Summary
Pediatric palmar contact burns are becoming a common trauma, especially in young children. Treatment of this kind of burn is challenging as well as controversial, regarding the choice between split-thickness or full-thickness skin graft to close the defect. The aim of this review was to evaluate the treatment algorithm at our clinic. We conducted a retrospective study including all patients 0 - 5 years of age admitted to our department from 2008 to 2012 with isolated superficial or deep partial-thickness palmar burns. The mean age was 16.1 months. In 27 cases (52.9%) we were able to close the wound conservatively. Average healing time in this group was 13.3 days. Two of these 27 patients developed flexion contractures, but none of them required additional operation. Twenty-four patients were treated using split-thickness skin graft. The average time period from the day of injury to the day of surgery was 14.2 days. Contractures occurred in 5 (20.8%) of the patients who underwent grafting, Secondary reconstruction using full-thickness skin graft was performed in all 5 of them, which represents 9.8% of all patients. We consider split-thickness grafting quick, easy and effective, with minimal to no donor site morbidity and insignificant inflammation complications. Due to reduced healing time after the actual grafting, rehabilitation can commence earlier.
Keywords: hand burns, contact burns, skin graft, contracture
Abstract
Les brûlures palmaires par contact sont devenues un traumatisme commun surtout chez les jeunes enfants. Le traitement de ce type de brûlures est non seulement un challenge, mais il est aussi controversé quant au choix de la greffe de peau mince ou de peau totale pour couvrir la perte de substance. Le but de cette revue est d’évaluer l’algorithme thérapeutique dans notre service. Nous avons conduit une étude rétrospective incluant tous les patients entre 0 et 5 ans admis dans notre département de 2008 à 2012 avec des brûlures palmaires du 2e degré superficiel ou du 2e degré profond. L’âge moyen était de 16,1 mois. Dans 27 cas (52,9%), nous avons pu fermer la plaie sans greffe. Le temps de cicatrisation moyen dans ce groupe était de 13,3 jours. Deux de ces 27 patients ont développé des rétractions en flexion, mais aucune n’a nécessité d’opération secondaire. 24 patients ont été traités par greffe de peau mince. La période moyenne entre le jour de la brûlure et le temps chirurgical était de 14,2 jours. Les rétractions ont été observées chez 5 patients (20,8%) qui avaient subi une greffe. La reconstruction secondaire par greffe de peau totale fur réalisée chez tous les 5, ce qui représente 9,8% de tous les patients. Nous considérons que la greffe de peau mince est rapide, aisée et efficace avec une morbidité minimale ou nulle du site donneur et des suites inflammatoires insignifiantes. La réduction du temps de cicatrisation après la greffe, autorise une rééducation précoce.
Introduction
The full scope of hand-burn treatment can be challenging, even for a skilled surgeon. Specifically, pediatric palmar contact burns, a common injury in young children,1, are currently becoming a widely-discussed topic due to their increasing incidence. The risk is increasing, especially in early childhood when the hand is a tool for interacting with the environment. Combined with the child’s inherent curiosity, slower withdrawal reflex and thinner skin barrier, this sets the stage for the development of deep contact burns when the child is exposed to heated surfaces such as fireplaces, cookers or irons for a prolonged period of time.2,3,
There are several specific histological and anatomic features that make skin grafting to the palm quite demanding. Glabrous skin - a thick type of skin occurring on the palms and feet - is more durable and less elastic, making it able to withstand pressure and traction. The epidermal part is coarse, stratum corneum that reaches a thickness of 400 – 600 um (while it is only 75 – 150 um on the rest of the body). It contains numerous sweat glands, tactile corpuscles, and is highly vascularized.4 On the other hand, melanocytes are sporadic and sebaceous glands and hair follicles are absent.
