Abstract
Chronic disease rates have become more prevalent in the modern American workforce, which has negative implications for workplace productivity and healthcare costs. Offering workplace health interventions is recognized as an effective strategy to reduce chronic disease progression, absenteeism, and healthcare costs as well as improve population health. This review documents intervention and evaluation strategies used for health promotion programs delivered in workplaces. Using predetermined search terms in five online databases, we identified 1,131 published items from 1995 to 2014. Of these items, 27 peer-reviewed articles met the inclusion criteria; reporting data from completed United States-based workplace interventions that recruited at-risk employees based on their disease or disease-related risk factors. A content rubric was developed and used to catalogue these 27 published field studies. Selected workplace interventions targeted obesity (n = 13), cardiovascular diseases (n = 8), and diabetes (n = 6). Intervention strategies included instructional education/counseling (n = 20), workplace environmental change (n = 6), physical activity (n = 10), use of technology (n = 10), and incentives (n = 13). Self-reported data (n = 21), anthropometric measurements (n = 17), and laboratory tests (n = 14) were used most often in studies with outcome evaluation. This is the first literature review to focus on interventions for employees with elevated risk for chronic diseases. The review has the potential to inform future workplace health interventions by presenting strategies related to implementation and evaluation strategies in workplace settings. These strategies can help determine optimal worksite health programs based on the unique characteristics of work settings and the health risk factors of their employee populations.
Keywords: chronic disease, employee health, health intervention, intervention strategies, worksite
1. Introduction
In 2015, the Bureau of Labor statistics reported that approximately 157 million adults were in the United States (US) workforce [1]. Most employees spend more than one-third of their day at the worksite. This has resulted in a modern workforce that has become increasingly sedentary over the past 60 years [2]. Excessive sedentary behavior is an independent risk factor for multiple chronic health outcomes including cardiovascular disease, type 2 diabetes, hypertension, metabolic syndrome, and obesity [3], [4], [5]. In addition, job strain at the workplace is also associated with the development of cardiovascular disease [6]. Nearly 70% of American adults are classified as overweight or obese, and it is estimated that 133 million Americans have at least one chronic health condition [7], [8]. This high rate of chronic disease has resulted in increased mortality rates and has become a public health challenge associated with higher health care costs and decreased workplace productivity [9], [10], [11], [12].
Employers are taking an important role in providing preventive health programs to their employees [13]. More than 51% of business with more than 50 employees implemented some type of wellness program in 2013 [14]. Employers are in a position to support employee health through the implementation of different types of worksite interventions that focus on nutrition, physical activity, disease management, or worksite environmental changes [15], [16], [17]. Studies have shown worksite health programs can reduce direct and indirect healthcare costs related to employee absenteeism, loss in productivity and health insurance costs [18], [19], [20], [21], [22].
Worksite health promotion programs directed at a small number of employees at higher risk of chronic disease have been shown to yield greater effectiveness and cost saving [23], [24], [25]. The purposes of this study were to: (1) review the current literature regarding workplace health promotion interventions for employees with elevated risk of chronic diseases including obesity, cardiovascular diseases, and diabetes; (2) catalogue the common intervention and evaluation strategies used when implementing and assessing those interventions; and (3) offer recommendations for future research and practice.
2. Materials and methods
The search strategy for this study followed recommendations of Smith and Shurtz [26] for conducting an efficient and well-contrived literature review. We initially searched for articles in five electronic databases: MEDLINE, PubMed, CINIAL, EBSCO, and Cochrane Library, and limited the search to academic journal articles in English from January 1995 to December 2014. The focus of the present study is on at-risk employees based on their disease or disease-related health risk factors. Thus, we divided our keywords into three categories. The first group of search terms was related to the workplace or worksite setting and the intended employee population. The second group of terms focused on the targeted physical health problem such as a chronic disease. The last group of terms focused on what has been done to deal with the problems such as an intervention and management (Table 1). Within these databases, we used a combination of keywords from the table related to the “setting/population” and “problem” and “outcome.”
Table 1.
Literature searching keywords
| Setting/population | Problem | Outcome |
|---|---|---|
| Worksite Workplace Employee |
Obesity Cardiovascular disease Diabetes Back pain Chronic disease |
Management Intervention |
The following example using only PubMed provides more detail about the search strategy used for this literature review. A search on January 25, 2015 of the literature database PubMed generated 453 results using the terms “(worksite OR workplace OR employee) AND (obesity OR cardiovascular disease OR diabetes OR back pain OR chronic disease) AND (management OR intervention)” and the restrictions “Limits: Journal articles, 01/01/1995 to 12/31/2014, English, Field: Title/Abstracts.”
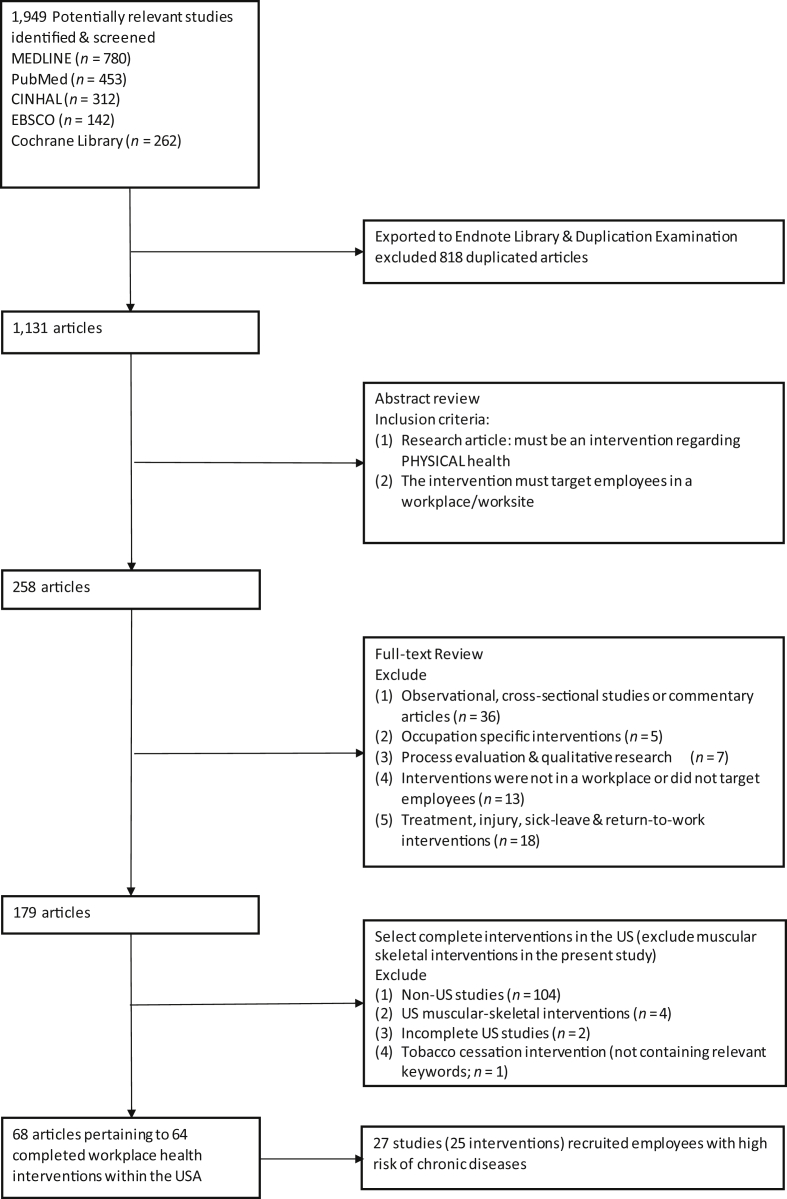
Fig. 1 shows the articles found during our search and the methods used to reduce this article pool to the analytic sample for this review. A total of 1,131 unique articles were identified using our search criteria. Abstracts were reviewed to determine the appropriateness of the study in terms of meeting our inclusion criteria. From this process, we found 68 articles pertaining to 64 completed workplace health interventions within the US that matched our inclusion criteria. Only US-based intervention studies were included in this review to create a meaningful inventory of workplace-delivered interventions targeting at-risk employees and ensure the findings from this review could be interpreted in the same context (thereby yielding more practical implications). Out of those 68 articles, 27 articles were retained for further review. The worksite studies selected were not those designed for the whole employee population, instead, they had to have clear recruitment criteria such as being obese and overweight, sedentary, or at least one baseline clinical measurement exceeding recommended range. For example, in a worksite intervention conducted by White and Jacques [16], the recruitment criteria targeted employees with at least one baseline measurement outside of the recommended rage, including blood pressure (≤ 120/80 mmHg), total cholesterol (≤ 200 mg/dL), low-density lipoprotein–cholesterol (≤ 100 mg/dL), triglycerides (≤ 150 mg/dL), fasting blood sugar (≤ 100 mg/dL), and body mass index (BMI; ≤ 25 kg/m2). In total, 25 completed workplace health interventions were descripted in the 27 articles, and were analyzed for the present study. Data regarding the workplace intervention and evaluation were extracted from articles and entered in a content rubric designed for this study. The content rubric included journal information, sample information, intervention information, evaluation information, and implication and recommendation. After this information was compiled in the rubric, it was reviewed for completeness by two researchers. Then, after being synthesized, the researchers summarized its contents based on the pre-determined scope and purposes of this review.
