Abstract
Background
Low back pain (LBP) is a major problem for office workers. Individuals adopting poor postures during prolonged sitting have a considerably increased risk of experiencing LBP. This study aimed to investigate seat pressure distribution characteristics, i.e., average pressure, peak pressure ratio, frequency of postural shift, and body perceived discomfort (BPD), during 1 hour of sitting among office workers with and without chronic LBP.
Methods
Forty-six participants (chronic LBP = 23, control = 23) typed a standardized text passage at a computer work station for an hour. A seat pressure mat device was used to collect the seat pressure distribution data. Body discomfort was assessed using the Body Perceived Discomfort scale.
Results
Office workers with chronic LBP sat significantly more asymmetrically than their healthy counterparts. During 1-hour sitting, all workers appeared to assume slumped sitting postures after 20 minutes of sitting. Healthy workers had significantly more frequent postural shifts than chronic LBP workers during prolonged sitting.
Conclusion
Different sitting characteristics between healthy and chronic LBP participants during 1 hour of sitting were found, including symmetry of sitting posture and frequency of postural shift. Further research should examine the roles of these sitting characteristics on the development of LBP.
Keywords: chronic low back pain, office worker, sitting posture
1. Introduction
Low back pain (LBP) is a major problem for office workers. For example, the 1-year prevalent rate of LBP in Thai and Greek office workers was 34% and 38%, respectively [1], [2]. Between 14% and 23% of office workers in Thailand and Denmark reported a new onset of (acute) LBP during the 1-year follow-up [3], [4]. A review of the literature revealed that the annual prevalence of chronic LBP in general population ranged from 15% to 45%, with a point prevalence of 30% [5]. LBP is often the cause of significant physical and psychological health impairments. It also affects work performance and social responsibilities. As a result, LBP can be a great burden on patients and society [6]. Its total socioeconomic burden in the United States in 2006 exceeded US$100 billion [7], whereas in the Netherlands the total cost of LBP in 2007 was estimated at €3.5 billion [8].
Office workers are usually required to sit for long hours in front of a computer. Although prolonged sitting by itself was not associated with the risk of developing LBP [9], occupational groups exposed to poor postures while sitting for longer than half a day have a considerably increased risk of experiencing LBP [10]. Previous studies showed that, when sitting, individuals with LBP placed their spines closer to the end range than their healthy counterparts [11], [12]. Sitting closer to the end range of spinal movement may lead to increased passive system loading and reduced activity of spinal stabilizing muscles [11]. Individuals with LBP have also been shown to assume more static postures and have large/infrequent—rather than subtle/regular—spinal movements while sitting [13]. Prolonged, low-level static load on the back during sitting means continuous and relatively high activity of a fraction of the motor units in the muscles [14]. Contraction level of the trunk extensors of as low as 2% of maximum voluntary force has been shown to impair oxygenation and create waste product buildup of this musculature [15]. Prolonged sitting also induces discomfort in the low back [16], which is a strong predictor of LBP [17], and prolonged work with a computer was associated with two predictive factors of musculoskeletal problem, i.e., infrequent postural change and presence of discomfort while sitting [18].
Sitting is an active, not a static, phenomenon, involving a regular spinal movement or a postural change during sitting. Thus, short-duration investigations of sitting posture may not completely represent time-dependent biological responses to prolong sitting. A previous study showed that 40% of workers performing an hour of seated typing developed LBP [19]. Also, perceived low back discomfort significantly increased after 1 hour of sitting compared with baseline values, regardless of the sitting posture [20]. Seat pressure distribution measurement is one of the methods to study sitting for long periods. Although seat pressure distribution measurement is not a direct measure of sitting posture, several previous studies indicated a correlation between seat pressure distribution and sitting postures [21], [22], [23], [24]. High pressure at the ischial tuberosities has also been shown to be closely associated with high load to the spine [22], [23], [25], which may lead to accelerating disk degeneration and increased capsuloligamentous loading, resulting in LBP [26]. Seat pressure distribution measurement is a reliable and objective measure associated with the subjective rating of perceived discomfort [27]. The general purpose of this study was to investigate sitting posture, using seat pressure distribution measurement, and body perceived discomfort (BPD) during 1 hour of sitting in office workers with and without chronic LBP. Specifically, the primary aim was to describe the characteristics of average pressure (AP), peak pressure ratio (PP ratio), and frequency of postural shift during prolonged sitting. The secondary aim was to compare the PP ratio between comfortable/neutral sitting postures. The hypothesis of this study was that there were differences in seat pressure distribution characteristics and BPD between office workers with and without chronic LBP. Such information would provide basic information for the development of a guideline to promote healthy sitting to prevent LBP in those who need to engage in prolonged sitting.
2. Materials and methods
2.1. Participants
A pilot study with the same methodology to this study was conducted on a convenience sample of 20 full-time office workers (chronic LBP = 10; control = 10). The seat pressure data (i.e., AP, PP) and Borg CR-10 scale of discomfort were then used to calculate sample size , in which the α level was set at 0.05 and the statistical power was set at 80% [28]. A power analysis revealed that the study had sufficient power (80%) to detect a small to moderate effect (f = 0.212–0.322). As a result, a convenience sample of 46 (10 males, 36 females) full-time office workers were recruited into the study. Participants were divided into two groups: chronic LBP (n = 23) and control groups (n = 23). Age, sex, and body mass index (BMI) were matched between groups. There were 5 males and 18 females in each group. The definition of office workers in the present study were those working in an office environment and generally worked with a computer, participated in meetings, read documents, and contact people by telephone. Individuals in both chronic LBP and healthy groups were included in the study if they were 20–45 years of age and had reported sitting at least 4 hours on a working day. Healthy participants were included in the healthy group if they reported no LBP or a period of LBP pain lasting less than 1 day or LBP with pain intensity on a visual analogue scale ≤3 on a 100-mm scale over the 6 months prior to the testing period [29], [30]. Inclusion criteria for chronic LBP participants were having nonspecific chronic LBP and reporting prolonged sitting as one of the aggravating factors of the current LBP episode. Nonspecific chronic LBP was defined as LBP with or without pain radiating to one or both legs, in the absence of any specific pathological condition, has persisted for at least 3 months, and has resulted in pain on at least half the days in the past 6 months [31]. The area of LBP was defined according to the standardized Nordic questionnaire, i.e., the area between the 12th rib and the inferior gluteal folds, with or without radiation to one or both legs [32].
