Summary
There are two types of prognostic model - burn-specific and general - to predict mortality risk in burn patients. Most prediction models were devised in developed countries. The aim of this study was to compare the performance of six outcome models in a developing country. In a retrospective cohort study, data of all thermal burned adult patients (age ≥ 18 years) admitted to the Burn Intensive Care Unit (BICU) were collected and then the following six prediction models were used to assess each patient: Acute Physiology and Chronic Health Evaluation (APACHE II), Abbreviated Burn Severity Index (ABSI), Belgian Outcome in Burn Injury (BOBI), the Ryan model, revised Baux and FLAMES model. Discriminative ability and goodness-of-fit of the prediction models were determined by receiver operating characteristic curve analysis and Hosmer–Lemeshow tests. We included 238 patients (mean age: 38.3 ± 18.39 years, average TBSA: 58.27% ± 24.55) in our study; 172 (72.3%) of them were diagnosed with inhalation injury and 178 (72.4%) were intubated. Mortality rate was 69.7%. Deceased patients had significantly higher mean age, %TBSA and number of inhalation injury. The area under the curve of the models was between 64.5 (APACHE II) and 85.9 (ABSI). The best estimation of predicted mortality was obtained with the ABSI model (67.2%).
Keywords: outcome prediction models, adult burn population, developing country, ABSI score, APACHE II
Abstract
Des scores de gravité spécifiques ou généraux peuvent être utilisés pour évaluer le pronostic d’un brûlé, la plupart d’entre eux ayant été construits dans des pays développés. Le but de cette étude était de comparer 6 d’entre eux dans un pays en développement. Les données de tous les patients admis en réanimation spécialisée ont été collectées pour calculer 6 scores de gravité qui étaient : APACHE II, ABSI, BOBI, Ryan, Baux révisé et FLAMES. La sensibilité et la spécificité de ces modèles ont été analysées par courbe ROC et test de Hosmer-Lemeshow. Deux cent trente huit patients de 38,3 +/- 18,39 ans, brûlés sur 58,27 +/- 24,55% de SCT ont été inclus. Cent soixante douze (72,3%) avaient inhalé des fumées et 178 (72,4%) avaient été intubés. La mortalité était de 69,7%. Les patients décédés étaient plus âgés, brûlés sur une plus grande surface et avaient plus fréquemment inhalé des fumées. Les aires sous la courbe ROC allaient de 64,5 (APACHE II) à 85,9 (ABSI). Cette étude confirme que l’ABSI reste le meilleur score de gravité pour les patients brûlés.
Introduction
Over the last few decades, the survival rate of burn-injured patients has increased significantly due to advancements in burn care. However, mortality rate for severe burn injuries is still high.1,2,3 Multiple predictive factors including patient characteristics (age, gender, comorbid diseases …) and burn features (total body surface area, inhalation injury, burn depth, associated trauma …) influence the prognosis. Consequently, if a prediction model considers all of the factors involved, it will be reliable and accurate.4,5 Many prognostic scoring models have been devised to predict mortality risk in burn patients. Mortality prediction models in burn injury have existed since the mid-20th century.6,7 Generally, there are two types of model. The first type is specific for burn-injured patients and applies the features of burn injuries to predicate prognosis. The second type is a general model which focuses on the patient’s acute physiological status and associated comorbidities to evaluate outcome.7,8,9
In addition to assessing the probability of burn patient mortality, accurate and reliable prediction models as a standardized tool can measure burn service performance.10 To evaluate burn service performance, standardized mortality ratio (SMR = observed mortality/predicted mortality) is a suitable index.8 A scoring model must have good predictive value to determine realistic predictions of mortality, as well as repeatability and generalizability potential in different burn populations and hospitals. 11
High mortality rate due to burn injury is still an important and challenging problem in developing countries. The World Health Organization (WHO) estimates that the vast majority of post-burn deaths occur in low- and middle-income countries.12 However, most prediction models were designed in developed countries, and all claim to be the most accurate in different burn populations.8,13,14 There are a limited number of studies that compare well-known prediction models in the same burn population group (cohort).9,13,15 We therefore conducted this study to assess the performance of the six bestknown models for predicting hospital mortality among severely burned adult patients admitted to a burn intensive care unit in a developing country.
