Abstract
Despite robust support for the role of affect in the maintenance of binge eating and purging, the relationship between affect and restrictive eating remains poorly understood. To investigate the relationship between restrictive eating and affect, ecological momentary assessment data from 118 women with anorexia nervosa (AN) were used to examine trajectories of higher-order dimensions of negative affect (NA) and positive affect (PA), as well as lower-order dimensions of NA (Fear, Guilt) and PA (Joviality, Self-Assurance) relative to restrictive eating. Affect trajectories were modeled before and after restrictive eating episodes and AN subtype was examined as a moderator of these trajectories. Across the sample, Guilt significantly increased before and decreased after restrictive eating episodes. Global NA, Global PA, Fear, Joviality, and Self-Assurance did not vary relative to restrictive eating episodes across the sample. However, significant subtype by trajectory interactions were detected for PA indices. Among individuals with AN restricting subtype, Global PA, Joviality, and Self-Assurance decreased prior to and Self-Assurance increased following restrictive eating episodes. In contrast, Global PA and Self-Assurance increased prior to, but did not change following, restrictive eating episodes among individuals with AN binge eating/purging subtype. Results suggest that dietary restriction may function to mitigate guilt across AN subtypes and to enhance self-assurance among individuals with AN restricting subtype.
Keywords: anorexia nervosa, restrictive eating, affect regulation, ecological momentary assessment
General Scientific Summary
It is not well understood why individuals with anorexia nervosa engage in persistent restrictive eating. The results of this study indicate that individuals with anorexia nervosa may engage in restrictive eating because it decreases guilt and, for those with anorexia nervosa, restricting subtype, enhances self-assurance.
Anorexia nervosa (AN) is a serious and often recalcitrant disorder that is associated with significant physical and psychological morbidity, as well as elevated mortality rates (Braun, Sunday, & Halmi, 1994; Crow et al., 2009; Mitchell & Crow, 2006). Unfortunately, effective interventions for adults with AN are lacking (Berkman et al., 2006) and, as a result, remission rates are low (Ackard, Richter, Egan, & Cronemeyer, 2015) and relapse is common (Pike, 1997). Perhaps the most distinctive feature of AN is the persistent and enduring nature of the restrictive eating that is required for diagnosis of this disorder (American Psychiatric Association, 2013; Walsh, 2013). Restrictive eating comprises eating behaviors in which caloric and/or nutrient intake is limited in a manner that is inadequate for the long-term management of weight and/or health for reasons primarily pertaining to body image (Haynos & Fruzzetti, 2015). Restrictive eating includes a diverse set of eating behaviors, including more discrete and extreme instances of reducing intake (e.g., fasting, skipping meals), as well as more chronic reduction of energy (e.g., consistently decreasing food portions). Restrictive eating has been shown to precede the development of AN (Affenito, Dohm, Crawford, Daniels, & Striegel-Moore, 2002), to persist following intensive intervention (Mayer, Schebendach, Bodell, Shingleton, & Walsh, 2012), and to predict poor treatment response (Schebendach, Mayer, Devlin, Attia, & Walsh, 2012). Thus, restrictive eating appears to play a key role in the initiation and persistence of AN.
Overall, the psychological processes involved in the development and maintenance of restrictive eating patterns among individuals with AN remain poorly understood, likely contributing to the paucity of effective treatments for this population (Walsh, 2013). To identify more effective treatment targets, a better understanding of the psychological mechanisms associated with restrictive eating in AN is needed. Etiological models emphasizing the role of affect regulation have received increasing attention in AN. According to such models, individuals with AN have deficits in the ability to effectively modulate affect and, therefore, rely on eating disordered behaviors to alter emotional experiences (Haynos & Fruzzetti, 2011). Specifically, eating disordered behaviors in AN, such as restrictive eating, are posited to reduce negative affect (NA) and/or increase positive affect (PA), thereby maintaining these behaviors through negative and/or positive reinforcement. However, despite evidence suggesting a clear affect regulation function of some eating disorder behaviors in AN (e.g., binge eating, purging, self-weighing; Engel et al., 2013; Goldschmidt et al., 2015), there is currently limited and mixed evidence regarding the relationship between affect and restrictive eating in AN.
Several studies have demonstrated a link between affective states and restrictive eating in AN. Results from objective meal studies of individuals with AN have found NA to increase and PA to decrease from immediately before to immediately after consuming a regular, non-restrictive meal (Anderson, Crow, & Peterson, 2014), suggesting that affect is impacted by consumption practices in this population. Further, our group has conducted several analyses of a data set that used ecological momentary assessment (EMA) of individuals with AN to examine the relationship between affect and disordered eating in real-time. These analyses have consistently identified a link between affective variables and restrictive eating, such that: (1) higher NA on one day predicts restriction on the subsequent day (Engel et al., 2013); (2) NA is lower and PA is higher before, during, and after restrictive eating episodes in comparison to non-restrictive episodes (Fitzsimmons-Craft et al., 2015); and (3) daily NA lability is associated with restriction (Haynos et al., 2015; Lavender et al., 2013).
However, despite these data suggesting associations between affect and restrictive eating, there is mixed evidence regarding the extent to which affect and restrictive eating are functionally related. In other words, it is unclear whether affective changes serve as clear precipitants and/or consequences of restrictive behavior. For instance, one laboratory test meal study conducted with an sample found that a negative mood induction resulted in an increased desire to restrict, but did not significantly alter caloric consumption among individuals with AN (Wildes, Marcus, Bright, & Dapelo, 2012). On the other hand, another laboratory study of individuals with AN found that a positive mood induction resulted in increased caloric consumption (Cardi, Esposito, Clarke, Schifano, & Treasure, 2015). Analyses of the AN EMA data from our research group have presented similar disparities. A recent analysis from these data examined affect at single time points immediately before, during, and after restrictive eating and found that NA increased prior to restrictive eating, but contrary to an affect regulation hypothesis, remained stable after restrictive eating (Fitzsimmons-Craft et al., 2015). This same study found that PA remained stable prior to restrictive eating and decreased following restrictive eating, which also runs contrary to an affect regulation hypothesis. However, in another analysis from the same data set, it was noted that findings regarding the extent to which a functional relationship between affect and restrictive behaviors exists vary considerably based on the method of analysis of EMA data (Engel et al., 2013). These mixed findings result in a confusing literature regarding the degree to which restrictive eating serves an affect regulation function for individuals with AN.
There are several potential explanations for these contradictory findings. First, previous research examining an affect regulation function of restriction in AN has typically used the method of comparing the most proximal single-point ratings of affect before and after restrictive eating episodes. Although this strategy is commonly used for examining affective changes with reference to a disordered eating behavior of interest (e.g., Haedt-Matt & Keel, 2011), this approach can result in the loss of relevant data pertaining to affect changes. Most notably, this approach potentially neglects patterns of affective changes that occur over a longer period of time preceding and following a particular behavior. An alternative approach would be to repeatedly assess affect over time, incorporating all affective data points and allowing for an examination of the trajectory of affect before and after a disordered eating behavior (e.g., Engel et al., 2013). Although this type of analysis has been used to assess affect relative to binge eating and purging (Engel et al., 2013; Smyth et al., 2007), this approach has not yet been used to examine affect relative to restrictive eating.
Another consideration is that NA and PA are multifaceted, higher-order constructs that encompass multiple, lower-order emotions that may exhibit differential associations with restrictive eating. In fact, there is evidence that discrete emotions may differentially impact disordered eating in clinical populations. One study demonstrated that, among individuals with BN, changes in NA relative to binge eating and purging were driven primarily by changes in guilt as opposed to changes in fear, hostility, or sadness (Berg et al., 2013). These findings pertaining to binge eating have since been replicated in a sample of obese adults (Berg et al., 2015). Thus, examining NA and PA more broadly may mask the effects of particular lower-order dimensions of emotion.
