Abstract
Larynx is the second most common site for cancer in the upper aerodigestive tract. One of the dreaded complications following total laryngectomy has been pharyngo cutaneous fistula (PCF). PCF merits special attention due to its significant negative impact on the recovery process. Total laryngectomy profoundly alters speech. Effective voice restoration is essential for the rehabilitation of these patients. Inadequate consensus exists as to the best technique of pharyngeal repair to decrease incidence of PCF and ensure good quality voice following total laryngectomy. 21 patients were included in the study for total laryngectomy with trachea oesophageal voice prosthesis placement. Patients were randomised into 2 groups. Group A had their pharynx repaired in two layers and Group B had it done in three layers. Post operatively the patients were followed up for a period of 12 months to look for incidence of PCF. Subjective and objective evaluation of voice was done. 9.52% of patients developed PCF. All of the cases of PCF were in the group repaired in three layers. In cases with repair by two layers the mean Voice Handicap Index 10 (VHI 10) score was 19.27 and those with three layers pharyngeal repair was 23.20. Average maximum phonation time amongst the study population was 13.09. In three layers and two layers pharyngeal repair the average maximum phonation time was 12.56 and 13.58 respectively. Surgical repair of pharynx in two layers excluding the third layer of pharyngeal musculature reduces the chance of PCF. Two layers pharyngeal repair supplemented by cricopharyngeal myotomy led to significantly better voice outcome.
Keywords: Laryngeal neoplasms, Laryngectomy, Neoplasm staging, Pharyngectomy, Suture techniques, Speech
Introduction
The larynx is the second most common site for cancer in the upper aerodigestive tract, of which squamous cell carcinoma is the predominant type (95%). There are about 1,36,000 new cases diagnosed worldwide per year, with an estimated overall 5-year survival rate of 68%, making it one of the more curable cancers of the upper aerodigestive tract [1]. In the recent years, the opportunity to preserve the functions of vocalization, swallowing, and natural airway respiration by organ preserving approaches led to a decrease in the number of total laryngectomy operations performed for laryngeal cancer. However, for advanced stage tumours or recurrent disease, despite its significant morbidity and high complication rates, a total laryngectomy operation is usually employed. One of the dreaded complications following total laryngectomy has been pharyngo cutaneous fistula (PCF). PCF merits special attention due to its significant negative impact on the recovery process of the patient and relatively high incidence rates ranging from 8.7 to 22% [2]. The PCF was found to be associated with increased hospital stay, delayed adjuvant postoperative therapy, nutritional deterioration of the patient, and severe life threatening complications. So far, in the literature, many factors were proposed to be significantly associated with the development of the PCF. Advanced primary tumour stage, preoperative radiotherapy, duration of surgery, transfusion requirement, patient co-morbidities, prior tracheotomy, low perioperative albumin and haemoglobin, hypothyroidism, presence of tumour beyond resection margin were implicated in the development of the PCF. In addition to the above causes, technique of Neopharynx closure deserves special mention [3]. Total laryngectomy profoundly alters speech, respiration, and sense of smell and taste. It is the loss of voice that is most responsible for the psychosocial and economic consequences following laryngectomy. Effective voice restoration is essential to the rehabilitation of these patients. There are three methods of alaryngeal speech: electrolarynx, oesophageal speech, and tracheoesophageal (TE) speech. Since the description of tracheoesophageal voice restoration technique of Blom and Singer in 1979, many studies have demonstrated the efficacies, safety and reproducibility of this form of postlaryngectomy voice rehabilitation [4]. There has been significant modification of the prosthesis itself and the means of placing the prosthesis. Although the tracheaoesophageal puncture (TEP) technique has been originally described as a secondary procedure in which stenting catheter was endoscopically placed well after laryngectomy, soon the primary TEP in which the tract for speech fistula was made primarily during laryngectomy was described [5]. Hypopharyngeal closure technique, significantly alter the quality of Tracheo-oesophageal voice post operatively. Techniques such as, oesophageal neurectomy, closure of pharynx in two layers versus three layers has been debated. Inadequate consensus exists as to the best technique, or techniques, to optimize wound healing, decrease pharyngocutaneous fistula formation, and ensuring good quality voice following Total Laryngectomy with partial pharyngectomy and repair of neopharynx with placement of trachea-oesophageal puncture using Provox prosthesis. Accordingly, the purpose of this study was to assess the possible impact of closure technique of neopharynx on the incidence and severity of fistula formation and voice outcome in laryngectomes.
