Abstract
Objective
To study the predictive value of transluminal attenuation gradient (TAG) derived from diastolic phase of coronary computed tomography angiography (CCTA) for identifying systolic compression of myocardial bridge (MB).
Materials and Methods
Consecutive patients diagnosed with MB based on CCTA findings and without obstructive coronary artery disease were retrospectively enrolled. In total, 143 patients with 144 MBs were included in the study. Patients were classified into three groups: without systolic compression, with systolic compression < 50%, and with systolic compression ≥ 50%. TAG was defined as the linear regression coefficient between intraluminal attenuation in Hounsfield units (HU) and length from the vessel ostium. Other indices such as the length and depth of the MB were also recorded.
Results
TAG was the lowest in MB patients with systolic compression ≥ 50% (-19.9 ± 8.7 HU/10 mm). Receiver operating characteristic curve analysis was performed to determine the optimal cutoff values for identifying systolic compression ≥ 50%. The result indicated an optimal cutoff value of TAG as -18.8 HU/10 mm (area under curve = 0.778, p < 0.001), which yielded higher sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy (54.1, 80.5, 72.8, and 75.0%, respectively). In addition, the TAG of MB with diastolic compression was significantly lower than the TAG of MB without diastolic compression (-21.4 ± 4.8 HU/10 mm vs. -12.7 ± 8 HU/10 mm, p < 0.001).
Conclusion
TAG was a better predictor of MB with systolic compression ≥ 50%, compared to the length or depth of the MB. The TAG of MB with persistent diastolic compression was significantly lower than the TAG without diastolic compression.
Keywords: Coronary computed tomography angiography, Myocardial bridge, Systolic compression, Transluminal attenuation gradient, TAG, Ischemic heart disease, Coronary artery disease
INTRODUCTION
Myocardial bridging (MB) is a congenital anomaly in which a bridge of the myocardium covers a segment of the coronary artery. It occurs mostly in the mid-portion of the left anterior descending (LAD) coronary artery (1). It has been widely accepted that functional MB linked to dynamic compression is associated with ischemic heart disease, arrhythmia, and sudden cardiac death, which suggests the clinical diagnostic importance of this anomaly (2,3,4,5).
On invasive coronary angiography (ICA), investigators observed that the extent of systolic narrowing of mural coronary artery was associated with potentially inducible myocardial ischemia (1). Gawor et al. (6) reported a significant correlation between summed stress score of nuclear myocardial perfusion imaging and a degree of systolic narrowing of MB. All perfusion abnormalities (12 of 42 patients) were found in the segments with > 50% systolic compression. Lee et al. (7) showed a higher incidence of perfusion defect (10 of 14 patients) induced by significant systolic compression of MB in Thallium-201 single photon emission computed tomography with dipyridamole stress. Defects were seen in patients with > 75% systolic narrowing. Coronary computed tomography angiography (CCTA) has been introduced as a useful imaging modality for patients with MB (8). However, direct detection of systolic stenosis by CCTA is difficult, due to a limited cardiac phase from the prospective electrocardiography (ECG)-gated acquisition (9). Even with a retrospective scan protocol, dose modulation leads to impaired image quality in the systolic phase (10,11). Recently, it has been recognized that dynamic compression is not only related to systolic phase, but also persists into mid-to-late diastole (12). The attenuation gradient in normal coronary arteries was initially known as contrast opacification gradients before the more generally accepted term–‘transluminal attenuation gradient (TAG)’ (13). Based on previous findings, TAG is defined as the transluminal opacification gradient of proximal to distal vessels in computed tomography. It exhibits linear correlation with the extent of intracoronary transluminal stenosis (14).
In this study, we hypothesize that TAG changes within the tunneled artery in diastole may indirectly predict systolic compression and help to differentiate MBs inducing myocardial ischemia in the systolic phase. Accordingly, the purpose of this study was to assess the clinical importance of the TAG sign in patients diagnosed with MB based on CCTA findings.
MATERIALS AND METHODS
Patient Population
Institutional Review Board approval was obtained for this retrospective study, and informed consent was waived. Between September 2014 and March 2015, consecutive patients with chest discomfort and suspected for coronary artery disease were referred for CCTA and retrospectively reviewed. All patients without obstructive coronary artery disease but with CCTA-confirmed MBs were included in the study. All included patients underwent retrospective ECG-gated CTA. The exclusion criteria were as follows: 1) patients whose CCTA images showed impaired quality either in the diastolic or systolic phase; 2) those with prospective ECG-triggered CTA; 3) those with a previous history of attempted coronary revascularization of target lesions (percutaneous coronary intervention or bypass surgery); 4) those with severely calcified target lesions (cross-sectional arc calcium, > 180°), in whom such lesions cannot be accurately evaluated; and 5) concomitant obstructive coronary artery disease (defined as diameter stenosis ≥ 50% diagnosed by CTA which might also cause the alteration of lumen attenuation) of the target vessel (MB vessel).
