Abstract
Background: Mind–body therapies are often used by people with autism spectrum disorders (ASD). However, there has been little examination into which types of mind–body therapies have been investigated for people with ASD and for what purposes. A systematic review was conducted to evaluate the existing evidence for mind–body therapies for people with ASD, particularly to determine the types of mind–body therapies used and the outcomes that are targeted.
Methods: PubMed, PsychInfo, and Scopus were searched using terms for ASD and mind–body therapies. Sixteen studies were selected for review; these studies tested interventions using mindfulness, meditation, yoga, Nei Yang Gong, and acceptance commitment therapy. Most study outcomes targeted behavior, psychological symptoms, and quality of life for children and adults with ASD as well as their parents.
Results: There was little overlap between studies on the types of mind–body therapies used and associated outcomes, and only three of the studies were randomized controlled trials. Most studies were small and uncontrolled. Some studies modified the mind–body therapies to increase accessibility for people with ASD.
Conclusion: The evidence for mind–body therapies for people with ASD is limited and would benefit from larger randomized controlled trials.
Keywords: : autism, Asperger syndrome, mind-body, yoga, mindfulness
Introduction
Mind–body therapies or techniques are used by up to 30% of people with an autism spectrum disorder (ASD).1 Mind–body therapies encompass a wide range of practices that focus on a connection between the mind, body, and health. Why individuals with ASD may use mind–body therapies, however, is unknown. That is, are mind–body therapies being used to treat core ASD characteristics? Are they used to address co-occurring conditions? It is also not known how successful such therapies are for people with ASD. In one parent survey, up to 80% of those who had used mind–body therapies for their children with ASD reported the therapies to be “moderately” or “very” helpful, but it was not specified in what way these therapies were helpful.2
Characteristics of ASD include differences in social communication and interaction.3 ASD is heterogeneous. People with ASD may also experience difficulties understanding metaphorical or non-literal language, slower information processing, and intellectual disability, which could influence the cognitive aspects of a mind–body intervention. Differences in these characteristics may influence the success of various mind–body therapies for different individuals within the ASD population. However, many people with ASD experience co-occurring conditions such as depression, anxiety, and high stress levels, for which mind–body therapies may be most beneficial.
In other populations, mind–body therapies have been shown in meta-analyses to improve symptoms of anxiety, depression, stress, and sleep problems.4–6 These conditions can have significant negative impacts on quality of life and independence for people with ASD. Determining if mind–body therapies are beneficial for people with ASD could provide a therapy option that could improve these symptoms. It is also worthwhile to determine if mind–body protocols should be adapted to increase accessibility for those with ASD.
This review evaluated mind–body studies that include individuals with ASD. Specifically, this review examined the types of mind–body practices, outcomes, and accessibility adaptations that have been explored for people with ASD.
Materials and Methods
Based on a preliminary search, it was anticipated that there would be few high-quality studies conducted on mind–body therapies and ASD. As such, the search strategy of this review was systematic, but the inclusion criteria were kept broad to capture best the overall state of the current research on this topic.
Eligibility
Studies were eligible if they included individuals with ASD. This included autistic disorder, Asperger syndrome, and pervasive developmental disorder not otherwise specified. In cases of samples with mixed populations, studies were eligible if they included individuals with ASD and specified the number of people within the overall sample with ASD. There were no criteria for determining ASD diagnosis. ASD participants of any age were included.
All included interventions utilized some form of mind–body therapy. Definitions for mind–body therapies vary widely. For this study, mind–body therapies had to include an attentional or mindfulness component. Mind–body therapies that were eligible for inclusion a priori included mindfulness-based interventions, meditation, yoga, t'ai chi, and acceptance and commitment therapy. Other therapies identified in the search were considered on a case-by-case basis. For instance, Nei Yang Gong was included due to its similarity to t'ai chi with an emphasis on mindful movement and breathing exercises. Multiple designs were included, such as quasi-experimental, randomized controlled trials (RCTs), and feasibility studies.
Interventions based on neurofeedback, applied kinesiology, massage, aromatherapy, and acupuncture were not included because these therapies do not necessarily include focused attentional or mindful components. For example, a t'ai chi intervention usually involves effortful awareness to breath and special attention to movement, while massage is a passive experience for the participant. Single retrospective case reports were excluded.