Fig. 1.
Flow chart of study selection.
3. Results
3.1. Study characteristics
After applying inclusion criteria, we included 27 articles, which describe the results from 25 interventions. All of the interventions were conducted in the US. Specific workplace settings included private-sector and public-sector employers. The employers included six universities, four hospital/health centers, two government entities, one insurance company, one manufacturer, one pharmaceutical corporation, and one bank (Table 2). The 25 interventions were implemented between 1997 and 2014. Two studies were published prior to 2000, seven studies were published between 2000 and 2009, and 16 studies were published after 2010. Nine of the 25 studies were randomized controlled trials and six were quasi-experiments. Ten studies used pre-experimental designs.
Table 2.
Intervention
| Publication year | Lead author | Study design | Setting (workplace type) | Disease-specific intervention | Intervention duration | Intervention description | Incentives |
|---|---|---|---|---|---|---|---|
| 1997 | Fouad [28] | Quasi-experimental design | Birmingham municipal government employees (principally blue-collar workers) | Hypertension | 12 mo | Health education sessions | Financial incentives & food |
| 1998 | Fries [29] | Quasi-experimental design | Principally white-collar workers | Chronic disease: arthritis, back pain, high blood pressure, diabetes mellitus, heart problems, smoking, obesity, stroke, chronic obstructive pulmonary disease | 6 mo | Participants receive educational modules based on individual's health risk problems (books, audiotapes, videotapes, letters & reports) | No |
| 2002 | Burton [23] | Pre-experimental design | Bank One employees | Diabetes | 2 mo | Five bimonthly 1-h seminars presented by certified diabetes nurse educators | Small gift incentives & food |
| 2006 | Aldana [30] | Pre-experimental design | BD Medical employees, Sandy, Utah | Diabetes | 12 mo +12 mo maintenance | Exercise classes; free membership to employee fitness center; Distribution of pedometer; diabetes education group sessions; quarterly 1-on-1 conferences; reading materials | Financial incentive |
| 2006 | John [27] | Pre-experimental design | Manufacturing workplace (Blue Ridge Paper Products) | Cardiovascular diseases & diabetes | 1 y (re-enroll up to 3 y) individual varies (1–3 y) | A minimum of 8 1-on-1 visits with pharmacists in the first y & 6 visits in subsequent y (if re-enrolled) | No |
| 2007 | Hughes [31] | Pre-experimental design | 3 Fortune 500 corporations in the Pacific Northwest | Overweight & obesity | 26- or 52- wk | Personal fitness training sessions; individual nutrition & behavioral change counseling; physician monitoring; group-based sessions | No |
| 2007 | White [16] | Pre-experimental design | Mid-sized regional comprehensive university employees | Cardiovascular diseases | 12 wk | Educational workshops (include various topics & exercise session); follow 1 of 4 exercise prescription | No |
| 2008 | Maron [32] | Randomized controlled trial | Vanderbilt University | Cardiovascular disease | 12 mo | Longitudinal individualized face-to-face counseling with nurse | No |
| 2009 | Ferdowsian [33] | Quasi- experimental design | Government Employees Insurance Company (GEICO) | Overweight & Obesity; Cardiovascular risk | 22 wk | Group meeting; follow a low-fat vegan diet for 22 wk; take daily multiple vitamin (B12); cafeteria management (offer low-fat vegan menu options) | Financial incentives |
| 2009 | Levin [34] | ||||||
| 2010 | Merrill [35] | Pre-experimental design | Ceridian, a business services company | Overweight & obesity | 12 mo in cycle (study last 8 y) | Telephone consultation with health coach; Health Coaching website; online discussions; e-mail/mail connection with coaches; distribution of pedometer; reading materials | No |
| 2010 | Touger-Decker [36] | Quasi- experimental design | Academic health science center employees | Overweight & obesity | 12 wk+ 14 wk maintenance | Weekly group sessions with Registered dietician; e-mail & telephone reminders of sessions; distribution of pedometer (Control group: weekly session content online & online forum) | Small gift incentives & food |
| 2011 | Barham [37] | Randomized controlled trial | Onondaga County employees | Diabetes | 3 mo+ 12 mo maintenance | Weekly group sessions; distribution of pedometer, portion plate, measuring cups & spoons, books, & exercise DVD; (maintenance period offer monthly sessions) | Administrative leave |
| 2011 | John [38] | Pre-experimental design | University of Tennessee faculty & staff members | Overweight & obesity, sedentary | 9 mo | Sit–stand table & a treadmill for each office worker | No |
| 2011 | Linde [39] | Randomized controlled trial | University of Minnesota employees | Overweight & obesity | 6 mo | Participate 1 of 5 90-min weight-control education sessions; weekly weight self-tracking cards; distribution of bathroom scale & pedometer | No |
| 2011 | Mauceri [40] | Pre-experimental design | Novartis Pharmaceuticals Corporation employees | Cardiovascular diseases & diabetes | 6 mo | Monthly educational lunchtime seminars; team activity; nutrition, medical, & fitness consultation; 3-mo interim meeting with physician; blood pressure monitors distribution; bimonthly weigh-ins | Financial incentives & small gifts |
| 2011 | Terry [41] | Quasi- experimental design | Ten large private-sector & public-sector employers | Overweight & obesity | About 250 d | Personalized, telephone-based weight management coaching program that included up to 5 calls | Financial incentive |
| 2012 | Lahiri [42] | Quasi-experimental design | Nursing home health care workers | Overweight & obesity | 16 wk+ 12 wk maintenance | Educational consultation; deposit (lose if gain weight, win more if lose weight) | Financial incentives |
| 2012 | Malarkey [43] | Randomized controlled trial | Faculty & staff of the Ohio State University | Cardiovascular disease risk | 8 wk+ maintenance period (up to 1 y) | Weekly standard Mindfulness-based Stress Reduction program (Yoga movement is done standing or seated, & music is in background); (Control group: lifestyle education group; assigned reading; quiz) | Financial incentives |
| 2013 | Batra [44] | Randomized controlled trial | Four office-based Massachusetts worksites | Overweight & obesity; cardiovascular risk | 6 mo+ 6 mo maintenance | Up to 19 educational group sessions; weekly email for weight self-monitoring; monthly nutrition & health seminar | No |
| 2013 | Salinardi [45] | ||||||
| 2013 | Carr [46] | Randomized controlled trial | South-eastern university | Overweight & obesity, sedentary | 12 wk | Portable pedal machine for each participant; motivational website; pedometer to use in conjunction with the website; e-mail communication | No |
| 2013 | Koepp [47] | Pre-experimental design | Educational Credit Management Corporation (ECMC) office workers | Job description as sedentary | 1 y | Treadmill desk replace pre-existing office desks | No |
| 2013 | Kullgren [48] | Randomized controlled trial | Children's Hospital of Philadelphia | Overweight & obesity | 36 wk | Website tracking; Individual- /Group- based financial incentives for losing weight | Financial incentives |
| 2013 | Mishra [15] | Randomized controlled trial | GEICO | Nutrition (the targeted population is overweight & diabetic) | 18 wk | Weekly lunch h classes; cafeteria management (offer low-fat vegan menu options); follow prescribed vegan diet; daily vitamin B12; online message board; instruction materials | Financial incentives |
| 2014 | Carpenter [49] | Pre-experimental design | Blue collar and white collar employees from a range of occupations | Overweight & obesity | 12 mo | 3 proactive counseling phone calls; comprehensive website with eLearning modules; online support community & emails; distribution of pedometer & tape measure | No |
| 2014 | Stites [50] | Randomized controlled trial | Large urban hospital | Overweight & obesity | 4 wk full intervention; 4 partial intervention | Up to 2 × 90 min session; online cafeteria pre-ordering system; e-mail communication | Financial incentives |
3.2. Population characteristics
Among the 25 interventions, the mean age of participants was about 45 years, with ages ranging from 18 years to 84 years. Women represented the majority of the participants at most worksites, ranging from 53% to 93.4%. Women represented an overwhelming majority of participants in nine studies, ranging from 75% to 93.4%. Men represented the majority of participants in only two settings. Those interventions included a paper product manufacturing company with 70% male participants, and a blue-collar setting with 86% male participants [27], [28] (Table 2). Thirteen studies reported the race/ethnicity of participants. Among those articles with detailed race/ethnicity data, Caucasians comprised the majority of participants, ranging from 50% to 90%, with the exception of one study conducted among municipal employees in Birmingham, Alabama, in which 63% of participants were African–American. African–Americans were the second largest race represented in the interventions (ranging from 11% to 63% in 9 studies), followed by Asian (ranging from 4% to 31.8% in 6 studies) and Hispanic (ranging from 1.5% to 13.6% in 8 studies) participants.