Aim of Study
The study was aimed to compare the post operative incidence of PCF and quality of voice outcome in laryngectomes having their neopharynx repaired in two layers versus three layers.
Materials and Methods
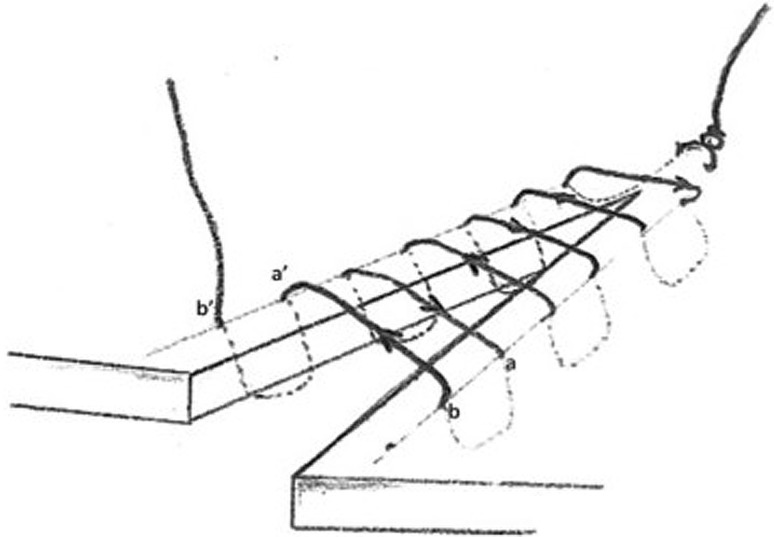
A randomised control trial was conducted in Department of ENT and Head Neck surgery, in a tertiary care hospital of Kolkata during April 2012 to January 2016. All patients diagnosed with carcinoma larynx having clinically negative neck node undergoing total laryngectomy with partial pharyngectomy and hemithyroidectomy were included in the study. Patients requiring neck dissection, undergoing preoperative radiotherapy and/or chemotherapy and poor lung reserve were excluded from the study. Diagnosis of carcinoma larynx was done by direct laryngoscopy and histopathological confirmation from the biopsy specimen. Standard radiological investigations were done. Proper disease staging was done using American Joint Committee on Cancer staging manual 2010 [6]. Pre operatively systemic comorbidities were taken into consideration and managed medically. Pulmonary function test (PFT) was done in all the cases. A rigorous pre-anaesthetic check up preceded the operation. Following total laryngectomy, partial pharyngectomy and ipsilateral hemi thyroidectomy the pharynx was repaired to create a neo pharynx. A naso-gastric tube was placed before repair of pharynx. The patients were randomised by block randomisation method and categorised into two groups. Single layer blinding was ensured. In the first group (Group A) the pharynx was repaired in two layers—extra mucosal and serosal. In the