A final limitation of prior studies is that most have not examined AN diagnostic subtype as a moderator of the relationship between affect and restrictive eating. Although restrictive eating is characteristic of AN independent of subtype, restriction in AN binge-eating/purging subtype (AN-BP) is often punctuated by episodes of binge eating and/or purging, while in AN restricting subtype (AN-R), restriction occurs consistently without interruption from binge eating or compensatory measures other than driven exercise (American Psychiatric Association, 2013). Given this notable difference in consumption habits, it is possible that AN subtypes differ in terms of the relationship between affect regulation strategies and eating disorder symptoms. In line with this hypothesis, prior research suggests that AN subtypes may differ in terms of emotion regulation difficulties. For instance, individuals with AN-BP appear to engage in more emotion-based impulsivity compared to individuals with AN-R (Haynos, Roberto, Martinez, Attia, & Fruzzetti, 2014; Rowsell, MacDonald, & Carter, 2016). The identification of subtype differences in affective patterns relative to restrictive eating could allow for greater clarity regarding the relationship between affect and restriction and provide critical information for treatment development (Lavender et al., 2015).
Thus, the objective of the current study was to address these limitations in an attempt to clarify and explicate the relationship between affect and restrictive eating in AN. This study was intended to expand upon prior analyses from the same data set that have produced mixed or unclear results pertaining to the affect regulation function of restrictive eating (Engel et al., 2013; Fitzsimmons-Craft et al., 2015; Haynos et al., 2015; Lavender et al., 2013). The specific aims of this analysis were to: (1) describe the trajectories of higher-order dimensions of NA and PA relative to restrictive eating episodes; (2) examine whether the trajectories of lower-order dimensions of NA (i.e., Fear and Guilt) and PA (i.e., Joviality and Self-Assurance) differed relative to restrictive eating episodes; and (3) determine whether AN subtype moderated the trajectories of higher- and lower-order dimensions of NA and PA relative to restrictive eating episodes.
Methods
Participants
Participants were 118 adult females who met criteria for threshold or sub-threshold AN, including both subtypes (AN-R and AN-BP). The Diagnostic and Statistical Manual of Mental Disorders 4th Edition (DSM-IV; American Psychiatric Association, 1994) criteria for AN were used and sub-threshold AN was defined as meeting all DSM-IV criteria for AN with the following exceptions: (1) body mass index of 17.6 to 18.5 kg/m2; (2) not meeting the amenorrhea criterion; or (3) not meeting the body image disturbance and intense fear of weight gain criteria. In prior examinations of these data, full- and sub-threshold AN participants did not differ significantly on most baseline measures of eating disorder pathology and comorbid psychological concerns (Le Grange et al., 2013).
Assessments
Diagnosis and Subtype
The Structured Clinical Interview for DSM-IV Axis-I Disorders, Patient Edition (SCID-I/P; First, Spitzer, Gibbon, & Williams, 1995) is a semi-structured interview to assess Axis-I psychiatric disorders. The SCID-I/P was used to establish DSM-IV diagnoses of full- and sub-threshold AN and to establish AN subtype. Interviews were recorded and a second independent assessor rated eating disorder diagnoses in a random sample of 25% of these interviews. Interrater reliability for current AN diagnosis based on a kappa coefficient was .93.
PA and NA
Items from the Positive and Negative Affect Schedule- Expanded Form (PANAS-X; Watson et al., 1988; Watson & Clark, 1994) were used to assess affect in the present moment. The PANAS-X in its original form consists of 60 items designed to capture two higher-order dimensions of affect (i.e., positive and negative), four specific lower-order dimensions of NA (i.e., Fear, Guilt, Hostility, and Sadness), and three specific lower-order dimensions of PA (i.e., Joviality, Self-Assuredness, and Attentiveness). In the current study, the items of the PANAS-X were reduced to decrease participant burden, and therefore reduce measurement error due to fatigue, over the multiple daily assessments required by the EMA procedures. The mood items used in this study were selected to represent each of the original subscales and were designated based on high factor loadings and theoretical relevance to AN. Eight items were used to measure NA (nervous, disgusted, distressed, ashamed, angry at self, afraid, sad, dissatisfied with self) and eight items were used to measure PA (strong, enthusiastic, proud, attentive, happy, energetic, confident, cheerful). Participants were asked to rate each of these items based on their current mood on a 5-point scale ranging from 1 = not at all to 5 = extremely. Alpha coefficients were .94 for NA and .92 for PA. Four lower-order dimensions of affect (Fear, Guilt, Joviality, and Self-Assurance) derived from the higher-order NA and PA dimensions were tested for inclusion in the current analyses. Other lower-order dimensions (i.e., Hostility, Sadness, and Attentiveness) associated with the PANAS-X could not be tested in the current sample due to there being too few items (< 3) available by which to construct these subscales.
Restrictive Eating
Participants were asked to report all episodes of eating and to indicate whether the episode was a snack, meal, or an unusually large amount of food. Participants were also asked to indicate (through an answer of “yes” or “no”) whether any of the following restrictive eating behaviors had taken place: (1) “I limited calories”; (2) “I limited fat grams”; (3) “I limited carbs”; and (4) “I ate as little as possible”. There is no widely accepted measure of restrictive eating and behaviors that constitute restrictive eating can vary considerably (Haynos & Fruzzetti, 2015). However, for the current analyses, restrictive eating episodes were defined as any eating episode during which an individual endorsed “I ate as little as possible”. This definition was chosen for consistency with prior analyses and because this item was more highly correlated with end of day measures of restrictive eating than any other restriction item or the combination of all four restriction items (Fitzsimmons-Craft et al., 2015)1.
Procedures
Participants were recruited at three sites (Fargo, Minneapolis, Chicago). Study approval was obtained from the institutional review board at each site. Potential participants were initially screened via phone and eligible individuals attended a meeting at which they received information regarding the study and provided informed consent. After this informational meeting, interested participants were scheduled for two assessment visits during which a physical examination and laboratory tests were conducted to ensure medical stability and the SCID-1/P (First et al., 1995) was conducted to confirm eligibility.
Participants were trained on the use of the palmtop computers at the end of the first visit. Participants participated in two practice days to gain familiarity with EMA methods and to minimize reactivity to recording procedures (these data were not used in analyses). Participants were then instructed to complete EMA recordings over the next two weeks. Attempts were made to schedule two to three visits for each participant during this two-week interval to obtain recorded data and minimize data lost as the result of technical problems. Participants were given feedback about their compliance rates at each visit. Participants were compensated $100/week for completing EMA recordings and were given a $50 bonus for a compliance rate of ≥ 80% to random signals.
The EMA protocol implemented three types of daily self-report methods (Wheeler & Reis, 1991). Two of these methods (i.e., event-contingent and signal-contingent recording) were used to assess restrictive eating episodes and affect. With regard to event-contingent recordings, participants were asked to complete recordings immediately following the occurrence of eating episodes and disordered eating behaviors. With regard to signal-contingent recordings, participants were signaled at six semi-random times throughout the day to complete recordings of mood and eating behaviors. Signal times were determined by selecting “anchor points” that subdivided the day into six roughly equivalent time blocks and then randomly distributing signal times in a normal distribution around each anchor point using a standard deviation of 30 minutes to provide assessments evenly across waking hours of the day. When signaled, participants were asked to rate their mood and report any recent behaviors not yet recorded or that they had forgotten to report during an event-contingent recording. This study also utilized interval-contingent recordings, in which participants were asked to complete EMA ratings at the end of each day; however, none of these ratings were used in the current analysis.
Statistical Analysis
All data analyses were conducted using IBM SPSS Version 21.