Methods
Patient selection
This retrospective population-based cohort study was carried out at the 18-bed Burns Intensive Care Unit (BICU) of Mothahary Hospital in Tehran. This tertiary burn hospital provides burn care services for over 12 million people and is the biggest referral burn center in the capital of Iran. The study was approved by the ethical committee of Iran University of Medical Sciences. Inclusion criteria were all thermal burned adult patients (age ≥ 18 years) admitted to the BICU. Those with multiple traumas, chemical and electrical burns were excluded.
Variable collection
Medical files of eligible burned patients admitted to the BICU over a period of 14 months (Jan 2015 - Mar 2016) were the source of demographic, clinical, physiologic and laboratory data. The worst point for each physiological variable on the first day of a patient’s admission to the ICU was as mentioned in the Acute Physiology and Chronic Health Evaluation (APACHE II)16,17,18 and FLAMES prediction model.19 Percentage of total body surface area (%TBSA), age, gender, clinical signs of inhalational injury and presence of third-degree burn were recorded to calculate Ryan Score,20 Revised Baux Score,21,22 Belgian Outcome in Burn Injury (BOBI) Score23 and Abbreviated Burn Severity Index (ABSI).24 Data on mortality during hospital stay was also collected.
In this study, the following six most well-known and routinely-used prediction models were compared:
Acute physiology and chronic health evaluation (APACHE II) is a physiology-based scoring system and is applicable on the first day of a patient’s admission to the intensive care unit (ICU) for prognosis assessment. The original APACHE was designed in 1981.16 The APACHE II was revised in 1985, eliminating infrequent variables.17,18 The new version includes 12 variables, each of them rated from 0 to 4. The worst point for each physiological variable on the first day of a patient’s admission to the ICU is recorded. Total score ranges from 0 to 71; a higher score is associated with higher mortality risk
FLAMES was developed by Gomez et al to predict outcome in severe burns.19 The probability of death in burn patients, percentage of partial and full thickness burns, age and gender are computed based on the APACHE II score on day 1. Inhalation injury is not considered in this model.
Ryan et al. published their mortality prediction model for burn injuries in 1998.20 This simple method uses 3 parameters - age, total burn surface area and inhalation injury - to assess the risk of mortality. An increasing number of risk factors (0-3) is associated with an increasing mortality rate. When there is no risk factor, mortality rate is 0.3%, one risk factor 3%, two risk factors 33% and 3 risk factors give a probability of death of 90%.
The main Baux Score was modified by Osler et al in 2010 (Revised Baux Score) and in inhalational injury cases, the number 17 is added to the sum of the patient’s age and TBSA.21 Risk of mortality goes from 0 to 100%. Introducing a new nomogram to calculate the Revised Baux Score has simplified its usage.22
Belgian outcome in burn injury (BOBI) was developed in 2009.23 In this model increased age, TBSA and presence of inhalation injury are the 3 risk factors. Age is divided into four groups (0–3 points) and TBSA into 5 groups (0– 4 points). Presence of inhalation injury takes 3 points. Based on total score (0-10 points), predicted mortality ranges between 0.1% and 99%.
The abbreviated burn severity index (ABSI) was published by Tobiasen et al in 1982.24 This system uses five variables to predict prognosis: increased TBSA (1–10 points), increased age (1–5 points), female gender (1 point), presence of inhalation injury (1 point) and presence of full-thickness burns (1 point).13 The sum of these values ranges from 2 to 18 points, and survival probability percentage decreases as the score increases (≤ 10% and ≥ 99%).
Statistical analysis
Statistical analysis was accomplished using the Statistical Package for Social Sciences (SPSS 16, SPSS Inc., Chicago, US). Comparison of demographic and burn characteristics between survivors and deceased patients was performed. Comparison of quantitative continuous variables was carried out using the sample t-test, and categorical variables were compared using the 𝜒2 test. Data are expressed as number (%) or mean ± standard deviation (SD). A P value <0•05 is considered statistically significant.
Binary logistic regression analyses were used to calculate LA50.
