Abstract
Purpose
The aim of our study was to investigate gender differences in factors related to prehospital delay and identify whether the knowledge of acute myocardial infarction symptoms affects this delay in Korean patients with ST-elevation myocardial infarction (STEMI).
Materials and Methods
A total of 350 patients (286 men, 64 women) with confirmed STEMI were interviewed to investigate socio-demographics, history of disease, symptom onset time, and factors that contributed to delayed decision time in seeking treatment and hospital arrival time from symptom onset. Factors associated with prehospital delay were examined separately by gender using univariate and multivariate analyses.
Results
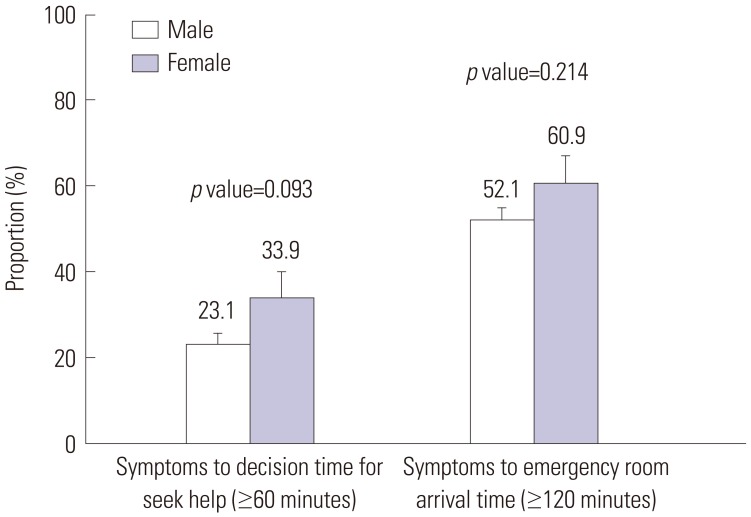
Female patients had higher proportions of ≥60-minute decision time and ≥120-minute arrival time compared to male patients (33.9% vs. 23.1%, 60.9% vs. 52.1%, respectively). However, the difference was not statistically significant (p=0.093 and 0.214, respectively). Previous cardiovascular disease (CVD) was associated with increased decision time in men, whereas, in women, lower educational status caused a greater delay in decision time. Factors associated with hospital arrival time excluding delayed decision time were referral from another hospital, previous CVD, and percutaneous coronary intervention in men, and referral from another hospital in women.
Conclusion
Gender differences exist in factors related to prehospital delay. Therefore, public education to reduce prehospital delay should be conducted according to gender with a focus on the pertinent factors.
Keywords: Acute coronary syndrome, healthcare timeout, sex differences
INTRODUCTION
Prompt reperfusion therapy, including percutaneous coronary intervention (PCI) and fibrinolytic therapy in patients with ST-segment elevation myocardial infarction (STEMI) is very important. Because prompt salvaging of the critical myocardium as much as possible improves patient survival rates or outcomes,1,2,3 effort is expended to reduce symptom onset-to-hospital arrival time (prehospital time) and door to needle time (hospital time, i.e., from presentation to treatment).
There are many factors affecting prehospital delay, which comprised of patient delay (decision time) and transport delay. Identification of factors influencing the delays may help reduce the time to receive treatment. Numerous studies on the factors related to prehospital delay in patients with acute myocardial infarction (AMI) have been conducted in many countries.4,5,6,7,8,9 However, few studies involving Korean patients with AMI have been conducted.10,11
Previous studies identified several major categories that might predict prehospital delay, such as socio-demographic factors, context at symptom onset, and clinical, cognitive, and behavioral factors.12,13,14 Among these factors, a significant cognitive factor known to be related to decision time delay is knowledge or recognition of AMI symptoms. Symptoms are a core element of a patient's decision to seek help, and have a decisive effect on the correct triage, thus affecting the decisions regarding additional early medical intervention.15 Moreover, there may be gender differences regarding time to seek medical care. Several studies have reported that women are more likely to experience longer delays than men.4,16,17 However, other studies have suggested that there are no gender differences in prehospital time delay.18,19 Thus, the relationship between gender and prehospital delay times in AMI is currently unclear, partially because of the differences in design and methodology in the studies.
Outcomes in women such as early death occur more frequently than in men; additionally, in-hospital and overall mortality after AMI is higher in women than in men.20 Thus, we believe that the reason for the higher mortality in women is a difference in prehospital delay, and it is important to identify the gender-related factors related to prehospital delay.
Consequently, the objective of this study was to investigate gender differences in factors related to prehospital delay, and to identify whether knowledge of AMI symptoms affects the delay in Korean patients with STEMI.
MATERIALS AND METHODS
Study participants
The participants were patients hospitalized with STEMI at 6 PCI-capable tertiary hospitals in various regions of Korea from July 2014 to June 2015.
Inclusion criteria for the present study were: 1) final diagnosis of STEMI, 2) hospitalization within 72 hours after the onset of symptoms, 3) hemodynamic stability (stable blood pressure and consistent blood flow), 4) Korean native speaker, and 5) mental alertness (information communicated through conversation). Among 359 patients with STEMI who were consecutively admitted during the data collection period, 350 (286 men and 64 women) were finally included in this study. Participants were selected using an electronic medical recoding system and then interviewed face-to-face after obtaining consent and agreeing to be in the study. The interview was conducted in the education room of the cardiac ward, and took less than 20 minutes. The survey was completed within 3 days after admission to the hospital.
At each hospital, the study design and protocol were approved by the Institutional Review Board (IRB) before data collection, and the IRB of Seoul National University approved the present study.
Questionnaire and data collection
The investigator developed a special questionnaire for this study in collaboration with several cardiologists, which was pre-tested on patients with STEMI and subsequently modified. The final questionnaire comprised 5 domains including: 1) sociodemographic characteristics, 2) history of disease, 3) symptoms and awareness of AMI, 4) patient decision time, and 5) transport-related items.