Both chronic LBP and healthy groups were excluded if they had current or past history of known spinal disorders, signs of neurological deficit (i.e., muscle weakness or loss/disturbance of sensation), osteoarthritis, rheumatoid arthritis, gout, kidney diseases, open wound or contusion at the buttocks or posterior thigh region, hemorrhoids, and current pregnancy. They were also excluded if they had a BMI of <18 kg/m2 or >23 kg/m2 [33]. A self-administered questionnaire was used to screen participants into the study. After they were given information about the study, all participants signed a consent form. The study was approved by the University Human Ethics Committee.
2.2. Equipment
The seat pressure distribution data were recorded using a seat pressure mat device (ConforMat; Tekscan Inc., Boston, MA, USA) with a specific-designed program (ConforMat Research, version 7.10c; Tekscan Inc.) and continuously sampled at a frame frequency of 5 Hz throughout the 1-hour period [34]. The device consists of 1024 (32 × 32) square (15 × 15 mm2) pressure sensing elements, which were calibrated with an upper limit threshold of 32.5 kPa (250 mmHg) and a lower limit threshold of 0.7 kPa (5 mmHg). The calibration was performed according to the manufacturer's instructions using a linear calibration method. The autoadjust sensitivity was selected. The seat pressure distribution was determined through three variables: the AP, PP, and dispersion index (DI), which are defined as follows.
-
(1)
AP is the total pressure divided by the total sitting contact surface area.
-
(2)
PP is the maximal pressure around ischial tuberosity. This is calculated between the maximum four adjacent sensors of seat pressure mapping. The PP ratio was calculated by the higher PP side to lower PP side. A higher PP ratio indicates more asymmetrical sitting between left and right sides during sitting;
-
(3)
DI, a relative measure of the load on the sitting surface, refers to the load on one tuberal zone divided by the total load on the sitting surface.
The seat pan was divided into two horizontal regions (anterior seat or thigh region and posterior seat or buttock region), which allowed for the description of the pressure distribution of each region. In addition, the locations of PP along the left/right on the seat were located.
The Borg CR-10 scale, a measuring tool for postural discomfort, was used to determine each participant's level of discomfort during 1-hour sitting. The Borg CR-10 scale and a body chart from a standardized Nordic questionnaire [32] were presented in such a way that the participants could indicate how much discomfort was felt in the low back (on a scale of 0–10; where 0 = no discomfort and 10 = extreme discomfort) [35].
2.3. Experimental procedure
At the beginning, participants were asked to change into legging pants without underwear and were instructed to complete the Borg CR-10 scale. After anthropometric measurement, participants sat on the adjustable office chair (Model E61B, Modernform Group Pub Co. Ltd., Bangkok, Thailand) with a pressure mapping device placed over the seat pan, which was made of polypropylene form (width × length × height = 45 cm × 50 cm × 11.5 cm) with a density of 40.4 kg/m3. The pressure mapping device was fixed to the seat pan using adhesive tape. The initial seat position was hips and knees at 90° flexion and feet in full contact with the floor. The distance between the monitor and the participant was about 18–30 inches, approximately at eye level. No backrest support or lumbar pad was used in this study. Participants were instructed to continuously type a standardized text passage at their own normal pace for an hour.
At the start of 1-hour sitting, each participant sat in a comfortable sitting posture for a minute then changed to a neutral sitting posture for another minute. The neutral sitting posture consisted of sitting with slight lumbar lordosis and a relaxed thorax [36]. After completion of sitting in the neutral sitting posture, participants were able to change their sitting posture freely with constraints imposed on leg crossing or lifting the buttocks. During the 1 hour of sitting, the Borg score was calculated at the 10th, 20th, 30th, 40th, 50th, and 60th minutes of the sitting period. Prior to actual testing, participants were given a practice run of about 5 minutes in a room with a constant temperature of 25°C. The purpose of the practice run was to allow participants to clearly understand the experiment procedure and to familiarize themselves with the experimental setup. As a result, the potential learning effect, which might affect the measurement outcomes, was minimized.
2.4. Reliability
Prior to data collection, the between-session repeatability of AP, PP, and Borg CR 10 scale of discomfort were assessed on 20 individuals (chronic LBP = 10, control = 10) from the pilot study. The data were collected according to the procedure described above. Each participant was tested twice on two separate days with at least a 24-hour lapse between measurements. The intraclass correlation coefficients (ICC; 3,1) were calculated [37].
2.5. Data analysis
The measurement outcomes in this study were AP, PP ratio, postural shift, and Borg scores. The raw pressure data (i.e., AP, PP) were collected, displayed, and extracted using the ConforMat Research, version 7.10c (Tekscan Inc.). To eliminate the artifact caused by movement of postural switching, the data that fell in the posture switching stage (1st minute for comfortable sitting posture and 2nd minute for neutral sitting posture) were discarded. Every 10 minutes of AP at anterior seat, AP at posterior seat, PP (left) and PP (right) data from the 1-hour sitting period (i.e., 3rd–10th minutes, 11th–20th minutes, 21st–30th minutes, 31st–40th minutes, 41st–50th minutes, and 51st–60th minutes) were retrieved for analysis. Data from the 3rd to 10th minutes were regarded as the baseline.