Considering anatomic peculiarities, ligamentous apparatus needs to be mentioned. Palmar cutaneous ligaments run from the synovial tendon sheath to the skin, while dorsal cutaneous ligaments run from the sides of the phalanges to the skin. Palmar ligaments are thinner and straighter than the dorsal ones. This is clinically significant in the formation of flexion contractures.5
Although this type of burn is considered a serious injury, the majority heal without the need for surgical intervention.6
Nevertheless, poorly managed palmar burns can result in hypertrophic scars with flexion contractures, which can also occur as a result of the uneven growth of the hand and scar itself. 7 Surgical procedures are needed in cases of deep-partial and full-thickness burns.2 The aim of grafting a hand burn is the best possible cosmetic and functional result, while minimizing the incidence of contractures. Great controversy exists over the choice between split-thickness skin grafts and fullthickness skin grafts to close the defect.8 The aim of this study was to review and evaluate the treatment approach to pediatric palmar contact burns at the Prague Burn Center.
Methods
Study design
We performed a retrospective review of all patients of 0 – 5 years of age admitted to our department from 2008 to 2012 with isolated superficial or deep partial-thickness palmar burns, whether or not grafting was conducted. The 5-year mark was set because the majority of patients were below this age. The individuals were picked from our burn center patient records. We excluded patients with multiple body part burns, scalds, flame, electric and chemical burns, as well as the ones admitted with full-thickness burns.
Treatment protocol
The therapeutic management of partial-thickness palmar contact burns (Fig. 1) at our center consists of daily wound dressing changes and intensive rehabilitation during the first 14 days post burn. The treatment is highly individualized, tailored to each patient’s condition. We apply antibacterial cream with 1% silver-sulfadizine (Flamazine®) in the burn unit treatment room and, if needed, debridement of the defect is performed under full sedation in our operating room. If the probability of future contracture formation is high, we use dorsal splints that position the wrist in neutral extension and the digits in extension. Splints are secured with elastic bandages and worn by the patient without intermission.
Fig. 1. Typical II a-b grade contact burn.

We usually prefer surgical treatment in those cases where healing does not progress after the first 14 days after injury (Fig. 2), or if the burn injury is an early stage full-thickness burn. The surgical procedure of choice is split-thickness skin grafting (Fig. 3) from the lateral upper thigh area.
Fig. 2. II a-b grade contact burn after 12 days of conservative tretment.

Fig. 3. Palm after the debridement and split-thickness skin grafting.

Our rehabilitation system consists of stretching and rangeof-motion physiotherapy, application of silicone sheets, custom-made elastic gloves, finger separators as well as thermoplastic palmar splints, which are applied at bedtime. Once the wound is closed and the graft properly healed (Fig. 4), the parents are thoroughly educated about rehabilitation techniques, with the aim that it is continued at home after patient discharge. We consider parental compliance, supervision and good cooperation crucial for the best possible aesthetic and functional outcomes in the long-term, assessed during patient follow-up visits at our out-patient clinic.
Fig. 4. Final result.

If contractures form after scar maturation, we perform reconstructive surgical procedures, which largely consist of scar tissue excision. The defect is closed with a full-thickness skin graft harvested from the left inguinal area. In indicated cases, we perform a z-plasty instead.
Results
Within the 5-year time period chosen for our study, 51 patients between the age of 0 – 5 years with isolated palmar contact burn were admitted to our burn center. The mean age was 16.1 months. 53% of the patients were male, 47% female, bilateral injury was most common (39%), followed by the left palm (35%) and right palm (26%). The mechanisms of the burns were the following: 59.4% fireplace, 11.8% iron, 7.8% cooker, 7.8% pots and pans, 7.8% ovens, 5.6% stoves, 2% grill and 2% toaster.
In 27 cases (52.9%) we were able to close the wound conservatively. The average healing time in this group was 13.3 days. Two of these 27 patients developed flexion contractures of the index finger, but none of them required additional operation.
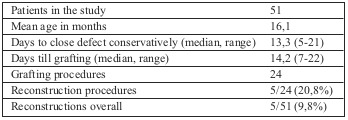
Twenty-four patients were treated with skin grafting using split-thickness skin graft. The average time period from the day of injury to the day of surgery was 14.2 days. Contractures occurred in 5 of the patients who underwent grafting. Secondary reconstruction using full-thickness skin graft was performed in all 5 of those cases (Table I).
Tab. I. Results overview.