More detailed items on the questionnaire, which were collected by interview after admission, were as follows: sociodemographic characteristics such as age (categorized as <60 and ≥60 years when analysis), gender, education level (categorized as ≤middle school and ≥high school), medical insurance status (national health insurance and Medicaid), residence (urban and rural), whether the patient lived alone or not, and health behavior (smoking status, alcohol use, and obesity).
Moreover, data regarding disease history [family history of cardiovascular diseases (CVD) and personal history of hypertension, diabetes mellitus, dyslipidemia, CVD, PCI, or stroke] were collected.
Information on symptoms and quality of symptoms included the chief complaint, accompanying symptoms, and onset time during the acute phase of STEMI. Patients were questioned on the 10 symptoms using a Yes/No format. These symptoms included the following: 1) chest pain, 2) radiating pain, 3) dyspnea, 4) sweating, 5) weakness, 6) indigestion, 7) nausea or vomiting, 8) dizziness, 9) palpitations, and 10) other (an option to write in the symptom). During analysis, these symptoms were categorized into two groups such as “chest pain” and “other symptoms” as a major symptom. Awareness of AMI symptoms was asked using the following question: “Did you usually know the AMI disease” and “Did you usually know the early symptoms of AMI”; patients answered “Yes” or “No” to these questions. Additionally, patients who answered “Yes” were asked about the following symptoms, consisting of 5 dichotomous Yes/No items: chest pain, radiating pain, dyspnea, sweating, and weakness/dizziness. When patients answered more than 3 symptoms correctly, we determined that the patient had knowledge of AMI symptoms.
Transport-related items comprised the use of emergency medical service (EMS) and whether the patient arrived directly at the hospital. These items were investigated using the medical record systems.
Prehospital delay was divided into patient decision time and arrival time. Patient decision time is the elapsed time from symptom onset to the decision to seek medical care or call EMS. We obtained the symptom onset time and decision time to seek medical care via interview. We then calculated the decision time and categorized the times as <60 minutes and ≥60 minutes during analysis. The arrival time is the elapsed time from symptom onset to arrival at the emergency room (ER). We investigated arrival time at the ER through the hospital medical record system. Based on this time, we calculated the time from symptom onset to ER arrival and categorized it to <120 minutes and ≥120 minutes.
Statistical analysis
Fisher's exact test was performed to compare the difference between male and female patients based on socio-demographic characteristics, clinical history, knowledge of AMI, decision time, and arrival to ER time.
In men and women, separate univariate logistic regression analyses were performed to calculate the odds ratio (OR) and to confirm factors related to the decision time (<60 minutes vs. ≥60 minutes). After that, by gender, multivariate logistic regression analyses were performed to confirm factors related to the decision time after adjustment. For the selection of variables for adjustment, when the p value was less than 0.20 in the univariate logistic regression analysis, the variables were included for the adjustment. Additionally, we included the known risk factors (age, education level, medical insurance, living with others, history of hypertension, diabetes mellitus, previous CVD and PCI, symptoms onset time, knowledge of disease and symptoms for AMI, and major symptoms) and considered the affected decision time and arrival time for the adjustment in multivariate logistic model. Using modeling in the multivariate logistic analysis, the multicollinearity between risk factors was confirmed by correlation coefficient between the risk factors. If the correlation coefficient was more than 0.8, we omitted the risk factor in the model. We conducted the same analysis to confirm the factors related to arrival in ER time (<120 and ≥120 minutes) in both genders. All analyses were performed using IBM SPSS Statistics for Window version 20 (IBM Corp., Armonk, NY, USA). The statistical significance level (α) was set at 0.05.
RESULTS
Characteristics of men and women
Among patients with STEMI, 286 (81.7%) were men and 64 (18.3%) were women. Patient characteristics are shown in Table 1. Many differences in socio-demographic, clinical history, and knowledge of disease characteristics between genders were seen.
Table 1. Socio-Demographic, Clinical History and Knowledge Characteristics of Participants between Male and Female.