The Hosmer and Lemeshow Chi-square statistic test was used to measure accuracy and goodness-of-fit of the prediction models. A Receiver Operator Characteristics (ROC) graph was plotted to assess the discriminative ability of these six prediction models. The area under the curve (AUC) was used to detect which model was more accurate at distinguishing between survivors (false positives) and non-survivors (true positives). An area over 0.9 indicates high accuracy, 0.7- 0.9 moderate accuracy, 0.5-0.7 low accuracy and 0.5 indicates chance discrimination.25
Results
During the study period, 238 eligible patients (59/24.8% female and 179/75.2% male) were admitted to the BICU. Mean age was 38.3 ± 18.39 years, ranging from 18 to 98 years, with a mean total body surface area of 58.27% (± 24.55), ranging from 10% to 100%. A total of 172 (72.3%) patients had inhala tion injury and 178 (72.4%) were mechanically ventilated. Mortality rate was 69.7% (N=166).
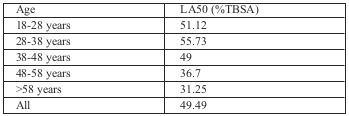
In a comparison between survivors and deceased victims (Table I), the survivors (N=72) had a significantly lower mean age, %TBSA and number of inhalation injuries (respectively P=.021, P=.000 and p=.027). Total LA50 was 49.49%, which was correlated with age (Table II).
Table I. Comparison of demographic and burn characteristics between survivors and deceased patients.
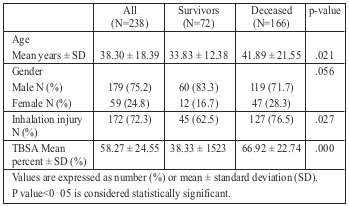
Table II. Lethal area fifty percent (LA50) in all burn patients.
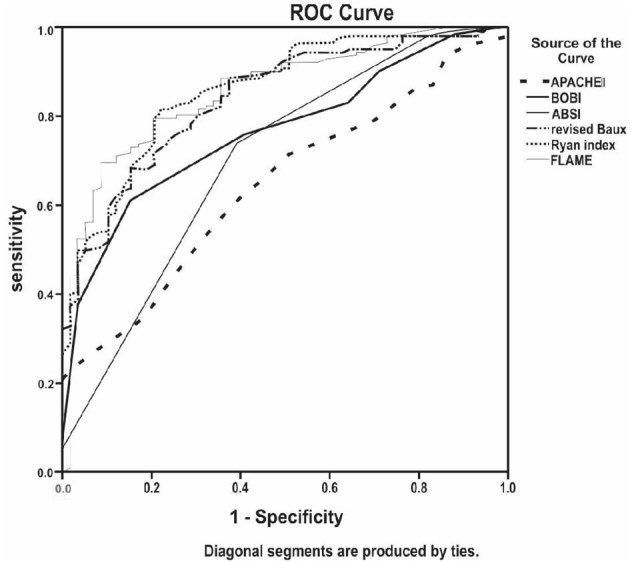
The probability of death predicted by BOBI, rBaux, ABSI, FLAMES, Ryan and APACHE II was respectively 181 (76.0%), 185 (77.7%), 160 (67.2%), 138 (57.9%), 223 (93.6%) and 200 (84.0%), while true mortality was 166 (69.7%) (Table III). The best prediction of mortality percentage was estimated by the ABSI model (67.2%), which had the highest area under the curve of 85.9 (80.5-91.3). Apart from FLAME, the other models over-predicted the number of deaths. The APACHE II area under the ROC curve of 64.5 (56.6-72.3) was lower than the other models, indicating low accuracy at discriminating between survivors and non-survivors (Fig. 1).
Table III. The area under the curve (AUC) analysis and predicted mortality by six models.
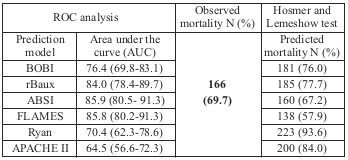
Fig. 1. Receiver operator characteristics (ROC) curve of predicting models. An area under the curve (AUC) of more than 0.9 indicates high accuracy, while an area of 0.5 indicates chance discrimination. The area under the curve (AUC) for the all the scoring models except APACHE II was 0.7–0.9, considered moderate accuracy at distinguishing between survivors and non-survivors. The area under the ROC curve of APACHE II was 64.5(56.6-72.3), indicating low accuracy at discriminating between mortality and survival in patients. The AUC of the ABSI model was higher than the other models 85.9(80.5- 91.3).