There were no criteria on what outcomes were included, as long as the outcomes addressed individuals with ASD.
Information sources and search strategy
Pubmed, Scopus, and PsychInfo were searched in December 2015. The following search terms were used: autism OR autism spectrum disorder OR pervasive developmental disorder OR Asperger; combined with: mind–body OR mindfulness OR meditation OR yoga OR acceptance commitment therapy OR t'ai chi OR qigong. The entry of search terms was adapted according to the database's search interface. Searches were limited to studies published after 1980 due to the introduction of autistic disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM) that year. Searches were also limited to articles available in English.
Selection and management
The first author performed the initial title and abstract search for articles that potentially included mind–body therapies and participants with ASD. The second author replicated this search separately with the same results. Full-text articles were independently screened by the two authors. Articles with therapies that were not initially included in our mind–body definitions were discussed by the reviewers for whether they should be classified as mind–body. If there were disagreements, a third reviewer would have been consulted, but this did not occur. Outcomes variables were extracted from the articles by one reviewer and verified by the other. All primary outcomes that included individuals with ASD were extracted. Any recorded modifications to intervention protocols to increase the accessibility for individuals with ASD were noted. Data were managed in Microsoft Excel.
Results
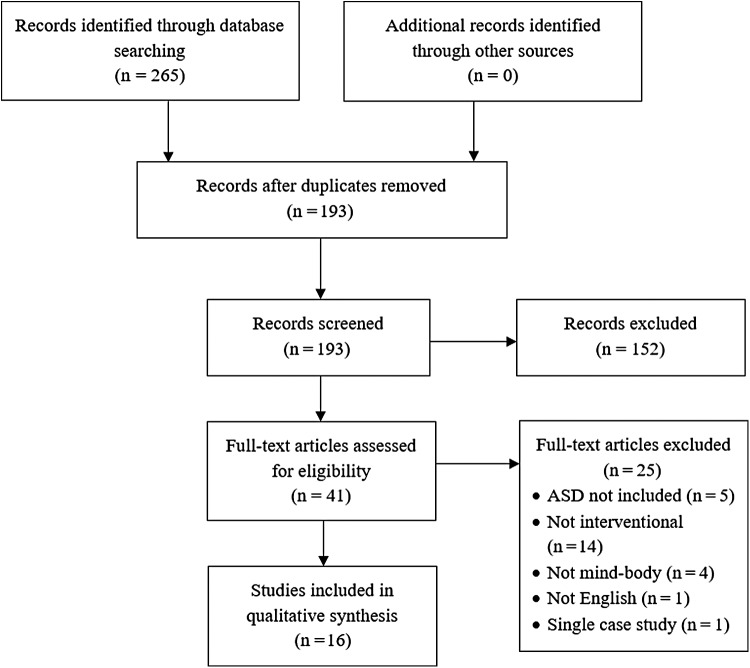
The initial search yielded 193 results once duplicate articles were removed. After title and abstract review, 41 articles were selected for full-text review. Five studies were excluded because people with ASD were not included in the outcomes or the inclusion of people with ASD was unclear. Fifteen articles were excluded because they were not interventional or experimental in design (e.g., review, book chapters, case reports). Four studies did not include mind–body interventions (i.e., neurofeedback, cognitive–behavioral therapy, emotion recognition, and a neuromuscular technique). One study was excluded because it was not in English. Sixteen studies were selected for final inclusion and discussion (see Fig. 1).
FIG. 1.
Flowchart of study selection.
Of the included studies, three were RCTs, four were quasi-experimental, and nine were cohort or multiple-baseline studies. The types of mind–body practices included were yoga, Nei Yang Gong (also known as Dejian), mindfulness, meditation, mindfulness-based cognitive therapy, mindfulness-based stress reduction, mindfulness-based therapy, mindfulness-based positive behavior support, MyMind mindfulness training, mindfulness-based soles of the feet meditation, mindful parenting, and acceptance and commitment therapy (see Table 1). Table 2 provides brief descriptions of the different types of interventions included in this review.
Table 1.