| Variables | Male (n=286) | Female (n=64) | p value |
|---|---|---|---|
| Age, mean (±SD) | 59.2 (±11.9) | 71.1 (±11.5) | <0.001 |
| <60 yr | 152 (53.1) | 12 (18.8) | <0.001 |
| ≥60 yr | 134 (46.9) | 52 (81.2) | |
| Education level, n (%) | <0.001 | ||
| <Middle school | 83 (30.2) | 42 (79.2) | |
| ≥Middle school | 192 (69.8) | 11 (20.8) | |
| Medical insurance status, n (%) | 0.746 | ||
| National Health Insurance | 272 (95.1) | 62 (96.9) | |
| Medicaid | 14 (4.9) | 2 (3.1) | |
| Residency region, n (%) | 0.849 | ||
| Urban | 243 (85.0) | 54 (84.4) | |
| Rural | 43 (15.0) | 10 (15.6) | |
| Living with others, n (%) | 0.023 | ||
| Alone | 31 (10.9) | 14 (21.9) | |
| With family | 254 (89.1) | 50 (78.1) | |
| Smoking status, n (%) | <0.001 | ||
| Non-smoker | 49 (17.1) | 63 (98.4) | |
| Current or past smoker | 237 (82.9) | 1 (1.6) | |
| Alcohol use status, n (%) | <0.001 | ||
| Non-drinker | 83 (29.0) | 42 (65.6) | |
| Current drinker | 203 (71.0) | 22 (34.4) | |
| Body mass index, n (%) | 0.003 | ||
| <25.0 kg/m2 | 165 (57.7) | 50 (78.1) | |
| ≥25.0 kg/m2 | 121 (42.3) | 14 (21.9) | |
| Family history of CVD, n (%) | 134 (46.9) | 17 (26.6) | 0.003 |
| Hypertension, n (%) | 104 (36.4) | 38 (59.4) | 0.001 |
| Diabetes mellitus, n (%) | 71 (24.8) | 19 (29.7) | 0.431 |
| Dyslipidemia, n (%) | 35 (12.2) | 11 (17.2) | 0.307 |
| Previous CVD, n (%) | 46 (16.1) | 18 (28.1) | 0.031 |
| Previous PCI, n (%) | 23 (8.0) | 7 (10.9) | 0.460 |
| Previous stroke, n (%) | 13 (4.6) | 5 (7.8) | 0.343 |
| Symptoms onset time, n (%) | 0.256 | ||
| Weekday and day (8 am–6 pm) | 106 (37.1) | 29 (45.3) | |
| Weekend or night (6 pm–8 am) | 180 (62.9) | 35 (54.7) | |
| Knowledge of disease for AMI, n (%) | 0.049 | ||
| Did not known | 84 (33.7) | 28 (48.3) | |
| Known | 165 (66.3) | 30 (51.7) | |
| Knowledge of symptoms for AMI, n (%) | <0.001 | ||
| Did not known | 170 (67.5) | 53 (89.8) | |
| Known | 82 (32.5) | 6 (10.2) | |
| Major symptom, chest pain, n (%) | 1.000 | ||
| Chest pain | 246 (86.0) | 55 (85.9) | |
| Other symptoms | 40 (14.0) | 9 (14.1) | |
| Use of EMS, n (%) | 0.886 | ||
| Did not used | 175 (61.8) | 40 (63.5) | |
| Used | 108 (38.2) | 23 (36.5) | |
| Referral hospital, n (%) | 0.324 | ||
| Did not referred | 120 (42.0) | 22 (34.4) | |
| Referred | 166 (58.0) | 42 (65.6) | |
| Decision time,* minute | 0.712 | ||
| Mean (±SD) | 49.4 (±85.2) | 59.2 (±95.6) | |
| Median (Min–Max) | 25.0 (5.0–720.0) | 20.0 (10.0–480.0) | |
| Arrival time,† minute | 0.041 | ||
| Mean (±SD) | 251.6 (±435.2) | 438.7 (±706.2) | |
| Median (Min–Max) | 124.5 (10.0–3138) | 171.0 (17.0–1814) |
SD, standard deviation; CVD, cardiovascular disease; PCI, percutaneous coronary intervention; AMI, acute myocardial infarction; EMS, emergency medical service.
*Decision time: the time of symptom onset to decision seek help, †Arrival time: the time of symptom onset to emergency room visiting.
The mean age of male patients was 59.2 years, which was less than the 71.1 years of the female patients (p<0.001). Additionally, the proportion of men with greater than middle school education was higher than that of women. Moreover, the proportion of men who lived with family was greater than that of women. The proportion of patients with body mass index (BMI) >25.0 kg/m2, family history of CVD, hypertension, and previous CVD was greater in male than in female patients (all has statistically significant level).
Differences in prehospital delay between men and women
A total of 23.1% of the male patients and 33.9% of the female patients decided to seek medical assistance at a hospital ≥60 minutes after symptom onset. Moreover, it took more than 120 minutes for 52.1% and 60.9% of the male and female patients, respectively, to arrive at the ER after symptom onset. Although both percentages were lower in male patients, no statistically significant difference was observed between the two genders (p=0.093 and 0.214, respectively) (Fig. 1).
Fig. 1. Proportion for patients of the ≥60 minutes of symptoms to decision seek help time and the ≥120 minutes of symptoms to emergency room arrival time between male and female. Error bars on the bar chart is standard error.
Factors associated with a prolonged delay in deciding to seek medical assistance at a hospital
Factors that led to the decision to seek medical assistance at a hospital were separately analyzed for male and female patients using univariate and multivariate logistic regression. In univariate logistic regression for male patients, the OR for a delay ≥60 minutes in deciding to seek medical assistance at a hospital was higher in those with dyslipidemia and those with a history of CVD {2.24 [95% confidence interval (CI), 1.03–4.90] and 2.66 [95% CI, 1.00–7.09], respectively}. A multivariate logistic regression was subsequently conducted with these and other variables (age, educational level, medical insurance, living with others, smoking status, hypertension, diabetes mellitus, dyslipidemia, previous CVD and PCI, symptom onset time, knowledge of disease and symptoms for AMI, and major symptoms) showing a high significance, albeit not statistical significance, as covariates. The OR for a delay ≥60 minutes in deciding to seek medical assistance at a hospital was high [4.86 (95% CI, 1.13–28.74)] in patients with a history of CVD (Table 2).
Table 2. Related Factors on Time from Symptom Onset to Seek Medical Care in Male and Female by Univariate and Multivariate Logistic Regression Analysis.