Confirmation of PANAS Lower-Order Dimension Structure
A multi-level confirmatory factor analysis (CFA) with random intercept was performed with EMA data to evaluate the factor structure of the lower-order dimensions of the PANAS in this sample. We expected a four-factor solution consistent with the dimensions specified by the PANAS-X (i.e., Fear, Guilt, Joviality, Self-Assurance; Watson et al., 1988; Watson & Clark, 1994). However, in line with previous analyses conducted in samples with disordered eating (Berg et al., 2013; 2015), we expected the item “disgusted” to load onto the Guilt factor. Model fit was evaluated using the confirmatory fit index (CFI), the Tucker–Lewis index (TLI), the root-mean-square error of approximation (RMSEA), and the standard root-mean-square residual (SRMR).
Within-Day Analyses
To examine the temporal relationship between affect and restrictive eating, we simultaneously modeled the pre- and post- event trajectories of higher-order dimensions of NA and PA, as well as lower-order dimensions of Fear, Guilt, Joviality, and Self-Assurance, separately using piecewise linear, quadratic, and cubic functions centered on the time at which the restrictive eating episodes occurred. Multilevel modeling is ideal for trajectory analyses because of its tolerance for data that is missing or unbalanced (i.e., differing numbers of observations over time), due to the use of maximum likelihood analysis methods. Therefore, this method allowed for an analysis of affective changes over time relative to restrictive eating, despite each restrictive episode differing in number of antecedent and consequent observations of affect.
All multilevel models included the following predictors: (1) linear functions, which reflected rate of change in affect prior to and following restrictive eating behaviors; (2) quadratic functions, which reflected the acceleration or deceleration in rate of affect change prior to and following restrictive eating behaviors; (3) and cubic functions, which reflected either further acceleration or deceleration in rate of affect change. For the analyses involving the lower-order dimensions of affect, these within-day analyses were repeated as described above, this time examining each lower-order dimension individually while controlling for the alternate dimension of the same valence (i.e., Guilt modeled controlling for Fear and vice versa; Joviality modeled controlling for Self-Assurance and vice versa) to further examine the unique effects of each lower-order dimension. For analyses examining AN subtype as a moderator of higher- and lower- order affect trajectories, the analyses outlined above were conducted with the addition of the following variables: (1) AN subtype; (2) AN subtype x linear time interactions; (3) AN subtype x quadratic time interactions; and (3) AN subtype x cubic time interactions. For all analyses and consistent with previous studies (e.g., Berg et al., 2013), when more than one restrictive eating episode was reported in a single day, only the first episode of the day was used to avoid confounding the relationship between antecedent and consequent affect ratings in relation to the multiple restrictive eating episodes within a day. Additionally, if subsequent restrictive eating episodes occurred within four hours following the first episode, only affect ratings made after the first restrictive eating episode and prior to the subsequent restrictive eating episode were included in the consequent analyses.
Results
Sample Characteristics
Half of the participants (n = 59) met threshold and half (n = 59) met subthreshold criteria for AN. Participants’ ages ranged from 18 to 58 years (M = 25.33, SD = 8.35 years). Mean BMI was 17.15 kg/m2 (SD = 1.04; range = 13.39 –18.55 kg/m2). Seventy-three (61.9%) of the participants were diagnosed with AN-R and 45 (38.1%) with AN-BP. Across the sample, 709 episodes of restrictive eating were reported, with an average of 6.01 (SD = 6.80) restrictive eating episodes endorsed per participant over the two-week recording period. Frequency of restrictive eating did not significantly differ between individuals with AN-R (M = 5.36, SD = 6.97) and AN-BP (M = 7.06, SD = 6.45), t(116) = 1.33, p = .19. A total of 1685 antecedent affect ratings (M = 7.07, SD = 3.76, Range = 1 to 22) and 1767 consequent affect ratings (M = 1.71, SD = 3.08, Range = 0 to 16) were reported relative to restrictive eating episodes.
Confirmation of PANAS Lower-Order Dimension Structure
The CFA indicated that the best-fitting model was a four-factor solution (RMSEA = .02; CFI = .97; TLI = .97; SRMR within = .03; SRMR between = .04). The four lower-order dimensions of affect were derived as follows: Fear (afraid, nervous, shaky), Guilt (ashamed, dissatisfied with self, angry with self, disgusted), Joviality (happy, cheerful, enthusiastic, energetic), and Self-Assurance (strong, proud, confident). The internal consistencies of the scales based on the alpha coefficient were .86 (Fear), .93 (Guilt), .91 (Joviality), and .83 (Self-Assurance).