Imaging Protocol of CCTA
A 128-slice single source multidetector CT (Definition AS, Siemens Medical Solutions, Forchheim, Germany) was used for scanning. Patients with a pre-scan heart rate > 65 bpm were orally administered 25–75 mg of a β-blocker (Betaloc ZOK, AstraZeneca, Shanghai, China) 1 hour prior to the scan. Sublingual nitroglycerin was given to all patients. A bolus of contrast media such as iopamidol 370 mg iodine/mL (Isovist; Bayer Healthcare, Berlin, Germany) was injected into the antecubital vein at the rate of 4.5–5.0 mL/s, followed by injection of a 20–40 mL saline flush, using a dual-barrel power injector (Tyco-Mallinckrodt, Cincinnati, OH, USA). The amount of contrast media was determined based on the patient's body weight and the scanning time. A test bolus was first injected, and the region of interest was placed within the ascending aorta to determine the accurate delay time, which was defined as 4 seconds plus the peak time of ascending aorta. Retrospective ECG-gated CTA was performed from cranially to caudally with 128 sections, with a section thickness of 0.6 mm and a rotation time of 300 ms. The pitch varied between 0.2 and 0.5 depending on the heart rate and patient size. The tube current was automatically adjusted in each patient based on body habitus by an automatic exposure control system (CareDose 4D, Siemens Medical Solutions) and electrocardiographically modified (an electrocardiographically-dependent dose modulation technique was applied with a full dose during the R-R interval of 40–70%). The tube voltage was also automatically determined from 80 kVp to 120 kVp based on body habitus by an automatic exposure control system. The images were reconstructed with a slice thickness of 0.6 mm, a reconstruction increment of 0.5 mm using a medium soft-tissue convolution kernel (B26F), and reconstructed matrix size of 512 × 512.
Imaging Reconstruction and Analysis
Data were transferred to an offline workstation (Syngo. via, Siemens Medical Solutions) for further analysis. Axial, cross-sectional, curved planar reformation (CPR), multiplanar reformation, and three-dimensional maximum intensity projection images were generated.
Myocardial bridging was diagnosed when part of a coronary artery was completely surrounded by the myocardium without the intervening fat (15). All parameters were measured during the diastolic phase with best image quality and least artifact as follows.
Intracoronary Transluminal Attenuation Gradient
Cross-sectional images perpendicular to the centerline were reconstructed for each target vessel. The TAG in Hounsfield units (HU) was measured manually at 5-mm intervals on CPR images, from the ostium to the distal level where the lumen area was < 2 mm2. The attenuation gradient was determined by the change in HU per 10-mm length of the coronary artery, and defined as the linear regression coefficient between intraluminal attenuation in HU and length from the vessel ostium in mm, as previously introduced by Choi et al. (14).
MB Length
The length of the MB was defined as the distance of the tunneled artery from the entrance to the exit beneath the bridging on the CPR images.
MB Depth
The thickness of the MB was defined as the thickness of the deepest part from the surface of the covering myocardial tissue to the tunneled segment, on the cross-sectional images.
The image quality was assessed by using a 3-point semi-quantitative scale: 3 = excellent (absence of artifact), 2 = acceptable (presence of mild artifact, but still diagnostic), 1 = poor (presence of severe artifact, non-diagnostic). Only patients with image quality of grade 3 were included for further analysis. The extent of systolic compression was defined as the percentage of diameter loss at the end-systolic phase compared to the end-diastolic phase on cross-sectional images. Based on the extent of lumen narrowing at the systolic phase on CCTA, MB patients were classified into three types: without systolic compression and no luminal stenosis, with < 50% systolic compression, and with systolic compression and thus, ≥ 50% luminal stenosis. The mean cardiac phase for measurement of TAG was 71.4 ± 2.3% of R-R interval (median 70% of R-R interval, 25–75% percentile: 70–75% of R-R interval); whereas, the mean end-systolic and end-diastolic phase used for determining the extent of systolic compression were 31.7 ± 3.8% of R-R interval and 2.9 ± 4.5% of R-R interval, respectively. Two experienced radiologists independently analyzed the lesions; and any disagreement was resolved by consensus.