| Variables | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|
| Crude OR | p value | Adjusted OR | p value | Crude OR | p value | Adjusted OR | p value | |
| Age, more than 60 yr | 1.10 (0.62–1.95) | 0.744 | 0.89 (0.43–1.87) | 0.766 | 0.65 (0.18–2.42) | 0.525 | 4.40 (0.60–48.07) | 0.123 |
| Education level, ≤middle school | 1.62 (0.88–3.01) | 0.124 | 0.79 (0.37–1.72) | 0.555 | 9.44 (1.09–81.88) | 0.042 | 33.28 (3.78–293.04) | 0.011 |
| Medical insurance, Medicaid | 1.69 (0.36–7.84) | 0.503 | 0.73 (0.13–4.10) | 0.718 | - | - | - | - |
| Residency region, rural | 1.47 (0.70–3.09) | 0.310 | - | - | 1.65 (0.30–9.06) | 0.567 | - | - |
| Living with others, alone | 0.89 (0.34–2.31) | 0.815 | 0.75 (0.22–2.62) | 0.656 | 0.73 (0.18–2.96) | 0.655 | 0.83 (0.10–7.22) | 0.867 |
| Smoking status, current/past smoker | 1.89 (0.80–4.47) | 0.146 | 2.18 (0.83–5.68) | 0.113 | - | - | - | - |
| Alcohol use status, current drinker | 1.07 (0.58–2.01) | 0.821 | - | - | 0.76 (0.23–2.45) | 0.644 | - | - |
| Body mass index, ≥25.0 kg/m2 | 0.74 (0.41–1.33) | 0.313 | - | - | 0.83 (0.22–3.15) | 0.784 | - | - |
| Family history of CVD, yes | 0.91 (0.51–1.61) | 0.745 | - | - | 1.25 (0.37–4.18) | 0.721 | - | - |
| Hypertension, yes | 1.18 (0.65–2.13) | 0.594 | 0.90 (0.42–1.93) | 0.795 | 0.49 (0.16–1.50) | 0.211 | 0.10 (0.01–0.83) | 0.033 |
| Diabetes mellitus, yes | 1.84 (0.99–3.44) | 0.055 | 2.05 (0.93–4.54) | 0.076 | 0.84 (0.24–2.92) | 0.789 | 3.39 (0.41–27.80) | 0.256 |
| Dyslipidemia, yes | 2.24 (1.03–4.90) | 0.043 | 1.73 (0.70–4.26) | 0.232 | 1.14 (0.29–4.52) | 0.849 | - | - |
| Previous CVD, yes | 2.66 (1.00–7.09) | 0.050 | 4.86 (1.13–28.74) | 0.032 | 1.18 (0.34–4.10) | 0.789 | 1.01 (0.07–13.55) | 0.996 |
| Previous PCI, yes | 0.29 (0.07–1.29) | 0.105 | 1.27 (0.10–16.50) | 0.854 | 0.75 (0.13–4.30) | 0.750 | 17.96 (0.20–165.02) | 0.211 |
| Previous stroke, yes | 0.97 (0.20–4.78) | 0.966 | - | - | 0.63 (0.06–6.50) | 0.698 | - | - |
| Symptoms onset time, | 1.59 (0.86–2.94) | 0.143 | 1.68 (0.83–3.42) | 0.151 | 0.85 (0.28–2.57) | 0.769 | 0.31 (0.05–2.12) | 0.232 |
| Knowledge of disease for AMI, did not known | 1.12 (0.59–2.14) | 0.731 | 1.08 (0.46–2.50) | 0.866 | 1.56 (0.50–4.88) | 0.442 | 0.69 (0.11–4.21) | 0.685 |
| Knowledge of symptoms for AMI, did not known | 0.97 (0.52–1.84) | 0.937 | 0.76 (0.34–1.69) | 0.501 | 2.12 (0.22–20.55) | 0.515 | 5.76 (0.65–512.54) | 0.770 |
| Major symptom, chest pain | 1.02 (0.44–2.37) | 0.970 | 0.73 (0.27–1.99) | 0.538 | 2.81 (0.30–25.98) | 0.362 | 0.26 (0.01–5.73) | 0.393 |
OR, odds ratio; CVD, cardiovascular disease; PCI, percutaneous coronary intervention; AMI, acute myocardial infarction.
In the univariate analysis for female patients, the OR for a delay ≥60 minutes in deciding to seek medical assistance at a hospital was very high [9.44 (95% CI, 1.09–81.88)] in those with low education. Moreover, after adjustment by the other variables (age, living with others, hypertension, diabetes mellitus, previous CVD and PCI, symptoms onset time, knowledge of disease and symptoms for AMI, and major symptoms), the OR for a delay ≥60 minutes in deciding to seek medical assistance at a hospital increased to 33.28 (95% CI, 3.78–293.04) in female patients with low education (Table 2). However, patients with hypertension had a shorter decision time [0.10 (95% CI, 0.01–0.83)].
Factors associated with a prolonged delay in arrival at ER
Regarding the factors that influenced the delay in arrival at the ER (‘arrival time’), the use of EMS and visits to other hospitals were included as variables, and the data for both genders were analyzed separately. In univariate analysis for male patients, those with a history of CVD, those who did not use EMS, those who visited other hospitals, and those who decided to seek medical assistance late at a hospital presented at the ER later. A multivariate analysis was conducted with these variables, age, education level, medical insurance, place of residence, living with others, drinking status, hypertension, diabetes mellitus, previous history of PCI, symptom onset time, knowledge of disease and symptoms for AMI, and major symptoms as covariates. The OR of arriving at the ER ≥120 minutes after symptom onset was 7.25 (95% CI, 1.69–31.12) in those with history of CVD, 7.25 (95% CI, 1.17–44.97) in those with a history of PCI, 4.02 (95% CI, 1.89–8.56) in those who visited other hospitals, and 74.82 (95% CI, 17.98–311.38) in those who made late decisions (Table 3).