Trajectories of Higher-Order Dimensions of NA and PA Relative to Restrictive Eating
As highlighted in Table 1, there were no significant changes in higher-order dimensions of NA or PA either before or after restrictive eating episodes.
Table 1.
Within-Day Multilevel Models of Higher-order Dimensions of Affect Surrounding Restrictive Eating Episodes
| Global Negative Affect | Global Positive Affect | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model/variables | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t | |
| Excluding subtype interactions | |||||||||
| Intercept | 18.97 | 0.56 | 17.86, 20.09 | 33.61*** | 17.74 | 0.48 | 16.78, 18.68 | 36.83*** | |
| Hours prior to event | 0.08 | 0.05 | −0.02, 0.17 | 1.63 | 0.02 | 0.04 | −0.07, 0.10 | 0.42 | |
| (Hours prior to event)2 | −0.002 | 0.002 | −0.01, 0.002 | −1.02 | −0.0001 | 0.002 | −0.004, 0.004 | −0.05 | |
| (Hours prior to event)3 | 0.0004 | 0.0003 | −0.0001, 0.001 | 1.21 | −0.001 | 0.0003 | −0.001, 0.0001 | −2.35* | |
| Hours following event | −0.29 | 0.15 | −0.59, 0.02 | −1.86 | 0.05 | 0.14 | −0.23, 0.32 | 0.33 | |
| (Hours following event)2 | 0.05 | 0.03 | −0.002, −0.10 | 1.88 | −0.02 | 0.02 | −0.07, 0.02 | −0.76 | |
| (Hours following event)3 | −0.002 | 0.001 | −0.01, 0.0001 | −1.87 | 0.001 | 0.001 | −0.002, 0.003 | 0.71 | |
| Including subtype interactions | |||||||||
| Intercept | 20.43 | 0.82 | 18.81, 22.04 | 24.94*** | 17.79 | 0.72 | 16.38, 19.20 | 24.86*** | |
| Subtype | −2.73 | 1.11 | −4.92, −0.53 | −2.45* | −0.10 | 0.97 | −2.01, 1.82 | −0.10 | |
| Hours prior to event | 0.05 | 0.07 | −0.10, 0.19 | 0.62 | 0.14 | 0.07 | 0.01, 0.27 | 2.14* | |
| (Hours prior to event)2 | −0.001 | 0.0003 | −0.01. 0.01 | −0.34 | 0.004 | 0.003 | −0.001, 0.01 | 1.47 | |
| (Hours prior to event)3 | 0.001 | 0.001 | −0.001, 0.001 | 0.95 | −0.001 | 0.0004 | −0.002, −0.001 | −3.02** | |
| Hours following event | −0.20 | 0.24 | −0.67, 0.26 | −0.85 | −0.18 | 0.22 | −0.60, 0.25 | −0.82 | |
| (Hours following event)2 | 0.06 | 0.04 | −0.02, 0.14 | 1.55 | −0.02 | 0.04 | −0.09, 0.05 | −0.51 | |
| (Hours following event)3 | −0.004 | 0.002 | −0.01, 0.0004 | −1.78 | 0.001 | 0.002 | −0.002, 0.01 | 0.77 | |
| Subtype*Hours prior to event | 0.03 | 0.10 | −0.14, 0.25 | 0.55 | −0.22 | 0.09 | −0.40, −0.05 | −2.53* | |
| Subtype*(Hours prior to event)2 | −0.002 | 0.01 | −0.01, 0.01 | −0.49 | −0.01 | 0.004 | −0.02, −0.001 | −2.09* | |
| Subtype*(Hours prior to event)3 | −0.0001 | 0.001 | −0.001, 0.001 | −0.16 | 0.001 | 0.001 | 0.00003, 0.002 | 2.03* | |
| Subtype*Hours following event | −0.14 | 0.31 | −0.75, 0.48 | −0.43 | 0.39 | 0.28 | −0.17, 0.95 | 1.37 | |
| Subtype*(Hours
following event)2 |
−0.03 | 0.05 | −0.13, 0.08 | −0.51 | 0.004 | 0.05 | −0.09, 0.10 | 0.09 | |
| Subtype*(Hours
following event)3 |
0.002 | 0.003 | −0.003, 0.01 | 0.81 | −0.001 | 0.002 | −0.01, 0.004 | −0.48 | |
p < .05,
p < .01
p < .001
Trajectories of Lower-Order Dimensions of NA and PA Relative to Restrictive Eating
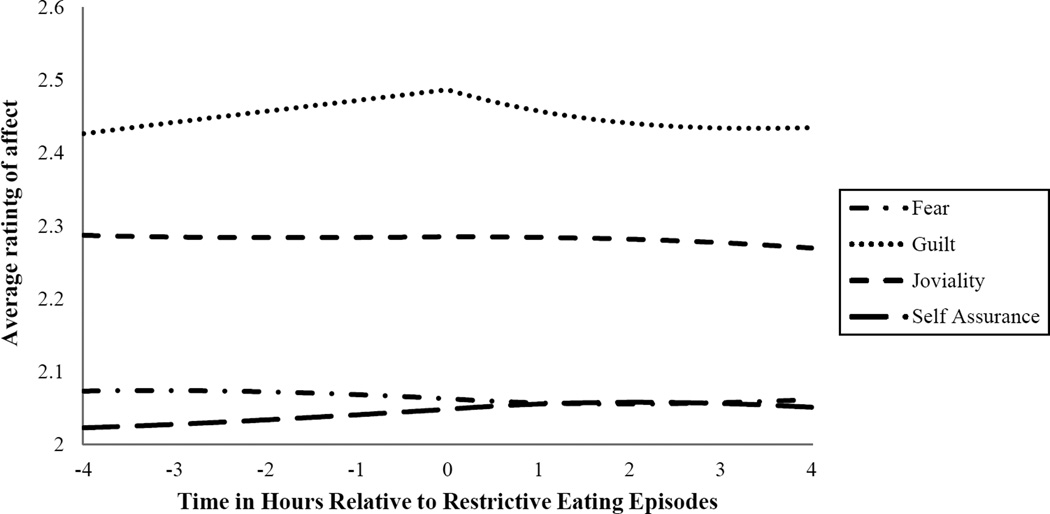
The results of the within-day analyses for the lower-order dimensions of NA and PA are provided in Table 2 and illustrated in Figure 1. There were significant changes in the Guilt trajectories anchored on the time at which a restrictive eating episode occurred both on the antecedent and consequent ends of the trajectory (ps < .05), suggesting that, across the sample, Guilt significantly increased in a consistent, linear manner in the hours prior to a restrictive eating episode and significantly decreased according to a curvilinear pattern, representing more rapid affect decrease immediately following the restrictive episode and less dramatic decreases in affect in the more distal hours following a restrictive eating episode. These results remained significant after controlling for Fear in the model.
Table 2.
Within-Day Multilevel Models of Lower-order Dimensions of Affect Surrounding Restrictive Eating Episodes
| Fear |
Guilt |
Joviality |
Self-assurance |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model/variables | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t |
| Excluding subtype interactions | ||||||||||||||||
| Intercept | 6.19 | 0.21 | 5.78, 6.60 | 29.74*** | 9.95 | 0.32 | 9.33, 10.57 | 31.50*** | 9.14 | 0.26 | 8.64, 9.64 | 35.87*** | 6.15 | 0.19 | 5.77, 6.52 | 32.30*** |
| Hours prior to event | −0.02 | 0.02 | −0.05, 0.02 | −1.07 | 0.06 | 0.03 | 0.01, 0.11 | 2.20* | 0.004 | 0.03 | −0.05, 0.05 | 0.17 | 0.02 | 0.02 | −0.01, 0.06 | 1.33 |
| (Hours prior to event)2 | −0.002 | 0.001 | −0.004, −0.001 | −2.48* | 0.001 | 0.001 | −0.002, 0.003 | 0.55 | 0.0003 | 0.0002 | −0.001, 0.003 | 0.25 | 0.0002 | 0.0001 | −0.001, 0.002 | 0.26 |
| (Hours prior to event)3 | 0.0002 | 0.001 | −0.004, 0.001 | 1.66 | 0.0002 | 0.0002 | −0.0001, 0.001 | 1.27 | −0.0003 | 0.0002 | −0.001, 0.000002 |
−1.97* | −0.0002 | 0.0001 | −0.001, -0.00002 |
−2.25* |
| Hours following event | −0.01 | 0.06 | −0.12, 0.11 | −0.11 | −0.21 | 0.09 | −0.38, −0.03 | −2.34* | −0.004 | 0.08 | −0.17, 0.16 | −0.05 | 0.01 | 0.06 | −0.10, 0.12 | 0.12 |
