had a severe pain score (see Fig. 1). Adults usually require approximately 14 days of convalescence after tonsillectomy before they are able to return to full dietary habits and work. After that time pain is usually much lower, as we saw in our patients, that at fourteenth post-operative day, most of them had no pain or was mild (72.8%) and none of them had severe pain.
Fig. 2.
Pain scores versus post-operative day after cold dissection (CD), monopolar–bipolar diathermy dissection (MBD) and coblation dissection (CBD), using: a visual analogue scale (VAS); b Lattinen test
Analgesic consumption is rarely cited in studies on post-tonsillectomy pain. We did a measurement of average consumption of analgesics during the first and second week, and made a comparison between CD, MBD and CBD, but we did not found any significant differences irrespective of the technique used. Naturally, differences in analgesic consumption comparing the first and second week were greater. These differences in paracetamol + codeine tablets, dexketoprofen tablets and metamizol drunk ampoules requirements were significant (p < 0.05) when first and second week after surgery were compared.
Bleeding remains the most significant complication following tonsillectomy, sometimes requiring revision surgery under general anaesthesia. The post-operative secondary haemorrhage rate in this study was 16.5%, higher to the general reported incidence of post-tonsillectomy bleeding, which ranges from 0 to 7% [14, 18, 19]. Although this is the incidence generally reported in the papers, it seems to be referred to bleeding rates in children tonsillectomy, and it is accepted that adult tonsillectomy had a more frequent bleeding. Tolska et al. [20] reported in a study of 842 adult tonsillectomies a post-operative haemorrhage rate of 14.5%, similar to our study, questioning whether post- tonsillectomy bleeding was more common than previously described. Controversy still persists in the world literature regarding the occurrence of significantly increased bleeding rates after hot tonsillectomy methods. Some studies have compared post-operative haemorrhage among electrocautery or coblation tonsillectomy patients versus cold dissection patients, and found significant increase in the first [18, 21–23]. However, other studies reported no significant differences [14], and concern was expressed that the number of well designed, large, randomised, controlled trials was insufficient to detect small differences in secondary haemorrhage rates [13]. Among our patients, post-operative bleeding seemed to be lower in the CD group (11.4%) compared to those techniques which includes coagulation methods (MBD, 19.5%; CBD, 18.5%), although no statistical difference in haemorrhage rates were found between the three groups (p > 0.05). By contrast, we found interesting differences between male and female in the post-tonsillectomy bleeding rate (male, 25%; female 10.1%), with significant differences (p < 0.05). Similar to our study, some authors have established male gender as a risk factor of post-tonsillectomy haemorrhage [20, 24]. Also among the patients who had to undergo review surgery for hemostasis, male gender represented 80% of them.
Finally, we must emphasize that this study has some limitations. Despite being a prospective study that has avoided using patients as their own control (some studies use the contralateral tonsil as comparative control), the sample size is insufficient to obtain statistically significant differences, and also, the surgeries were performed by more than one surgeon, and ideally only one would be involved.
Conclusions
When we compare CD, MBD and CBD we did not find significant differences in post-operative pain scores. Also, no reliable conclusions regarding post-operative haemorrhage rate can be drawn based on this study because of low number of patients. Thus, larger randomized studies would be required to know what technique of tonsillectomy causes less post-operative pain and bleeding.
Compliance with Ethical Standards
Conflict of interest
None.
Human and Animal Rights
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Itziar Álvarez Palacios, Email: Itziar.alvarez.palacios@gmail.com.
Ricardo González-Orús Álvarez-Morujo, Email: ricardomorujo@hotmail.com.
Cristina Alonso Martínez, Email: krisalonsomar@gmail.com.
Alejandra Ayala Mejías, Email: sandri_ayala@hotmail.com.
Oscar Arenas Brítez, Email: osands@gmail.com.