Each worksite intervention seemed to attract participants with a specific chronic disease, based on the focus of the intervention. This is attributed to each intervention having a clear set of inclusion criteria for recruiting eligible employees. Those high-risk employees either had already been diagnosed with a chronic disease or were at high risk of getting a chronic disease such as cardiovascular disease or diabetes.
3.3. Targeted diseases
The most common chronic diseases targeted by the interventions included overweight and obesity, diabetes, and cardiovascular diseases. Some interventions targeted more than one chronic disease (Table 2). Thirteen worksite interventions targeted overweight and obesity; six interventions targeted diabetes, and eight interventions targeted cardiovascular disease. Two interventions targeted changing daily risky behavior such as sedentary work lifestyle. Only one intervention targeted overall chronic diseases, including cardiovascular disease, diabetes, arthritis, back pain, obesity, and chronic obstructive pulmonary disease [29].
3.4. Intervention components
3.4.1. Instructional education/consultation components
Of the 25 interventions, 20 incorporated educational and informative components, such as group discussion, one-on-one consultation, and health coaching (Table 3). Nine interventions used one-on-one consultation/health coaching and 15 used group-based sessions/seminars. Four interventions used both one-on-one consultations and group-based discussions. Most group sessions were held on-site at the worksite and during lunch breaks. Almost all instructional interventions included educational materials, such as brochures, mails, books, or videotapes. Topics covered by group education and consultation included self-care, health management, chronic disease, and the benefits of physical activity and a healthy diet. All education sessions and health consultations were conducted by health professionals, including trained health coach, nutritionist, physician, registered dietitian, cooking instructor, nurse, psychologist, physical therapist, health educator, pharmacist, researcher, exercise physiologist, and behavior health specialist. Two studies did not report the training/expertise of the facilitators [16], [37].
Table 3.
Intervention components
| Publication year | Lead author | Instructional education/ consultation |
Environmental change | Physical activity | Technology (phone) | Technology (Internet/computer) |
|---|---|---|---|---|---|---|
| 1997 | Fouad [28] | X | – | – | – | – |
| 1998 | Fries [29] | – | – | – | – | X |
| 2002 | Burton [23] | X | – | – | – | – |
| 2006 | Aldana [30] | X | – | X | – | – |
| 2006 | John [27] | X | – | – | – | – |
| 2007 | Hughes [31] | X | – | X | – | – |
| 2007 | White [16] | X | – | X | – | – |
| 2008 | Maron [32] | X | – | – | – | – |
| 2009 | Ferdowsian [33] | X | X | – | – | – |
| 2009 | Levin [34] | |||||
| 2010 | Merrill [35] | X | – | X-p∗ | X | X |
| 2010 | Touger-Decker [36] | X | – | X-p | X | X |
| 2011 | Barham [37] | X | – | X-p | – | – |
| 2011 | John [38] | – | XX† | – | – | |
| 2011 | Linde [39] | X | – | X-p | – | – |
| 2011 | Mauceri [40] | X | – | – | – | – |
| 2011 | Terry [41] | X | – | – | X | – |
| 2012 | Lahiri [42] | X | – | – | – | – |
| 2012 | Malarkey [43] | X | – | X | – | – |
| 2013 | Batra [44] | X | – | – | – | X |
| 2013 | Salinardi [45] | |||||
| 2013 | Carr [46] | – | XX | – | X | |
| 2013 | Koepp [47] | – | XX | – | – | |
| 2013 | Kullgren [48] | – | – | – | – | X |
| 2013 | Mishra [15] | X | X | – | – | X |
| 2014 | Carpenter [49] | X | – | X-p | X | X |
| 2014 | Stites [50] | X | X | – | – | X |
“p” represents intervention that included pedometer distribution as physical activity-based components.
“XX” represents intervention that used environmental change to facilitate physical activity.
3.4.2. Environmental change components
Of the 25 interventions, six studies featured environmental changes (Table 3). Common worksite environmental changes were classified into two main types: facilitated physical activity and facilitated diet change. To facilitate physical activity, some interventions installed treadmill desks and distributed exercise equipment (e.g., pedal machines) to participants [38], [46], [47]. To facilitate healthy diet changes, three studies included an organizational policy related to cafeteria management, which made low-fat vegan menu options available for participants [15], [34], [50]. In Stites and colleagues’ [50] study, an online preordering system was designed to allow participants to order their lunch prior to mealtime while viewing the nutrient content of the food choices. Making the nutrition information and low-fat/calories food available to employees was the main purpose of interventions making environmental changes to facilitate diet change.
3.4.3. Physical activity components
Physical activity topics were addressed in the education or consultations, and many interventions included actual physical activity exercises or distributed exercise tracking tools to reinforce behavioral change (Table 3). As mentioned above, there were three interventions using environmental change to facilitate physical activity. There were another five interventions that distributed pedometers to participants to prompt their physical activity and reduce sedentary time. In addition, group-based exercise sessions were incorporated in two studies in university settings. One was a diet and exercise intervention, while the other was a mindfulness practice program [16], [43]. In three Fortune 500 corporations, a lifestyle-based weight management program included exercise rooms and one-on-one fitness training for participants [31]. In a diabetes prevention program for medical employees, free fitness center memberships were provided to encourage more physical activity [30].
3.4.4. Multicomponent interventions
In this review, multicomponents are defined based on the three components described above (instructional education/consultation, environmental change, and physical activity). That is, a multicomponent intervention had to include at least two of the three categories. Among the 15 multicomponent studies, three interventions had physical activity-based components facilitated by environmental changes (treadmill and pedal-machine), five interventions combined education/consultation with distribution of pedometers, and three studies combined education/consultation components with worksite environmental changes to facilitate a healthy diet. Another four interventions combined education/consultation components with physical activity-based group sessions, one-on-one training, or free fitness facility memberships.
Of the 25 interventions, 23 interventions used at least one component described above, including the 15 multicomponent interventions, and eight single component interventions used instructional education/consultation components only. In the other two studies without components described above, self-directed learning was used. Participants received printed or online materials containing health information. In one study conducted in 1998, high-risk employees received health education materials such as books, audiotapes, and videotapes regarding their personal health risk factors [29]. The other study combined health information distribution with large financial rewards for weight loss [48].
3.5. Technology for interventions
Four interventions involved telephones/cellphones, and nine interventions used websites and the internet (Table 3). Telephone/cellphone communications were used most for one-on-one health consultation, but other phone functions (such as sending text messages) were also used as reminders for attending appointments or sessions [36].