Discussion
Despite the large number of burn prognostic models, none can claim to be the most accurate across the entire burn population. 8 The sheer number of different models suggests that none accurately predicts outcome in every population.26 The models have mostly been validated on populations in developed countries, and the number of studies on external validation of the models on populations in developing countries are sparse. There are several studies with varying results regarding the performance of the same outcome prediction models.7,8,13,18,21,26-28 These different results may be due to variations in the population or differences in standards of care in various regions.28 Internally validated prediction models may degrade in other populations.29,30 Therefore, it is very important to evaluate the independent or external validation of the prediction models before using them in a new population or case mix.28,31
In this cohort study, five specific outcome models for burn injured patients and one general prognostic model were evaluated for predicting mortality.
Compared with survivors, deceased patients had a significantly higher mean age, %TBSA and number of inhalation injuries (respectively P =.021, .000, .027). These three important factors are the foundation of nearly all specific burn prediction models.9 Consequently, the importance of these prognostic factors in burn injuries was confirmed by our study.
The area under the curve (AUC) for the five specific outcome models was 0.7–0.9, demonstrating moderate accuracy at distinguishing between survivors and non-survivors, so the majority of burn injured patients who died were expected to die. In this study, true mortality was 166 (69.7%). The predicted mortality estimated by ABSI (160/67.2%) showed the least difference with observed mortality and had the highest area under the curve 85.9 (80.5-91.3). Our finding was similar to other recent studies.13,27,32 Based on one new study, the ABSI scoring system is still an accurate and useful tool to predict mortality in burn patients.32
Percent of inhalation injury in our study was 72.3%, which was higher than previous studies.33,34 Inhalation injury was mostly diagnosed by history taking of exposure to smoke in closed areas, burns due to explosion and physical examination findings. Fiberoptic bronchoscopy had been performed in only a few cases, therefore overestimation of inhalation was possible. This may explain why the Ryan model predicted the highest mortality rate (93%). Because of the importance of inhalation injury in the Ryan model, an increase in inhalation injury percentage increases its score more so than in the other models. The diagnosis of inhalation injury needs to be standardized before using the Ryan model.
The area under the curve (AUC) for APACHE II as a general prognostic model was 64.5, meaning low accuracy at distinguishing between survivors and non-survivors and weak compatibility between observed and predicted deaths. APACHE II is a useful tool to predict mortality in a general intensive care unit, but its validation for burn victims is not clear. The original investigators of the APACHE scoring system did not include burn patients in their study.16,17 As we know that the influence of comorbidities is important in the APACHE II model and since burn patients before injury compared with those admitted to the general ICU are usually healthy, there are fewer comorbidities to increase their APACHE II score.34
Gomez et al. incorporated specific burn risk factors (percentages of partial and full thickness burns, age and gender) in APACHE II and FLAMES.19 In our analysis the FLAMES model under-predicted the number of deaths (57.9 vs. 69.7). Inhalation injury was not considered in this model, and this is probably the reason for the underestimation of predicted mortality in our analysis.
In this study, unlike in that of Brusselaers et al.,13 these three models (BOBI, Ryan and rBaux) overestimated the number of deaths. This difference might be due to the higher number of diagnosed inhalation injuries in our study.
Compared to similar studies,13,15,27,32,35 observed mortality (69.7%) in the present study was higher. Also, lethal area fifty percent (LA50) (49.49%) was lower than in a recent study conducted in our center.36 It is important to take into account that the present study was carried out on severely burned patients with a higher incidence of inhalation injuries admitted to the burn ICU. The higher mortality observed and lower LA50 in our study may be due to a high TBSA mean and high rate of inhalation injury (58.27 ± 24.55% and 72.3% respectively). However, as mentioned by Heng et al., the selection of extensively burn-injured patients had a relative strength due to the high mortality rate that enabled us to reach adequate statistical power, especially when we had a small sample size.9
Limitations
The first limitation of our study was the lack of fiberoptic bronchoscopy to diagnose inhalation injury in all the cases. In most patients, the diagnosis of inhalation injury had been made based on clinical findings. Despite this limitation, the high number of patients receiving mechanical ventilation in the first few days after admission probably confirms the diagnosis of inhalation injury. Moreover, the study was conducted in only one center with a small sample size.
