Abstract
The area southeast of Iran still copes with malaria as an unstable infectious disease and includes the most autochthonous malaria reports in the country. This comprehensive study was carried out for the evaluation of environmental factors, welfare indicators and health facilities on the malaria situation before and at the beginning of a pre-elimination programme in this area. The probable factors affecting the malaria situation, including the water-pipe network, electricity, rainfall, long-lasting integrated nets (LLINs), indoor residual spraying and malaria diagnosis-treatment centres were analysed using SPSS software. The Pearson correlation test showed no significant correlation between some factors such as piped water networks, annual precipitation, number of sprayed villages and autochthonous cases as well as autochthonous foci. But a significant correlation between electricity coverage, number of diagnoses of malaria-treatment centres and autochthonous cases\foci was observed. Also, the number of distributed LLINs didn’t have any correlation with the number of total malaria cases, but a significant correlation between LLINs and autochthonous foci was seen. Detailed studies on the correlation of various variables, such as piped water, spraying coverage and number of malaria diagnosis centres, with the malaria situation is limited in Asia and other parts of the world. This study and others like it can help malaria managers and directors in the more accurate allocation of financial resources.
Keywords: Malaria, Environmental factors, Welfare, Health facility, Iran
Introduction
Malaria is considered a serious infectious disease in tropical and subtropical regions (Phillips 2001). It is estimated that 3.4 billion people inhabit regions with malaria risk. Based on the annual malaria report of the World Health Organization (WHO), malaria is currently endemic in 104 countries. Despite the efforts that have been made for malaria control and elimination, nearly 214 million cases and 438 thousands deaths (with most in children under 5 years of age) have occurred due to this disease (WHO 2016).
The Eastern Mediterranean Region (EMR) has about 276 million populations at risk of malaria, living in eight countries. The number of confirmed malaria cases was 1.5 million and 960 deaths in 2014. However the malaria trends in cases and the deaths from malaria showed significant reduction compared with the year 2000. On the other hand malaria control funding by WHO was increased from US$ 59 million in 2005 to US$ 120 million in 2014. Some interventions such as distribution of antimalarial medicines and insecticide-treated mosquito nets (ITNs) were widely done in some of countries in this region (WHO 2016).
Iran, which is located in the EMR, has a low rate of malaria cases as well as being classified in the elimination phase (WHO 2016). In this phase there isn’t any local transmission of Plasmodium vivax (P. vivax) and/or P. falciparum in specific geographic areas. This country started its elimination program as a pre-elimination phase in 2009 (Hemami et al. 2013). Nevertheless, malaria in this country is still considered one of the endemic diseases which have been limited to south and southeastern.
In the past decade, the autochthonous malaria cases have been reported only from three provinces, including Sistan-Baluchestan, Hormozgan and Kerman (Izadi 2016; Yeryan et al. 2016; Hanafi-Bojd et al. 2012).
Sistan-Baluchestan Province (also named Sistan and Baluchistan or Sistan va Baluchestan), located south east of Iran, includes the most (42–60 %) malaria cases. In line with WHO policy, the distribution of free long-lasting integrated nets (LLINs), indoor residual spraying (IRS), establishment of malaria diagnosis-treatment centers and other interventions, have been widely implemented by the Ministry of Health in recent years. Also, welfare facilities such as electricity and the water-pipe network, as well as heath facilities have been expanded and improved by the government in the past decade (Tasnim 2015). The evaluation of the all mentioned facilities on malaria situation (autochthonous cases and foci) will be important for health systems. Also the epidemiological studies are valuable for malaria control and planning of its elimination (Greenwood 2008).
So, in order for awareness of the effective factors on reduction of malaria and for better planning of elimination of malaria, this comprehensive study was carried out for the evaluation of several probable factors, such as environmental factors, welfare indicators and health facilities on the malaria situation before and at the beginning of a pre-elimination program in southeastern Iran.
