Summary
Plasma lactate (PL) has been used as a marker of cellular hypoxia and shock. The correlation between PL and clinical outcome has been well accepted in hemorrhagic and septic shock. In contrast to the existing evidence, there are no or almost no data dealing with lactate and burn-related outcome. We attempted to assess whether early plasma lactate (PL) is a useful parameter to predict outcome in burned patients. A prospective study was conducted in a 20-bed adult burn ICU at a university-affiliated teaching hospital in Tunis. Patients admitted within the first 24h post burn with greater than 10% total body surface area (TBSA) burned were enrolled in the study. There were 60 males and 20 females. Mean age was 40.7 ± 19.5 years old, and average TBSA was 32 ± 21%. At admission, 86.7% patients had an initial lactate value of more than 2 mmol/L. In our study, an initial lactate value of 4 mmol/L provided the best sensitivity and specificity: 88% and 79% respectively for predicting sepsis, with an area under the ROC curve of 0,82. Furthermore, plasma lactate cut-off value for mortality prediction was 4.46 mmol/l with a good sensitivity (86%) and specificity (92%). Mortality rate was 36.25%. Plasma lactate appears to be a powerful predictor biomarker of sepsis and mortality in burn patients.
Keywords: lactate, prognostic biomarker, severely burned, sepsis, mortality
Abstract
Le lactate plasmatique (LP) est utilisé comme marqueur de choc et d’hypoxie cellulaire. La corrélation entre LP et pronostic est validée dans les chocs hémorragique et septique. Il n’y a que peu voire pas de données concernant PL et pronostic chez les brûlés. Nous avons étudié si la mesure précoce de PL avait une valeur pronostique chez les brûlés. Une étude prospective a ainsi été menée dans l’unité de réanimation pour adultes brûlés (20 lits) du CHU de Tunis. Les patients (60 hommes et 20 femmes) admis dans les 24 h d’une brûlure touchant plus de 10% de SCT ont été inclus. L’âge était de 40,5 +/- 19,5 ans, la surface brûlée de 32 +/- 21%. La grande majorité (86,7%) des patients avaient LP > 2 mmol/L à l’admission. Une valeur > 4 mmol/L étaient la plus prédictive de complication septique, avec une sensibilité de 88%, une spécificité de 9% et une aire sous la courbe ROC de 0,82. La mortalité était de 36,25% et un seuil de LP à 4,46 mmol/L prédisait le décès avec une sensibilité de 86% et une spécificité de 92%. LP semble donc être un marqueur prédictif fiable de sepsis et de mortalité chez les brûlés.
Introduction
Severe burn results in rapid loss of intravascular volume due to the development of a severe capillary leak.1,2 Burn shock is initially hypovolaemic in nature and is characterized by profound hemodynamic changes including decreased plasma volume, cardiac output and urinary output with consecutively increased systemic vascular resistance resulting in diminished peripheral blood flow.3 So, resuscitation of critical care patients is guided by a combination of clinical findings and invasive monitoring.4-5 The optimal guide to the endpoint of resuscitation still remains controversial with all forms of shock.6-7 However, abnormal serum lactate is reported in some clinical studies to be a precise marker of cellular and whole organism shock.6-8-9 No study of the prognostic value of this serum marker has been reported in burn injury. Therefore, we sought to determine in this study whether plasma lactate (PL) could be used as a prognostic tool in burn injury.
Patients and methods
A prospective and observational study was conducted in a 20-bed intensive burn care unit at a university teaching hospital in Tunis. All consecutive adult burned patients admitted within the first 24h post burn from January 1st 2009 to June 30th 2010 were included in the study. Adult patients admitted after 24h from the thermal injury, or those who were discharged or died 48h after admission were excluded. The Local Ethics Committee approved the study, and informed consent was obtained from all participants or next of kin.