The DI data of both ischial tuberosities were analyzed and used to define postural shifts. The raw data from the pressure mapping device were exported in ASCII (American Standard Code for Information Interchange) format. A MATLAB script, version 7.12.0.635 (The MathWorks Inc., Nattick, MA, USA) was used to calculate a defined region that was expected to surround the ischial tuberosities; this region was defined by a zone of 6 × 6 pressure sensors (9 × 9 cm) to calculate the DI. The sum of the mean DI values of both ischial tuberosities and the ratio of the mean DI values of both ischial tuberosities were calculated to identify posture shifts in the sagittal and frontal planes, respectively. A posture shift was identified when the signal exceeded the threshold (±10% for both sagittal and frontal movements) [38]. Posture shifts that occurred within 1 minute were regarded as one posture shift. A combination of postural shifts in the frontal and sagittal planes were combined to represent the postural shifts in 1 hour of sitting [38].
2.6. Statistical analysis
Shapiro–Wilk test was performed to check the distribution of the data, and the results indicated normal distribution. The characteristics of participants were compared between groups using the independent t test for continuous data and the Chi-square test for noncontinuous data. The effects of sitting time, group, and their interaction on AP at anterior seat, AP at posterior seat, PP ratio, and frequency of postural shift were examined using a two-way analysis of variance (ANOVA) for repeated measures. When a significant interaction between independent variables was detected, the effect of each variable was examined separately using one-way ANOVA. The Bonferroni procedure was performed to determine whether two selected means significantly differed from each other.
The effects of sitting time, group, and their interaction on the Borg scores were investigated using a two-way analysis of covariance (ANCOVA), with the Borg score at the beginning as the covariate. When a significant interaction between independent variables was detected, the effect of each variable was examined separately using one-way ANCOVA. The relationships between the Borg score and seat pressure distribution variables and frequency of postural shift during 1 hour of sitting was examined using the Pearson correlation coefficients. The effects of comfortable/neutral sitting postures, group, and their interaction on PP ratio were examined using a two-way ANOVA for repeated measures. Statistical analyses were performed using the SPSS statistics software, version 17.0 (SPSS Inc., Chicago, IL, USA). For all tests, significance was determined using the 0.05 level.
3. Results
3.1. Test–retest reliability
The reliability results demonstrated moderate to excellent reliability of measurement variables (i.e., AP, PP, and Borg CR 10 scale of discomfort) with the ICC (3,1) scores ranging from 0.71 to 0.97 for AP, ranging from 0.72 to 0.97 for PP, and from 0.76 to 1.00 for Borg scores.
3.2. Characteristics of participants
Table 1 shows the characteristics of participants in both groups. There was no significant difference in any of the characteristics of the participants, except for the BPD scores at the low back. The Borg score of the low back at baseline in the chronic LBP group was significantly greater than that in the control group (p < 0.001).
Table 1.
Characteristics of participants (n = 46)
| Characteristics | Mean (SD) |
p | |
|---|---|---|---|
| Chronic LBP (n = 23) | Control (n = 23) | ||
| Age (y) | 29.6 (5.3) | 29.6 (5.1) | 1.00 |
| Sex (n) | |||
| Male | 5 | 5 | 1.00 |
| Female | 18 | 18 | |
| Weight (kg) | 56.1 (6.7) | 56.2 (6.3) | 0.937 |
| Height (cm) | 162.0 (7.6) | 162.7 (6.8) | 0.744 |
| BMI (kg/m2) | 21.2 (1.6) | 21.2 (1.5) | 0.995 |
| BPD at baseline | |||
| Neck | 0.4 (1.3) | 0 | 0.186 |
| Shoulder | 0.8 (1.6) | 0.2 (0.8) | 0.980 |
| Upper back | 0.5 (1.2) | 0.3 (1.1) | 0.612 |
| Low back | 1.5 (0.9) | 0.2 (0.6) | <0.001* |
| Thigh | 0.4 (1.5) | 0.4 (0.2) | 0.330 |
*p < 0.05.
BMI, body mass index; BPD, body perceived discomfort; LBP, low back pain; SD = standard deviation.
3.3. Seat pressure distribution during 1-hour sitting
Table 2 summarizes AP at anterior seat, AP at posterior seat, PP ratio, and frequency of postural shift during 1-hour sitting.
Table 2.
Mean (SD) of average pressure (AP) at anterior seat, AP at posterior seat, peak pressure (PP) ratio, and frequency of postural shift during 1-hour sitting in the chronic low back pain (LBP) and control groups
| Chronic LBP (n = 23) | Control (n = 23) | |
|---|---|---|
| AP at anterior seat (kPa) | 7.49 (0.94) | 7.51 (0.96) |
| AP at posterior seat (kPa) | 10.67 (1.18) | 10.42 (1.36) |
| PP ratio | 1.22 (0.15)* | 1.12 (0.10) |
| Frequency of postural shift (times/h) | 5.5 (3.80) | 9.6 (8.30) |
*p < 0.05.
3.3.1. AP at anterior seat
The two-way ANOVA indicated no significant effect for sitting time (F5,220 = 1.952, p = 0.09), group (F1,44 = 0.130, p = 0.91), and their interaction (F5,220 = 0.657, p = 0.68) on the AP at anterior seat during 1 hour of sitting.