second group (Group B) pharynx was repaired in three layers—extra mucosal, serosal and muscular. The extra mucosal layer was repaired in continuous Connell stitch with 3-0 absorbable polyglactin suture material on a round body needle (Figs. 1, 2). The other layers were repaired in interrupted fashion with similar suture material. Cricopharyngeal myotomy was done, and tracheo-esophageal voice prosthesis ProvoxTM was inserted in all the cases. Wound suction drain was applied. Circumferential neck dressing was done. The drains were taken out on postoperative 3rd–5th day, when the drainage is less than 15–20 mL per drain. The circumferential neck dressing was applied for additional 2 days to prevent de-attaching of skin flaps from underlying tissue. All cases were fed via nasogastric tube during postoperative 11 days. Oral feeding was started on 12th postoperative day firstly with plain water to control any possible fistula. PCF was diagnosed when the drainage of saliva was noted under the skin flaps from postoperative 11 days or a reflux was detected around the stoma or suture line after the first oral intake of liquid. The patients were followed up for 12 months for any evidence of PCF. Speech therapist was consulted from third post operative week. Voice assessment began from one week of starting speech therapy and it was followed up at 4 and 12 weeks. All patients underwent voice assessment in similar condition in sound proof room. They were asked to perform following tasks: Each subject was asked to sustain a vowel at conversational loudness level and at a comfortable pitch on a single breath for as long as possible (3 successive