Finally, this research was not a prospective study and the authors could not control confounding factors. This is a preliminary study, and in order to validate our results we need a prospective, multicenter study with a large study population.
Conclusion
In the present study, the six prediction models (five specific burn outcome models and one general prognostic model) were validated, with the ABSI scoring system showing the best performance in predicting mortality and APACHE II the worst.
Our findings confirmed that age, %TBSA and inhalation injury are the most important prognostic factors in burn patients. The variations between our results and other previous studies may be due to differences in population and standards of burn care in various places. Therefore, it is better to verify the validity of prediction models before applying them in a new population.
Acknowledgments
Conflict of interest.There were no conflicts of interest.
Acknowledgments.We thank the Head of the Burn Research Center at Iran University of Medical Sciences, Dr. Mohammad Javad Fatemi, for providing general support in the study.
References
- 1.Brusselaers N, Hoste EA, Monstrey S, Colpaert KE. Outcome and changes over time in survival following severe burns from 1985 to 2004. Intensive Care Med. 2005;31:1648–1653. doi: 10.1007/s00134-005-2819-6. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen LN, Nguyen TG. Characteristics and outcomes of multiple organ dysfunction syndrome among severe-burn patients. Burns. 2009;35(7):937–941. doi: 10.1016/j.burns.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 3.Bloemsma GC, Dokter J, Boxma H, Oen IMMH: Mortality and cause of death in a burn center. Burns. 34(8);2008:1103–1107. doi: 10.1016/j.burns.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Macedo JL, Santos JB. Predictive factors of mortality in burn patients. Rev Inst Med Trop Sao Paulo. 2007;49(6):365–370. doi: 10.1590/s0036-46652007000600006. [DOI] [PubMed] [Google Scholar]
- 5.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–366. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 6.Stylianou N, Akbarov A, Kontopantelis E, Buchan I, Dunn KW. Mortality risk prediction in burn injury: Comparison of logistic regression with machine learning approaches. Burns. 2015;41(5):925–934. doi: 10.1016/j.burns.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Hussain A, Choukairi F, Dunn K. Predicting survival in thermal injury: a systematic review of methodology of composite prediction models. Burns. 2013;39(5):835–850. doi: 10.1016/j.burns.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Sheppard NN, Hemington-Gorse S, Shelley OP, Philp B, Dziewulski P. Prognostic scoring systems in burns: a review. Burns. 2011;37(8):1288–1295. doi: 10.1016/j.burns.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Heng JS, Clancy O, Atkins J, Leon-Villapalos J. Revised Baux Score and updated Charlson comorbidity index are independently associated with mortality in burns intensive care patients. Burns. 2015;41(7):1420–1427. doi: 10.1016/j.burns.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 10.Bowser BH, Caldwell FT, Baker JA, Walls RC. Statistical methods to predict morbidity and mortality: self-assessment techniques for burn units. Incl Therm Inj. 1983;9:318–326. doi: 10.1016/0305-4179(83)90077-3. [DOI] [PubMed] [Google Scholar]
- 11.Williams DJ, Walker JD. A nomogram for calculation of the Revised Baux Score. Burns. 2015;41(1):85–90. doi: 10.1016/j.burns.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organisation: Injury, a leading cause of the global burden of disease. Geneva: World Health Organisation. 2002 [Google Scholar]
- 13.Brusselaers N, Agbenorku P, Hoyte-Williams PE. Assessment of mortality prediction models in a Ghanaian burn population. Burns. 2013;39(5):997–1003. doi: 10.1016/j.burns.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 14.United Nations Development Programme. Human Development Report 2011 – Human development statistical annex. 2011 [Google Scholar]
- 15.Roberts G, Lloyd M, Parker M, Martin R. The Baux score is dead. Long live the Baux score: a 27-year retrospective cohort study of mortality at a regional burns service . J Trauma Acute Care Surg. 2012;72:251–256. doi: 10.1097/TA.0b013e31824052bb. [DOI] [PubMed] [Google Scholar]