| (Hours following event)2 | 0.01 | 0.01 | −0.01, 0.03 | 1.09 | 0.03 | 0.02 | 0.003, 0.06 | 2.16* | −0.003 | 0.01 | −0.03, 0.02 | −0.24 | −0.01 | 0.01 | −0.03, 0.01 | −0.90 |
| (Hours following event)3 | −0.001 | 0.001 | −0.002, 0.0002 | −1.50 | −0.002 | 0.001 | −0.003, -0.0001 |
−2.15* | −0.000002 | 0.001 | −0.001, 0.001 | −0.003 | 0.001 | 0.001 | −0.0004, 0.002 | 1.20 |
| Including subtype interactions | ||||||||||||||||
| Intercept | 6.76 | 0.30 | 6.16, 7.35 | 22.42*** | 10.73 | 0.46 | 9.82, 11.63 | 23.35*** | 9.19 | 0.38 | 8.44, 9.94 | 24.22*** | 6.20 | 0.28 | 5.64, 6.76 | 21.97*** |
| Subtype | −1.06 | 0.41 | −1.89, −0.25 | −2.59* | −1.46 | 0.62 | −2.69,-0.23 | −2.34* | −0.09 | 0.51 | −1.11, 0.92 | −0.18 | −0.10 | 0.38 | −0.85, 0.66 | −0.25 |
| Hours prior to event | −0.04 | 0.03 | −0.09, 0.02 | −1.29 | 0.04 | 0.04 | −0.05, 0.12 | 0.85 | 0.07 | 0.04 | −0.001, 0.15 | 1.93 | 0.06 | 0.03 | 0.01, 0.11 | 2.30* |
| (Hours prior to event)2 | −0.002 | 0.001 | −0.004, 0.001 | −1.48 | 0.001 | 0.002 | −0.003, 0.005 | 0.50 | 0.004 | 0.002 | 0.0001, 0.01 | 1.99* | 0.002 | 0.001 | −0.001, 0.004 | 1.50 |
| (Hours prior to event)3 | 0.0003 | 0.0002 | −0.0001, 0.001 | 1.59 | 0.0003 | 0.0003 | −0.0002, 0.001 | 1.19 | −0.001 | 0.0003 | −0.001, −0.0002 | −2.84** | −0.0004 | 0.0002 | −0.001, -0.00001 |
−2.04* |
| Hours following event | −0.01 | 0.09 | −0.18, 0.16 | −0.14 | −0.08 | 0.14 | −0.35, 0.18 | −0.61 | −0.08 | 0.13 | −0.32, 0.17 | −0.63 | −0.14 | 0.09 | −0.31, 0.03 | −1.63 |
| (Hours following event)2 | 0.03 | 0.02 | −0.004, 0.06 | 1.72 | 0.03 | 0.02 | −0.02, 0.07 | 1.11 | −0.01 | 0.02 | −0.06, 0.03 | −0.66 | 0.01 | 0.02 | −0.02, 0.04 | 0.48 |
| (Hours following event)3 | −0.002 | 0.001 | −0.003, −0.0004 | −2.44* | −0.002 | 0.001 | −0.004, 0.001 | −1.34 | 0.001 | 0.001 | −0.001, 0.003 | 0.84 | −0.0002 | 0.001 | −0.002, 0.001 | −0.21 |
| Subtype*Hours prior to event | 0.03 | 0.04 | −0.04, 0.10 | 0.75 | 0.04 | 0.06 | −0.07, 0.15 | 0.76 | −0.13 | 0.05 | −0.23, −0.03 | −2.48* | −0.07 | 0.04 | −0.14,-0.0004 | −1.97* |
| Subtype*(Hours prior to event)2 | −0.0004 | 0.002 | −0.004, 0.003 | −0.26 | −0.001 | 0.003 | −0.01, 0.01 | −0.18 | −0.01 | 0.002 | −0.01, −0.001 | −2.52* | −0.003 | 0.002 | −0.01, 0.0003 | −1.81 |
| Subtype*(Hours prior to event)3 | −0.0002 | 0.0002 | −0.001, 0.0003 | −0.64 | −0.0002 | 0.0004 | −0.001, 0.001 | −0.44 | 0.001 | 0.0003 | 0.0001, 0.001 | 2.13* | 0.0002 | 0.0002 | −0.0002, 0.001 | 0.90 |
| Subtype*Hours following event | 0.01 | 0.12 | −0.22, 0.23 | 0.07 | −0.21 | 0.18 | −0.56, 0.14 | −1.17 | 0.14 | 0.17 | −0.19, 0.46 | 0.83 | 0.26 | 0.11 | 0.03, 0.48 | 2.26* |
| Subtype*(Hours following event)2 | −0.03 | 0.02 | −0.06, 0.01 | −1.36 | 0.01 | 0.03 | −0.05, 0.07 | 0.30 | 0.02 | 0.03 | −0.04, 0.08 | 0.72 | −0.03 | 0.02 | −0.06, 0.01 | −1.34 |
| Subtype*(Hours following event)3 | 0.002 | 0.001 | 0.00002, 0.004 | 1.98* | 0.00002 | 0.002 | −0.003, 0.003 | 0.01 | −0.002 | 0.001 | −0.004, 0.001 | −1.16 | 0.001 | 0.001 | −0.001, 0.003 | 1.23 |
p < .05
p < .01
p < .001
Figure 1.
Lower-order Dimensions of Affect over Time Relative to Restrictive Eating Episodes
In the original model, there were no significant changes in affect trajectories either before or after restrictive eating episodes for Fear. However, when these analyses were repeated controlling for Guilt, the antecedent affect trajectory was significant for Fear (linear model: Estimate = - .04, SE = .02, p = .01; quadratic model: Estimate = - .002, SE = .001, p = .001; cubic model: Estimate = .00001, SE = .0001, p = .27), suggesting that Fear significantly decreased in a curvilinear manner prior to restrictive eating episodes across the sample. The consequent trajectory for Fear remained non-significant even after controlling for Guilt. There were no significant changes in affect trajectories for Joviality or Self-Assurance relative to restrictive eating in the models with or without the alternate lower-order dimension entered as a covariate.
AN Subtype as a Moderator of NA and PA Relative to Restrictive Eating
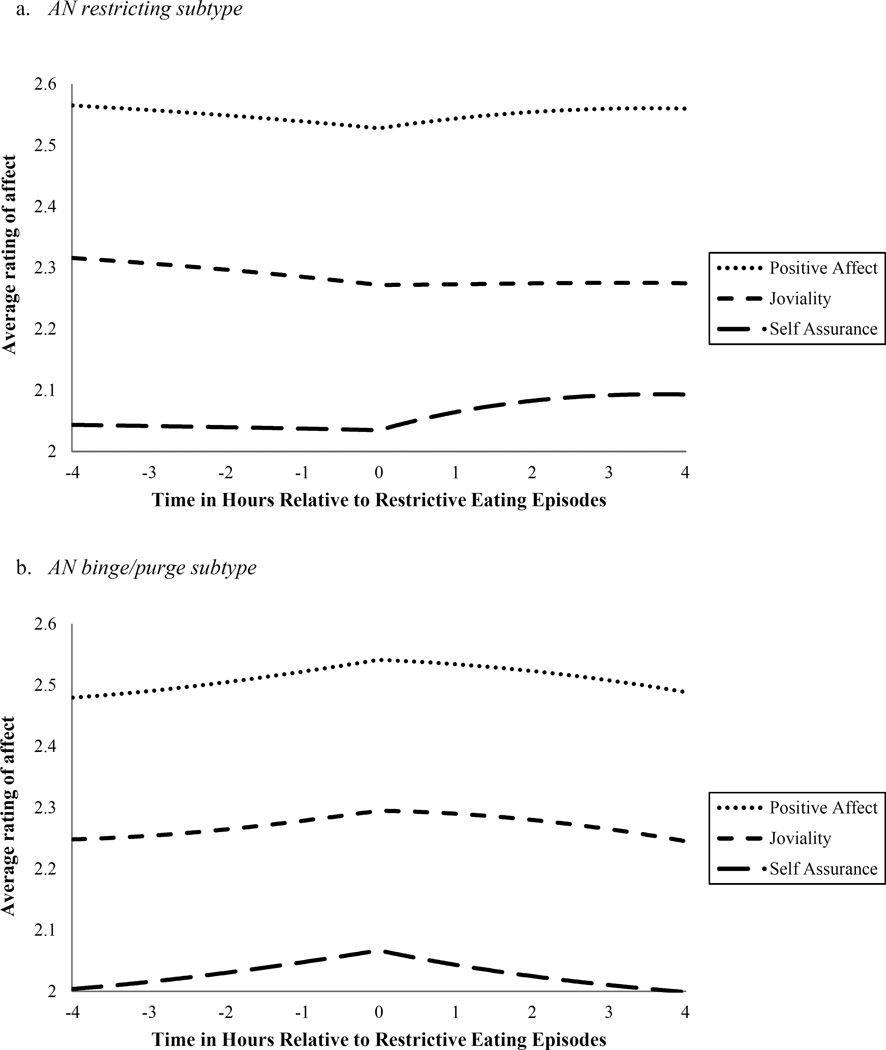
With regard to the higher-order dimension of NA, the main effect for subtype was significant (p = .02), indicating that individuals with AN-BP reported greater NA across time compared to individuals with AN-R (See Table 1). However, subtype did not significantly moderate the trajectories of NA relative to restrictive eating episodes. With regard to the higher-order dimension of PA, there was a significant time by subtype interaction for the antecedent model (ps < .05). Specifically, for individuals with AN-R, PA decreased in a significant curvilinear pattern prior to a restrictive eating episode (ps < .05), which represented more accelerated PA decreases in the time most proximal to restrictive eating. In contrast, for individuals with AN-BP, PA increased in a significant curvilinear pattern prior to a restrictive eating episode (linear model: p = .03; quadratic model: p = .14; cubic model: p = .003), which represented more accelerated PA increases in the time most proximal to restrictive eating. Subtype did not significantly moderate the consequent trajectory of PA (see Figure 2).