Initial PL measurements were obtained within 4 hours after admission and checked every 6 hours until normalization. The normal lactate value was defined as 1 ± 0.5 mmol/l. Resuscitation of these patients was undertaken according to current standards of care. Parkland formula based on the burn size and body weight of the patient was applied as a first approximation of required fluid administration rates. Thereafter, fluid resuscitation was adapted in order to meet a target urine output of 0.5 to 1 ml/Kg/h and a target mean arterial pressure >65 mmHg. Vital signs, essentially haemodynamic variables, urine outputs and serum lactate were closely recorded in patients with predictive signs of hypovolemia and/or sepsis.
Circulatory shock was defined by the development of arterial hypotension (systolic arterial pressure <90 mmHg requiring the administration of vasopressors) and hyperlactatemia (blood lactate level >2.0 mmol/L) in the presence of signs of alterated perfusion such as oliguria (urine output <0.5 ml/kg/h) or altered mental status. Sepsis was defined by the presence of fever (temperature above 38.5°C), an abnormal white blood cell count (above 13.0 x 109/L or below 4.0 x 109/L), and either positive blood cultures or a documented source of infection. Resuscitation of the patients enrolled was not altered in any fashion by inclusion in the study. A frequent complication of sepsis is the development of organ system dysfunction including acute lung injury, shock renal failure and shock liver failure. Organ failure is defined by the presence of altered organ function in an acutely ill patient in whom homeostasis cannot be maintained without intervention: respiratory failure defined as PaO2/FiO2 less than 300; renal failure defined as serum creatinine level increase by 1.5 and/or urinary output <0.5 ml/kg/h over 6 hours. Liver failure is defined as a development of hepatocellular dysfunction, specifically coagulopathy and mental status changes (encephalopathy) in a patient without known prior liver disease.
Clinical decisions about the rate of fluid resuscitation were adapted by physicians according to clinical findings and hemodynamic monitoring. All statistical analyses were performed using SPSS 16.0. For statistical analysis, we used the Chi-2 test or Fisher test when the conditions of validity of the Chi-2 test were not met. A value of p ≤0.05 was considered statistically significant for the comparison of results. The different predictive values were studied with the area under the ROC curve. Optimum sensitivity, predictive value and area under the receiver operating characteristic (ROC) curve were evaluated. A separate statistical analysis (logistic regression) was then performed to determine biological variables predicting mortality.
Results
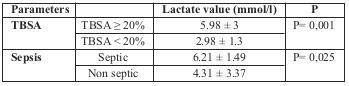
Over an 18-month period from 01/01/2009 to 30/06/2010, a total of 527 burn patients were admitted to our burn intensive care unit (ICU). 447 patients were excluded: 147 patients were discharged during the first 48 hours, 50 patients died in the first 2 days after admission because of severe and extensive burn injury (>80% of TBSA), 80 patients were transferred after 24 hours post injury, 75 patients were under 18 years old, in 30 patients lactate wasn’t measured and 65 patients refused to participate. 80 were investigated and enrolled in the study. There were 60 men and 20 women. The mean age was 40.7 ± 19.5 years old, and the average TBSA was 32 ± 21%. Initial PL measurements were obtained within 4 hours after admission. At admission, 86.7% patients had an initial lactate value of more than 2 mmol/L. Initial PL value was proportional to total body surface area burned (TBSA). In fact, we noted that PL of more than 4 mmol/L was found in patients with burns greater than 20% (Table I).
Table I. Correlation between lactate, TBSA and sepsis.
In evaluating if PL at admission is really useful for estimating septic complications in burned patients, we found that patients with initial PL=4 mmol/l developed sepsis (Table I), knowing that fluid resuscitation goals (a urine output of 0.5 to 1 ml/Kg/h and mean arterial pressure >65 mmHg) were achieved and guided by a close haemodynamic approach. We performed a linear discrimination function by measuring the area under the ROC curve in order to evaluate the potential use of initial lactate measurement (24 h post burn injury) in predicting sepsis in burn patients, and we found that initial lactate value of more than 4 mmol/l provides the best sensitivity and specificity: 88% and 79% respectively. The area under the ROC curve was 0.82 (Fig. 1). Higher blood lactate concentrations can be used to identify patients at high risk of developing organ dysfunction following major burns. So, in a multivariate analysis, it appears that higher serum lactate above 4 mmol/l was correlated to shock and to respiratory failure (Tables II and III).