References
- 1.Jeffrey A. On the origin of tonsillectomy and the dissection method. Laryngoscope. 2002;112:1583–1586. doi: 10.1097/00005537-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Silveira H, Soares JS, Lima HA. Tonsillectomy: cold dissection versus bipolar electrodissection. Int J Pediatr Otorhinolaryngol. 2003;67:345–351. doi: 10.1016/S0165-5876(02)00399-3. [DOI] [PubMed] [Google Scholar]
- 3.Ozkiris M, Kapusuz Z, Saydam L. Comparison of three techniques in adult tonsillectomy. Eur Arch Otorhinolaryngol. 2013;270(3):1443–1447. doi: 10.1007/s00405-012-2160-y. [DOI] [PubMed] [Google Scholar]
- 4.Wilson YL, Merer DM, Moscatello AL. Comparison of three common tonsillectomy techniques: a prospective randomized, double- blinded, clinical study. Laryngoscope. 2009;119(1):162–170. doi: 10.1002/lary.20024. [DOI] [PubMed] [Google Scholar]
- 5.Darrow HD, Siemens C. Indications for tonsillectomy and adenoidectomy. Laryngoscope. 2002;112:6–10. doi: 10.1002/lary.5541121404. [DOI] [PubMed] [Google Scholar]
- 6.Hasan H, Raitiola H, Chrapek W, Pukenader J. Randomized study comparing postoperative pain between coblation and bipolar scissor tonsillectomy. Eur Arch Otorhinolaryngol. 2008;265(7):817–820. doi: 10.1007/s00405-007-0537-0. [DOI] [PubMed] [Google Scholar]
- 7.Dutta N, Bordoloi BM. Indian J Otolaryngol Head Neck Surg. 2002;54:74–76. doi: 10.1007/BF02911016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rakesh S, Anand TS, Payal C, Pranjal K. A prospetive, randomized, double- blind study of coblation versus dissection tonsillectomy in adult patients. Indian J Otolaryngol Head Neck Surg. 2012;64(3):290–294. doi: 10.1007/s12070-011-0355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wexler DB. Recovery after tonsillectomy: electrodissection vs sharp dissection techniques. Otolaryngol Head Neck Surg. 1996;114:576–581. doi: 10.1016/S0194-5998(96)70249-8. [DOI] [PubMed] [Google Scholar]
- 10.Maddern B. Electrosurgery for tonsillectomy. Laryngoscope. 2002;112:11–13. doi: 10.1002/lary.5541121405. [DOI] [PubMed] [Google Scholar]
- 11.Timms MS, Temple RH. Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol. 2002;116:450–452. doi: 10.1258/0022215021911031. [DOI] [PubMed] [Google Scholar]
- 12.Belloso A, Chidambaran A, Morar P, Timms MS. Coblation tonsillectomy versus dissection tonsillectomy: postoperative haemmorhage. Laryngoscope. 2003;113:2010–2013. doi: 10.1097/00005537-200311000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Ragab SM. Six years of evidence- based adult dissection tonsillectomy with ultrasonic scapel, bipolar electrocautery, bipolar radiofrequency or “cold steel” dissection. J Laryngol Otol. 2012;126(10):1056–1062. doi: 10.1017/S0022215112002022. [DOI] [PubMed] [Google Scholar]
- 14.Leinbach RF, Markwell SJ, Colliver JA, Lin SY. Hot versus cold tonsillectomy: a systematic review of the literature. Otolaryngol Head Neck Surg. 2003;129:360–364. doi: 10.1016/S0194-5998(03)00729-0. [DOI] [PubMed] [Google Scholar]
- 15.Cardozo AA, Hallikeri C, Lawrence H, Sankar V, Hargreaves S. Teenage and adult tonsillectomy: dose–response relationship between diathermy energy used and morbidity. Clin Otolaryngol. 2007;32:366–371. doi: 10.1111/j.1749-4486.2007.01529.x. [DOI] [PubMed] [Google Scholar]
- 16.Polites N, Joniau S, Wabnitz D, Fassina R, Smythe C, Varley P, Carney AS. Postoperative pain following coblation tonsillectomy: randomized clinical trial. ANZ J Surg. 2006;76:226–229. doi: 10.1111/j.1445-2197.2006.03700.x. [DOI] [PubMed] [Google Scholar]
- 17.Temple RH, Timms MS. Paediatric cobaltion tonsillectomy. Int J Pediatr Otorhinolaryngol. 2001;61:195–198. doi: 10.1016/S0165-5876(01)00553-5. [DOI] [PubMed] [Google Scholar]
- 18.Lowe D, van der Meulen J. Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet. 2004;364:697–702. doi: 10.1016/S0140-6736(04)16896-7. [DOI] [PubMed] [Google Scholar]
- 19.Hopkins C, Geyer M, Topham J. Post- tonsillectomy haemorrhage: a 7-year retrospective study. Eur Arch Otorhinolaryngol. 2003;260:454–455. doi: 10.1007/s00405-003-0609-8. [DOI] [PubMed] [Google Scholar]
- 20.Tolska HL, Takala A, Pitkaniemi J, Jero J. Post-tonsillectomy haemorrhage more common than previously described- an institutional chart review. Acta Otolaryngol. 2013;133:181–186. doi: 10.3109/00016489.2012.723825. [DOI] [PubMed] [Google Scholar]
- 21.Betancourt AR, Lopez Z, Zerpa V, Carrasco M, Dalmau J. Does surgical technique influence post-tonsillectomy haemorrhage? Our experience. Acta Otorrinolaringol Esp. 2015;66:218–223. doi: 10.1016/j.otorri.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Windfuhr JP, Wienke A, Chen YS. Electrosurgery as a risk factor for secondary hemorrhage. Eur Arch Otorhinolaryngol. 2009;266:110–116. doi: 10.1007/s00405-008-0720-y. [DOI] [PubMed] [Google Scholar]
- 23.Praveen AC, Parthiban S, Terry RM. High incidence of post- tonsillectomy secondary haemorrhage following coblation tonsillectomy. Indian J Otolaryngol Head Neck Surg. 2013;65:24–28. doi: 10.1007/s12070-012-0584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mueller J, Boeger D, Buentzel J, Esser D, Hoffman K, Jecker P, Mueller A, et al. Population- based analysis of tonsil surgery and postoperative hemorrhage. Eur Arch Otorhinolaryngol. 2015;272(12):3769–3777. doi: 10.1007/s00405-014-3431-6. [DOI] [PubMed] [Google Scholar]