trials). Maximum phonation time (MPT) out of 3 trials at the 12th weeks was recorded. The patients were asked to fill in a Voice Handicap Index 10 (VHI 10) [7] at the end of 12 weeks post speech therapy initiation. All patients received radiotherapy post operatively.
Fig. 1.
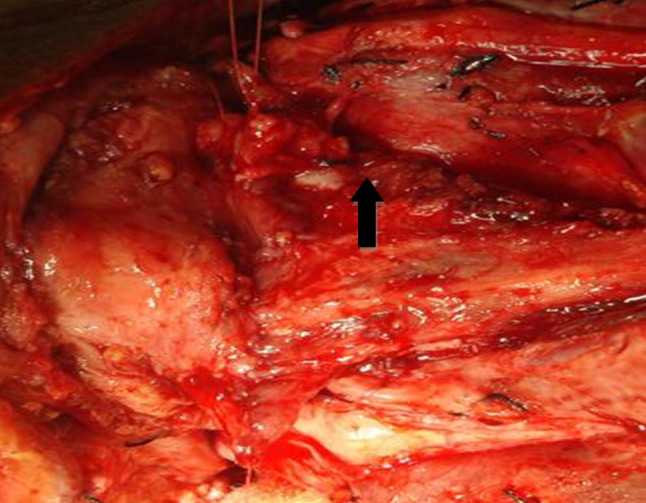
Per operative photograph showing continuous Connell stitch (black arrow)
Fig. 2.
Schematic diagram showing Connell stitch [16]
Result Analysis
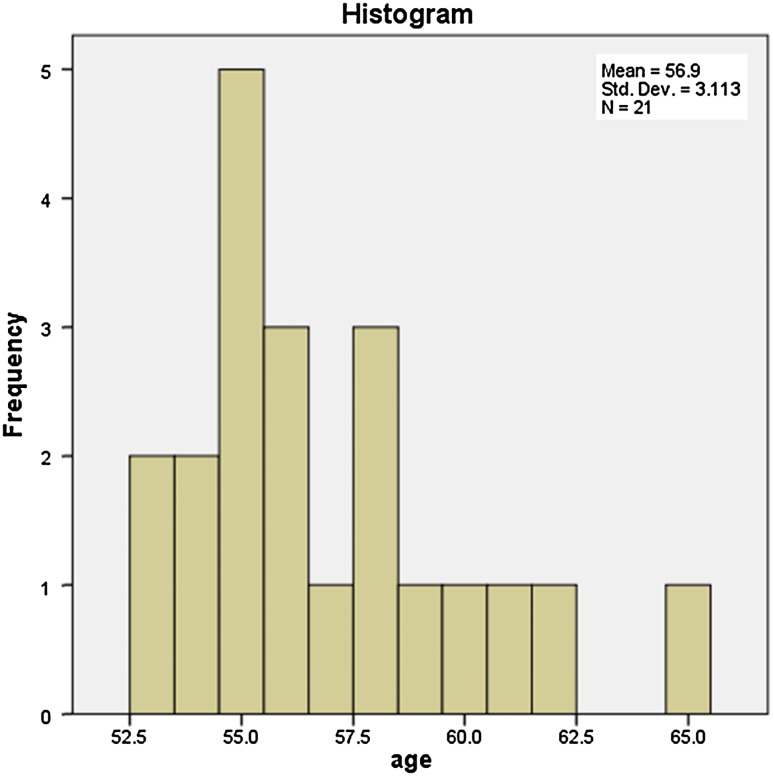
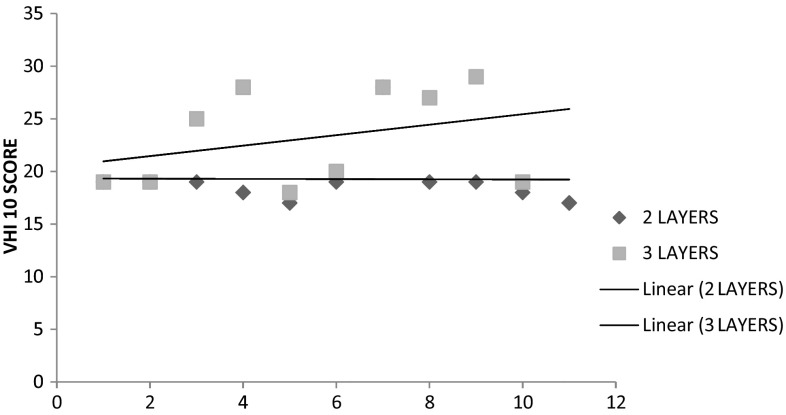
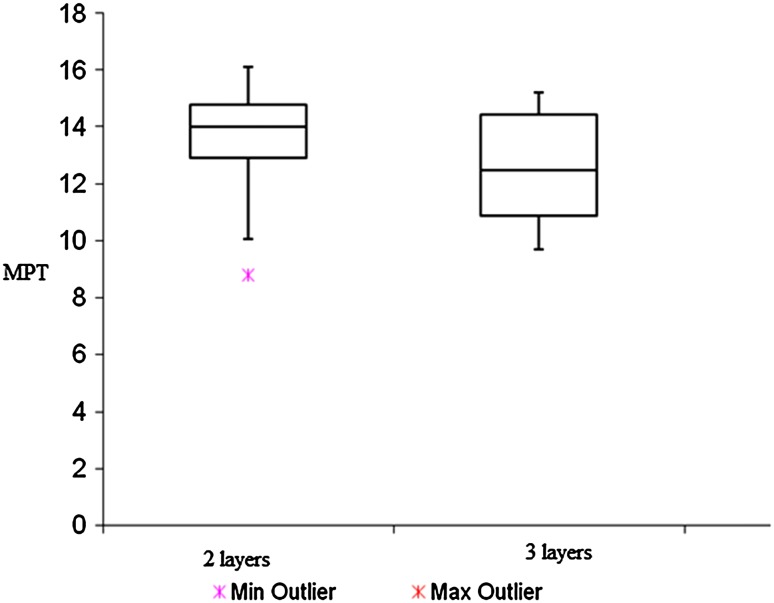
Average age of the patients treated with laryngectomy and provoxTM insertion was 56.9 years. Maximum and minimum age of the patient was 65 and 56 years respectively. There were 20 male and 1 female (Fig. 3). Out of the total, 12 had supraglottic growth and 9 had transglottic growth. The laryngeal carcinoma was staged and found to have Stage 3 in 14 cases and Stage 4 in 7. 10 patients had their larynx repaired in three layers and 11 in two layers. Width of the pharyngeal remnant was measured with standard scale at the most constricted part in the relaxed state. The minimum width was found to be 1.8 cm. Remnant pharyngeal mucosa could be closed without the need of distant flaps (Fig. 4). 9.52% of patients developed PCF. These patients presented with fistula between 1 and 12 months duration. The mean duration of closure of fistula was 2 weeks. The fistula developed in the lateral part of the suture line. According to fistula classification by Horgan and Dedo [8] the fistulas were of Minor category. Fistula resolved with conservative management like compression