Materials and methods
Study area
This study was conducted over an extensive part of southeast Iran including eight districts (Zahedan, Khash, Saravan, Iranshahr, Sarbaz, Nikshahr, Chabahar and Konarak) in Sistan-Blauchestan Province (Fig. 1). This province has a long border with Pakistan and Afghanistan as countries also involved with malaria (Basseri et al. 2008). Also, due to the subtropical climate, monsoon winds and summer rainfall, it is suitable for the existence of vectors and malaria transmission (Basseri et al. 2010; Nejati et al. 2013).
Fig. 1.
Map of study area, Sistan-Baluchestan Province, Southeast of Iran
Epidemiological survey
This is a descriptive analytical study which was conducted over 5 years (2006–2010), including before and at the beginning of the malaria elimination program.
At first, the probable factors in malaria reduction were exploited via literature reviews. Some of them, including electricity, rainfall, LLINs, IRS and malaria diagnosis-treatment centers, were selected (Izadi 2016; Keiser et al. 2004; Magalhães et al. 2012; Rehman et al. 2013; Thomson et al. 2005). Also, we evaluated the effect of the water-pipe network on malaria situation as a subject with less references and reasons.
Malaria data, including parasite species, patients’ nationality, number of cases under 5 years of age, indigenous\imported, number of autochthonous vivax, number of autochthonous falciparum, number of foci with autochthonous vivax and number of foci with autochthonous falciparum, were collected from forms available in the Department of Communicable Disease Control and Prevention in the province health centre. These forms had been daily completed by physicians\health workers in hospitals and/or were received via phone reports from health centers of the different districts. The number of free-given LLINs, IRS coverage and number of malaria diagnoses and treatment centers, was also obtained from archived folders in the malaria vector control section in the province health centre. The rainfall data was received from the province’s meteorological organization. Electricity and the situation of water piped networks were taken from the Environmental Health Department in the province health centre. After that, obtained data were analyzed using the Pearson’s correlation co-efficient and other statistical tests in SPSS software.
Results
Malaria indicators
During the 5 year period 2006–2010, the Annual Parasite Incidence showed a considerable drop from 4.1 (per 1000 of the population) in 2006 to 0.9 in 2010. In addition, the number of autochthonous cases of P. vivax and P. falciparum, foci with local transmission of P. vivax and P. falciparum, also decreased during the study period. As the risk group, number of children under 5 years of age infected with malaria declined in 2010 compared with 2006 (Table 1).
Table 1.
Malaria indicators, before and at the Beginning of Pre-Elimination Program, Southeastern Iran, 2006–2010
| Year/index | 2006 | 2007 | 2008 | 2009 | 2010 |
|---|---|---|---|---|---|
| Total of malaria cases | 8300 | 8657 | 7296 | 4390 | 2140 |
| API | 4.1 | 4.2 | 3.3 | 2 | 0.9 |
| Parasite | |||||
| P. vivax | 7307 | 7358 | 6483 | 3921 | 1789 |
| P. falciparum | 896 | 1208 | 697 | 363 | 284 |
| Mix | 97 | 91 | 116 | 106 | 65 |
| Nationality | |||||
| Iranian | 6903 | 7233 | 5552 | 3394 | 1461 |
| Foreign | 1397 | 1424 | 1744 | 996 | 679 |
| Epidemiology | |||||
| Indigenous | 5981 | 6000 | 4671 | 3551 | 1182 |
| Imported | 2276 | 2575 | 2581 | 1399 | 936 |
| Cases under 5 years age | |||||
| P. vivax | 594 | 621 | 425 | 373 | 129 |
| P. falciparum | 54 | 85 | 55 | 19 | 14 |
| No. of autochthonous vivax | 5980 | 6092 | 4523 | 2997 | 1106 |
| No. of autochthonous falciparum | 542 | 684 | 292 | 185 | 116 |
| No. of foci with autochthonous vivax | 871 | 936 | 1084 | 688 | 397 |
| No. of foci with autochthonous falciparum | 135 | 202 | 222 | 104 | 38 |
Welfare indicators
Access to piped water
During these 5 years, the percentages of rural households with access to the drinking piped water network increased from 72.6 % in 2006 to 76.1 % in 2010 (Table 2). The Pearson correlation test showed no significant correlation between piped-water networks and vivax autochthonous cases and falciparum autochthonous cases, respectively (p = 0.058), (p = 0.06). Also, no significant correlation between this factor and number of vivax autochthonous foci (p = 0.29) and falciparum autochthonous foci (p = 0.23), was observed.