In four studies, the internet was used to facilitate communication among participants and health professionals, in the form of weekly e-mail for individual support and self-monitoring reminders, or online interactive message boards [15], [36], [45], [48]. Program websites were created along with the intervention as a comprehensive resource offering eLearning modules and other session materials and tools [35], [49]. Computer-based technology was designed to facilitate the intervention, such as online lunch pre-ordering system [50]. In a physical activity-based intervention, pedal machines were distributed to the sedentary employees. Carr and colleagues [46] used a personal computer interface and software package that accompanied the pedal machine, which allowed for objective monitoring of individual pedal activity.
3.6. Duration
The duration of program refers to the length of the intervention periods. In the chosen studies, 14 intervention periods varied from 1 month to 6 months. Eleven studies had an intervention period > 6 months but < 1 year (Table 2). Two studies collected and analyzed data from multiple years (range, from 3 years to 8 years) when programs were delivered in cycles or on a repeated basis [27], [35]. For example, a 1-year telephone health coach intervention was offered to a business services company in cycles over 8 years from 2001 to 2008 [35]. Six studies included a maintenance period, after which outcomes were measured again. Maintenance periods varied from 3 months to 12 months postintervention, and depended on the design and duration of the intervention period.
3.7. Incentives
Incentives were frequently used in the health promotion programs, and can be classified into many different types (Table 2). Of the 25 interventions, 13 used either financial or other types of incentives such as paid leave time, health devices, and free water bottles. Financial incentives were given to employees for different purposes including participating in the intervention and achieving health goals, compensating control group participants, and completing data collection. In a diabetes study, participants were given 30 minutes of administrative leave at no cost as an incentive for encouraging continuous participation [37]. In another diabetes study, participants were awarded a free glucose monitor as an incentive [28]. Most interventions were provided at no cost to the participants, except one weight management program implemented at three Fortune 500 corporations in the Pacific Northwest where the participants paid for 20–30% of the program cost [31].
3.8. Measurement
Outcomes for workplace health promotion programs were classified into three different categories: health outcomes, work-related outcomes, and economic outcomes (Table 4). Among the 25 interventions, 24 evaluated health outcomes such as laboratory tests and self-reported questionnaires assessing health behaviors, three evaluated work-related outcomes such as presentism and absenteeism, and four evaluated economics outcomes such as pharmaceutical usage and costs due to sick days. Common measures for worksite health promotion programs can be classified into two categories: subjective measures and objective measures (Table 5). Objective measures included anthropometric measures such as weight, height, waist circumstance; laboratory tests such as fasting glucose, lipid profile; and other medical or company documentation on medical claims and absenteeism. Common subjective measures included self-reported questionnaires and telephone interviews that collected data related to health status, quality of life, physical activity, nutrition intake, and work performance. Twenty of the 25 intervention measurements featured at least one objective measure, and 20 featured at least one subjective measure, and 15 featured both subjective and objective measure.
Table 4.
Evaluation
| Publication year | Lead author | Outcome of interest | No. of data collection time points | Data collection time point | Measures/items/scales/instruments collected |
|---|---|---|---|---|---|
| 1997 | Fouad [28] | Health | 2 | Baseline & postintervention | Blood pressure |
| 1998 | Fries [29] | Health & economics | 2 | Baseline & postintervention | Health risk scores, physician use, hospital stay, the duration of illness or confinement to home; medical cost |
| 2002 | Burton [23] | Health & economics | 3 | Baseline, 3 mo, & 6 mo | Knowledge of diabetes, blood specimen analysis, self-rated of diabetic control, eye examination, medical & pharmaceutical costs; laboratory tests: plasma glucose, hemoglobin A1c, high-performance liquid chromatography |
| 2006 | Aldana [30] | Health | 4 | Baseline, 6 mo, 12 mo, & 24 mo | Weight, BMI, waist circumference, two-h oral glucose tolerance testing, fasting insulin, hemoglobin A1c, HDL, LDL, triglycerides & aerobic fitness, high-sensitivity C-reactive protein |
| 2006 | John [27] | Health | 2 | Baseline & postintervention | BMI, systolic & diastolic blood pressures, full lipid profile |
| 2007 | Hughes [31] | Health & economics | 3 | Baseline, postintervention, & 1-y post | Weight, BMI, waist circumference, blood pressure, physical activity (self-reported), Beck Depression Inventory, Rosenberg Self-Esteem Scale, Self-reported medical visits; Self-reported sick days, Pharmaceutical use (from 3rd party administrator) |
| 2007 | White [16] | Health | 2 | Baseline & postintervention | Blood pressure, weight, body composition, BMI, blood glucose, total cholesterol, LDL, HDL, triglyceride; program adherence |
| 2008 | Maron [32] | Health | 2 | Baseline & postintervention | Smoking status, dietary assessment, physical activity assessment, BMI, heart rate, blood pressure, fasting lipids & lipoproteins, fasting glucose, hemoglobin A1c |
| 2009 | Ferdowsian [33] | Health & work | 2 | Baseline & postintervention (24 h diet recalls & absenteeism were measured multiple times during the 22 wk) | Program adherence by measuring diet recall, body weight, waist, hip circumference, blood pressure, plasma lipid concentrations |
| 2009 | Levin [34] | Health | 2 | Baseline & post-intervention | 3 consecutive d diet record |
| 2010 | Merrill [35] | Health | 4 | Baseline, 3 mo, 6 mo, & 12 mo | Health status, BMI, confidence to reduce weight |
| 2010 | Touger-Decker [36] | Health | 3 | Baseline, 12 wk, & 26 wk | Health-related quality of life (14), 24-h diet recall, physical activity questionnaire, body weight & waist circumference; body fat, Framingham Risk Score-Heart Study General Cardiovascular Disease |
| 2011 | Barham [37] | Health | 4 | Baseline, 3 mo, 6 mo, & 12 mo | Weight, height, BMI, waist circumference, blood pressure, fasting blood glucose, fasting lipid profiles; Survey: Short Form-12, Perceived stress scale, Impact of weight on quality of life, Three-Factors Eating Questionnaire-R18; National Cancer Institute Dietary Fat Screener; International Physical Activity Questionnaire, The Work Stress Inventory |
| 2011 | John [38] | Health | 3 | Baseline, 3 mo, & 9 mo | ActivPAL detects accelerations; height, weight, waist & hip circumferences; body composition, bone mineral density, resting heart rate & blood pressure; serum lipid profile, plasma glucose, insulin, glycosylated hemoglobin; 24-h diet recall (telephone interview) |
| 2011 | Linde [39] | Health | 3 | Baseline, 3 mo, & 6 mo; (behavior tracking was measured weekly during the 6 mo) | Weight, weight self-monitoring, behavior tracking, intervention salience, & reinforcement |
| 2011 | Mauceri [40] | Health | 2 | Baseline & post-intervention (Blood pressure, lipid profiles & HbA1C were measured 3 times during the 6 mo) | General health status, diet & exercise; metabolic syndrome (abdominal obesity, waist circumference, triglyceride, HDL, BP, Fasting glucose); Medication adherence, Framingham heart disease risk assessment. Clinical: to hypertension cohort--blood pressure; to hyperlipidemia cohort-HDL, LDL, Triglyceride; to diabetes cohort--HbA1c. |
| 2011 | Terry [41] | Health | 2 | Baseline & postintervention | Validated Health Risk Assessment, established previously based on associations between assessed health risks & cardiac-associated mortality rates |
| 2012 | Lahiri [42] | Work | 3 | Baseline, 16 wk, & 28 wk (absenteeism & presentism were only measured at baseline & wk 28) | Absenteeism, Presentism by Work Limitations Questionnaires |
| 2012 | Malarkey [43] | Health | 4 | Baseline, 2 mo, 6 mo, & 12 mo | Blood pressure, pulse rate, BMI, blood sample; Biomarkers: level of inflammatory peptide C-reactive protein, interleukin 6, salivary cortisol, leptin. Questionnaires: Perceived Stress Scale, Sleep-Pittsburgh Sleep Quality Index, depressive symptoms: Center for Epidemiological Studies Depression; mindfulness: The Toronto Mindfulness Scale |
| 2013 | Batra [44] | Health | 2 | Baseline & postintervention | Weight; Food craving questionnaire, Three-factor eating questionnaire |
| 2013 | Salinardi [45] | Health | 2 | Baseline & postintervention (weight was measured 6 times in intervention group during the 6 mo) | Weight, height, blood pressure, blood glucose, total cholesterol & triglycerides |
| 2013 | Carr [46] | Health | 2 | Baseline & postintervention | Sedentary time measured by StepWatch physical activity monitor, blood pressure, body mass, heart rate, waist circumference, fasting blood lipids, estimated aerobic fitness |
| 2013 | Koepp [47] | Work & health | 3 | Baseline, 6 mo, & 12 mo | Daily physical activity (using accelerometers), work performance, body composition, & blood variables: glucose, insulin, hemoglobin A1C, & lipids |
| 2013 | Kullgren [48] | Health | 3 | Baseline, 24 wk, & 36 wk (weight was measured monthly during the 36 wk) | Weight; Physical Activity Questionnaire, Three-Factor Eating Questionnaire-R18, participation in weight-related wellness programs |
| 2013 | Mishra [15] | Health | 2 | Baseline & postintervention | Online automated self-administered 24-h diet recall |
| 2014 | Carpenter [49] | Health | 3 | Baseline, 6 mo, & 12 mo | Weight loss, program use, health behavior change |
| 2014 | Stites [50] | Health | 2 | Baseline & postintervention | Mindful Eating Questionnaire; height, body weight, BMI, hemoglobin A1c, cholesterol, triglycerides, lipid, lipoprotein; glycohemoglobin; lunch purchases via card swiping record |
BMI, body mass index; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Table 5.