bandage, regular dressing and naso gastric feeding; and didn’t recur in the follow up period. All of the cases of PCF were in the group repaired in three layers. The post operative voice outcome was analysed both subjectively and objectively by VHI 10 score and MPT respectively. Mean VHI 10 score was 21.14. In cases with repair by two layers the mean VHI 10 score was 19.27 and those with three layers pharyngeal repair was 23.20. A scattered diagram (Fig. 5) was plotted correlating VHI 10 score in the 2 above mentioned groups. Average maximum phonation time amongst the study population was 13.09. In three layers and two layers pharyngeal repair the average maximum phonation time was 12.56 and 13.58 respectively. A box plot diagram (Fig. 6) was constructed comparing the maximum phonation time in the two layers and three layers pharyngeal repair groups. Pearson correlation coefficient of VHI 10 score and MPT was—0.86. Unpaired T test was performed to determine statistical significance of the difference in VHI 10 score amongst the two study groups. P value was 0.035 (p < 0.05, statistically significant). In case of supraglottic laryngeal carcinoma post operative mean MPT was 13.258, VHI 10 score of 20.75. In case of transglottic laryngeal carcinoma post operative mean MPT was 12.87 and VHI 10 score was 21.66.
Fig. 3.
Histogram showing the demographic distribution of the population
Fig. 4.
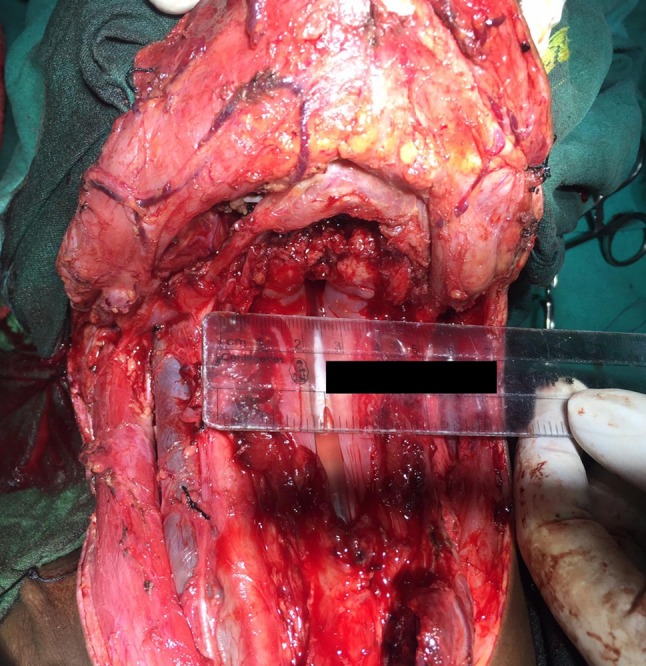
Measurement of width of remnant pharyngeal mucosa
Fig. 5.
A scatter diagram correlating VHI 10 Score among Group A (two layers pharyngeal repair) and Group B (three layers pharyngeal repair)
Fig. 6.