Fig. 1. ROC Curve of plasma lactate to predict sepsis.
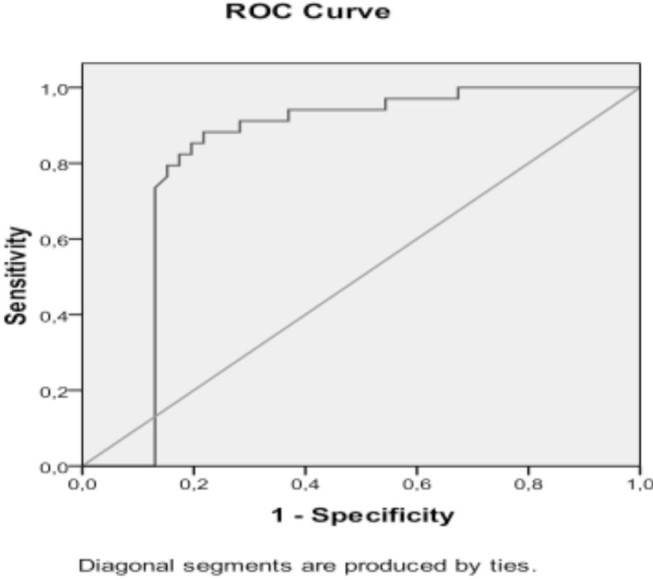
Table II. Initial lactate and organ failure.
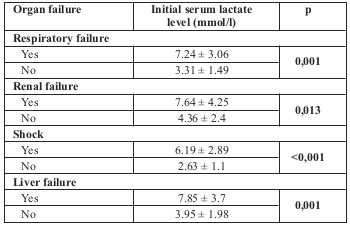
Table III. Multivariate analysis for organ failure for plasma lactate > 4 mmol/l.
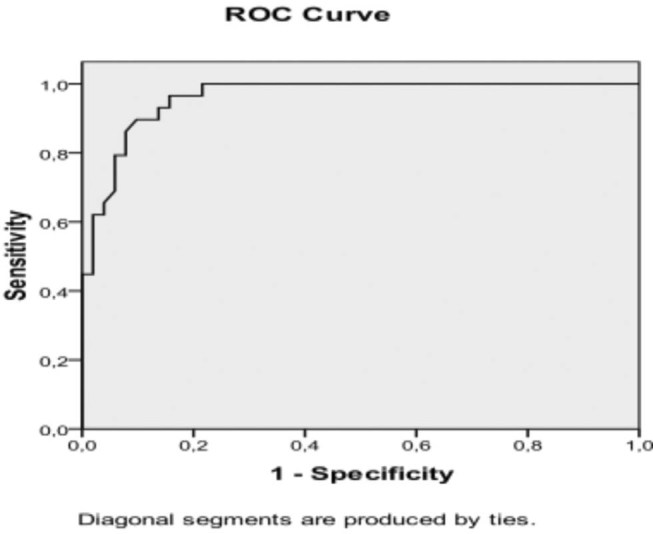
To determine the impact of recorded variables - age, TBSA, inhalation injury and serum lactate - in predicting mortality, a separate multivariate statistical analysis was performed and showed that serum lactate >4.46 mmol/l is an independent predictor factor for mortality (Table IV). A linear discrimination function was performed by measuring the area under the ROC curve to assess the validity of initial PL for predicting mortality in burned patients. This shows that plasma lactate has a discriminative power with an area under the ROC curve of 0.96. Cut-off value of PL for mortality prediction was 4.46 mmol/l with a good sensitivity (96.6%) and specificity (84.3%) (Fig.2). In fact, there was a significant difference in lactate levels between non-survivors and survivors, respectively 8.27 ± 3.02 versus 4.88 ± 1.4 mmol/l (p<0.001).
Table IV. Multivariate analysis of factors predicting mortality.
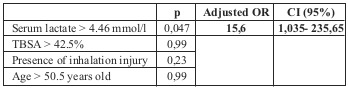
Fig. 2. ROC Curve of plasma lactate in predicting mortality.