Table 2.
Some probable factors affecting malaria situation, southeastern Iran, 2006–2010
| Probable factors/years | 2006 | 2007 | 2008 | 2009 | 2010 |
|---|---|---|---|---|---|
| Welfare indicators | |||||
| Percent of households with access to piped water | 72.6 | 69.6 | 74.3 | 74.8 | 76.1 |
| Percent of households have electricity | 59.4 | 61.3 | 67.9 | 70 | 70 |
| Environmental indicator | |||||
| Annual rainfall | 902.1 | 2094.6 | 697.7 | 1081.2 | 774.1 |
| Average of annual rainfall | 137 | 278 | 114 | 170 | 79 |
| Health facilities | |||||
| Distributed bed nets | 500 | 27,100 | 13,072 | 42,772 | 169,718 |
| No of sprayed villages | 520 | 485 | 509 | 468 | 843 |
| Percent of sprayed villages | 9.1 | 8.5 | 8.9 | 8.1 | 14 |
| Spraying coverage | 90 | 90 | 89 | 91 | 91 |
| No. of malaria diagnosis and treatment centers | 118 | 116 | 119 | 161 | 186 |
Access to electricity
The villages with electricity have increased during the past 5 years (Table 2). The statistical analysis showed that there was a significant correlation between electricity coverage and vivax autochthonous cases (p = 0.050) as well as falciparum autochthonous cases (p = 0.02).
Environmental indicator
Rainfall
The rate of annual precipitation decreased from 2006 to 2010 in Sistan-Baluchestan Province. In Table 2, the amounts of annual rainfall and their average have been shown.
Not significant correlation was observed between rainfall and total malaria cases (p = 0.43), as well as vivax autochthonous cases (p = 0.38) and falciparum autochthonous (p = 0.16) via the Pearson test. This research also showed that there wasn’t a significant correlation between the amount of rainfall and the number of vivax autochthonous foci (p = 0.70), and falciparum autochthonous foci (p = 0.53).
Health facilities
Bed net distribution
During the current study, a total of 253,162 LLINs were distributed free of cost in rural areas. Their distribution showed a 339-fold increase as a remarkable and considerable point in 2010 compared with 2006 (Table 2).
Although the Pearson test did not show a significant correlation between the number of distributed LLINs and the number of total malaria cases in the study period (p = 0.50), there was a significant correlation between the number of distributed LLINs and the number of vivax autochthonous foci (p = 0.041).
Indoor residual spraying coverage
The number and per cent of sprayed villages during the 5 years of the study is shown in Table 2. In addition to an increasing per cent of sprayed villages, rates of sprayed coverage have increased too.
Although the number and percentage of villages covered by IRS has increased within the 5 years (2006–2010), a significant correlation was not observed between the number of sprayed villages and the number of vivax autochthonous cases (p = 0.16), the number of falsiparum autochthonous cases (p = 0.37), the number of vivax autochthonous foci (p = 0.12) and also the number of falciparum autochthonous foci (p = 0.17).
The number of malaria diagnoses: treatment centers
The number of malaria diagnoses-treatment centres increased from 118 in 2006 to 186 in 2010 (Table 2).
Based on the Pearson test, there was a significant correlation between the number of malaria diagnoses-treatment centres and the number of malaria cases (p = 0.001). Also, there was a significant correlation between the number of malaria diagnoses-treatment centres and the number of vivax autochthonous cases (p = 0.009), as well as the number of vivax autochthonous foci (p = 0.017), falciparum autochthonous cases (p = 0.038) and also falciparum autochthonous foci (p = 0.00).
Discussion
The current study was done in Sistan-Baluchestan as the largest province with the most malaria cases in Iran (Nejati et al. 2012b). The importance of the study on malaria in this area is clear, especially on probable factors which can affect its situation. Also, detailed studies related with various variables such as piped water, spraying coverage, number of malaria diagnoses centers and the malaria situation are limited in Asia and other parts of the world.