Type of measures
| Publication year | Lead author | Subjective measures |
Objective measures |
||
|---|---|---|---|---|---|
| Self-reported | Measured Anthropometry |
Laboratory tests | Other measures | ||
| 1997 | Fouad [28] | – | – | – | Blood pressure |
| 1998 | Fries [29] | X | – | – | – |
| 2002 | Burton [23] | X | – | X | Eye examination; medical cost (diabetes medication cost) |
| 2006 | Aldana [30] | – | X | X | Aerobic fitness |
| 2006 | John [27] | – | X | X | Systolic & diastolic blood pressures |
| 2007 | Hughes [31] | X | X | – | Blood pressure; medical claims of prescription drugs (pharmaceutical use) |
| 2007 | White [16] | X | X | X | Blood pressure |
| 2008 | Maron [32] | – | X | X | Heart rate; blood pressure |
| 2009 | Ferdowsian [33] | X | X | X | Blood pressure |
| 2009 | Levin [34] | X | – | – | – |
| 2010 | Merrill [35] | X | – | – | – |
| 2010 | Touger-Decker [36] | X | X | – | – |
| 2011 | Barham [37] | X | X | X | Blood pressure |
| 2011 | John [38] | X | X | X | Body composition; bone mineral density; resting heart rate; blood pressure; ActivPAL accelerator |
| 2011 | Linde [39] | X | X | – | – |
| 2011 | Mauceri [40] | X | X | X | To hypertension cohort: blood pressure |
| 2011 | Terry [41] | X | – | – | – |
| 2012 | Lahiri [42] | X | X | – | – |
| 2012 | Malarkey [43] | X | X | X | Blood pressure; pulse rate |
| 2013 | Batra [44] | X | – | – | – |
| 2013 | Salinardi [45] | – | X | X | Blood pressure |
| 2013 | Carr [46] | – | X | X | Blood pressure; body mass; heart rate; estimated aerobic fitness; physical activity monitor |
| 2013 | Koepp [47] | X | – | X | Body composition; accelerometers |
| 2013 | Kullgren [48] | X | X | – | – |
| 2013 | Mishra [15] | X | – | – | – |
| 2014 | Carpenter [49] | X | – | – | – |
| 2014 | Stites [50] | X | X | X | Lunch purchase record |
3.9. Objective measures
Among those studies using objective measures, 17 articles used measured anthropometry such as weight, height, waist circumstance and hip circumstance. Self-reports of height, weight, and so forth were not treated as measured anthropometry [51]. Fourteen studies applied laboratory tests to analyze the health outcomes. Laboratory tests examined blood and saliva samples. Common tests in diabetes interventions included fasting blood glucose, lipid profiles, hemoglobin A1c, and fasting insulin. Other frequently measured health indicators in those interventions included blood pressure, body composition, heart rate, and body mass. Aerobic fitness was assessed in two studies. Both of these interventions incorporated physical activity elements such as free gym memberships and distribution of pedal machines and pedometers [30], [46]. In addition, eye examinations were added as health outcome assessments in another diabetes program [23].
Other objective measures included employee lunch/food purchase record and data from devices such as accelerometers, physical activity monitors, treadmill desk monitors. Those objective measures were used in four of the interventions that incorporated worksite environmental change to facilitate physical activity or healthy diet. In the lifestyle-based weight management intervention conducted in three Fortune 500 corporations, Hughes [31] measured the pharmaceutical purchases from medical claims data, which was collected by a third-party administrator. In another diabetes management program from 1995 to 1997, the cost of diabetes medications and supplies, and the proportion of diabetes-related costs represented in total medical costs were also evaluated from the medical plan [23].
3.9.1. Subjective measures
Subjective measures included sociodemographic characteristics such as age, sex, education, occupation, and disease history. Apart from sociodemographic data, subjective measures were also frequently used to assess health outcomes, health behaviors, and workplace performance. Data were collected by printed or online questionnaires and telephone interviews. Commonly used established instruments are identified and summarized by different outcomes categories below (Table 6). Outcome categories included diet, mental health, work-related, and physical activity. Diet outcomes were assessed in six studies using diet recall and questionnaires such as Three-Factor Eating Questionnaire and Mindful Eating Questionnaire [52], [53]. Mental health outcomes included stress, health related quality of life, depressive symptoms and self-esteem, and were assessed by validated instruments in three studies. Work-related outcomes were assessed in two studies by validated instruments such as Work Limitation Questionnaire to measure presentism and absenteeism due to health problems [54]. Physical activity outcomes were assessed by two studies using the International Physical Activity Questionnaire to measure the amount of activity in which the individual engaged [55].
Table 6.
Validated instruments. This table summarizes the studies using validated established instruments for subjective measures
| Publication year | Lead author | Validated instruments |
|---|---|---|
| 1998 | Fries [29] | Health Risk Assessment with Framingham risk factors model |
| 2007 | Hughes [31] | Beck Depression Inventory; Rosenberg Self-Esteem Scale |
| 2008 | Maron [32] | Health Risk Assessment with Framingham risk score |
| 2009 | Ferdowsian [33] | 3-d diet recall: analyzed using Nutrition Data System for Research software version 2007 |
| 2009 | Levin [34] | Diet recall |
| 2010 | Touger-Decker [36] | Twenty-four-h diet recall; Health-Related Quality of Life (HRQOL-14); Self-administrated International Physical Activity Questionnaire short form |
| 2011 | Barham [37] | Health-related quality of life Short Form-12; Perceived Stress Scale; Impact of Weight on Quality of Life; Three-Factors Eating Questionnaire-R18; National Cancer Institute Dietary Fat Screener, International Physical Activity Questionnaire, The Work Stress Inventory |
| 2011 | John [38] | 24-h diet recall: analyzed using Nutrition Data System for Research software |
| 2011 | Mauceri [40] | Self-administered Morisky adherence questionnaire; Prochaska & DiClemente’s willingness to change model |
| 2011 | Terry [41] | Health Risk Assessment |
| 2012 | Lahiri [42] | Work Limitations Questionnaires |
| 2012 | Malarkey [43] | Perceived stress scale; Pittsburgh Sleep Quality Index; Center for Epidemiological Studies Depression (CES-D); The Toronto Mindfulness Scale |
| 2013 | Batra [44] | Food craving questionnaire; food craving inventory (previously known as Three Factors Eating Questionnaire) |
| 2013 | Koepp [47] | Validated workplace performance survey |
| 2013 | Kullgren [48] | International Physical Activity Questionnaire; Three-Factor Eating Questionnaire-R18 |
| 2013 | Mishra [15] | Online automated self-administered 24-h diet recall developed by National Cancer Institute |
| 2014 | Stites [50] | Mindful Eating Questionnaire |
3.9.2. Combination of objective and subjective measures: Health Risk Assessment and Framingham risk score
Two intervention studies used Health Risk Assessment data to collect self-report biometric outcomes and various health behaviors [41] and calculated a Framingham risk score for high-risk individuals [32]. The Framingham risk score is used to predict estimates of heart attack risks over a 10-year period [56]. A Framingham risk score was calculated for each participant based on both objective and subjective measures, including variables such as age, cholesterol, blood pressure, diabetes, smoking, and other self-reported health behaviors.