Studies by Intervention Type
| Mindfulness |
| Bogels et al. (2008) |
| De Bruin et al. (2015) |
| Hwang et al. (2015) |
| Kiep et al. (2015) |
| Neece (2013) |
| Singh et al. (2006) |
| Singh, Lancioni GE, Singh et al. (2011) |
| Singh, Lancioni, Manikam, et al. (2011) |
| Singh et al. (2014) |
| Spek et al. (2013) |
| Yoga |
| Koenig et al. (2012) |
| Radhakrishna (2010) |
| Radhakrishna et al. (2010) |
| Rosenblatt et al. (2011) |
| Nei Yang Gong/Dejian |
| Chan et al. (2013) |
| Acceptance Commitment Therapy |
| Pahnke et al. (2014) |
Table 2.
Brief Descriptions of Mind–Body Interventions
| Intervention | Description |
|---|---|
| Mindfulness | Being aware of the present moment and present thoughts in a nonjudgmental way. Often taught by a trained instructor in sessions for several weeks in conjunction with home practice. |
| Mindful parenting | Parents learn meditation and mindfulness skills that they can exercise when interacting with children. |
| Yoga | A movement-based therapy that incorporates physical poses and attention to breath. Taught by a trained instructor. |
| Nei Yang Gong | A movement-based therapy that uses a sequence of slow movements, mental exercises, and breathing exercises. Similar to qigong or t'ai chi, it also incorporates the Chinese theory of qi. |
| Acceptance Commitment Therapy | A type of cognitive–behavioral therapy that includes mindfulness aspects. It emphasizes a nonjudgmental stance when monitoring thoughts. The commitment component is an active process on identifying life values and promoting behaviors that work toward them. |
Sample sizes ranged from 3 to 50 participants with ASD (M = 20, median = 6). Ages ranged from 2.5 to 65 years. One intervention was directed toward parents but also included outcomes from their children with ASD. The main outcomes of interest were diverse and included behavioral, social, and psychological symptoms, as well as the subjective well-being of children and adults with ASD and their parents. A summary of the interventions and outcomes can be found in Table 3.
Table 3.
Study Characteristics Arranged by Intervention Type and Author
| Study | Design | Intervention description | Age (years) | Dropout rate | Outcomes | Results |
|---|---|---|---|---|---|---|
| Bogels et al. (2008) | Quasi-experimental | Children (n = 14) taught mindfulness-based cognitive therapy, and parents taught mindful parenting in parallel for 8 weeks with 8-week follow-up Control: waitlist |
11–17 | 35.7% | Personal goals (GAS—parent- and self-report); behavior symptoms (CBCL, D2, YSR, CSBQ, SCRS); QOL (SHS, PedsQL); Mindful awareness (MAAS) | Child and parent GAS ratings improved (p < 0.001). Improvement on YSR (p = 0.001), D2 and SCRS (p < 0.05), happiness (p < 0.05), and mindful awareness (p < 0.05). No changes in CBCL, CSBQ, or QOL. |
| Chan et al. (2013) | RCT | Nei Yang Gong/Dejian (n = 23) for 4 weeks with 2-week follow-up Control: PMR (n = 23) |
6–17 | 13.0% | Self-control (TOL, CCTT, FPT); behavior (ATEC (parent rated); self-control, temper tantrum, and rigid thoughts/act questionnaires) | All self-control measures improved (p < 0.01). All ATEC subscales, except speech/language, improved (p < 0.05). Temper outburst improved (p = 0.026), but not obsessive behavior or verbal expression. |
| de Bruin et al. (2015) | Cohort | Mindfulness training (MYmind), parents (n = 29) and adolescents (n = 23) taught in parallel for 9 weeks with 9-week follow-up Control: none |
11–23 | 9.6% | Rumination (RRS), worry (PSQW), autism symptoms (AQ), QOL (WHO-5); mindfulness (MAAS-A); social responsiveness (SRS—parent rated) | Improvement on RRS (p < 0.05) and WHO-5 (p < 0.05). No changes on PSWQ, AQ, or MAAS-A. SRS score improved at follow-up (p < 0.001), but not immediately post intervention. |
| Hwang et al. (2015) | Cohort | Mindfulness training for 8 weeks. Mothers learned, then taught children (n = 6) at home for 3 weeks with 12 months of practice Control: none |
8–15 | 16.7% | Problem behaviors (CBCL) | Total problems on CBCL decreased after parent mindfulness training (p = 0.046). Child mindfulness training reduced anxiety (p = 0.039) and thought problem (p = 0.043) subscales. |
| Kiep et al. (2014) | Cohort | Mindfulness-based therapy (n = 50) for 9 weeks with 9-week follow-up Control: none |
20–65 | 16.0% | Psychological symptoms (SCL-90-R, RRQ, GMS) | Overall main effect of time (p = 0.027) and for all scales and subscales, except hostility |