Table 3. Related Factors on Time form Symptom Onset to Emergency Room Arrival in Male and Female by Univariate and Multivariate Logistic Regression Analysis.
| Variables | Female | Female | ||||||
|---|---|---|---|---|---|---|---|---|
| Crude OR | p value | Adjusted OR | p value | Crude OR | p value | Adjusted OR | p value | |
| Age, more than 60 yr | 1.27 (0.79–2.02) | 0.321 | 2.04 (0.94–4.45) | 0.073 | 4.12 (1.09–15.61) | 0.037 | 2.88 (0.80–10.43) | 0.107 |
| Education level, ≤middle school | 1.22 (0.73–2.04) | 0.455 | 0.98 (0.45–2.13) | 0.958 | 8.53 (1.89–38.43) | 0.005 | 5.65 (0.99–23.69) | 0.062 |
| Medical insurance, Medicaid | 1.70 (0.55–5.20) | 0.354 | 2.71 (0.48–15.36) | 0.259 | - | - | - | - |
| Residency region, rural | 1.67 (0.86–3.26) | 0.130 | 1.87 (0.74–4.76) | 0.188 | 2.97 (0.58–15.31) | 0.194 | 2.97 (0.58–15.31) | 0.194 |
| Living with others, alone | 1.51 (0.70–3.24) | 0.290 | 1.63 (0.52–5.10) | 0.403 | 1.20 (0.35–4.11) | 0.772 | 0.83 (0.24–2.85) | 0.772 |
| Smoking status, current/past smoker | 0.86 (0.47–1.60) | 0.644 | - | - | - | - | - | - |
| Alcohol use status, current drinker | 1.43 (0.86–2.39) | 0.173 | 1.84 (0.86–3.96) | 0.116 | 0.37 (0.13–1.08) | 0.070 | 0.26 (0.09 –0.78) | 0.016 |
| Body mass index, ≥25.0 kg/m2 | 0.84 (0.53–1.34) | 0.467 | - | - | 0.82 (0.25–2.72) | 0.742 | - | - |
| Family history of CVD, yes | 0.96 (0.60–1.52) | 0.847 | - | - | 0.64 (0.21–1.96) | 0.432 | - | - |
| Hypertension, yes | 1.26 (0.78–2.05) | 0.348 | 0.70 (0.33–1.52) | 0.371 | 0.73 (0.26–2.05) | 0.547 | 1.01 (0.37–2.77) | 0.987 |
| Diabetes mellitus, yes | 1.46 (0.85–2.52) | 0.171 | 1.49 (0.62–3.58) | 0.377 | 1.14 (0.38–3.46) | 0.813 | 1.37 (0.46–4.13) | 0.574 |
| Dyslipidemia, yes | 0.97 (0.48–1.97) | 0.933 | - | - | 0.47 (0.13–1.73) | 0.254 | - | - |
| Previous CVD, yes | 2.61 (1.34–5.09) | 0.005 | 7.25 (1.69–31.12) | 0.008 | 1.87 (0.62–5.66) | 0.265 | 1.19 (0.39–3.68) | 0.758 |
| Previous PCI, yes | 0.69 (0.29–1.62) | 0.390 | 7.25 (1.17–44.97) | 0.033 | 0.44 (0.09–2.15) | 0.308 | 0.83 (0.17–4.07) | 0.822 |
| Previous stroke, yes | 2.12 (0.64–7.05) | 0.220 | - | - | 0.96 (0.15–6.18) | 0.964 | - | - |
| Symptoms onset time, weekend and night time | 0.80 (0.49–1.29) | 0.355 | 0.58 (0.29–1.19) | 0.137 | 0.70 (0.25–1.94) | 0.495 | 1.24 (0.46–3.35) | 0.665 |
| Knowledge of disease for AMI, did not known | 1.25 (0.74–2.13) | 0.400 | 0.89 (0.37–2.09) | 0.782 | 3.92 (1.28–12.02) | 0.017 | 1.72 (0.57–5.18) | 0.335 |
| Knowledge of symptoms for AMI, did not known | 1.15 (0.68–1.95) | 0.603 | 0.99 (0.43–2.26) | 0.979 | 3.30 (0.55–19.69) | 0.190 | 0.72 (0.19–2.69) | 0.634 |
| Major symptom, chest pain | 0.69 (0.35–1.36) | 0.283 | 0.57 (0.20–1.67) | 0.308 | 2.19 (0.53–9.09) | 0.282 | 0.52 (0.12–2.16) | 0.365 |
| Use of EMS, did not used | 1.96 (1.20–3.18) | 0.007 | 1.28 (0.61–2.68) | 0.509 | 20.40 (5.47–76.15) | 0.000 | 2.48 (0.72–8.58) | 0.152 |
| Referral hospital, referred | 3.79 (2.31–6.23) | 0.000 | 4.02 (1.89–8.56) | <0.001 | 14.45 (4.10–50.94) | 0.000 | 17.0 (4.70–61.49) | <0.001 |
| Make decision, late decision | 32.31 (9.78–106.71) | 0.000 | 74.82 (17.98–311.38) | <0.001 | 13.96 (2.79–69.77) | 0.001 | 18.9 (3.85–92.68) | 0.003 |
OR, odds ratio; CVD, cardiovascular disease; PCI, percutaneous coronary intervention; AMI, acute myocardial infarction; EMS, emergency medical service.
According to the univariate analysis conducted for female patients, factors that exerted statistically significant influences on arrival time included age, education level, place of residence, living with others, drinking status, hypertension, diabetes mellitus, history of CVD and PCI, symptoms onset time, knowledge of disease and symptoms for AMI, and major symptoms. The OR for late arrival was 5.65 (95% CI, 0.99–23.69) for patients with low education, 17.0 (95% CI, 4.70–61.49) for those who visited other hospitals, and 18.9 (95% CI, 3.85–92.68) for those who made late decisions. Those who drank alcohol arrived at the ER earlier (Table 3).