4. Discussion
The goal of the present study was to describe the intervention and evaluation characteristics of programs delivered at the workplace for high-risk employee populations, including targeted diseases, intervention components, and outcome measurement types. The present study has the potential to inform future interventions and evaluate programs for diverse workplaces that include employee populations with high risk of chronic diseases. The 27 articles showed variation with regard to research design, intervention components, and evaluation strategies. Most of the studies were conducted in a sedentary job setting such as office or clerical jobs. Some of the chosen interventions were adapted from community or clinical research, evidence-based interventions, or commercial programs [32], [49]. It is important for researchers and practitioners to seek a firm foundation built on previous practice to develop new interventions. Common behavioral change strategies were applied in most interventions, including goal setting, behavior/weight self-tracking, and motivational interviewing [35], [46], [49].
Different work settings have unique characteristics. Researchers and practitioners may need to examine their worksite and employee populations before developing health promotion interventions. In the chosen studies, small group education or physical activity interventions were the most prevalent and feasible format. This was used by worksites that have regular lunch breaks or settings where employees have a certain degree of work autonomy [57]. In some small work settings with a small sample of participants, office environmental change to facilitate physical activity could be practical, such as providing sit–stand tables, treadmill desk and pedal machines. In a large worksite where a cafeteria was provided to employees and purchase transactions were recorded, interventions incorporated food labels and nutrition notifications that were feasible and measurable.
Some studies have shown that employees prefer multicomponent interventions, which are also more likely to be successful [58], [59]. Additional elements in such interventions can assist and supplement education and consultation components by adding worksite environmental changes to facilitate physical activity and healthy diet. However, they may also increase program costs. The growth in mobile device applications and Internet access has increased the number of technology-based workplace health promotion interventions. This can help reduce the common barriers to participation such as time, place, and costs [60], [61], [62]. In worksites where it may be difficult for employees to attend face-to-face interventions together or those that lack regularly scheduled break times, telephonic health coaches and online modules and forums could be considered as intervention delivery choices. Those strategies could also be applied in the modern workplace where employees work through telecommuting and virtual teams. In addition, offering incentives is prevalent in workplace health interventions for promoting healthy behaviors and participation retention, and it is estimated that 69% of large employers use this strategy [63]. Understandably, other strategies such as supervisor support, job modification, and organizational and policy changes for developing workplace health interventions were rarely described in the selected articles; however, they are still crucial elements to program implementation in workplace settings [64].
Effective evaluation strategies are important for assessing program success. Researchers and practitioners may need to choose optimal and suitable measurement based on the intervention components and outcome of interests. In the chosen studies, all the worksite diabetes interventions used laboratory tests to examine blood glucose. Some of them also included other biomarkers such as hemoglobin A1c and fasting insulin. Interventions targeting cardiovascular diseases commonly included biometric measurements such as blood pressures and lipid profiles. However, when using biometric measurements for evaluation of high risk populations, evaluators need to consider their previous and ongoing medication use. This is important because medication use may mitigate program effectiveness in some cases [37]. Interventions that targeted overweight and obesity were the most diversely designed and evaluated. In general, anthropometry measurements were the most prevalent and efficient assessment. Those interventions that incorporated diet education/consultation may assess diet change and behavior using diet recall and validated questionnaires [34]. Interventions that incorporated physical activity may assess aerobic fitness or results from physical activity tracking devices/software [46]. For worksite interventions with economic outcomes of interest (e.g., cost-effectiveness), presentism, absenteeism, and medical costs may be assessed by either self-reported questionnaires or medical documentation [42]. Interventions that involve technology, the Internet, or computer record systems may be used to efficiently and objectively assess online program adherence, healthy food purchases, and physical activity device use [38], [50].
In sum, based on outcome of interests, measurements could include health outcomes, work-related outcomes, and economic outcomes, and evaluation strategies could include objective or subjective measurements. Choosing specific evaluation strategies for an intervention can be based on the intervention component, targeted disease, intervention technology, intervention purpose, and the budget for studies. However, validated and standardized evaluation measures are recommended. Subjective measurement, typically self-reported data, may not be considered as strong as objective measurements. Additional information may be collected regarding participants’ help-seeking behaviors outside the intervention to determine program effectiveness more accurately [41].
4.1. Limitation
This study included common chronic diseases overweight and obesity, cardiovascular disease, and diabetes. A thorough literature search was conducted based on term combinations using “chronic disease,” with results focusing highly on the diseases mentioned above. Our study excluded studies such as chronic mental diseases and muscular skeletal disorders. Future reviews may include other chronic conditions such as muscular skeletal disorders, depression, lung diseases, and asthma. Future studies may also expand upon the intervention-related aspects included in this review to examine outcomes associated with workplace health interventions. Further, it is recommended that future reviews include non-US-based workplace interventions so that country-based comparisons can be made. Based on the focus of this review, the interventions included in this study recruited employees with elevated risk of common chronic diseases in each work setting, which may have limited the generalizability of our findings. The present study summarized the intervention and evaluation strategies, but did not specifically analyze quantitative data, cost or statistical results. Future studies may need to consider a meta-analysis of intervention results to further discuss intervention effectiveness. In addition, when analyzing intervention characteristics, the present study did not exclude the interventions to control group or multiple arms. All intervention and evaluation characteristics were analyzed based on the content provided in the published manuscripts without further contact with the study authors.
5. Conclusion
Despite its limitations, this is the first literature review to focus on workplace interventions for populations with elevated risk for chronic diseases including obesity, cardiovascular diseases, and diabetes. The majority of systematic literature reviews for workplace health promotion focus on entire workforce populations that may or may not include study participants with chronic conditions [65], [66], [67], [68], [69]. Although it is important to target the general workforce in health promotion efforts, workplace interventions may be more beneficial if they purposively recruit and serve at-risk employees (e.g., to address conditions that may reduce work productivity, absenteeism, and healthcare costs). Findings from this review highlight the diverse strategies used to improve health and wellbeing in workplace settings. While the strategies used are not universal, understanding the components and processes included in such interventions has vast implications to inform employers about intervention options (e.g., intervention components, format, duration, technology) and opportunities that exist to improve the health of their workforce.
Conflicts of interest
All authors declare no conflicts of interest.
References
- 1.The Employment Situation—October 2015 Bureau of Labor Statistics 2015 [Internet]. [cited 2015 Dec 11]. Available from: http://www.bls.gov/news.release/pdf/empsit.pdf.
- 2.Thorp A.A., Healy G.N., Winkler E., Clark B.K., Gardiner P.A., Owen N., Dunstan D.W. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int J Behav Nutr Phys Act. 2012;9:128. doi: 10.1186/1479-5868-9-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duncan G.E. Exercise, fitness, and cardiovascular disease risk in type 2 diabetes and the metabolic syndrome. Curr Diab Rep. 2006;6:29–35. doi: 10.1007/s11892-006-0048-1. [DOI] [PubMed] [Google Scholar]
- 4.Warren T.Y., Barry V., Hooker S.P., Sui X., Church T.S., Blair S.N. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42:879–885. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beunza J.J., Martínez-González M.A., Ebrahim S., Bes-Rastrollo M., Núñez J., Martínez J.A., Alonso A. Sedentary behaviors and the risk of incident hypertension: the SUN Cohort. Am J Hypertens. 2007;20:1156–1162. doi: 10.1016/j.amjhyper.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Kivimäki M., Leino-Arjas P., Luukkonen R., Riihimäki H., Vahtera J., Kirjonen J. Work stress and risk of cardiovascular mortality: prospective cohort study of industrial employees. Br Med J. 2002;325:857–860. doi: 10.1136/bmj.325.7369.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bodenheimer T., Chen E., Bennett H.D. Confronting the growing burden of chronic disease: can the U.S. health care workforce do the job? Health Aff. 2009;28:64–74. doi: 10.1377/hlthaff.28.1.64. [DOI] [PubMed] [Google Scholar]
- 8.Fighting obesity in the workplace: National Center for Chronic Disease Prevention and Health Promotion [Internet]. 2013 [cited 2015 Dec 17]. Available from: http://www.cdc.gov/nationalhealthyworksite/docs/fighting_obesity_in_the_workplace_final_2_8_13.pdf.