| Koenig et al. (2012) | Quasi-experimental | Yoga in school classroom (n = 25) for 16 weeks Control: Usual classroom activity (n = 24) |
5–12 | 2.1% | Behavior (ABC-C—parent and teacher rated) | Decreased ABC-C score for teacher rated (p = 0.029) but not parent rated (p = 0.564) |
| Neece (2013) | RCT | Parents trained in mindfulness-based stress reduction for 8 weeks. Children (n = 19) observed for changes Control: waitlist (n = 16) |
2.5–5 | 0% | Child behavior problems (CBCL) | Improved attention deficit/hyperactivity subscale (p < 0.05), but no other changes |
| Pahnke et al. (2014) | Quasi-experimental (randomized by classroom) | ACT (n = 15)—school setting for 6 weeks with 2-month follow-up Control: waitlist (n = 13) |
13–21 | 0% | Stress (SSS—teacher reported and self-reported); behavior (SDQ—teacher reported and self-reported); psychological distress (BYI) | No differences in self- or teacher-reported SSS or SDQ, or BYI |
| Radhakrishna (2010) | Cohort | Yoga (n = 6) for 10 months Control: none |
8–14 | 0% | Imitation behavior rated on three-point scale (parent report) | Improved imitation behaviors by up to 1.7 points (statistics NR) |
| Radhakrishna et al. (2010) | Quasi-experimental | Yoga (n = 6) for 82 weeks Control: none |
8–14 | 0% | Child behavior (ARI-E-2 checklist, ITB, RSBTB—parent and teacher reports) | Improvements in receptive skills, imitation skills, and self-injurious behavior (statistics NR) |
| Rosenblatt et al. (2011) | Cohort | Combined yoga, dance, music therapy for 8 weeks (n = 33) Control: none |
3–18 | 27.2% | Child behavior (BASC-2, ABC) | Improvement on BASC-2 Behavioral Symptom Index subscale (p = 0.04) but not on other subscales. No change on ABC. |
| Singh et al. (2006) | Multiple baseline | Mindful parenting, mothers (n = 3) trained for 12 weeks with 52 weeks of practice and variable follow-up Control: none |
4–6 | 0% | Aggression, noncompliance, and self-injury behaviors (parent report) | Decreased frequency (statistics NR) |
| Singh, Lancioni, Singh, et al. (2011) | Multiple baseline | Meditation: children (n = 3) taught by mothers, 5 days of training, up to 24 weeks of practice with 4-year follow-up Control: none |
13–18 | 0% | Physical aggression (self-report and sibling/parent report) | Decreased frequency (statistics NR) |
| Singh Lancioni, Manikam, et al. (2011) | Multiple baseline | Meditation: children (n = 3) taught by mothers, 5 days of training, up to 30 weeks of practice, 3-year follow-up Control: none |
14–17 | 0% | Physical aggression (sibling/parent report) | Decreased frequency (statistics NR) |
| Singh et al. (2014) | Multiple baseline | Mindfulness-based positive behavior support: children (n = 3) taught by mothers, 8 weeks of training, up to 37 weeks of practice Control: none |
15–19 | 0% | Aggression, compliance, disruptive behavior (parent report) | Aggression and disruptive behaviors decreased frequency. Compliance increased frequency (statistics NR). |
| Spek et al. (2013) | RCT | Mindfulness-based therapy (n = 21) for 9 weeks Control: waitlist (n = 21) |
18–65 | 2.3% | Mood, rumination, affect (SCL-90-R, RRQ, GMS) | Improvement for depression (p = 0.02), anxiety (p = 0.02), positive affect (p = 0.02), and rumination (p < 0.001) |
ABC, Aberrant Behavior Checklist; ABC-C, Aberrant Behavior Checklist-Community; ACC, Anterior Cingulate Cortex; ACT, Acceptance Commitment Therapy; ARI-E-2 checklist, Autism Research Institute E-2 checklist; AQ, Autism Quotient; ATEC, Autism Treatment Evaluation Checklist; BASC-2, Behavioral Assessment System for Children; BYI, Beck Youth Inventories; CBCL, Child Behavior Checklist; CCTT, Children's Color Trails Test; CSBQ, Children's Social Behavior Questionnaire; D2, D2 Test of Attention; FPT, Five Point Test; GAS, Goal Attainment Scale; GMS, Dutch Global Mood Scale; ITB, imitation test battery; MAAS, Mindful Attention and Awareness Scale; MAAS-A, Mindful Attention and Awareness Scale-Adolescent; PedsQL, Pediatric Quality of Life Inventory; PMR, progressive muscle relaxation; PSWQ, Penn State Worry Questionnaire; QOL, quality of life; RCT, randomized controlled trial; RRQ, Rumination-Reflection Questionnaire; RRS, Ruminative Response Scale; RSBTB, repetitive stereotyped behavior test battery; SCL-90-R, Symptom Checklist-90-Revised; SCRS, Self-Control Rating Scale; SDQ, Strengths and Difficulties Questionnaires; SHS, Subjective Happiness Scale; SRS, Social Responsiveness Scale; SSS, Stress Survey Schedule; TOL, Tower of London Test; WHO-5, World Health Organization-Five Well-Being Index; YSR, Youth Self Report.