Discussion
The aim of palmar burn therapy is an optimal functional and aesthetic result. Our strategy is primarily a conservative approach with topical antibacterial treatment in the first two weeks after injury. Burns that take more than 3 weeks to heal develop burn scars and contractures regardless of type and depth of the injury.1 Barret et al1 stated that 96.7% of patients healed spontaneously, and 6.6% required reconstructive surgery. Scott et al6 treated 87% conservatively, while 4.6% of patients needed secondary reconstruction. In our study, 52.9% of patient burns healed spontaneously and 9.8% developed contractures requiring reconstructive operation. None of our patients with conservatively closed wounds underwent reconstructive surgery. The lower count of spontaneously healed patients in our department may be due to the fact that Barret’s study did not involve only contact burns, and that the majority of our patients were treated as outpatients for whom no register is available.
If surgery is needed, we perform split-thickness skin grafting followed by multimodal rehabilitation therapy. If subsequent reconstruction is needed, the method of choice is a full-thickness skin graft. 24 (47.1%) of our patients required split-thickness grafting, while 5/24 (20.8%) underwent secondary reconstruction using full-thickness skin graft.
Controversy still exists regarding the choice of graft. The current trend is to use full-thickness skin grafting because it is believed to be associated with a lower secondary contracture rate, decreasing the need for secondary surgical procedures; however, it has limited donor sources so it cannot be used to cover larger areas and it has a lower take rate due to increased number of edema and inflammatory reactions. Split-thickness skin grafts, on the other hand, have a higher rate of secondary contractures, mainly when covering metacarpo-phalangeal joints, and less aesthetic value. However, they can cover large areas, have high take rates and fewer infections.2 Prasetyno et al.2 state that currently there is no strong, high-quality evidence to prove that full-thickness skin grafting is superior to splitthickness skin grafting to cover pediatric palmar burns.
Pham at al7 performed full-thickness skin graft if the burn did not heal within 2 weeks. None of the patients in the study required any further procedures. Chandrasegaram et al9 support full-thickness skin grafting, particularly when palmar burns extend to the phalanges, with the result of 1/12 contractures. Pensler8 favours the split-thickness skin graft, as this type of graft does not influence the final functional result. Barret1 used split-thickness skin graft to close the wounds, however all of these patients developed late sequelae. Scott6 selected the skin grafting method according to the size of the palm burn. 4/19 patients who underwent initial split-thickness skin grafting required subsequent full-thickness grafting, which is consistent with our own results.
We consider split-thickness grafting quick, easy and effective, with minimal to no donor site morbidity and insignificant inflammation complications. Healing time is reduced to 5-7 days after the actual grafting and therefore rehabilitation can be commenced earlier.
The area we believe should be explored further is the use of glabrous skin in the treatment of pediatric palmar burns. It meets the objective of replacing like with like, providing excellent functional and aesthetic results10 with improved sensation, texture and durability.11,12
Discussion
Palmar contact burns are severe and potentially debilitating injuries, yet they have a good prognosis and high probability of spontaneous healing. Their treatment is challenging mainly because of the nature of glabrous skin. Therefore, early range-of-motion physiotherapy should be performed, preferentially to close the wound within 14 days. Grafting should only be considered in cases where healing fails to progress. Parent compliance, education and supervision is imperative for optimal long-term outcomes. With respect to the increased incidence of palmar contact burns, the importance of increased public awareness regarding their prevention is emphasized and needed.