- 9.Brown H., Roberts J. Exercising choice: the economic determinants of physical activity behaviour of an employed population. Soc Sci Med. 2011;73:383–390. doi: 10.1016/j.socscimed.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finkelstein E.A., Brown D.S., Wrage L.A., Allaire B.T., Hoerger T.J. Individual and aggregate years-of-life-lost associated with overweight and obesity. Obesity. 2010;18:333–339. doi: 10.1038/oby.2009.253. [DOI] [PubMed] [Google Scholar]
- 11.Kleinman N., Abouzaid S., Andersen L., Wang Z., Powers A. Cohort analysis assessing medical and nonmedical cost associated with obesity in the workplace. J Occup Env Med. 2014;56:161–170. doi: 10.1097/JOM.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 12.Goetzel R.Z., Pei X., Tabrizi M.J., Henke R.M., Kowlessar N., Nelson C.F., Metz R.D. Ten modifiable health risk factors are linked to more than one-fifth of employer-employee health care spending. Health Aff. 2012;31:2474–2484. doi: 10.1377/hlthaff.2011.0819. [DOI] [PubMed] [Google Scholar]
- 13.Carnethon M., Whitsel L.P., Franklin B.A., Kris-Etherton P., Milani R., Pratt C.A., Wagner G.R. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120:1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- 14.Soeren Mattke HL, Caloyeras JP, Huang CY, Van Busum KR, Khodyakov D, Shier V. Workplace Wellness Programs Study Final Report RAND Corporation 2013 [Internet]. [cited 2015 Dec 17]. Available from: http://www.rand.org/content/dam/rand/pubs/research_reports/RR200/RR254/RAND_RR254.sum.pdf. [PMC free article] [PubMed]
- 15.Mishra S., Barnard N.D., Gonzales J., Xu J., Agarwal U., Levin S. Nutrient intake in the GEICO multicenter trial: the effects of a multicomponent worksite intervention. Eur J Clin Nutr. 2013;67:1066–1071. doi: 10.1038/ejcn.2013.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White K., Jacques P.H. Combined diet and exercise intervention in the workplace: effect on cardiovascular disease risk factors. AAOHN J. 2007;55:109–114. doi: 10.1177/216507990705500303. [DOI] [PubMed] [Google Scholar]
- 17.French S.A., Harnack L.J., Hannan P.J., Mitchell N.R., Gerlach A.F., Toomey T.L. Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev Med. 2010;50:180–185. doi: 10.1016/j.ypmed.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chapman L.S. Meta-evaluation of worksite health promotion economic return studies: 2012 update. Am J Health Promot. 2012;26 doi: 10.4278/ajhp.26.4.tahp. TAHP1–12. [DOI] [PubMed] [Google Scholar]
- 19.Bachman K.H. Obesity, weight management, and health care costs: a primer. Dis Manag. 2007;10:129–137. doi: 10.1089/dis.2007.103643. [DOI] [PubMed] [Google Scholar]
- 20.Aldana S.G., Greenlaw R.L., Diehl H.A., Salberg A., Merrill R.M., Ohmine S. The effects of a worksite chronic disease prevention program. J Occup Env Med. 2005;47:558–564. doi: 10.1097/01.jom.0000165743.18570.66. [DOI] [PubMed] [Google Scholar]
- 21.Goetzel R.Z., Ozminkowski R.J., Bruno J.A., Rutter K.R., Isaac F., Wang S. The long-term impact of Johnson & Johnson's Health & Wellness Program on employee health risks. J Occup Env Med. 2002;44:417–424. doi: 10.1097/00043764-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Goetzel R.Z., Henke R.M., Tabrizi M., Pelletier K.R., Loeppke R., Ballard D.W., Grossmeier J., Anderson D.R., Yach D., Kelly R.K., McCalister T., Serxner S., Selecky C., Shallenberger L.G., Fries J.F., Baase C., Isaac F., Crighton K.A., Wald P., Exum E., Shurney D., Metz R.D. Do workplace health promotion (wellness) programs work? J Occup Env Med. 2014;56:927–934. doi: 10.1097/JOM.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 23.Burton W.N., Connerty C.M. Worksite-based diabetes disease management program. Dis Manag. 2002;5:1–8. [Google Scholar]
- 24.Groeneveld I.F., Proper K.I., van der Beek A.J., Hildebrandt V.H., van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease – a systematic review. Scand J Work Environ Health. 2010;36:202–215. doi: 10.5271/sjweh.2891. [DOI] [PubMed] [Google Scholar]
- 25.Caloyeras J.P., Liu H., Exum E., Broderick M., Mattke S. Managing manifest diseases, but not health risks, saved PepsiCo money over seven years. Health Aff. 2014;33:124–131. doi: 10.1377/hlthaff.2013.0625. [DOI] [PubMed] [Google Scholar]
- 26.Smith M.L., Shurtz S. Search and ye shall find: practical literature review techniques for health educators. Health Promot Pract. 2012;13:666–669. doi: 10.1177/1524839911432930. [DOI] [PubMed] [Google Scholar]
- 27.John E.J., Vavra T., Farris K., Currie J., Doucette W., Button-Neumann B., Osterhaus M., Kumbera P., Halterman T., Bullock T. Workplace-based cardiovascular risk management by community pharmacists: impact on blood pressure, lipid levels, and weight. Pharmacotherapy. 2006;26:1511–1517. doi: 10.1592/phco.26.10.1511. [DOI] [PubMed] [Google Scholar]
- 28.Fouad M.N., Kiefe C.I., Bartolucci A.A., Burst N.M., Ulene V., Harvey M.R. A hypertension control program tailored to unskilled and minority workers. Ethn Dis. 1997;7:191–199. [PubMed] [Google Scholar]
- 29.Fries J.F., McShane D. Reducing need and demand for medical services in high-risk persons. A health education approach. West J Med. 1998;169:201–207. [PMC free article] [PubMed] [Google Scholar]
- 30.Aldana S., Barlow M., Smith R., Yanowitz F., Adams T., Loveday L., Merrill R.M. A worksite diabetes prevention program: two-year impact on employee health. AAOHN J. 2006;54:389–395. doi: 10.1177/216507990605400902. [DOI] [PubMed] [Google Scholar]
- 31.Hughes M.C. A lifestyle-based weight management program delivered to employees: examination of health and economic outcomes. J Occup Environ Med. 2007;49:1212–1217. doi: 10.1097/JOM.0b013e318159489d. [DOI] [PubMed] [Google Scholar]
- 32.Maron D.J., Forbes B.L., Groves J.R., Dietrich M.S., Sells P., DiGenio A.G. Health-risk appraisal with or without disease management for worksite cardiovascular risk reduction. J Cardiovasc Nurs. 2008;23:513–518. doi: 10.1097/01.JCN.0000338933.81587.b4. [DOI] [PubMed] [Google Scholar]
- 33.Ferdowsian H.R., Barnard N.D., Hoover V.J., Katcher H.I., Levin S.M., Green A.A., Cohen J.L. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot. 2010;24:384–387. doi: 10.4278/ajhp.081027-QUAN-255. [DOI] [PubMed] [Google Scholar]
- 34.Levin S.M., Ferdowsian H.R., Hoover V.J., Green A.A., Barnard N.D. A worksite programme significantly alters nutrient intakes. Public Health Nutr. 2010;13:1629–1635. doi: 10.1017/S136898000999303X. [DOI] [PubMed] [Google Scholar]
- 35.Merrill R.M., Aldana S.G., Bowden D.E. Employee weight management through health coaching. Eat Weight Disord-St. 2010;15:52–59. doi: 10.1007/BF03325280. [DOI] [PubMed] [Google Scholar]
- 36.Touger-Decker R., Denmark R., Bruno M., O'Sullivan-Maillet J., Lasser N. Workplace weight loss program; comparing live and internet methods. J Occup Environ Med. 2010;52:1112–1118. doi: 10.1097/JOM.0b013e3181f9ee8c. [DOI] [PubMed] [Google Scholar]
- 37.Barham K., West S., Trief P., Morrow C., Wade M., Weinstock R.S. Diabetes prevention and control in the workplace: a pilot project for county employees. J Public Health Manag Pract. 2011;17:233–241. doi: 10.1097/PHH.0b013e3181fd4cf6. [DOI] [PubMed] [Google Scholar]
- 38.John D., Thompson D.L., Raynor H., Bielak K., Rider B., Bassett D.R. Treadmill workstations: a worksite physical activity intervention in overweight and obese office workers. J Phys Act Health. 2011;8:1034–1043. doi: 10.1123/jpah.8.8.1034. [DOI] [PubMed] [Google Scholar]