3.3.2. AP at posterior seat
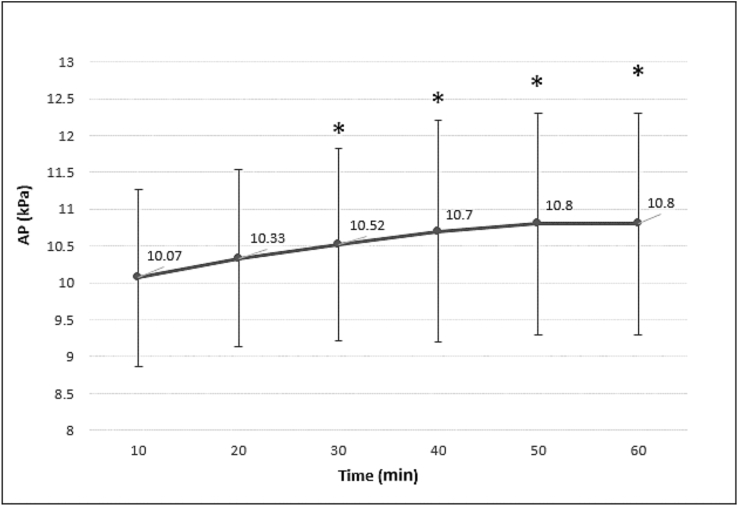
The two-way ANOVA indicated significant effects for sitting time (F5,220 = 11.690, p < 0.001) on the AP at posterior seat during 1-hour sitting. No significant effect for group (F1,44 = 0.390, p = 0.54) and interaction between sitting time and group (F5,220 = 0.380, p = 0.86) was detected. Post hoc Bonferroni tests indicated that AP at posterior seat increased progressively and significantly from baseline (i.e., the 3rd–10th minutes) after 20 minutes of sitting in both chronic LBP and control groups (p < 0.05; Fig. 1).
Fig. 1.
Mean (standard deviation) of average pressure (AP) distribution at posterior seat during 1-hour sitting of all participants (n = 46). * Significantly different from baseline, i.e., the 3rd–10th minutes; p < 0.05.
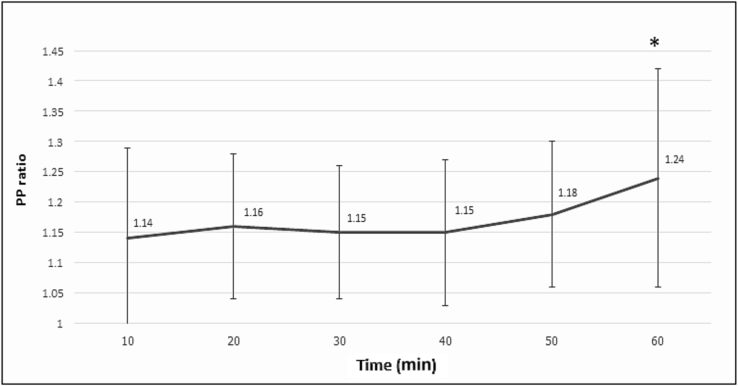
3.3.3. PP ratio
The two-way ANOVA indicated significant effects for sitting time (F5,220 = 9.290, p < 0.001) and group (F1,44 = 10.430, p = 0.002) on the PP ratio during 1-hour sitting. No significant effect for interaction between sitting time and group (F5,220 = 0.360, p = 0.87) was found. Post hoc Bonferroni tests showed that the PP ratio at the 51st–60th minutes was significantly greater than that at baseline (i.e., the 3rd–10th minutes) in both chronic LBP and control groups (p < 0.05; Fig. 2). In addition, the PP ratio in the chronic LBP group was significantly greater than that in the control group (p < 0.05; Table 2). Based on PP ratio data, which is an index of asymmetrical sitting posture, those with chronic LBP sat significantly more asymmetrically than their healthy counterparts during 1 hour of sitting.
Fig. 2.
Mean (standard deviation) of peak pressure (PP) ratio during 1-hour sitting of all participants (n = 46). * Significantly different from baseline, i.e., the 3rd–10th minutes; p < 0.05.
3.3.4. Frequency of postural shift
The two-way ANOVA indicated significant effects for sitting time (F5,220 = 3.370, p = 0.01) and group (F1,44 = 4.630, p = 0.04) on frequency of postural shift (the frontal + sagittal planes). No significant effect for the interaction between sitting time and group was found (F5,220 = 0.350, p = 0.88). Post hoc Bonferroni tests indicated that frequency of postural shifting after 40 minutes of sitting was significantly greater than that at baseline (i.e., the 3rd–10th minutes) in both chronic LBP and control groups [baseline mean (95% confidence interval, CI), 0.7 (0.4–1.0) times; 41th–50th minute: 1.3 (1.0–1.7) times; 51th–40th minute: 1.7 (1.2–2.1) times] (p < 0.05). In addition, frequency of postural shift in 10 minutes during 1-hour sitting in the chronic LBP group [0.9 (0.5–1.4) times] was significantly lower than that in the control group [1.6 (1.1–2.1) times] (p < 0.05).
3.4. Body perceived discomfort
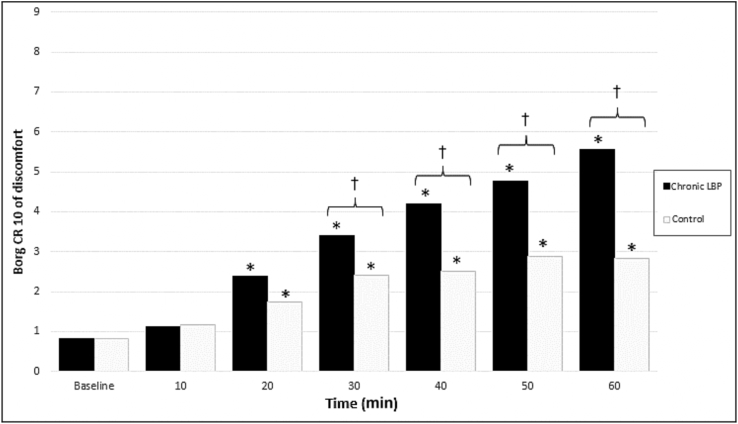
A two-way ANCOVA, with the Borg score at the beginning as the covariate, indicated significant effects for sitting time (F6,258 = 63.0, p < 0.001), group (F1,43 = 14.940, p < 0.001), and their interaction (F6,258 = 12.310, p < 0.001) on Borg scores at the low back. Thus, follow-up analyses were performed using one-way ANCOVA to investigate the effect of sitting time within each group and the effect of group for each sitting period.