In our research, we have not found any significant correlation between the piped-water network and autochthonous malaria cases or with autochthonous foci. This result doesn’t seem reasonable because in the villages without a piped-water network, people stored their drinking water in ponds that were perfect breeding places for anopheles larvae (Fig. 2). These cement tanks needed a larval survey and Bacillus thuringiensis may be used by health workers for the anopheles larvae control, if required (Vatandoost and Hanafi-Bojd 2005). There is not much study for the investigation of this issue on the malaria situation, although it is clear that the removal of these water storage places can decrease the habitats of malaria vectors (Nath and Kumari 2006). The research which conducted in Uganda, has shown that malaria cases in villages with access to piped water are less than the villages using open springs (Hu 2016). Nevertheless, some researchers in India believe that piped-water supply can promote the spread of Anopheles stephensi in urban areas (Shanna 1998). It seems that although development of piped-water networks done within the 2006–2010 period is admirable, it was not enough for malaria reduction in this period. In addition, damage and leakage of piped-water networks can provide new breeding places for malaria vectors (Fig. 3).
Fig. 2.

The cement tanks (ponds) for using drinking and washing water before implementation of piped water network, southeastern Iran
Fig. 3.

Larval habitat due to damage and leakage of piped water network, southeastern Iran
Electricity is considered an effective factor in malaria reduction (Izadi 2016). Our results confirm this. Before access to electricity, people usually slept outdoors during the night in the villages. This behavior without using a bed net can increase exposure to the vectors’ bites (Hu 2016; Vatandoost and Hanafi-Bojd 2005). Nowadays, villagers prefer sleeping indoors where the presence of Anopheles and the chance of getting its bites are decreased.
Different factors such as temperature (Poudat et al. 2006), weather conditions (Ermert et al. 2012), humidity and high temperature (Zhang et al. 2012), sunshine and precipitation (Guo et al. 2015), have been evaluated in various studies as effective factors in the incidence of malaria. Usually, malaria increase is expected after precipitation. Precipitation can be considered an important climate variable in malaria early-warning systems for prediction of epidemics, especially in warm semi-arid and desert areas (Grover-Kopec et al. 2005; Thomson et al. 2005). But, our study does not show any significant correlation between rainfall and autochthonous malaria cases also with autochthonous foci. While we analyzed the correlation between the amount of annual rainfall and the malaria situation, it seems the number of rainy months is more important than that. Frequent rainfall can usually affect durability of breeding sites but heavy rainfall causes reduction of the mosquito population due to flooding and flushing out of breeding places (WHO 1982). In a study conducted in Uganda, a near correlation between monthly rainfall and malaria with a 2–3 month time interval between them was found. In this 3-year study, researchers reported the most precipitation in October–December and malaria increase in January of the next year (Kilian et al. 1999).
Distribution of free LLINs and also replacement of traditional and worn-out bed nets have been implemented during this study (Fig. 4).The current study showed significant correlation between distributed LLINs and malaria autochthonous foci. Nowadays, ITNs and LLINs are considered the most important interventions for prevention of malaria morbidity (Kabir et al. 2014). This led to 63 % of spending on total malaria control commodities (artemisinin-based combination therapy, ITNs, insecticides and spraying equipment for IRS, and rapid diagnostic tests) being allocated to ITNs by WHO in 2014. In that year, US$ 1.6 billion were spent on these commodities (WHO 2016). It seems that the population sleeping under ITN/LLINs is more effective in malaria prevention and reduction than only ITN/LLIN distribution. So, education of villagers in order to increase their knowledge, attitude and practise of bed net use is suggested.
Fig. 4.