- 39.Linde J., Jeffery R. Testing a brief self-directed behavioral weight control program. Behav Med. 2011;37:47–53. doi: 10.1080/08964289.2011.568992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mauceri E., Bienkowski C., Hanson K.A., Doyle J.J., Jackson J., Bramer S. A Health outcome assessment of the cardio metabolic mission health program at Novartis. J Occup Env Med. 2011;53:647–652. doi: 10.1097/JOM.0b013e31821b7ade. [DOI] [PubMed] [Google Scholar]
- 41.Terry P.E., Seaverson E.L.D., Grossmeier J., Anderson D.R. Effectiveness of a worksite telephone-based weight management program. Am J Health Promot. 2011;25:186–189. doi: 10.4278/ajhp.081112-QUAN-281. [DOI] [PubMed] [Google Scholar]
- 42.Lahiri S., Faghri P.D. Cost-effectiveness of a workplace-based incentivized weight loss program. J Occup Env Med. 2012;54:371–377. doi: 10.1097/JOM.0b013e318247a394. [DOI] [PubMed] [Google Scholar]
- 43.Malarkey W.B., Jarjoura D., Klatt M. Workplace based mindfulness practice and inflammation: a randomized trial. Brain Behav Immun. 2013;27:145–154. doi: 10.1016/j.bbi.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Batra P., Das S.K., Salinardi T., Robinson L., Saltzman E., Scott T., Pittas A.G., Roberts S.B. Relationship of cravings with weight loss and hunger. Results from a 6 month worksite weight loss intervention. Appetite. 2013;69:1–7. doi: 10.1016/j.appet.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 45.Salinardi T.C., Batra P., Roberts S.B., Urban L.E., Robinson L.M., Pittas A.G., Lichtenstein A.H., Deckersbach T., Saltzman E., Das S.K. Lifestyle intervention reduces body weight and improves cardiometabolic risk factors in worksites. Am J Clin Nutr. 2013;97:667–676. doi: 10.3945/ajcn.112.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carr L.J., Karvinen K., Peavler M., Smith R., Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ Open. 2013;3:e003261. doi: 10.1136/bmjopen-2013-003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koepp G.A., Manohar C.U., McCrady-Spitzer S.K., Ben-Ner A., Hamann D.J., Runge C.F., Levine J.A. Treadmill desks: a 1-year prospective trial. Obesity. 2013;21:705–711. doi: 10.1002/oby.20121. [DOI] [PubMed] [Google Scholar]
- 48.Kullgren J.T., Troxel A.B., Loewenstein G., Asch D.A., Norton L.A., Wesby L., Tao Y., Zhu J., Volpp K.G. Individual- versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013;158:505–514. doi: 10.7326/0003-4819-158-7-201304020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carpenter K.M., Lovejoy J.C., Lange J.M., Hapgood J.E., Zbikowski S.M. Outcomes and utilization of a low intensity workplace weight loss program. J Obes. 2014;2014:1–7. doi: 10.1155/2014/414987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stites S.D., Singletary S.B., Menasha A., Cooblall C., Hantula D., Axelrod S., Figueredo V.M., Phipps E.J. Pre-ordering lunch at work. Results of the what to eat for lunch study. Appetite. 2015;84:88–97. doi: 10.1016/j.appet.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 51.Preedy V.R. Springer; New York: 2012. Handbook of anthropometry: physical measures of human form in health and disease; pp. 168–169. [Google Scholar]
- 52.Framson C. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009;109:1439–1444. doi: 10.1016/j.jada.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stunkard A.J., Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 54.Lerner D., Amick B.C., Rogers W.H., Malspeis S., Bungay K., Cynn D. The work limitations questionnaire. Med Care. 2001;39:72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 55.Craig C.L., Marshall A.L., Sjöström M., Bauman A.E., Booth M.L., Ainsworth B.E., Pratt M., Ekelund U., Yngve A., Sallis J.F., Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 56.Smith K.W., McKinlay S.M., Thorington B.D. The validity of health risk appraisal instruments for assessing coronary heart disease risk. Am J Public Health. 1987;77:419–424. doi: 10.2105/ajph.77.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kruger J., Yore M.M., Bauer D.R., Kohl H.W. Selected barriers and incentives for worksite health promotion services and policies. Am J Health Promot. 2007;21:439–447. doi: 10.4278/0890-1171-21.5.439. [DOI] [PubMed] [Google Scholar]
- 58.Centers for Disease Control and Prevention Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR. 2005;54(No. RR-10):11. [PubMed] [Google Scholar]
- 59.Goldgruber J., Ahrens D. Effectiveness of workplace health promotion and primary prevention interventions: a review. J Public Health. 2010;18:75–88. [Google Scholar]
- 60.Anderson L.M., Quinn T.A., Glanz K., Ramirez G., Kahwati L.C., Johnson D.B., Buchanan L.R., Archer W.R., Chattopadhyay S., Kalra G.P., Katz D.L. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med. 2009;37:340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 61.Carr L.J., Bartee R.T., Dorozynski C., Broomfield J.F., Smith M.L., Smith D.T. Internet-delivered behavior change program increases physical activity and improves cardiometabolic disease risk factors in sedentary adults: results of a randomized controlled trial. Prev Med. 2008;46:431–438. doi: 10.1016/j.ypmed.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 62.Tate D.F., Jackvony E.H., Wing R.R. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a Randomized Trial. JAMA. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 63.Watson T. The New Health Care Imperative: Driving Performance, Connecting to Value. 19th Annual Towers Watson/National Business Group on Health Employer Survey on Purchasing Value in Health Care [Internet]. 2014 [cited 2015 Dec 17]. Available from: https://www.towerswatson.com/en-US/Insights/IC-Types/Survey-Research-Results/2014/05/full-report-towers-watson-nbgh-2013-2014-employer-survey-on-purchasing-value-in-health-care.
- 64.Wilson M.G., DeJoy D.M., Vandenberg R.J., Richardson H.A., McGrath A.L. Work characteristics and employee health and well-being: test of a model of healthy work organization. J Occup Organ Psychol. 2004;77:565–588. [Google Scholar]
- 65.Ausburn T.F., LaCoursiere S., Crouter S.E., McKay T. Review of Worksite Weight Management Programs. Workplace Health Saf. 2014;62:122–126. doi: 10.1177/216507991406200306. [DOI] [PubMed] [Google Scholar]
- 66.Benedict M.A., Arterburn D. Worksite-based weight loss programs: a systematic review of recent literature. Am J Health Promot. 2008;22:408–416. doi: 10.4278/ajhp.22.6.408. [DOI] [PubMed] [Google Scholar]
- 67.Gudzune K., Hutfless S., Maruthur N., Wilson R., Segal J. Strategies to prevent weight gain in workplace and college settings: a systematic review. Prev Med. 2013;57:268–277. doi: 10.1016/j.ypmed.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 68.Pratt C.A., Lemon S.C., Fernandez I.D., Goetzel R., Beresford S.A., French S.A., Stevens V.J., Vogt T.M., Webber L.S. Design characteristics of worksite environmental interventions for obesity prevention. Obesity. 2007;15:2171–2180. doi: 10.1038/oby.2007.258. [DOI] [PubMed] [Google Scholar]
- 69.Gwin S., Branscum P., Zacharia S., Alshuwaiyer G., Taylor E.L., Funk M. Internet-based physical activity interventions at the worksite: a systematic review. Am J Health Stud. 2013;28:114–126. [Google Scholar]