Figure 2.
Anorexia Nervosa (AN) Subtype as a Moderator of Positive Affect over Time Relative to Restrictive Eating Episodes
With regard to Fear and Guilt, the main effect of subtype was significant (ps < .05), such that individuals with AN-BP reported greater Fear and Guilt across time compared to individuals with AN-R (See Table 2). However, subtype did not significantly moderate the trajectories of Fear and Guilt relative to restrictive eating episodes. With regard to Joviality, there was a significant time by subtype interaction for the antecedent model (ps < .05). As highlighted in Figure 2, for individuals with AN-R, Joviality decreased in a significant curvilinear pattern prior to a restrictive eating episode (ps < .05), which represented more accelerated decreases in Joviality in the time most proximal to restrictive eating. In contrast, for individuals with AN-BP, Joviality trended towards increasing in a curvilinear pattern prior to a restrictive eating episode (linear model: p = .05; quadratic model: p = .05; cubic model: p = .01), representing more accelerated increases in Joviality in the time most proximal to restrictive eating. With regard to Self-Assurance, there were significant linear time by subtype interactions for both the antecedent (p = .049) and consequent (p = .02) models. As highlighted in Figure 2, for individuals with AN-R, the linear time model for Self-Assurance decreased significantly prior to a restrictive episode (p = .049) and increased significantly following a restrictive eating episode (p = .02), indicating steady rates of change in Self-Assurance before and after engaging in restriction. For individuals with AN-BP, the linear time model for Self-Assurance increased significantly prior to a restrictive eating episode (p = .02), indicating a consistent antecedent rate of increase in this facet, but did not change significantly following a restrictive episode (p = .10).
Discussion
The objective of the current study was to further explicate whether a functional relationship between affect and restrictive eating exists in AN using momentary, naturalistic data. Our first two study aims were to examine the trajectories of the higher- and lower-order dimensions of NA and PA relative to restrictive eating episodes among women with AN. Although higher-order dimensions of NA and PA did not change significantly before or after restrictive episodes across the group, Guilt increased significantly prior to restrictive eating episodes and decreased significantly following restrictive eating episodes. These findings suggest that restrictive eating may function to specifically regulate guilt among individuals with AN, thus adding to a growing body of evidence supporting an affect regulation model of AN (Haynos & Fruzzetti, 2011).
This study is the first to implicate a functional relationship between any dimension of NA (i.e., Guilt) and restrictive eating. These data could indicate that prior analyses not finding a clear relationship between NA and restrictive eating may have been limited by examining comparisons of single proximal ratings of affect and by investigating affect at the composite level, rather than at the level of specific lower-order dimensions of emotion. This finding is also consistent with two prior studies, which found that the lower-order dimension of Guilt drove affective changes relative to binge eating in individuals with bulimia nervosa (Berg et al., 2013) and obesity (Berg et al., 2015). As previously noted (Berg et al., 2013; 2015), the items in the Guilt scale utilized in this study may be more reflective of the construct of shame (i.e., negative evaluation of one’s self) than guilt (i.e., negative evaluation of one’s behavior) per se. Thus, this study adds to a literature suggesting that eating disordered behaviors may function to specifically regulate guilt or shame, regardless of the behavior or eating disorder diagnosis. Unexpectedly, after controlling for Guilt, the lower-order dimension of Fear significantly decreased in the hours prior to restrictive eating episodes. This finding may be accounted for by individuals with AN experiencing a decrease in fear by planning for restrictive eating episodes or, alternatively, could suggest that individuals with AN are more inclined to engage in eating episodes (restrictive or otherwise) when fear is lower. In either case, these findings suggest that guilt/shame and fear function differently in the context of restrictive eating. Thus, examining NA in composite can result in a misinterpretation of the role of NA in relation to restrictive eating.
The mechanism by which restrictive eating mitigates guilt among individuals with AN remains unknown. Some initial research indicates that individuals with eating disorders may experience disorder-specific guilt related to eating and body weight and shape (Burney & Irwin, 2000; Troop & Redshaw, 2012) resulting from an internalized thin-ideal weight standard (Stice, 2002). Therefore, restrictive eating may function to regulate disorder-specific guilt by promoting thinness-related objectives. Alternatively, feelings of guilt and shame may be more generalized among individuals with eating disorders (Keith, Gillanders, & Simpson, 2009). In this case, restrictive eating may reduce guilt through another process, such as enhancing an overall sense of self-control or achievement. Further, restrictive eating may produce physiological changes that serve to numb or dampen the experience of guilt (Kaye, Wierenga, Bailer, Simmons, & Bischoff-Grethe, 2013). Additional research is needed in order to better understand how restrictive eating might reduce guilt among individuals with AN.
Our third aim was to explore AN subtype as a moderator of the trajectories of higher- and lower-order dimensions of affect relative to restrictive eating episodes. In this sample, the association between PA and restrictive eating differed according to AN subtype; however, the association between NA and restrictive eating did not. Whereas individuals with AN-R experienced significant decreases in PA, Joviality, and Self-Assurance prior to restrictive eating episodes and significant increases in Self-Assurance following restrictive eating episodes, individuals with AN-BP experienced significant increases in PA and Self-Assurance (and trending increases in Joviality) prior to restrictive eating episodes, but no change in PA indices following restrictive eating episodes. These results indicate that, although restriction may function to mitigate guilt across individuals with AN, regardless of subtype, restriction may function to enhance aspects of PA only among individuals with AN-R. The possibility that restrictive eating is maintained through a dual process of emotion-based negative reinforcement and positive reinforcement among individuals with AN-R may provide insight into why these individuals are able to persist in restrictive behavior so remarkably.
It is unclear why individuals with AN-R may experience increases in self-assurance following restrictive eating. One potential explanation is that these individuals may over-generalize thinness expectancies, such that they believe thinness will have broad positive effects on multiple life domains (Fischer, Settles, Collins, Gunn, & Smith, 2012). Therefore, restrictive eating may enhance self-assurance through promotion of thinness-related goals. Another possibility is that restrictive eating may promote more generalized enhancement of positive self-reference due to an achievement of self-control or perfectionistic standards (Culbert et al., 2015; Fairburn, Shafran, & Cooper, 1999), which may be more compelling among this group. The association between PA and restrictive eating demonstrated by individuals with AN-BP, in which higher- and lower-order dimensions of PA increased prior to restriction, but did not change following restriction, also warrants consideration. This pattern suggests that restriction itself is not clearly rewarding in the sense of generating PA for this subgroup of individuals with AN. One potential interpretation of this finding is that individuals with AN-BP may receive positive reinforcement to a greater degree by planning to restrict prior to the restrictive episode, rather than by the restrictive episode itself. This potential difference in the timing of reinforcement may be due in part to the punctuated pattern of restriction characterizing AN-BP, versus the consistent pattern found in AN-R. The findings regarding subtype differences in PA trajectories suggest that further research on the role of PA and AN subtypes is needed in studies examining affect regulation processes in AN.
It is also worth noting that this study specifically examined the function of restrictive eating among individuals with AN. However, restrictive eating is common among individuals with other eating disorders (Elran-Barak et al., 2015), as well as non-clinical samples (Haynos & Fruzzetti, 2011). However, this study does not provide information about whether restrictive eating would function similarly for individuals without a diagnosis of AN. Further investigation is warranted to examine whether the relationship between restrictive eating and guilt and self-assurance extends to populations beyond AN.