Discussion
The main finding of this study is that higher blood lactate concentration could be used as a prognostic tool in burn injury including septic complications, organ dysfunction and mortality. A higher admission lactate concentration and PL changes are significant markers of shock and resuscitation. Both parameters are important for assessment of burn severity and are strongly associated with increased hospital complications and mortality. They might help to improve therapeutic strategies. It is widely accepted that blood pressure and urinary output are useful but do not sufficiently reflect global perfusion, regional microcirculation nor reversal of shock.10 The optimal marker of resuscitation would possess these qualities: accuracy, easy and rapid acquisition, reproducibility in different types of shock states and rapid change in response to resuscitation.
Lactate is a by-product of anaerobic cellular metabolism due to insufficient cellular oxygen supply. Concerning shock resuscitation, PL is frequently used as a predictor of morbidity and outcome. Kamolz et al.11 have demonstrated, in the largest study performed in burned patients, that lactate level, as well as lactate clearance, accurately predicts shock and response to resuscitation. PL may be reflective of injury severity coupled with the effectiveness of the host response. In our series, PL is higher in patients with TBSA ≥20% versus patients in whom TBSA <20%, respectively 5,98 ± 3 and 2,98 ± 1,3 (p= 0,001) and appears to be a powerful marker in predicting outcome in a common clinical cause of shock: severe burns. In fact, in our study occurrence of sepsis was predicted by the initial serum lactate level with an initial lactate value of 4 mmol/ providing the best sensitivity and specificity: 88% and 79% respectively, with an area under the ROC curve of 0,82. Also, higher blood lactate concentrations can be used to identify patients at high risk of developing organ dysfunction following major burns. Mortality after burns was clearly predicted by serum lactate over the 24 h observation period. Cut-off value of PL for prediction of mortality was 4.46 mmol/l with a good sensitivity (86%) and specificity (92%). So, when presenting with a severe elevation and/or persistence of serum lactate, the clinician would be advised to maximize scrutiny of the patient’s care, or alternatively, recognize the possible futility of clinical interventions. In many types of shock elevated blood lactate levels have been correlated strongly with mortality12,13 and the results of this study indicate that lactate leads also to separating survivors from non-survivors in burn shock. In contrast to the existing evidence mentioned above, there are no or almost no data dealing with lactate and lactate clearance in burns. Kamolz et al.11 demonstrated that survival was related when resuscitation efforts normalized lactate values within 24 h. Survival was 68% if the lactate reached normal values within 24 h, compared with 32% if the lactate level was higher than 2 mmol/l.11 These results are comparable to the findings in other shock scenarios.14,15,16 Normalization of initial elevated arterial lactate indicates adequate tissue perfusion, correction of the oxygen debt and adequate oxygen extraction in combination with an intact lactate metabolism in the liver, whereas a failure is associated with the inability to reach end points of resuscitation. We also think that initial lactate level is influenced by burn size. The main strength of our study is the significant degree to which the initial lactate level predicted severity of burns and thereby mortality (p < 0.001). In burned patients, hyperlactataemia is associated with increased hospital complications such as septic complications and organ failure. Blood lactate concentrations >4 mmol/l can be used by clinicians to identify patients at high risk of complications and those at high risk of death. Jeng et al. have also demonstrated that lactate has a predictive value for outcome after burns.17 Nevertheless, the current reference range for lactate in burns may need to be re-assessed and to emphasize mainly in higher time-weighted lactate concentrations in a large cohort of critically burned patients. The present study has its limitations. First, it included patients with a large total body surface area burned (average TBSA was 32 ± 21%), and lactate increases due to capillary hyperpermeability and oedema. Second, in our study we focused only on admission lactate levels but the addition of time course of blood lactate levels may improve the prediction of outcome of burns. Therefore it should be emphasized that none of the parameters studied could accurately predict outcome of burns, which can be influenced by numerous factors.
Conclusion
Plasma lactate has been proven to be a good predictor marker of sepsis and mortality in burn patients. It is sensitive, specific, reliable and easy to measure. A serum lactate of 4 mmol/L provides the best sensitivity and specificity. Therefore titration of burn resuscitation to nearly normalize PL levels may be a reasonable method to reduce burn mortality. As the outcome of burn patients is affected by a large number of modulating factors, a multi-center prospective study would be necessary to confirm the hypothesis that correction of PL during burn shock resuscitation affects outcome due to less organ dysfunction, and might lead to a lower mortality rate.