DISCUSSION
Timely reperfusion is very important for patients with myocardial infarction. Therefore, patients should arrive at the hospital and receive treatment as soon as possible after symptom onset. The American College of Cardiology Foundation/American Heart Association guidelines recommend that patients receive treatment within 120 minutes.21 Thus, a 120-minute “symptom onset-to-door time” duration is considered the gold standard for preventing cardiac muscle necrosis.6 However, delays in prehospital time remain common in many patients. In the present study, the time from symptom onset to the decision to seek medical assistance at a hospital exceeded 60 minutes in 23.1% of male patients and 33.9% of female patients. Moreover, the arrival time exceeded 120 minutes for 52.1% of male patients and 60.9% of female patients. Therefore, there is a need to investigate the factors influencing the time at which patients decide to seek medical assistance and arrival time at a hospital in patients with myocardial infarction. Furthermore, basic data are required to establish national policies to decrease delays. In particular, the characteristics (age at onset, symptoms, medical history, and prognosis) of AMI differ greatly between men and women,22,23,24,25 and differences in decision time or symptom onset to arrival time were also observed in certain studies;12,17,26,27,28,29 thus, separate investigations are necessary for male and female patients.
In the present study, 286 of 350 patients with myocardial infarction (81.7%) were men, while 18.3% were women. Differences were observed in socioeconomic characteristics, clinical characteristics, and knowledge of AMI. The mean age was lower and educational level was higher in male patients. The proportions of smokers and alcohol consumers, those living with family and those with a BMI ≥25 kg/m2 were also higher in male patients. Moreover, more male patients had a family history of CVD and appropriate knowledge of AMI and its symptoms. The proportion of female patients with history of CVD was high. The present study did not differ considerably from previous studies in terms of patient characteristics. In most studies,16,17,30,31 the mean age and proportions of CVD history of the male patients were lower than that of female patients, while the mean education level was lower for female than for male patients.
In the present analysis, the proportion of persons who decided to seek medical assistance at a hospital ≥60 minutes after symptom onset was 10.8% higher in female than in male patients (33.9% in female patients and 23.1% in male patients). Moreover, the proportion of those who arrived at the ER ≥120 minutes after symptom onset was 8.8% higher in female than in male patients (60.9% in female patients and 52.1% in male patients). However, these differences were not statistically significant. Currently, studies have reached inconsistent conclusions regarding the time spent deciding to seek medical assistance at a hospital, arrival time, or prehospital time. Some studies concluded that there was no difference between male and female patients;19,32,33,34 whereas other studies concluded that female patients had longer delays12,26,27,28,35,36 or that the prehospital time was longer in male patients. In our study, the 10.8% and 8.8% differences in proportions between male and female patients may have been non-significant due to the small sample size. In other words, the notion that female patients tended to arrive later at hospitals appears rational.
When factors influencing the time spent deciding to seek medical assistance at a hospital in male and female patients were analyzed, male patients with a history of CVD made later decisions (OR, 4.86; decision delay ≥60 minutes). Moreover, although the differences were not statistically significant (p>0.05), male patients with diabetes and dyslipidemia tended to make decisions to seek medical assistance at a hospital later. Such findings are similar to those of the randomized clinical trial conducted by Mooney, et al.37 They divided 1944 patients who were treated for acute coronary syndrome into an intervention group receiving education and a control group (n=972 patients in each group). In the control group, the arrival time was more prolonged for recurrent episodes of acute coronary syndrome than for the initial episode. Considering the results of our study and those of the study by Mooney, et al.,37 patients who appear to be less interested in their health seem to have worse health-related behaviors. Accordingly, these people would be more susceptible to chronic diseases and myocardial infarction. In addition, these people would arrive at hospitals later when myocardial infarction symptoms appear, since they appear uninterested in their symptoms or consider them trivial. Because a recurrent infarction in patients with previous CVD may be associated with different symptoms and more tolerable pain compared to first infarction,38 education on prevention and recurrence would be necessary in male patients with chronic diseases or a history of AMI.
Among the female patients, the time spent deciding to seek medical assistance at a hospital was more prolonged in those with low education. Up to the present, studies in female patients have investigated prehospital delay times according to education level only. Moser, et al.17 found no differences by education level. However, some studies39,40,41 that did not assess male and female participants separately reported that education level exerted significant influences on the decision time to seek medical assistance at a hospital, and, as in the present study, the delay in these studies could have been further prolonged in female patients. Late decisions in poorly educated female patients may be due to aging and lack of knowledge of symptoms for AMI. In fact, in our data, poorly educated female patients were older and did not have knowledge of symptoms for AMI compared to highly educated female patients. Therefore, preventive measures and education for females should be customized appropriately for their education level.
The present study also analyzed factors influencing arrival time with some predictable outcomes. The OR for an arrival time delay ≥120 minutes was 74.82 for men who made late decisions to seek medical assistance at hospitals. Moreover, the arrival time was also prolonged when patients visited other hospitals. This is consistent with the findings of several previous studies,7,10,27,36,42 which reported that the arrival and treatment delay times are prolonged when patients visit other hospitals that are unable to treat their conditions. In contrast, the use of EMS did not exert any significant influence on arrival time (OR 1.28). This finding contradicts the findings of some previous studies,12,43 but is consistent with those of other studies.37 Since the use of EMS requires additional time to call the EMS and travel, it would not have exerted any significant influence. Particularly for those living in urban areas where the distance to hospitals is often short, the arrival time would not have been different considerably according to EMS use. Other factors that influenced arrival time included a history of CVD and PCI. These factors also influenced the time spent deciding to seek medical assistance at a hospital; in other words, they are effective modifiers of arrival time. Patients with disease histories made decisions late to seek medical assistance at a hospital, which prolongs the arrival time.
Similarly, the time spent deciding to seek medical assistance at a hospital was a factor that influenced the arrival time of female patients; late decisions resulted in late arrival at the ER. Moreover, patients arrived at the ER later when they visited other hospitals. As in male patients, arrival time was not influenced by use of the EMS. Those that consumed alcohol arrived at the hospital earlier; however, due to the small number of female patients who consumed alcohol, this finding is unreliable. Furthermore, in univariate analysis, the arrival time was prolonged in those with low education; however, in multivariate analysis, education level did not lead to any significant differences in arrival time. Since this finding is inconsistent with those of other previous studies,39,40,41 an analysis of more patients would be required to assess arrival time by education level. Nonetheless, since those with low education made decisions late to seek medical assistance at a hospital, these late decisions would have led to ER arrival delays.