Investigation of the effect of sitting time in each group revealed that Borg scores at the low back were significantly affected by the sitting time for both groups (F6,3 = 39.10, p < 0.001 for chronic LBP; F6,38 = 7.310, p = 0.001 for control group). Post hoc Bonferroni tests showed that the Borg scores in both chronic LBP and control groups were significantly greater than those at baseline (i.e., at the start of testing) after 10 minutes of sitting (p < 0.05; Fig. 3).
Fig. 3.
Borg score at the low back during 1-hour sitting for chronic low back pain (LBP) and control groups. * Significantly different from baseline (i.e., at the start of testing). † Significantly different between groups; p < 0.05.
Investigation of the effect of group on each time point revealed that Borg scores at the low back were significantly affected by group after 20 minutes of sitting (p < 0.05). Post hoc Bonferroni tests indicated that the Borg scores in the chronic LBP group were significantly greater than those in the control group (p < 0.05; Fig. 3).
3.5. Relationships between BPD and AP, PP ratio, and frequency of postural shift
Table 3 shows the results of the correlations between the Borg score and seat pressure distribution variables and frequency of postural shift during 1 hour of sitting. Significant correlations between the Borg score and AP at posterior seat and frequency of postural shift during 1 hour of sitting were detected (p < 0.05).
Table 3.
Pearson correlation coefficients between Borg score and seat pressure distribution variables [i.e., average pressure (AP) at anterior seat, AP at posterior seat, and peak pressure (PP) ratio] and frequency of postural shift of all participants (n = 46)
| Borg score (r) | |
|---|---|
| Borg score | 1 |
| AP at anterior seat | 0.250 |
| AP at posterior seat | 0.996* |
| PP ratio | 0.414 |
| Frequency of postural shift | 0.929* |
*p < 0.05.
3.6. Comfortable and neutral sitting posture
The two-way ANOVA indicated significant effects for sitting posture (F1,44 = 11.360, p = 0.002) and group (F1,44 = 11.220, p < 0.02). No significant effect for interaction between sitting posture and group was found (F1,44 = 0.130, p = 0.72). Post hoc Bonferroni tests revealed that the PP ratios for both comfortable and neutral sitting postures in the chronic LBP group were significantly greater than those for the control group [chronic LBP group: mean (95% CI) = 1.24 (1.18–1.3); control group: 1.1 (1.0–1.63)] (p < 0.05).
In addition, the PP ratio in neutral sitting posture was significantly lower than that in the comfortable sitting posture in both groups [neutral sitting posture: mean (95% CI) = 1.14 (1.1–1.18); comfortable sitting posture = 1.2 (1.15–1.36)] (p < 0.05).
4. Discussion
The findings of this study demonstrate that office workers with chronic LBP sat significantly more asymmetrically, i.e., sitting with trunk leaning toward either left or right side, than their healthy counterparts in both comfortable and neutral sitting postures. During 1 hour of sitting, both chronic LBP and healthy workers appeared to assume slumped sitting postures after 20 minutes of sitting, which may partly be explained by increased discomfort experienced in the low back. Healthy workers had significantly more frequent postural shifts than chronic LBP workers during prolonged sitting, despite chronic LBP participants reporting significantly greater low back discomfort than their healthy counterparts. Significantly greater asymmetrical sitting posture and more frequent postural shift were found toward the end of the 1-hour sitting period in both chronic LBP and control groups.
Office workers with chronic LBP had significantly greater PP ratio, which is an index of asymmetrical sitting posture, than their healthy counterparts in both comfortable and neutral sitting postures. Differences in PP ratio between chronic LBP and control groups remained throughout the 1-hour sitting period. Patients with chronic LBP have been shown to demonstrate poorer postural control of the lumbar spine than healthy controls [39]. Pelvic asymmetry has also been shown to cause higher stress on the lumbar spine in individuals with LBP [40] and changes in soft tissue tightness [41], thus making the spine susceptible to injury. Neutral sitting posture, consisting of sitting with slight lumbar lordosis and a relaxed thorax, has been proposed as an optimal seat posture at work [36], [42]. Neutral sitting posture was associated with increased internal oblique and transversus abdominis muscles activity compared with slumped sitting posture [11], [16]. The current study showed that asymmetry in the sitting posture in chronic LBP participants reduced significantly when they sat in a neutral sitting posture, although it still persisted and was greater than that in healthy participants. The results lend further support to the notion that the neutral sitting posture, which leads to more symmetrical sitting posture, is healthy for the low back.
After 20 minutes of sitting, both participants with and without chronic LBP assumed sitting posture with significantly increased AP at posterior seat, indicating pelvic backward tilting or slumped sitting posture. Sitting with backward leaning is usually achieved by a backward pelvic rotation, resulting in lumbar kyphosis, and less than 25% of the body weight is transmitted to the floor [43], [44]. Backward rotation caused by long hours spent at the visual display terminal has been shown to generate load on the lumbar spine and increase intradiskal pressure [24], [45], [46]. When the seat position is not optimal, more muscular activity may be needed for stabilization resulting in a distinctly larger pressure in the disk [24]. Also, internal oblique and transversus abdominis muscle fatigue was induced by slumped sitting posture after 1 hour of sitting in office workers [20]. Patients who habitually adopt passive spinal postures or slump may decondition their lumbar stabilizing muscles [47], leading to increased passive system loading, injury, and pain [48]. Sustained stretch of passive lumbar structures in combination with essentially silent muscles may exacerbate LBP in office workers [49]. One of several identified interventions to reduce the onset and severity of LBP included periodic rest breaks. Previous studies suggested that frequent, short, rest breaks resulted in short-term decrease in both discomfort and postural immobility [18], [19]. In this study, low back discomfort in both chronic LBP and control groups was significantly greater than that at baseline after 10 minutes of sitting, and a significant correlation between Borg score at the low back and AP at posterior seat was detected. Thus, based on the findings, it is hypothesized that sitting for as short as 10 minutes has a deteriorative effect on the low back by causing low back discomfort, which consequently induces the posterior seat posture.