Four studies confirmed an ASD diagnosis by the Autism Diagnostic Interview—Revised or Autism Diagnostic Observation Schedule.7–10 Four studies confirmed an ASD diagnosis, but did not clearly specify how or by what measure.11–14 One study did not specify how the ASD diagnosis was confirmed, but participants were recruited from a school for children with ASD.15 Seven studies did not clearly report whether an ASD diagnosis was confirmed.16–22 Of those that reported the DSM criteria, one study used the DSM-IV criteria16 and five used the DSM-IV-TR.7–10,13 Four studies had some exclusion criteria based on IQ, intellectual disability, or cognitive condition.8–10,16 Two studies included some individuals with intellectual or cognitive disabilities.11,19 All other studies were unclear whether there were any exclusion criteria related to intellectual or cognitive disabilities, but two of these studies noted that all child participants were in regular education classes.20,22 Two studies included people with ASD as well as other developmental delays or conditions.11,18
Seven mindfulness-based studies involved the parents of children with ASD. In two of the studies, parents and children were taught mindfulness concurrently in separate sessions.7,11 In one study, only the mothers learned mindfulness to determine if that would improve problem behaviors in their children with ASD.18 One study used mindful parenting.19 Four studies taught parents the mindfulness protocols, so that they could deliver the intervention to their children.17,20–22
Only two studies reported on adverse events, and none were reported.10,16
Discussion
The goal of this review was to summarize the current literature on mind–body interventions for people with ASD. This review found only three RCTs and one group randomized trial on mind–body therapies. One of these studies was in adults with ASD, which found statistically significant positive effects from a mindfulness intervention for depression, anxiety, and rumination.9 The other randomized studies in children showed insignificant effects on stress and psychological distress in children receiving classroom-based acceptance commitment therapy compared to normal classroom activities16; significant positive effects on self-control and some measures of behavior from Nei Yang Gong therapy10; and significant positive effects on hyperactivity but no other behavior measures when a mindfulness program is delivered only to parents.18
Effects on mental and emotional health
Multiple studies showed improved mental health with different mind–body therapies in people with ASD.7–9,11,16 Moreover, a RCT of an autism-adapted mindfulness program showed moderate to large effect sizes for improving anxiety, depression, and rumination in adults with ASD.9 A follow-up study reported the longer-term effects of the autism-adapted mindfulness program and found that positive effects were maintained at 9 weeks after the intervention ended, although the follow-up study did not include a control group.8 These results are consistent with meta-analyses in other populations, which support the use of mindfulness-based therapies for depression and anxiety.4,5 Other mindfulness-based studies that were not randomized found pre–post improvements on happiness ratings and rumination.8,11 There were mixed reports on changes in quality of life for children and adolescents.7,11 Participants also reported improvements in managing thoughts. An anecdotal experience of this was illustrated by one investigator (p. 911):
One adolescent explained that his thoughts were like overcrowded subways in rush hour. In the MYmind training, he had learned to just be on the platform. Subways with many thoughts would still come to his platform, but he was now able to let them pass, to just observe them and stay calm.7
There was only one study on acceptance and commitment therapy, which found improvements in psychological distress post intervention, although this was not significant compared to the waitlist group.16 There was also a discrepancy between teacher reports and self-reports of stress, where adolescents with ASD reported no improvements on stress while teachers reported improvements. None of the yoga-based interventions evaluated mental/emotional outcomes.