There are important clinical implications related to the study findings. First, these findings suggest that, in treatment for AN, targeting affect regulation may be effective in reducing restrictive eating. There is early support for AN treatments that target emotion management (e.g., Chen et al., 2015; Lynch et al., 2013; Wildes, Marcus, Cheng, McCabe, & Gaskill, 2014). The findings of this study suggest that continued research on such treatments is warranted. Additionally, these results indicate that, for individuals with AN-R, a focus on increasing positive experiences, especially those that promote a sense of self-assurance, may assist in replacing one function of restrictive eating and, therefore, decreasing a reliance on such behavior. There are existing treatments (Hayes, Strosahl, & Wilson, 1999; Jacobson, Martell, & Dimidjian, 2001) that specifically aim to assist patients in obtaining healthy sources of positive reinforcement either through pleasant events or long-term values-guided behavior. There is also some initial support for interventions incorporating such approaches into the treatment of AN (Berman, Boutelle, & Crow, 2009; Juarascio et al., 2013; Timko, Zucker, Herbert, Rodriguez, & Merwin, 2015). Additionally, since Guilt and Self-Assurance emerged as the most prominent lower-order dimensions of affect maintaining restrictive eating, emotions of self-reference may be particularly relevant to restrictive eating. Thus, a specific focus on assisting individuals in managing affective responses related to self-concept may be especially appropriate in the treatment of AN. Finally, this study, taken together with prior studies (Berg et al., 2013; 2015), provides some evidence that several disordered eating behaviors may serve similar functions across diagnostic groups. Therefore, treatment approaches targeting common processes, such as guilt or shame, could have a positive impact on a variety of maladaptive behaviors among different patient groups.
There are notable strengths of this study. The first strength is the use of EMA, which allows measurement in real-time (decreasing retrospective recall biases) and within real-world settings (increasing ecological validity). Further, EMA allows for an examination of the temporal relationship between variables, promoting a greater ability to examine issues related to functionality. In addition, examination of affect trajectories relative to restrictive eating that comprise a number of data points over a period of time allowed for a potentially more thorough and precise measurement of affect patterns before and after restriction than a single-point comparison approach. Similarly, use of multilevel modeling for examination of affect trajectories was well suited for EMA data because this method was tolerant of unbalanced affect ratings before and after restrictive eating episodes. Further, the sample size was large for a study of individuals with AN, and therefore included a large number of restrictive eating episodes, providing adequate power for examining moderators of the relationship between affect and restrictive eating.
However, there are also limitations to this study. Although the study utilized a previously validated methodology for assessing restrictive eating episodes (Fitzsimmons-Craft et al., 2015), it is notoriously difficult to identify methods of assessing restrictive eating that correspond with objective caloric intake (Stice, Cooper, Schoeller, Tappe, & Lowe, 2007). Further, individuals with AN have been found to overestimate caloric consumption (Sysko, Walsh, Schebendach, & Wilson, 2005); therefore, there may be other eating episodes in this study not coded as restrictive eating that would constitute restriction by behavioral criteria. The self-report of affect may also be limited because research indicates that individuals with AN have difficulty accurately reporting their emotional experiences (Haynos & Fruzzetti, 2011). However, the results of this study suggest the affect ratings had predictive validity, increasing confidence in self-report of these indices.
There are other limitations related to the measurement of affect trajectories that warrant consideration. Both the higher- and lower- order dimensions of affect were measured using shortened versions of the original subscales. Although there is a precedent for use of abbreviated subscales (Berg et al., 2013; 2015) and the structure of the lower-order dimensions was established using CFA, it remains possible that this approach introduced error. Related, potentially relevant lower-order dimensions of affect (e.g., Sadness, Hostility, Attentiveness) were not assessed, limiting the ability to draw conclusions about the role of other dimensions of affect relative to restrictive eating. Further, on average, a greater number of affect ratings comprised the antecedent curves (M = 7.07) than the consequent curves (M = 1.71). Although multilevel modeling is well suited to manage unbalanced data, this may have resulted in relatively lesser ability to detect significant consequent changes relative to restrictive eating. Finally, while the timing and repeated measurement of EMA methodology allows greater ability to infer functional relationships between variables, these data are still correlational in nature and, therefore, cannot definitely establish causality. Future research ought to examine trajectories of affect relative to restrictive eating utilizing more objective measures of restrictive eating (e.g., test meal intake) and affect (e.g., physiological measures), novel affective dimensions, and experimental manipulations of affect.
The results of this study demonstrate that, although examination of trajectories of higher-order dimensions of NA and PA across individuals with AN does not provide evidence for an affect regulation function of restriction, examination of trajectories separated by specific lower-order dimensions of affect and differentiated by AN subtype does support an affect regulation model of restriction. Specifically, these analyses indicate that restrictive eating may be maintained across individuals with AN through negative reinforcement associated with reducing guilt/shame, and for individuals with AN-R through positive reinforcement associated with enhancing of self-assurance. This study adds to literature suggesting that the core symptoms of AN may serve to manage affective experiences and provides additional evidence suggesting the utility of treatments targeting affect regulation within this population.
Acknowledgments
This work was supported by grants P30DK050456 from the National Institute of Diabetes and Digestive and Kidney Diseases, grants R01MH059674 and T32MH082761 from the National Institute of Mental Health, and the Neuropsychiatric Research Institute. The hypotheses and results of this study have been previously presented at the 2016 Academy for Eating Disorders annual conference in San Francisco, CA.
Footnotes
Of note, in contrast to a prior study utilizing “I ate as little as possible” as the operational definition for restrictive eating (Fitzsimmons-Craft et al., 2015), the current study did not exclude two cases in which the participant reported both “I ate as little as possible” and “I ate an excessive amount of food” at the same assessment point. These cases were considered to reflect situations in which excessive eating occurred within close proximity to restrictive eating. Therefore, these episodes were believed to be important to include in order to investigate subtype differences in the relationship between affect and restrictive eating.