In terms of postural shift, healthy workers had more frequent postural shifts (the combination of shift in the frontal and sagittal planes) than chronic LBP workers by 43% during 1 hour of sitting. The frequency of postural shift in healthy participants reported in the present study (9.6 ± 8.3 times/h) was in line with a previous study (7.8 ± 5.2 times/h) [35]. The current study also found a significant correlation between Borg score at the low back and frequency of postural shift. The results concur with a study by Dunk and Callaghan [34], who reported less frequent postural shift in individuals with LBP compared with healthy individuals. Excessive load transmission and tissue deformation associated with prolonged loading in a certain posture may contribute to degenerative change in spinal tissues [50], [51]. Postural shift has been found to increase subcutaneous oxygen saturation, which positively influences tissue viability [38]. Also, postural shifts may alleviate low back discomfort and LBP during prolonged sitting through alternating activity between different parts of the trunk muscles [14]. However, it is interesting to note that despite chronic LBP workers having significantly greater Borg scores than healthy workers after 20 minutes of sitting, chronic LBP workers changed their sitting postures less frequently than their healthy counterparts during 1-hour sitting. The findings shed some light on the notion that sitting characteristics, particularly frequency of postural shift, may partly relate to the etiology of LBP in those required to sit for long periods.
A major strength of this study is that the characteristics of prolonged sitting were objectively and continuously assessed using a seat pressure mat device distribution measurement. Additionally, because LBP among office workers is unlikely to originate from identical causes, a distinct group of participants with chronic LBP was selected for the present study—that is, those reporting sitting for at least 4 hours on a working day and prolonged sitting as one of aggravating factors of their current LBP episode. However, at least three main limitations are worth noting. First, owing to the cross-sectional design of the present study, it is not possible to establish a causal relationship between exposure and outcome. Only the association between exposure and outcome was examined. Therefore, future study with a prospective study design is required to validate the findings of this study. Second, in this study, a healthy participant was defined as one reporting no LBP or a period of LBP pain lasting less than 1 day or LBP with pain intensity on visual analogue scale ≤3 on a 100-mm over the 6 months prior to the testing. Chronic LBP participants were those experiencing nonspecific LBP that persisted for at least 3 months and which has resulted in pain on at least half the days in the past 6 months. Only those with a BMI between 18 and 23 kg/m2 were included in this study. Different results may emerge with different definitions of healthy and symptomatic cases. Third, the task and sitting postures tested in this study were controlled. Participants were asked to continuously type a standardized text passage and were not allowed to cross their legs, lift their buttocks or use a back rest during testing. Variations in task performed and how a person sits may exist and influence outcome measurement. Further research on the effect of task and sitting posture on seat pressure distribution and perceived body discomfort is recommended.
In summary, the results of the present study showed that, for both comfortable and neutral sitting postures, chronic LBP workers sat more asymmetrically than their healthy counterparts. During 1 hour of sitting, office workers with and without chronic LBP appeared to assume slumped sitting posture after 20 minutes of sitting. Healthy participants had significantly more frequent postural shifts than chronic LBP participants. Greater asymmetrical sitting posture and more frequent postural shift was detected toward the end of the 1-hour sitting period in both chronic LBP and control groups. Positive relationships between BPD and slump sitting posture and frequency of postural shift were also found during 1 hour of sitting in both chronic LBP and control groups. Further research should examine the roles of these sitting characteristics on the development of LBP in workers who are required to sit for long hours.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Authors' contributions
The authors have contributed in the following ways: AN provided concept/research design, data collection, data analysis, and manuscript writing. PJ provided concept/research design and manuscript writing. All authors read and approved the final manuscript.
Acknowledgments
This study was funded by the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund, GCUGR1125582046M).