Effects on behavior
Most of the studies that included children with ASD focused on various aspects of behavior, including aggressive, maladaptive, imitation, and aberrant behaviors. Considering that there was little homogeneity between studies on either outcome measures or intervention type, it is difficult to compare effects between studies. Most studies were without control groups and had extended follow-up periods (≥1 years), making it impossible to differentiate behavioral changes due to interventions, child development, or other factors.
One study delivered a yoga intervention randomized by school classrooms.15 There were significant changes in aberrant behaviors for teacher but not parent ratings. Another study evaluated the effects of Nei Yang Gong compared to Progressive Muscle Relaxation Therapy on self-control for children with ASD.10 Neuropsychological tests of executive function were used as measures of self-control (Tower of London, Children's Color Trials Test, The Five Point Test), which were found to be significantly improved in the Nei Yang Gong group.
Parent-based interventions
Of the parent-based interventions, there was only one RCT.18 Parents were trained in mindfulness-based stress reduction, which improved hyperactivity but not other behaviors in children. Another uncontrolled parent-based intervention, which targeted mental health by teaching mindfulness to both parents and children, found significant improvement in rumination and quality of life but not in worry or mindfulness.7 These results are consistent with the RCT of an autism-adapted mindfulness program mentioned earlier that improved rumination in adults with ASD who were taught directly.9 It is unknown whether interventions delivered to both parent and child have an additive effect compared to interventions delivered to one or the other. Considering the potential negative impact parent mental health can have on child behaviors, these findings support studying whether well-designed mindfulness interventions for parents can help improve children's health.23,24
Modifications for accessibility
Another goal of this review was to determine if modifications were made to any mind–body therapies in order to improve accessibility for people with ASD. Many mind–body therapies use figurative language, which can be challenging for people with ASD, who are more likely to take language literally. Four studies included detailed descriptions on intervention modifications. No studies directly compared modified to non-modified protocols. Of the mindfulness-based interventions, two used the same 9-week protocol adapted for ASD.8,9 The protocols used less metaphorical and ambiguous language, omitted cognitive elements (e.g., “examination of one's thoughts”), and increased the amount of time for breathing exercise and weeks of training to account for participants with slower information processing. Similarly, another mindfulness-based study used less abstract language and added an additional week of mindfulness training.7 They also provided detailed, outlined overviews of each session to participants so they would feel more at ease and able to anticipate the goals and tasks of each mindfulness session. Participants in this study provided feedback that they preferred silence during meditation sessions rather than verbal guidance. Interestingly, a special mindfulness session on coping with changes that was specifically designed for people ASD received low ratings on usefulness from participants.7
An acceptance commitment therapy protocol was also modified for individuals with ASD.16 Smaller group sizes were used for the sessions, mindfulness exercises were shortened, mindfulness exercises on sensory sensitivities were added, stress management worksheets were modified, and metaphors were limited. Participants reported that these adaptations were useful and that they were satisfied with the program overall.16
Future directions and considerations
Most of the reviewed studies do not have control groups and only three are RCTs. Several of the published studies did not report significance values or effect sizes, which would have allowed determination of the strength of the results. In some studies, the results were simply described as “significant” without formal statistical analysis or detailed reporting. Multiple studies had small sample sizes, control groups were uncommon, and reports of aggregate results were sometimes missing. Some studies also relied on parent or teacher reports. These were frequently used for outcomes related to behavior in children.