Acknowledgments
Acknowledgements.We thank all authors for their contribution to the study design, the collection, analysis and interpretation of data, writing the manuscript and in the decision to submit the manuscript for publication.
References
- 1.Rutledge R, Osler T, Emery S, Kromhout-Schiro S. The end of the Injury Severity Score (ISS) and the Trauma and Injury Severity Score (TRISS): ICISS and International Classification of Diseases, ninth revision- based prediction tool, outperforms both ISS and TRISS as predictors of trauma patient survival, hospital charges, and hospital length of stay. J Trauma. 1988;44:41–49. doi: 10.1097/00005373-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Ishihara H, Otomo N, Suzuki A, Takamura K. Detection of capillary protein leakage by glucose and indocyanine green dilutions during the early post-burn period. Burns. 1998;24(6):525–531. doi: 10.1016/s0305-4179(98)80004-1. [DOI] [PubMed] [Google Scholar]
- 3.Germann G, Steinau HU. Current aspects of burn treatment. Zentralbl Chir. 1993;118(5):290–302. [PubMed] [Google Scholar]
- 4.Baxter CR. Fluid volume and electrolyte changes of the early post burn period. Clin Plast Surg. 1974;4:693–703. [PubMed] [Google Scholar]
- 5.Herndon DN, Hilton JG, Traber DL, Barrow RE. Burn shock and its resuscitation. Prog Clin Biol Res. 1987;236A:539–557. [PubMed] [Google Scholar]
- 6.Mikulaschek A, Henry SM, Donovan R. Serum lactate is not predicted by an ion gap or base excess after trauma resuscitation. J Trauma. 1996;40:218. doi: 10.1097/00005373-199602000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Vincent JL. End-points of resuscitation: arterial blood pressure, oxygen delivery, blood lactate, or. . . ? Intensive Care Med. 1996;22:3. doi: 10.1007/BF01728324. [DOI] [PubMed] [Google Scholar]
- 8.Allison PD. The SAS Institute Inc. Cary, NC: 1995. Survival analysis using the SAS® system: a practical guide. [Google Scholar]
- 9.Shires GT, Black EA. Second conference on supportive therapy in burn care. J Trauma. 1981;21:665. [PubMed] [Google Scholar]
- 10.Wo CC, Shoemaker WC. Unreliability of blood pressure and heart rate to evaluate cardiac output in emergency resuscitation and critical illness. Crit Care Med. 1993;21:218–223. doi: 10.1097/00003246-199302000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Kamolz LP, Andel H, Schramm W, Meissl G. Lactate: early predictor of morbidity and mortality in patients with severe burns. Burns. 2005;31:986–990. doi: 10.1016/j.burns.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Weil MH, Afifi AA. Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation, 1970;41:989–1001. doi: 10.1161/01.cir.41.6.989. [DOI] [PubMed] [Google Scholar]
- 13.Bakker J, Gris P. Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg. 1996;224:97–102. doi: 10.1016/S0002-9610(97)89552-9. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen HB, Rivers EP. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32:1637–1642. doi: 10.1097/01.ccm.0000132904.35713.a7. [DOI] [PubMed] [Google Scholar]
- 15.McNelis J, Marini CP. Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit. Am J Surg. 2001;182:481–485. doi: 10.1016/s0002-9610(01)00755-3. [DOI] [PubMed] [Google Scholar]
- 16.Nichol AD, Egi M, Pettila V. Relative hyperlactatemiae and hospital mortality in critically ill patients: a retrospective multi-center study. Critical Care. 2010;14:R25. doi: 10.1186/cc8888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeng CJ, Jablonski K, Bridgeman A, Jordan MH. Serum lactate, not base deficit, rapidly predicts survival after major burns. Burns. 2002;28:161–166. doi: 10.1016/s0305-4179(01)00098-5. [DOI] [PubMed] [Google Scholar]