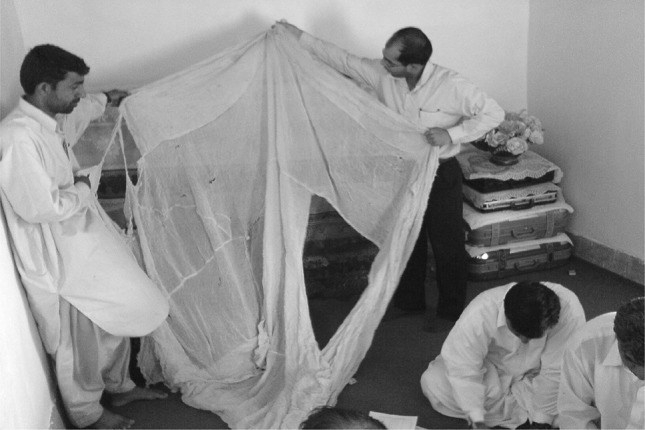
Replacement of worn-out bednets with free LLINs, Southeastern Iran
Although IRS has been applied as one of the effective interventions in malaria-control programs up to now in Iran (Nejati et al. 2012b) and in countries affected malaria (WHO 2016), we couldn’t see any correlation between IRS coverage and autochthonous cases including foci. This result can be controversial but this point maybe show that the targeted spraying is more important than it’s widely used for all of them in this area. In recent years, a guideline about the necessary criteria for selection of villages which need IRS that will help target spraying and cost saving, has been provided by the Iranian centre for Communicable Disease Control (CDC).
This study showed a significant correlation between the number of malaria diagnoses-treatment centers and malaria autochthonous cases and their foci. Free and early detection is the most important part of the elimination program in Iran (McKelvie et al. 2012). Thus, use of the rapid diagnostic test (RDT) has been expanded in various parts of the health system (Turki et al. 2015). On the other hand, the numbers of malaria diagnoses -treatment centers are markedly increased. Surely faster access to free diagnosis and treatment services is considered a critical point in the prevention of malaria epidemics (Ernst et al. 2006; Salehi et al. 2010), especially when immigrants from Iran’s eastern neighbours inhabit rural areas temporarily (Nejati et al. 2012a; Raiesi et al. 2012).
However, we emphasise that increased usage of bed nets, RDTs and early treatment in newly-opened medical centres had a commutative effect on total outcome of malaria.
With the beginning of the malaria elimination programme, many facilities and commodities such as thermal fogs, pumps, insecticides, cars, LLINs and RDTs were given to the provincial health centre. Although these commodities have been used previously, it seems their marked increase could play a major role in malaria reduction at the beginning of the malaria elimination programme. The assessment of these commodities and facilities and also the correlation between other probable factors on malaria reduction after the beginning of the malaria elimination programme (2009 up to now), are recommended. Surely this study and further studies can help the malaria managers and directors in more accurate allocation of financial resources.
Acknowledgments
Great acknowledgment goes to Mr. Abdolghafar Hasanzehi, Mr. Mohammad Sakeni and Mr. Naser Daneshmand Naruei from the Communicable Disease Control Department and also to Eng. Alireza Hoseini from the Environmental Health Department in the Province Health Centre, Zahedan University of Medical Sciences, for their kind cooperation in data collection.
Contributor Information
Jalil Nejati, Email: jalilnejati@yahoo.com.
Seyed Mehdi Tabatabaei, Email: dr_smt2001@yahoo.com.
Masoud Salehi, Email: shahestan@gmail.com.
Abedin Saghafipour, Email: jnejati@razi.tums.ac.ir.
Ehssan Mozafari, Email: ehssan.mozafari@gmail.com.