- 16.Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Critical Care Medicine. 1981;9(8):591–597. doi: 10.1097/00003246-198108000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Critical Care Medicine. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 18.Wong DT, Knaus WA. Predicting outcome in critical care: the current status of the APACHE prognostic scoring system. Can J Anaesth. 1991;38:374–383. doi: 10.1007/BF03007629. [DOI] [PubMed] [Google Scholar]
- 19.Gomez M, Wong DT, Stewart TE, Redelmeier DA, Fish JS. The FLAMES score accurately predicts mortality risk in burn patients. J Trauma. 2008;65:636–645. doi: 10.1097/TA.0b013e3181840c6d. [DOI] [PubMed] [Google Scholar]
- 20.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–362. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 21.Osler T, Glance LG, Hosmer DW. Simplified estimates of the probability of death after burn injuries: extending and updating the Baux score. J Trauma. 2010;68(3):690–697. doi: 10.1097/TA.0b013e3181c453b3. [DOI] [PubMed] [Google Scholar]
- 22.Williams DJ, Walker JD. A nomogram for calculation of the Revised Baux Score. Burns. 2015;41(1):85–90. doi: 10.1016/j.burns.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Belgian Outcome in Burn Injury Study Group: Development and validation of a model for prediction of mortality in patients with acute burn injury. Br J Surg. 2009;96(1):111–117. doi: 10.1002/bjs.6329. [DOI] [PubMed] [Google Scholar]
- 24.Tobiasen J, Hiebert JM, Edlich RF. The abbreviated burn severity index. Ann Emerg Med. 1982;11(5):260–262. doi: 10.1016/s0196-0644(82)80096-6. [DOI] [PubMed] [Google Scholar]
- 25.Fischer JE, Bachman LM, Jaeschke R. A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med. 2003;29:1043–1051. doi: 10.1007/s00134-003-1761-8. [DOI] [PubMed] [Google Scholar]
- 26.Taylor SL, Lawless M, Curri T, Sen S. Predicting Mortality from Burn Injuries: The need for age-group specific models. Burns. 2014;40(6):1106–1115. doi: 10.1016/j.burns.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dahal P, Ghimire S, Maharjan NK, Rai SM. Baux’s and Abbreviated Burn Severity Score for the Prediction of Mortality in Patients with Acute Burn Injury. Journal of College of Medical Sciences-Nepal. 2015;11(4):2091–2157. [Google Scholar]
- 28.Sathe PM, Bapat SN. Assessment of performance and utility of mortality prediction models in a single Indian mixed tertiary intensive care unit. Int J Crit Illn Inj Sci. 2014;4(1):29–34. doi: 10.4103/2229-5151.128010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med. 1999;30:515–524. doi: 10.7326/0003-4819-130-6-199903160-00016. [DOI] [PubMed] [Google Scholar]
- 30.Roelen CA, Bültmann U, Rhenen WV. External validation of two prediction models identifying employees at risk of high sickness absence: cohort study with 1-year follow-up. BMC Public Health. 2013;13:105. doi: 10.1186/1471-2458-13-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hendriksen JM, Geersing GJ, Moons KG, de Groot JA. Diagnostic and prognostic prediction models. J Thromb Haemost. 2013;11 Suppl 1:129–141. doi: 10.1111/jth.12262. [DOI] [PubMed] [Google Scholar]
- 32.Forster NA, Zingg M, Haile SR, Kunzi W. 30 years later - does the ABSI need revision? Burns. 2011;37:958–963. doi: 10.1016/j.burns.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 33.Sterner JB, Zanders TB, Morris MJ, Cancio LC. Inflammatory mediators in smoke inhalation injury. Inflamm Allergy Drug Targets. 2009;8(1):63–69. doi: 10.2174/187152809787582471. [DOI] [PubMed] [Google Scholar]
- 34.Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med. 2013;21(31):1757–7241. doi: 10.1186/1757-7241-21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pantet O, Faouzi M, Brusselaers N, Vernay A, Berger MM. Comparison of mortality prediction models and validation of SAPS II in critically ill burns patients. Ann Burns Fire Disasters. 2016;29(2):123–129. [PMC free article] [PubMed] [Google Scholar]
- 36.Seyed-Forootan K, Karimi H, Motevalian SA, Momeni M. LA50 in burn injuries. Ann Burns Fire Disasters. 2016;29(1):14–17. [PMC free article] [PubMed] [Google Scholar]