A box plot graph displaying the 10th, 25th, 50th, 75th and 90th percentiles of the objective variable MPT in patients treated with pharyngeal repair in two layers and three layers respectively
Discussion
Organ preservation techniques in treatment of laryngeal cancer has revolutionised the disease treatment protocol. Laryngectomy as a salvage technique is still popular [9]. One of the dreaded complications of laryngectomy is development of PCF. Various factors dictating wound healing are responsible for formation of PCF [10, 11]. In our study population of 21 laryngectomes, the incidence of fistula was 9.52%. The fistulas presented between 1 and 12 months duration. The fistulas were managed conservatively and all of those healed. All the cases of fistula formation were in the group where neopharynx was repaired in three layers. The study population had co-morbid conditions like diabetes, hypertension. But there was no statistical correlation between the co-morbidities and PCF. Probably tight control of systemic diseases and good surgical technique explains the condition. Neopharynx created even with the minimum amount the pharyngeal mucosa (1.8 cm) had no evidence of PCF. According to Hui et al. [12] narrowest widths of the pharyngeal remnant of 1.5 cm relaxed is sufficient both for primary closure of the pharynx and in restoring swallowing function. Wang et al. [13] demonstrated the surgical technique of pharyngeal closure sparing the pharyngeal musculature reduced the chance of PCF. Our study is in coherence to the same. In gastrointestinal system surgery, continuous suturing techniques (Connell and Cushing suture) are widely used for ileal, jejunal, and other colonic anastomoses either for cancer resection or traumatic perforations and successful results were presented in the literature [14]. In our study population we have used Connell suture technique for extramucosal pharyngeal closure with adequate success. Various studies have shows the added benefit of vascularized tissue at the time of pharyngeal closure to reduce fistula and promote early return to oral diet [15].Voice outcome following total laryngectomy has always been an enigma. Various alaryngeal communication techniques have evolved over time. Tracheo Esophageal Prosthesis (TEP) has been one of them. In this study population primary provox insertion was done in all the patients. Statistically significant improvement in voice outcome in terms of VHI 10 was found in the group with two layers repair of pharynx as compared to three layers. p value of 0.035 (<0.05). Objective analysis of voice outcome in terms of average MPT demonstrated a value of 13.58 s in the two layer repair group and 12.56 s in three layers pharyngeal repair group. Studies have proposed non closure of the pharyngeal constrictor muscle is preferable to muscular closure because it reduces the spasm of the pharyngoesophageal segment which limits voice rehabilitation [13]. Supraglottic laryngeal carcinoma had a average VHI 10 score of 13.25 and MPT of 20.75, as compared to average VHI 10—12.87 and average MPT—21.66 in Transglottic carcinoma undergoing laryngectomy. Better post surgical voice outcome in Supraglottic growth as compared to transglottic growth can be proposed from the study.
Conclusion
Considering the fact that the systemic co-morbid factors were adequately controlled, none undergoing neck dissection and all patients manifesting PCF before induction of radiotherapy proves the hypothesis that closure in two layers has significant impact. Closure in three layers increases the intra-luminal pressure of the neopharynx, thus causing PCF. Two layers pharyngeal repair supplemented by cricopharyngeal myotomy led to significantly better voice outcome as perceived by the subject. MPT was also found to be higher in the groups undergoing pharyngeal repair in two layers. Probably the non closure of the pharyngeal musculature reduced the intra luminal pressure of the neo pharynx and reduced pharyngo esophageal spasm. Thus leading to an improved voice outcome and decreased rate of PCF.
Compliance with Ethical Standards
Conflict of interest
The authors of this article declare that he/she has no conflict of interest.