References
- Basseri H, Holakouie Naieni K, Raeisi A, Shahandeh K, Akbarzadeh K, Ranjbar M, Parvin A. Comparison of knowledge, attitude and practice (KAP) regarding malaria transmission and protection between afghan refugees and Iranian residents in Iranshahr, 2005–2006. Iran J Epidemiol. 2008;3(3):7–13. [Google Scholar]
- Basseri H, Raeisi A, Ranjbar Khakha M, Pakarai A, Abdolghafar H. Seasonal abundance and host-feeding patterns of anopheline vectors in malaria endemic area of Iran. J Parasitol Res. 2010;2010:8. doi: 10.1155/2010/671291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ermert V, Fink AH, Morse AP, Jones AE, Paeth H, Di Giuseppe F, Tompkins AM. Development of dynamical weather-disease models to project and forecast malaria in Africa. Malar J. 2012;11(Suppl 1):P133. doi: 10.1186/1475-2875-11-S1-P133. [DOI] [Google Scholar]
- Ernst KC, Adoka SO, Kowuor DO, Wilson ML, John CC. Malaria hotspot areas in a highland Kenya site are consistent in epidemic and non-epidemic years and are associated with ecological factors. Malar J. 2006;5(1):78. doi: 10.1186/1475-2875-5-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood BM. Control to elimination: implications for malaria research. Trends Parasitol. 2008;24(10):449–454. doi: 10.1016/j.pt.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Grover-Kopec E, Kawano M, Klaver RW, Blumenthal B, Ceccato P, Connor SJ. An online operational rainfall-monitoring resource for epidemic malaria early warning systems in Africa. Malar J. 2005;4(1):6. doi: 10.1186/1475-2875-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo C, Yang L, Ou C-Q, Li L, Zhuang Y, Yang J, Zhou Y-X, Qian J, Chen P-Y, Liu Q-Y. Malaria incidence from 2005–2013 and its associations with meteorological factors in Guangdong, China. Malar J. 2015;14(1):116. doi: 10.1186/s12936-015-0630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Oshaghi MA, Haghdoost AA, Shahi M, Sedaghat MM, Abedi F, Yeryan M, Pakari A. Entomological and epidemiological attributes for malaria transmission and implementation of vector control in southern Iran. Acta Trop. 2012;121(2):85–92. doi: 10.1016/j.actatropica.2011.04.017. [DOI] [PubMed] [Google Scholar]
- Hemami MR, Sari AA, Raisi A, Vatandoost H, Majdzadeh R. Malaria elimination in Iran, importance and challenges. Int J Prev Med. 2013;4(1):88–94. [PMC free article] [PubMed] [Google Scholar]
- Hu M (2016) Analyzing the connections among water access, sanitation, malaria and diarrhea outcomes in rural Central Uganda. Undergraduate Thesis in Global Health. Duke University Durham, North Carolina
- Izadi S. The effects of electricity network development besides routine malaria control measures in an underdeveloped region in the pre-elimination phase. Malar J. 2016;15(10):1. doi: 10.1186/s12936-016-1273-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabir MM, Naher S, Islam A, Karim A, Rasid M, Laskar SI. Vector control using LLIN/ITN: reduction of malaria morbidity in Bengladesh. Malar J. 2014;13:47. doi: 10.1186/1475-2875-13-S1-P47. [DOI] [Google Scholar]
- Keiser J, Utzinger J, De Castro MC, Smith TA, Tanner M, Singer BH. Urbanization in sub-saharan Africa and implication for malaria control. Am J Trop Med Hyg. 2004;71(2 suppl):118–127. [PubMed] [Google Scholar]
- Kilian A, Langi P, Talisuna A, Kabagambe G. Rainfall pattern. El Niño and malaria in Uganda. Trans R Soc Trop Med Hyg. 1999;93(1):22–23. doi: 10.1016/S0035-9203(99)90165-7. [DOI] [PubMed] [Google Scholar]
- Magalhães RJS, Langa A, Sousa-Figueiredo JC, Clements AC, Nery SV. Finding malaria hot-spots in northern Angola: the role of individual, household and environmental factors within a meso-endemic area. Malar J. 2012;11(1):1. doi: 10.1186/1475-2875-11-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKelvie WR, Haghdoost AA, Raeisi A. Defining and detecting malaria epidemics in south-east Iran. Malar J. 2012;11:81. doi: 10.1186/1475-2875-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nath B, Kumari R. Environmental management for malaria control. J Commun Dis. 2006;38(2):181–184. [PubMed] [Google Scholar]