Several studies made autism-specific modifications to the therapies, but not all reported whether participants with ASD found the modifications useful or sufficient. Qualitative methods were not included in any of the studies reviewed here but could be considered for future mind–body research for people with ASD for input on how to improve the delivery and reception of mind–body therapies.
The length of the interventions is another area for future exploration. Mindfulness-based therapies often entail 8 weeks of training, with weekly group sessions and daily meditation. Such a lengthy time commitment can be discouraging, and shorter interventions may increase compliance. Two of the included studies actually increased the length of training for people with ASD. Shorter intervention lengths are successful in other populations and can improve accessibility of interventions for various psychosocial outcomes.25,26 Remote applications, such as Internet-based mindfulness interventions, may also be a viable option to increase the accessibility of therapies for individuals with time constraints and social or mobility barriers.26,27
The studies included in this review cover a wide-range of applications of mind–body therapies. Mind–body therapies were taught to parents, children with ASD and their parents, as well as adults with ASD. Standardization of training techniques is a promising area for future research, as some interventions were applied in schools, others in clinics, others by parents at home, and others by parents and clinicians together. There was also great variation in age, with most studies focusing on interventions for children and adolescents. Adapting different types of mind–body therapies for use by people with more profound intellectual disabilities is largely unexplored, but could benefit from caregiver-mediated, movement-based approaches such as yoga to replace more cognitive-based options. There may be future issues with generalizability of the currently reviewed studies because most included only higher IQ individuals with ASD and those identified as high functioning.
Adverse event reporting was not included in the majority of studies. Those that did noted no adverse events. While generally considered low risk, mind–body therapies can pose a risk for musculoskeletal injuries (e.g., yoga) and may trigger anxiety or trauma (e.g., mindfulness). Adverse event reporting is therefore an important clinical outcome to report in future studies.
Conclusions
Current work on mind–body interventions for people with ASD is progressing but still in the early stages. Several different types of mind–body therapies have been studied for people with ASD, but existing studies include very different age groups and outcome measures. Therefore, at this time, there is not enough data to compare different therapy dosages or types for particular outcomes or to make definitive recommendations. This review found that mind–body therapies are feasible for children and adults with ASD and are generally considered safe. There is a strong rationale for additional studies. Future research would benefit from larger randomized designs, careful and detailed reporting of modifications and statistics, and more input from individuals with ASD.
Acknowledgments
We would like to thank our mentors, Barry Oken, MD, PhD, and Heather Zwickey, PhD, for their guidance and support.
Author Disclosure Statement
This study was funded by the National Institutes of Health National Center for Complementary and Integrative Health (grant number T32 AT002688 11). No competing financial interests exist.
References
- 1.Hanson E, Kalish LA, Bunce E, et al. Use of complementary and alternative medicine among children diagnosed with autism spectrum disorder. J Autism Dev Disord 2007;37:628–636 [DOI] [PubMed] [Google Scholar]
- 2.Owen-Smith AA, Bent S, Lynch FL, et al. Prevalence and predictors of complementary and alternative medicine use in a large insured sample of children with autism spectrum disorders. Res Autism Spectr Disord 2015;17:40–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing, 2013 [Google Scholar]
- 4.Gotink RA, Chu P, Busschbach JJ, et al. Standardized mindfulness-based interventions in healthcare: An overview of systematic reviews and meta-analyses of RCTs. PLoS One 2015;10:e0124344. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med 2014;174:357–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu WW, Kwong E, Lan XY, et al. The effect of a meditative movement intervention on quality of sleep in the elderly: A systematic review and meta-analysis. J Altern Complement Med 2015;21:509–519 [DOI] [PubMed] [Google Scholar]