Limitations
The present study has several limitations. First, symptom onset and the time spent deciding whether to seek medical assistance at a hospital, which are important variables in the present study, were recalled based on the patients' memories. Although the investigation was conducted by a professional nurse, recall bias could have been present. Second, patients who died on arrival and those who could not be interviewed because of their severity of condition were not investigated. Such fundamental limitations must be considered in the interpretation of our results. Third, a smaller number of female patients was included, considering the whole patient could have led to limited reliability. In fact, the CIs in female patients were often very wide. Furthermore, even OR values that were deemed clinically significant had no statistical significance because of the small sample size. This necessitated the interpretation of the absolute OR and CI values.
Conclusion
Despite the limitations due to the study design, the present study is significant as it addresses the need to separately analyze the decision times to seek medical assistance at a hospital and arrival times for each gender among patients with myocardial infarction. This is because myocardial infarction presents different characteristics in men and women. Moreover, since few studies have investigated Korean patients, our study's findings are even more significant and may be used to prepare national policies. Factors that influenced the time spent deciding to seek medical assistance at a hospital included CVD history in men and a lower education level in women. Visits to other hospitals influenced the arrival time for both men and women. In addition, the arrival time in men was delayed when the patients had a previous history of CVD or PCI.
These findings suggest the need to prepare appropriate education programs on preventing cardio-cerebrovascular diseases for men and women. For men, education about symptoms and the risks of complications would be required for those with chronic diseases or CVD. For women, customized education for individuals with different educational backgrounds would be required. Furthermore, for symptomatic patients to arrive as early as possible at a hospital for treatment, the contents of educational programs for the general public and emergency medical technicians should to be reinforced.
ACKNOWLEDGEMENTS
This study was supported by funding from the Ministry of Health and Welfare and six regional Cardiocerebrovascular Centers.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Bulluck H, Yellon DM, Hausenloy DJ. Reducing myocardial infarct size: challenges and future opportunities. Heart. 2016;102:341–348. doi: 10.1136/heartjnl-2015-307855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 3.Baek YS, Park SD, Kim SH, Lee MJ, Shin SH, Kim DH, et al. Clinical and angiographic predictors of microvascular dysfunction in ST-segment elevation myocardial infarction. Yonsei Med J. 2015;56:1235–1243. doi: 10.3349/ymj.2015.56.5.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3:82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, et al. Prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 6.Peng YG, Feng JJ, Guo LF, Li N, Liu WH, Li GJ, et al. Factors associated with prehospital delay in patients with ST-segment elevation acute myocardial infarction in China. Am J Emerg Med. 2014;32:349–355. doi: 10.1016/j.ajem.2013.12.053. [DOI] [PubMed] [Google Scholar]
- 7.Løvlien M, Schei B, Hole T. Prehospital delay, contributing aspects and responses to symptoms among Norwegian women and men with first time acute myocardial infarction. Eur J Cardiovasc Nurs. 2007;6:308–313. doi: 10.1016/j.ejcnurse.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Isaksson RM, Holmgren L, Lundblad D, Brulin C, Eliasson M The Northern Sweden MONICA Study. Time trends in symptoms and prehospital delay time in women vs. men with myocardial infarction over a 15-year period. Eur J Cardiovasc Nurs. 2008;7:152–158. doi: 10.1016/j.ejcnurse.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Fukuoka Y, Dracup K, Rankin SH, Froelicher ES, Kobayashi F, Hirayama H, et al. Prehospital delay and independent/interdependent construal of self among Japanese patients with acute myocardial infarction. Soc Sci Med. 2005;60:2025–2034. doi: 10.1016/j.socscimed.2004.08.053. [DOI] [PubMed] [Google Scholar]
- 10.Park YH, Kang GH, Song BG, Chun WJ, Lee JH, Hwang SY, et al. Factors related to prehospital time delay in acute ST-segment elevation myocardial infarction. J Korean Med Sci. 2012;27:864–869. doi: 10.3346/jkms.2012.27.8.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang SY, Zerwic JJ, Jeong MH. Impact of prodromal symptoms on prehospital delay in patients with first-time acute myocardial infarction in Korea. J Cardiovasc Nurs. 2011;26:194–201. doi: 10.1097/JCN.0b013e3181f3e2e0. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 13.Dracup K, Moser DK, Eisenberg M, Meischke H, Alonzo AA, Braslow A. Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med. 1995;40:379–392. doi: 10.1016/0277-9536(94)00278-2. [DOI] [PubMed] [Google Scholar]
- 14.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 15.DeVon HA, Ryan CJ, Rankin SH, Cooper BA. Classifying subgroups of patients with symptoms of acute coronary syndromes: a cluster analysis. Res Nurs Health. 2010;33:386–397. doi: 10.1002/nur.20395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meischke H, Larsen MP, Eisenberg MS. Gender differences in reported symptoms for acute myocardial infarction: impact on prehospital delay time interval. Am J Emerg Med. 1998;16:363–366. doi: 10.1016/s0735-6757(98)90128-0. [DOI] [PubMed] [Google Scholar]