References
- 1.Janwantanakul P., Pensri P., Jiamjarasrangsri V., Sinsongsook T. Prevalence of self-reported musculoskeletal symptoms among office workers. Occup Med (Lond) 2008;58:436–438. doi: 10.1093/occmed/kqn072. [DOI] [PubMed] [Google Scholar]
- 2.Spyropoulos P., Papathanasiou G., Georgoudis G., Chronopoulos E., Koutis H., Koumoutsou F. Prevalence of low back pain in Greek public office workers. Pain Physician. 2007;10:651–659. [PubMed] [Google Scholar]
- 3.Juul-Kristensen B., Søgaard K., Strøyer J., Jensen C. Computer users' risk factors for developing shoulder, elbow and back symptoms. Scand J Work Environ Health. 2004;30:390–398. doi: 10.5271/sjweh.827. [DOI] [PubMed] [Google Scholar]
- 4.Sitthipornvorakul E., Janwantanakul P., Lohsoonthorn V. The effect of daily walking steps on preventing neck and low back pain in sedentary workers: a 1-year prospective cohort study. Eur Spine J. 2015;24:417–424. doi: 10.1007/s00586-014-3577-3. [DOI] [PubMed] [Google Scholar]
- 5.Manchikanti L., Singh V., Datta S., Cohen S.P., Hirsch J.A. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12:E35–E70. [PubMed] [Google Scholar]
- 6.Manchikanti L., Singh V., Falco F.J., Benyamin R.M., Hirsch J.A. Epidemiology of low back pain in adults. Neuromodulation. 2014;17:3–10. doi: 10.1111/ner.12018. [DOI] [PubMed] [Google Scholar]
- 7.Katz J.N. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88:21–24. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 8.Lambeek L.C., van Tulder M.W., Swinkels I.C.S., Koppes L.L.J., Anema J.R., van Mechelen W. The trend in total cost of back pain in the Netherlands in the period 2002 to 2007. Spine (Phila Pa 1976) 2011;36:1050–1058. doi: 10.1097/BRS.0b013e3181e70488. [DOI] [PubMed] [Google Scholar]
- 9.Kwon B.K., Roffey D.M., Bishop P.B., Dagenais S., Wai E.K. Systematic review: occupational physical activity and low back pain. Occup Med. 2011;61:541–548. doi: 10.1093/occmed/kqr092. [DOI] [PubMed] [Google Scholar]
- 10.Lis A., Black K., Korn H., Nordin M. Association between sitting and occupational LBP. Eur Spine J. 2007;16:283–298. doi: 10.1007/s00586-006-0143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Sullivan P.B., Mitchell T., Bulich P., Waller R., Holte J. The relationship between posture and back muscle endurance in industrial workers with flexion-related low back pain. Man Ther. 2006;11:264–271. doi: 10.1016/j.math.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Womersley L., May S. Sitting posture of subjects with postural backache. J Manipulative Physiol Ther. 2006;29:213–218. doi: 10.1016/j.jmpt.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 13.O'Sullivan K., O'Keeffe M., O'Sullivan L., O'Sullivan P., Dankaerts W. The effect of dynamic sitting on the prevention and management of low back pain and low back discomfort: a systematic review. Ergonomics. 2012;55:898–908. doi: 10.1080/00140139.2012.676674. [DOI] [PubMed] [Google Scholar]
- 14.van DieËn J.H., De Looze M.P., Hermans V. Effects of dynamic office chairs on trunk kinematics, trunk extensor EMG and spinal shrinkage. Ergonomics. 2001;44:739–750. doi: 10.1080/00140130120297. [DOI] [PubMed] [Google Scholar]
- 15.McGill S., Hughson R., Parks K. Lumbar erector spinae oxygenation during prolonged contractions: implications for prolonged work. Ergonomics. 2000;43:486–493. doi: 10.1080/001401300184369. [DOI] [PubMed] [Google Scholar]
- 16.Waongenngarm P., Rajaratnam B.S., Janwantanakul P. Perceived body discomfort and trunk muscle activity in three prolonged sitting postures. J Phys Ther Sci. 2015;27:2183–2187. doi: 10.1589/jpts.27.2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamberg-van Reenen H.H., van der Beek A.J., Blatter B.M., van der Grinten M.P., van Mechelen W., Bongers P.M. Does musculoskeletal discomfort at work predict future musculoskeletal pain? Ergonomics. 2008;51:637–648. doi: 10.1080/00140130701743433. [DOI] [PubMed] [Google Scholar]
- 18.Fenety A., Walker J.M. Short-term effects of workstation exercises on musculoskeletal discomfort and postural changes in seated video display unit workers. Phys Ther. 2002;82:578–589. [PubMed] [Google Scholar]
- 19.Sheahan P.J., Diesbourg T.L., Fischer S.L. The effect of rest break schedule on acute low back pain development in pain and non-pain developers during seated work. Appl Ergon. 2016;53:64–70. doi: 10.1016/j.apergo.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Waongenngarm P., Rajaratnam B.S., Janwantanakul P. Internal oblique and transversus abdominis muscle fatigue induced by slumped sitting posture after 1 hour of sitting in office workers. Saf Health Work. 2016;7:49–54. doi: 10.1016/j.shaw.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koo T.K.K., Mak A.F.T., Lee Y.L. Posture effect on seating interface biomechanics: comparison between two seating cushions. Arch Phys Med Rehabil. 1996;77:40–47. doi: 10.1016/s0003-9993(96)90218-x. [DOI] [PubMed] [Google Scholar]
- 22.Makhsous M., Lin F., Bankard J., Hendrix R.W., Hepler M., Press J. Biomechanical effects of sitting with adjustable ischial and lumbar support on occupational low back pain: evaluation of sitting load and back muscle activity. BMC Musculoskelet Disord. 2009;10:17. doi: 10.1186/1471-2474-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Geffen P., Reenalda J., Veltink P.H., Koopman B.F.J.M. Decoupled pelvis rotation in sitting: a passive motion technique that regulates buttock load associated with pressure ulcer development. J Biomech. 2009;42:1288–1294. doi: 10.1016/j.jbiomech.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 24.Zenk R., Franz M., Bubb H., Vink P. Technical note: spine loading in automotive seating. Appl Ergon. 2012;43:290–295. doi: 10.1016/j.apergo.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Gyi D.E., Porter J.M., Robertson N.K.B. Seat pressure measurement technologies: considerations for their evaluation. Appl Ergon. 1998;29:85–91. doi: 10.1016/s0003-6870(97)00036-7. [DOI] [PubMed] [Google Scholar]