- 7.de Bruin EI, Blom R, Smit FM, et al. MYmind: Mindfulness training for youngsters with autism spectrum disorders and their parents. Autism 2015;19:906–914 [DOI] [PubMed] [Google Scholar]
- 8.Kiep M, Spek AA, Hoeben L. Mindfulness-based therapy in adults with an autism spectrum disorder: Do treatment effects last? Mindfulness 2015;6:637–644 [Google Scholar]
- 9.Spek AA, van Ham NC, Nyklicek I. Mindfulness-based therapy in adults with an autism spectrum disorder: A randomized controlled trial. Res Dev Disabil 2013;34:246–253 [DOI] [PubMed] [Google Scholar]
- 10.Chan AS, Sze SL, Siu NY, et al. A Chinese mind–body exercise improves self-control of children with autism: A randomized controlled trial. PLoS One 2013;8:e68184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bogels S, Hoogstad B, van Dun L, et al. Mindfulness training for adolescents with externalizing disorders and their parents. Behav Cogn Psychother 2008;36:193–209 [Google Scholar]
- 12.Rosenblatt LE, Gorantla S, Torres JA, et al. Relaxation response-based yoga improves functioning in young children with autism: A pilot study. J Altern Complement Med, 2011;17:1029–1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Radhakrishna S. Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorder. Int J Yoga 2010;3:26–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radhakrishna S, Nagarathna R, Nagendra HR. Integrated approach to yoga therapy and autism spectrum disorders. J Ayurveda Integr Med 2010;1:120–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koenig KP, BuckleyReen A, Garg S. Efficacy of the get ready to learn yoga program among children with autism spectrum disorders: A pretest–posttest control group design. Am J Occup Ther 2012;66:538–546 [DOI] [PubMed] [Google Scholar]
- 16.Pahnke J, Lundgren T, Hursti T, et al. Outcomes of an acceptance and commitment therapy-based skills training group for students with high-functioning autism spectrum disorder: A quasi-experimental pilot study. Autism 2014;18:953–964 [DOI] [PubMed] [Google Scholar]
- 17.Hwang Y, Kearney P, Klieve H, et al. Cultivating mind: Mindfulness interventions for children with autism spectrum disorder and problem behaviours, and their mothers. J Child Fam Stud 2015;24:3093–3106 [Google Scholar]
- 18.Neece CL. Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. J Appl Res Intellect Disabil 2014;27:174–186 [DOI] [PubMed] [Google Scholar]
- 19.Singh NS, Lancioni GE, Winston AS, et al. Mindful parenting decreases aggression, noncompliance, and self-injury in children with autism. J Emot Behav Disord 2006;14:169–177 [Google Scholar]
- 20.Singh NN, Lancioni GE, Singh ADA, et al. Adolescents with Asperger syndrome can use a mindfulness-based strategy to control their aggressive behavior. Res Autism Spectr Disord 2011;5:1103–1109 [Google Scholar]
- 21.Singh NN, Lanioni GE, Manikam R, et al. A mindfulness-based strategy for self-management of aggressive behavior in adolescents with autism. Res Autism Spectr Disord 2011;5:1153–1158 [Google Scholar]
- 22.Singh NN, Lancioni GE, Winton ASW, et al. Mindfulness-based positive behavior support (MBPBS) for mothers of adolescents with autism spectrum disorder: Effects on adolescents' behavior and parental stress. Mindfulness 2014;5:646–657 [Google Scholar]
- 23.Narayanan MK, Naerde A. Associations between maternal and paternal depressive symptoms and early child behavior problems: Testing a mutually adjusted prospective longitudinal model. J Affect Disord 2016;196:181–189 [DOI] [PubMed] [Google Scholar]
- 24.Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: A transactional relationship across time. Am J Intellect Dev Disabil 2012;117:48–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greeson JM, Toohey MJ, Pearce MJ. An adapted, four-week mind–body skills group for medical students: Reducing stress, increasing mindfulness, and enhancing self-care. Explore (NY) 2015;11:186–192 [DOI] [PubMed] [Google Scholar]
- 26.Kemper KJ, Khirallah M. Acute effects of online mind–body skills training on resilience, mindfulness, and empathy. J Evid Based Complementary Altern Med 2015;20:247–253 [DOI] [PubMed] [Google Scholar]
- 27.Wahbeh H, Goodrich E, Oken BS. Internet-based mindfulness meditation for cognition and mood in older adults: A pilot study. Altern Ther Health Med 2016;22:44–53 [PMC free article] [PubMed] [Google Scholar]