- 17.Moser DK, McKinley S, Dracup K, Chung ML. Gender differences in reasons patients delay in seeking treatment for acute myocardial infarction symptoms. Patient Educ Couns. 2005;56:45–54. doi: 10.1016/j.pec.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Goff DC, Jr, Feldman HA, McGovern PG, Goldberg RJ, Simons-Morton DG, Cornell CE, et al. Rapid Early Action for Coronary Treatment (REACT) Study Group. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Am Heart J. 1999;138(6 Pt 1):1046–1057. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 20.Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, et al. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803–2810. doi: 10.1161/CIRCULATIONAHA.108.789800. [DOI] [PubMed] [Google Scholar]
- 21.American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions. O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:485–510. doi: 10.1016/j.jacc.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Rosengren A, Wallentin L, K Gitt A, Behar S, Battler A, Hasdai D. Sex, age, and clinical presentation of acute coronary syndromes. Eur Heart J. 2004;25:663–670. doi: 10.1016/j.ehj.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 23.Canto JG, Goldberg RJ, Hand MM, Bonow RO, Sopko G, Pepine CJ, et al. Symptom presentation of women with acute coronary syndromes: myth vs reality. Arch Intern Med. 2007;167:2405–2413. doi: 10.1001/archinte.167.22.2405. [DOI] [PubMed] [Google Scholar]
- 24.Hailer B, Naber C, Koslowski B, van Leeuwen P, Schäfer H, Budde T, et al. Gender-related differences in patients with ST-elevation myocardial infarction: results from the registry study of the ST elevation myocardial infarction network Essen. Clin Cardiol. 2011;34:294–301. doi: 10.1002/clc.20916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307:813–822. doi: 10.1001/jama.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walsh JC, Lynch M, Murphy AW, Daly K. Factors influencing the decision to seek treatment for symptoms of acute myocardial infarction: an evaluation of the Self-Regulatory Model of illness behaviour. J Psychosom Res. 2004;56:67–73. doi: 10.1016/S0022-3999(03)00082-5. [DOI] [PubMed] [Google Scholar]
- 27.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 28.Ting HH, Bradley EH, Wang Y, Lichtman JH, Nallamothu BK, Sullivan MD, et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–968. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKee G, Mooney M, O'Donnell S, O'Brien F, Biddle MJ, Moser DK. Multivariate analysis of predictors of pre-hospital delay in acute coronary syndrome. Int J Cardiol. 2013;168:2706–2713. doi: 10.1016/j.ijcard.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 30.Heer T, Gitt AK, Juenger C, Schiele R, Wienbergen H, Towae F, et al. Gender differences in acute non-ST-segment elevation myocardial infarction. Am J Cardiol. 2006;98:160–166. doi: 10.1016/j.amjcard.2006.01.072. [DOI] [PubMed] [Google Scholar]
- 31.Løvlien M, Schei B, Hole T. Myocardial infarction: psychosocial aspects, gender differences and impact on pre-hospital delay. J Adv Nurs. 2008;63:148–154. doi: 10.1111/j.1365-2648.2008.04654.x. [DOI] [PubMed] [Google Scholar]
- 32.Grace SL, Abbey SE, Bisaillon S, Shnek ZM, Irvine J, Stewart DE. Presentation, delay, and contraindication to thrombolytic treatment in females and males with myocardial infarction. Womens Health Issues. 2003;13:214–221. doi: 10.1016/j.whi.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 33.Dracup K, Moser DK. Beyond sociodemographics: factors influencing the decision to seek treatment for symptoms of acute myocardial infarction. Heart Lung. 1997;26:253–262. doi: 10.1016/s0147-9563(97)90082-0. [DOI] [PubMed] [Google Scholar]
- 34.McKinley S, Moser DK, Dracup K. Treatment-seeking behavior for acute myocardial infarction symptoms in North America and Australia. Heart Lung. 2000;29:237–247. doi: 10.1067/mhl.2000.106940. [DOI] [PubMed] [Google Scholar]
- 35.Heer T, Schiele R, Schneider S, Gitt AK, Wienbergen H, Gottwik M, et al. Gender differences in acute myocardial infarction in the era of reperfusion (the MITRA registry) Am J Cardiol. 2002;89:511–517. doi: 10.1016/s0002-9149(01)02289-5. [DOI] [PubMed] [Google Scholar]
- 36.O'Donnell S, Condell S, Begley C, Fitzgerald T. Prehospital care pathway delays: gender and myocardial infarction. J Adv Nurs. 2006;53:268–276. doi: 10.1111/j.1365-2648.2006.03722.x. [DOI] [PubMed] [Google Scholar]
- 37.Mooney M, McKee G, Fealy G, O'Brien F, O'Donnell S, Moser D. A randomized controlled trial to reduce prehospital delay time in patients with acute coronary syndrome (ACS) J Emerg Med. 2014;46:495–506. doi: 10.1016/j.jemermed.2013.08.114. [DOI] [PubMed] [Google Scholar]
- 38.Kirchberger I, Heier M, Golüke H, Kuch B, von Scheidt W, Peters A, et al. Mismatch of presenting symptoms at first and recurrent acute myocardial infarction. From the MONICA/KORA Myocardial Infarction Registry. Eur J Prev Cardiol. 2016;23:377–384. doi: 10.1177/2047487315588071. [DOI] [PubMed] [Google Scholar]
- 39.Zhang B, Zhang W, Huang R, Zhu H, Liu J, Jiang D, et al. Gender and age differences associated with prehospital delay in Chinese patients presenting with ST-elevation myocardial infarction. J Cardiovasc Nurs. 2016;31:142–150. doi: 10.1097/JCN.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 40.Song L, Yan HB, Yang JG, Sun YH, Hu DY. Impact of patients' symptom interpretation on care-seeking behaviors of patients with acute myocardial infarction. Chin Med J (Engl) 2010;123:1840–1845. [PubMed] [Google Scholar]
- 41.Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FA, et al. Age and sex differences and 20-year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3:590–598. doi: 10.1161/CIRCOUTCOMES.110.957878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johansson I, Strömberg A, Swahn E. Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung. 2004;33:291–300. doi: 10.1016/j.hrtlng.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 43.Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A. Pre-hospital delay in patients with acute coronary syndrome: factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs. 2009;8:26–33. doi: 10.1016/j.ejcnurse.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]