- 26.Marras W.S., Davis K.G., Ferguson S.A., Lucas B.R., Gupta P. Spine loading characteristics of patients with low back pain compared with asymptomatic individuals. Spine (Phila Pa 1976) 2001;26:2566–2574. doi: 10.1097/00007632-200112010-00009. [DOI] [PubMed] [Google Scholar]
- 27.De Looze M.P., Kuijt-Evers L.F.M., Van Dieën J. Sitting comfort and discomfort and the relationships with objective measures. Ergonomics. 2003;46:985–997. doi: 10.1080/0014013031000121977. [DOI] [PubMed] [Google Scholar]
- 28.Portney L.G., Watkins M.P. 3rd ed. Pearson/Prentice Hall; Upper Saddle River, NJ: 2009. Foundations of clinical research: applications to practice. [Google Scholar]
- 29.Hush J., Michaleff Z., Maher C., Refshauge K. Individual, physical and psychological risk factors for neck pain in Australian office workers: a 1-year longitudinal study. Eur Spine J. 2009;18:1532–1540. doi: 10.1007/s00586-009-1011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsauo J.-Y., Jang Y., Du C.-L., Liang H.-W. Incidence and risk factors of neck discomfort: a 6-month sedentary-worker cohort study. J Occup Rehabil. 2007;17:171–179. doi: 10.1007/s10926-007-9076-1. [DOI] [PubMed] [Google Scholar]
- 31.Deyo R.A., Dworkin S.F., Amtmann D., Andersson G., Borenstein D., Carragee E., Carrino J., Chou R., Cook K., DeLitto A., Goertz C., Khalsa P., Loeser J., Mackey S., Panagis J., Rainville J., Tosteson T., Turk D., Von Korff M., Weiner D.K. Focus article report of the NIH Task Force on Research Standards for Chronic Low Back Pain. Clin Biomech. 2014;30:701–712. doi: 10.1097/AJP.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 32.Kuorinka I., Jonsson B., Kilbom A., Vinterberg H., Biering-Sorensen F., Andersson G., Jørgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 33.Anuurad E., Shiwaku K., Nogi A., Kitajima K., Enkhmaa B., Shimono K., Yamane Y. The new BMI criteria for Asians by the regional office for the Western Pacific Region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health. 2003;45:335–343. doi: 10.1539/joh.45.335. [DOI] [PubMed] [Google Scholar]
- 34.Dunk N.M., Callaghan J.P. Gender-based differences in postural responses to seated exposures. Clin Biomech. 2005;20:1101–1110. doi: 10.1016/j.clinbiomech.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16:55–58. doi: 10.5271/sjweh.1815. [DOI] [PubMed] [Google Scholar]
- 36.O'Sullivan P.B., Dankaerts W., Burnett A.F., Farrell G.T., Jefford E., Naylor C.S., O'Sullivan K.J. Effect of different upright sitting postures on spinal–pelvic curvature and trunk muscle activation in a pain-free population. Spine (Phila Pa 1976) 2006;31:E707–E712. doi: 10.1097/01.brs.0000234735.98075.50. [DOI] [PubMed] [Google Scholar]
- 37.Shrout P.E.F.J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 38.Reenalda J., Van Geffen P., Nederhand M., Jannink M., Ijzerman M., Rietman H. Analysis of healthy sitting behavior: interface pressure distribution and subcutaneous tissue oxygenation. J Rehabil Res Dev. 2009;46:577–586. doi: 10.1682/jrrd.2008.12.0164. [DOI] [PubMed] [Google Scholar]
- 39.Radebold A., Cholewicki J., Polzhofer G.K., Greene H.S. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine (Phila Pa 1976) 2001;26:724–730. doi: 10.1097/00007632-200104010-00004. [DOI] [PubMed] [Google Scholar]
- 40.Al-Eisa E., Egan D., Deluzio K., Wassersug R. Effects of pelvic asymmetry and low back pain on trunk kinematics during sitting: a comparison with standing. Spine (Phila Pa 1976) 2006;31:135–143. doi: 10.1097/01.brs.0000201325.89493.5f. [DOI] [PubMed] [Google Scholar]
- 41.Cibulka M.T. Understanding sacroiliac joint movement as a guide to the management of a patient with unilateral low back pain. Man Ther. 2002;7:215–221. doi: 10.1054/math.2002.0474. [DOI] [PubMed] [Google Scholar]
- 42.O'Sullivan K., O'Dea P., Dankaerts W., O'Sullivan P., Clifford A., O'Sullivan L. Neutral lumbar spine sitting posture in pain-free subjects. Man Ther. 2010;15:557–561. doi: 10.1016/j.math.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 43.Harrison D., Harrison S., Croft A., Harrison D., Troyanovich S. Sitting biomechanics: Part I. Review of the literature. J Manipulative Physiol Ther. 1999;22:594–609. doi: 10.1016/s0161-4754(99)70020-5. [DOI] [PubMed] [Google Scholar]
- 44.Pope M.H., Goh K.L., Magnusson M.L. Spine ergonomics. Annu Rev Biomed Eng. 2002;4:49–68. doi: 10.1146/annurev.bioeng.4.092101.122107. [DOI] [PubMed] [Google Scholar]
- 45.Wu C.S., Miyamoto H., Noro K. Research on pelvic angle variation when using a pelvic support. Ergonomics. 1998;41:317–327. doi: 10.1080/001401398187062. [DOI] [PubMed] [Google Scholar]
- 46.Sato K., Kikuchi S., Yonezawa T. In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine (Phila Pa 1976) 1999;24:2468–2474. doi: 10.1097/00007632-199912010-00008. [DOI] [PubMed] [Google Scholar]
- 47.O'Sullivan P.B., Grahamslaw K.M., Kendell M., Lapenskie S.C., Moller N.E., Richards K.V. The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine (Phila Pa 1976) 2002;27:1238–1244. doi: 10.1097/00007632-200206010-00019. [DOI] [PubMed] [Google Scholar]
- 48.Cholewicki J., McGill S.M. Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clin Biomech (Bristol, Avon) 1996;11:1–15. doi: 10.1016/0268-0033(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 49.Mork P.J., Westgaard R.H. Back posture and low back muscle activity in female computer workers: a field study. Clin Biomech (Bristol, Avon) 2009;24:169–175. doi: 10.1016/j.clinbiomech.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 50.Hedman T.P., Fernie G.R. Mechanical response of the lumbar spine to seated postural loads. Spine. 1997;22:734–743. doi: 10.1097/00007632-199704010-00004. [DOI] [PubMed] [Google Scholar]
- 51.McGill S.M., Brown S. Creep response of the lumbar spine to prolonged full flexion. Clin Biomech. 1991;7:43–46. doi: 10.1016/0268-0033(92)90007-Q. [DOI] [PubMed] [Google Scholar]