Human and Animal Rights
Animals were not involved in this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Cattaruzza M, Maisonneuve P, Boyle P. Epidemiology of laryngeal cancer. Eur J Cancer B Oral Oncol. 1996;32(5):293–305. doi: 10.1016/0964-1955(96)00002-4. [DOI] [PubMed] [Google Scholar]
- 2.Markou K, Vlachtsis K, Nikolaou A, Petridis D, Kouloulas A, Daniilidis I. Incidence and predisposing factors of pharyngocutaneous fistula formation after total laryngectomy. Is there a relationship with tumor recurrence? Eur Arch Otorhinolaryngol. 2004;261(2):61–67. doi: 10.1007/s00405-003-0643-6. [DOI] [PubMed] [Google Scholar]
- 3.Paydarfar J, Birkmeyer N. Complications in head and neck surgery. Arch Otolaryngol Head Neck Surg. 2006;132(1):67. doi: 10.1001/archotol.132.1.67. [DOI] [PubMed] [Google Scholar]
- 4.Elmiyeh B, Dwivedi RC, Jallali N, Chisholm EJ, Kazi R, Clarke PM, Rhys-Evans PH. Surgical voice restoration after total laryngectomy: an overview. Indian J Cancer. 2010;47:239–247. doi: 10.4103/0019-509X.64707. [DOI] [PubMed] [Google Scholar]
- 5.Singer M, Blom E. An endoscopic technique for restoration of voice after laryngectomy. Ann Otol Rhinol Laryngol. 1980;89(6):529–533. doi: 10.1177/000348948008900608. [DOI] [PubMed] [Google Scholar]
- 6.Edge S, Compton C. The American Joint Committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 7.Rosen C, Lee A, Osborne J, Zullo T, Murry T. Development and validation of the Voice Handicap Index-10. Laryngoscope. 2004;114(9):1549–1556. doi: 10.1097/00005537-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Horgan EC, Dedo HH. Prevention of major and minor fistulae after laryngectomy. Laryngoscope. 1979;89:250–260. doi: 10.1288/00005537-197902000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Weber RS, Berkey BA, Forastiere A, Cooper J, Maor M, Goepfert H, Morrison W, Glisson B, Trotti A, Ridge JA, Chao KS, Peters G, Lee DJ, Leaf A, Ensley J. Outcome of salvage total laryngectomy following organ preservation therapy: the Radiation Therapy Oncology Group trial 91-11. Arch Otolaryngol Head Neck Surg. 2003;129(1):44–49. doi: 10.1001/archotol.129.1.44. [DOI] [PubMed] [Google Scholar]
- 10.Johansen LV, Overgaard J, Elbrond O. Pharyngo-cutaneous fistulae after laryngectomy. Influence of previous radiotherapy and prophylactic metronidazole. Cancer. 1988;61(4):673–678. doi: 10.1002/1097-0142(19880215)61:4<673::AID-CNCR2820610410>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 11.Patel UA, Keni SP. Pectoralis myofascial flap during salvage laryngectomy prevents pharyngocutaneous fistula. Otolaryngol Head Neck Surg. 2009;141(2):190–195. doi: 10.1016/j.otohns.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 12.Hui Y, Wei WI, Yuen PW, Lam LK, Ho WK. Primary closure of pharyngeal remnant after total laryngectomy and partial pharyngectomy: How much residual mucosa is sufficient? Laryngoscope. 1996;106(4):490–494. doi: 10.1097/00005537-199604000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Wang Ching-Ping, Tseng Tzu-Chan, Lee Rheun-Chuan, Chang Shyue-Yih. The techniques of nonmuscular closure of hypopharyngeal defect following total laryngectomy: the assessment of complication and pharyngoesophageal segment. J Laryngol Otol. 1997;111:1060–1063. doi: 10.1017/S0022215100139337. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Ke N, Tan C, et al. Continuous versus interrupted suture techniques of pancreaticojejunostomy after pancreaticoduodenectomy. J Surg Res. 2015;193(2):590–597. doi: 10.1016/j.jss.2014.07.066. [DOI] [PubMed] [Google Scholar]
- 15.Dirven R, Swinson BD, Gao K, Clark JR. The assessment of pharyngocutaneous fistula rate in patients treated primarily with definitive radiotherapy followed by salvage surgery of the larynx and hypopharynx. Laryngoscope. 2009;119(9):1691–1695. doi: 10.1002/lary.20521. [DOI] [PubMed] [Google Scholar]
- 16.Haksever M, Akduman D, Aslan S, Solmaz F, Ozmen S. Modified continuous mucosal connell suture for the pharyngeal closure after total laryngectomy: zipper suture. Clin Exp Otorhinolaryngol. 2015;8(3):281. doi: 10.3342/ceo.2015.8.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]