References
- Ackard DM, Cronemeyer CL, Richter S, Egan A. Do symptom-specific stages of change predict eating disorder treatment outcome? Eating and Weight Disorders. 2015;20:49–62. doi: 10.1007/s40519-014-0153-0. [DOI] [PubMed] [Google Scholar]
- Affenito SG, Dohm FA, Crawford PB, Daniels SR, Striegel-Moore RH. Macronutrient intake in anorexia nervosa: The National Heart, Lung, and Blood Institute Growth and Health Study. The Journal of Pediatrics. 2002;141:701–705. doi: 10.1067/mpd.2002.129840. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- Anderson LM, Crow SJ, Peterson CB. The impact of meal consumption on emotion among individuals with eating disorders. Eating and Weight Disorders. 2014;19:347–354. doi: 10.1007/s40519-013-0084-1. [DOI] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, et al. Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders. 2015;48:641–653. doi: 10.1002/eat.22401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, et al. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. Journal of Abnormal Psychology. 2013;122:111–118. doi: 10.1037/a0029703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman MI, Boutelle KN, Crow SJ. A case series investigating acceptance and commitment therapy as a treatment for previously treated, unremitted patients with anorexia nervosa. Europeam Eating Disorder Review. 2009;17:426–434. doi: 10.1002/erv.962. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Bulik CM, Brownley KA, Lohr KN, Sedway JA, Rooks A, et al. Management of eating disorders. Evidence Report/Technology Assessment (Full Report) 2006;135:1–166. [PMC free article] [PubMed] [Google Scholar]
- Braun DL, Sunday SR, Halmi KA. Psychiatric comorbidity in patients with eating disorders. Psychological Medicine. 1994;24:859–867. doi: 10.1017/s0033291700028956. [DOI] [PubMed] [Google Scholar]
- Burney J, Irwin HJ. Shame and guilt in women with eating-disorder symptomatology. Journal of Clinical Psychology. 2000;56:51–61. doi: 10.1002/(sici)1097-4679(200001)56:1<51::aid-jclp5>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Cardi V, Esposito M, Clarke A, Schifano S, Treasure J. The impact of induced positive mood on symptomatic behaviour in eating disorders. An experimental, AB/BA crossover design testing a multimodal presentation during a test-meal. Appetite. 2015;87:192–198. doi: 10.1016/j.appet.2014.12.224. [DOI] [PubMed] [Google Scholar]
- Chen EY, Segal K, Weissman J, Zeffiro TA, Gallop R, Linehan MM, et al. Adapting dialectical behavior therapy for outpatient adult anorexia nervosa--a pilot study. International Journal of Eating Disorders. 2015;48:123–132. doi: 10.1002/eat.22360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, et al. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Elran-Barak R, Sztainer M, Goldschmidt AB, Crow SJ, Peterson CB, Hill LL, et al. Dietary restriction behaviors and binge eating in anorexia nervosa, bulimia nervosa and binge eating disorder: Trans-diagnostic examination of the restraint model. Eating Behaviors. 2015;18:192–196. doi: 10.1016/j.eatbeh.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow S, Peterson CB, et al. The role of affect in the maintenance of anorexia nervosa: evidence from a naturalistic assessment of momentary behaviors and emotion. Journal of Abnormal Psychology. 2013;122:709–719. doi: 10.1037/a0034010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Shafran R, Cooper Z. A cognitive behavioural theory of anorexia nervosa. Behavior Research and Therapy. 1999;37:1–13. doi: 10.1016/s0005-7967(98)00102-8. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM–IV Axis I Disorders: Patient Edition (SCIDI/P) New York, NY: Biometrics; 1995. [Google Scholar]
- Fitzsimmons-Craft EE, Accurso EC, Ciao AC, Crosby RD, Cao L, Pisetsky EM, et al. Restrictive eating in anorexia nervosa: Examining maintenance and consequences in the natural environment. International Journal of Eating Disorders. 2016;48:923–931. doi: 10.1002/eat.22439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and Commitment Therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Haynos AF, Crosby RD, Engel SG, Lavender JM, Wonderlich SA, Mitchell JE, et al. Initial test of an emotional avoidance model of restriction in anorexia nervosa using ecological momentary assessment. Journal of Psychiatry Research. 2015;68:134–139. doi: 10.1016/j.jpsychires.2015.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynos AF, Fruzzetti AE. Anorexia nervosa as a disorder of emotion dysregulation: Theory, evidence, and treatment implications. Clinical Psychology: Science and Practice. 2011;18:183–202. [Google Scholar]
- Haynos AF, Roberto CA, Martinez MA, Attia E, Fruzzetti AE. Emotion regulation difficulties in anorexia nervosa before and after inpatient weight restoration. International Journal of Eating Disorders. 2014;47:888–891. doi: 10.1002/eat.22265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice. 2001;8:255–270. [Google Scholar]
- Juarascio A, Shaw J, Forman E, Timko CA, Herbert J, Butryn M, et al. Acceptance and commitment therapy as a novel treatment for eating disorders: an initial test of efficacy and mediation. Behavior Modification. 2013;37:459–489. doi: 10.1177/0145445513478633. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Wierenga CE, Bailer UF, Simmons AN, Bischoff-Grethe A. Nothing tastes as good as skinny feels: the neurobiology of anorexia nervosa. Trends in Neurosciences. 2013;36:110–120. doi: 10.1016/j.tins.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keith L, Gillanders D, Simpson S. An exploration of the main sources of shame in an eating-disordered population. Clinical Psychology and Psychotherapy. 2009;16:317–327. doi: 10.1002/cpp.629. [DOI] [PubMed] [Google Scholar]
- Lavender JM, De Young KP, Anestis MD, Wonderlich SA, Crosby RD, Engel SG, et al. Associations between retrospective versus ecological momentary assessment measures of emotion and eating disorder symptoms in anorexia nervosa. Journal of Psychiatric Research. 2013;47:1514–1520. doi: 10.1016/j.jpsychires.2013.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Crosby RD, Engel SG, Cao L, Ndungu A, Crow SJ, et al. DSM-IV-defined anorexia nervosa versus subthreshold anorexia nervosa (EDNOS-AN) European Eating Disorder Review. 2013;21:1–7. doi: 10.1002/erv.2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR, Gray KL, Hempel RJ, Titley M, Chen EY, O’Mahen HA. Radically open-dialectical behavior therapy for adult anorexia nervosa: feasibility and outcomes from an inpatient program. BMC Psychiatry. 2013;13:293. doi: 10.1186/1471-244X-13-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer LES, Schebendach J, Bodell LP, Shingleton RM, Walsh BT. Eating behavior in anorexia nervosa: before and after treatment. International Journal of Eating Disorders. 2012;45:290–293. doi: 10.1002/eat.20924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Current Opinions is Psychiatry. 2006;19:438–443. doi: 10.1097/01.yco.0000228768.79097.3e. [DOI] [PubMed] [Google Scholar]
- Pike K. Long-term course of anorexia nervosa: response, relapse, remission, and recovery. Clinical Psychology Review. 1997;18:447–475. doi: 10.1016/s0272-7358(98)00014-2. [DOI] [PubMed] [Google Scholar]
- Rowsell M, MacDonald DE, Carter JC. Emotion regulation difficulties in anorexia nervosa: associations with improvements in eating psychopathology. Journal of Eating Disorders. 2016;4:17. doi: 10.1186/s40337-016-0108-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schebendach J, Mayer LES, Devlin MJ, Attia E, Walsh BT. Dietary energy density and diet variety as risk factors for relapse in anorexia nervosa: A replication. International Journal of Eating Disorders. 2012;45:79–84. doi: 10.1002/eat.20922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Stice E, Cooper JA, Schoeller DA, Tappe K, Lowe MR. Are dietary restraint scales valid measures of moderate- to long-term dietary restriction? Objective biological and behavioral data suggest not. Psychological Assessment. 2007;19:449–458. doi: 10.1037/1040-3590.19.4.449. [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh BT, Schebendach J, Wilson GT. Eating behavior among women with anorexia nervosa. Am J Clin Nutr. 2005;82:296–301. doi: 10.1093/ajcn.82.2.296. [DOI] [PubMed] [Google Scholar]
- Timko CA, Zucker NL, Herbert JD, Rodriguez D, Merwin RM. An open trial of Acceptance-based Separated Family Treatment (ASFT) for adolescents with anorexia nervosa. Behaviour Research and Therapy. 2015;69:63–74. doi: 10.1016/j.brat.2015.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troop NA, Redshaw C. General shame and bodily shame in eating disorders: a 2.5-year longitudinal study. European Eating Disorder Review. 2012;20:373–378. doi: 10.1002/erv.2160. [DOI] [PubMed] [Google Scholar]
- Walsh BT. The enigmatic persistence of anorexia nervosa. American Journal of Psychiatry. 2013;170:477–484. doi: 10.1176/appi.ajp.2012.12081074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA. The PANAS-X: Manual for the positive and negative affect schedule- Expanded form. The University of Iowa; 1994. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. [Google Scholar]
- Wildes JE, Marcus MD, Bright AC, Dapelo MM. Emotion and eating disorder symptoms in patients with anorexia nervosa: an experimental study. International Journal of Eating Disorders. 2012;45:876–882. doi: 10.1002/eat.22020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Marcus MD, Cheng Y, McCabe EB, Gaskill JA. Emotion acceptance behavior therapy for anorexia nervosa: a pilot study. International Journal of Eating Disorders. 2014;47:870–873. doi: 10.1002/eat.22241. [DOI] [PMC free article] [PubMed] [Google Scholar]