- Nejati J, Ansari Moghadam S, Tabatabai A, Keyhani A. Effects of immigration on malaria incidence and its foci classification. Bimon J Hormozgan Univ Med Sci. 2012;16(4):283–291. [Google Scholar]
- Nejati J, Mahjoob M, Kiyani M, Keyhani A, Hasanzehi A. Status of indoor residual spraying by deltamethrin in malaria elimination program, Southeastern Iran. Iran J Toxicol. 2012;6(16):600–604. [Google Scholar]
- Nejati J, Vatandoost H, Oshghi MA, Salehi M, Mozafari E, Moosa-Kazemi SH. Some ecological attributes of malarial vector Anopheles superpictus Grassi in endemic foci in southeastern Iran. Asian Pac J Trop Biomed. 2013;3(12):1003–1008. doi: 10.1016/S2221-1691(13)60193-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips R. Current status of malaria and potential for control. Clin Microbiol Rev. 2001;14(1):208–226. doi: 10.1128/CMR.14.1.208-226.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poudat A, Ladoni H, Raissi A. Probable effective factors on malaria situation and morbidity in Bandar. Bimon J Hormozgan Univ Med Sci. 2006;10(2):101–110. [Google Scholar]
- Raiesi A, Nejati J, Ansari-moghaddam A, Sakeni M, Faraji L, Paktinat B, Nikpour F, Kamali F, Raiesi F. Effects of foreign immigrants on malaria situation in cleared up and potential foci in one of the highest malaria burden district of southern Iran. Malar J. 2012;11(Suppl 1):P81. doi: 10.1186/1475-2875-11-S1-P81. [DOI] [Google Scholar]
- Rehman AM, Mann AG, Schwabe C, Reddy MR, Roncon Gomes I, Slotman MA, Yellott L, Matias A, Caccone A, Nseng Nchama G. Five years of malaria control in the continental region, Equatorial Guinea. Malar J. 2013;12(1):154. doi: 10.1186/1475-2875-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehi M, Mashhadi E, Hakemi Y, Mirinezhad A. Analysis of malaria epidemic features in Sistan and Baluchistan province, southeast of Iran, 2005–2008. Iran Red Crescent Med J. 2010;3:247–253. [Google Scholar]
- Shanna V. Fighting malaria in India. Curr Sci. 1998;75(11):1127–1140. [Google Scholar]
- Tasnim (2015) Iran completes new power plant in Southeastern Province In. http://www.tasnimnews.com/en/news/2015/02/14/654588/iran-completes-new-power-plant-in-southeastern-province
- Thomson MC, Mason SJ, Phindela T, Connor SJ. Use of rainfall and sea surface temperature monitoring for malaria early warning in Botswana. Am J Trop Med Hyg. 2005;73(1):214–221. [PubMed] [Google Scholar]
- Turki H, Raeisi A, Malekzadeh K, Ghanbarnejad A, Zoghi S, Yeryan M, Nejad MA, Mohseni F, Shekari M. Efficiency of nested-PCR in detecting asymptomatic cases toward malaria elimination program in an endemic area of Iran. Iran J Parasitol. 2015;10(1):39. [PMC free article] [PubMed] [Google Scholar]
- Vatandoost H, Hanafi-Bojd A. Current resistant status of Anopheles stephensi liston to different larvicides in hormozgan province, southeastern Iran, 2004. Pak J Biol Sci. 2005;8:1568–1570. doi: 10.3923/pjbs.2005.1568.1570. [DOI] [Google Scholar]
- WHO . Manual on environmental management for mosquito control, with special emphasis on malaria control. Geneva: WHO; 1982. [PubMed] [Google Scholar]
- WHO (2016) World Malaria Report 2015. France
- Yeryan M, Basseri HR, Hanafi-Bojd AA, Raeisi A, Edalat H, Safari R. Bio-ecology of malaria vectors in an endemic area, Southeast of Iran. Asian Pac J Trop Med. 2016;9(1):32–38. doi: 10.1016/j.apjtm.2015.12.007. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Liu QY, Luan RS, Liu XB, Zhou GC, Jiang JY, Li HS, Li ZF. Spatial-temporal analysis of malaria and the effect of environmental factors on its incidence in Yongcheng, China, 2006–2010. BMC Pub Health. 2012;12(1):544. doi: 10.1186/1471-2458-12-544. [DOI] [PMC free article] [PubMed] [Google Scholar]