Acknowledgments
Editor’s CommentPediatric palmar burns continue to be a common injury. They are primarily caused by contact with stoves or fireplaces or other hot objects and are often deep; they are a particularly unique subset of burns. Poorly managed palm burns can result in functionally debilitating contractures that interfere with hand growth and function and have long-term implications for the psychosocial well-being of growing children. Though the majority of pediatric palm burns heal without the need for acute or reconstructive surgery, ideal management of these burns remains unclear and is still controversial. There is great disagreement among experienced burn care providers over the optimal management approach. While the need for wound care and aggressive early range of motion is clear, the optimal timing and details of the surgical management of these injuries is less clear. The actual gold standard is to practice early excision followed by skin grafting. Palmieri and others have advocated early excision and grafting with full thickness grafts. On the other hand, according to Sheridan et al and Zamboni et al the majority of pediatric palm burns heal without the need for excision and grafting, with excellent functional outcome. Good results have been reported following spontaneous healing combined with splinting and rehabilitation. The favored approach by many includes a period of watchful waiting with early, aggressive range of motion therapy maximizing combined full passive range of motion stretching at the digits, thumb, palm and wrist, reserving grafting only for those palms that do not heal in a timely manner. When range of motion therapy is not being performed sufficiently or when contracture starts to develop, splinting is initiated. Aggressive non-operative management does not lead to higher subsequent rates of reconstruction. Ultimately, the decision for excision and grafting is based on whether or not the wound has the potential for re-epithelialization and healing. Wounds that can heal within 3 weeks may have superior sensation and function than those that are excised and grafted. In the minority of cases where full-thickness injury is clearly evident, excision and grafting must not be delayed. Timing of surgical intervention is not the only subject of controversy. The type of skin graft for optimal functional and cosmetic outcomes, full-thickness skin grafts (FTSG) or thick split-thickness skin grafts (STSG), is another subject of heated debate. Clearly, final outcomes are influenced greatly by compliance with hand therapy exercises and splinting, nevertheless decreased function has been reported when STSG is applied, with increased need for subsequent reconstructive procedures. On the other hand, excellent aesthetic and functional outcomes have been reported in pediatric palm burns treated with FTSG. The use of FTSG is preferred particularly when the burn extends into the digits. Generally, available data suggest improved outcome with FTSG, however, with the exception of scar pliability, differences in outcome between FTSG and STSG are not highly significant as reported by some authors. Split-thickness and full-thickness skin grafts result as well in palm skin texture and pigmentation notably different from nonburned palms. The use of plantar glabrous skin grafts, particularly for dark-skinned children, may offer a reliable and preferable option for coverage.
Conflict of interest.The authors declare that they have no conflict of interest related to this article.
References
- 1.Barret JP. The isolated burned palm in children: epidemiology and long-term sequelae. Plast Reconstr Surg. 2000;105:949–952. doi: 10.1097/00006534-200003000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Prasetyono TO. The use of split-thickness versus full-thickness skin graft to resurface volar aspect of pediatric burned hands: A systematic review. Burns. 2015;41:890–906. doi: 10.1016/j.burns.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 3.Smith MA. Burns of the hand and upper limb - a review. Burns. 1998;24:493–505. doi: 10.1016/s0305-4179(98)00063-1. [DOI] [PubMed] [Google Scholar]
- 4.Konigova R, Blaha J. Complex treatment of the burn trauma. Karolinum, Charles University, Prague. 2010:38–39. [Google Scholar]
- 5.Sabnis A. Morphological study of cutaneous ligaments of phalanges. Int J Morphol. 2013;31(2):606–608. [Google Scholar]
- 6.Scott JR. Pediatric palm contact burns: a ten-year review. J Burn Care Res. 2008;29(4):614–616. doi: 10.1097/BCR.0b013e31817db8f2. [DOI] [PubMed] [Google Scholar]
- 7.Pham TN. Results of early excision and full-thickness grafting of deep palm burns in children. J Burn Care Rehabil. 2001;22(1):54–57. doi: 10.1097/00004630-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Pensler JM. Reconstruction of the burned palm: full-thickness versus split-thickness skin grafts: long-term follow-up. Plast Reconstr Surg. 1988;81(1):46–49. [PubMed] [Google Scholar]
- 9.Chandrasegaram MD. Full-thickness vs split-skin grafting in pediatric hand burns - a 10-year review of 174 cases. J Burn Care Res. 2009;30(5):867–871. doi: 10.1097/BCR.0b013e3181b48610. [DOI] [PubMed] [Google Scholar]
- 10.Friel MT. The use of glabrous skins grafts in the treatment of pediatric palmar hand burns. Ann Plast Surg. 2015;75:153–157. doi: 10.1097/SAP.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 11.Engelhardt TO. Plantar intermediate-thickness skin graft for palmar resurfacing: a valuable alternative with low morbidity. Ann Plast Surg. 2011;67:675. doi: 10.1097/SAP.0b013e31822afb10. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura K. A retrospective study of thick split-thickness plantar skin grafts to resurface the palm. Ann Plast Surg. 1984;12:508–513. doi: 10.1097/00000637-198406000-00003. [DOI] [PubMed] [Google Scholar]