Statistical Analysis
Statistical analysis was performed using the commercially available statistical software (SPSS, version 13.0, SPSS Inc., Chicago, IL, USA; MedCalc Statistical Software version 15.2.2, MedCalc Software bvba, Ostend, Belgium). Quantitative variables were expressed as mean ± standard deviation. One-way analysis of variance was used for normally distributed data; whereas, Mann-Whitney U test was used for data that were not normally distributed. TAG was determined as a linear regression coefficient from the coronary ostium to the most distally measured value per 10-mm. Receiver operating characteristic (ROC) curve analysis was used to determine the optimal cutoffs for continuous variables. Bland-Altman analysis as well as Cohen's kappa analysis was performed in 40 randomly selected lesions to determine the inter-rater agreement. A p value < 0.05 was considered statistically significant.
RESULTS
Clinical Characteristics
Four hundred and seventy-three patients with retrospective ECG-gated CTA and at least one MB were initially eligible for inclusion. Two hundred and sixteen patients whose CCTA images showed impaired quality either in the diastolic or systolic phase were excluded; whereas, 77 patients with a previous history of attempted coronary revascularization of target were also excluded. Sixty-three patients with severely calcified target lesions (cross-sectional arc calcium, > 180°) and 117 patients with concomitant obstructive coronary artery disease on the target MB vessel were further excluded. In total, 143 patients {67 male patients (mean age 57.4 ± 14.6 [range, 22–91] years), 76 female patients (mean age 62.9 ± 9.1 [range, 37–85] years)} with a mean age of 60.1 ± 12.3 (range, 22–91) years, with 144 MBs, were included in the study. The dose-length product of CCTA was 562.3 ± 95.4 mGy*cm, and the mean effective dose was 7.87 ± 1.34 (range, 5.2–10.6) mSv. The mean heart rate during CT acquisition was 66.3 ± 3.8 (range, 51–82) bpm. Detailed demographic data are shown in Table 1.
Table 1. Clinical Characteristics.
| Characteristic | |
|---|---|
| Number of patients | 143 |
| Number of lesions | 144 |
| Age (years) | 60.1 ± 12.3 (22–91) |
| Male (%) | 67 (46.9) |
| Lesion location (%) | |
| Left anterior descending branch | 139 (96.5) |
| Right coronary artery | 3 (2.1) |
| Ramus intermedius | 2 (1.4) |
Characteristics of CCTA Findings
A total of 144 MBs were detected on CCTA in 143 patients, which occurred almost exclusively in the LAD artery, followed by the right coronary artery, and the ramus intermedius (Table 1). Among these, CCTA revealed 42 lesions without systolic compression, 41 with systolic compression < 50%, and 61 with systolic compression ≥ 50% (Table 2). The Bland-Altman analysis showed a mean difference of TAG measured by two raters of -5.4 HU/10 mm (Fig. 1). The correlation coefficient for the measurement of TAG between the two raters was 0.718 (p < 0.001).
Table 2. Lesion Characteristics of CCTA Parameters between Three Groups.
| All Lesions (n = 144) | Compression Absent (n = 42) | Compression < 50% (n = 41) | Compression ≥ 50% (n = 61) | |
|---|---|---|---|---|
| TAG (HU/10 mm) | -15.2 ± 8.2 | -9.6 ± 6.2 p < 0.001* |
-14.0 ± 4.8 p < 0.001† |
-19.9 ± 8.7 p < 0.001‡ |
| MB length (mm) | 21.9 ± 10.6 | 17.6 ± 6.2 p = 0.049* |
21.4 ± 10.8 p = 0.089* |
25.3 ± 11.7 p < 0.001* |
| MB depth (mm) | 1.57 ± 1.1 | 1.32 ± 1.07 p = 0.521* |
1.46 ± 0.90 p = 0.102* |
1.81 ± 1.12 p = 0.028* |
*Comparison between compression-absent group and compression < 50% group, †Comparison between compression < 50% group and compression ≥ 50% group, ‡Comparison between compression-absent group and compression ≥ 50% group. CCTA = coronary computed tomography angiography, HU = Hounsfield units, MB = myocardial bridge, TAG = transluminal attenuation gradient
Fig. 1. Bland-Altman analysis plot comparing observer 1 and observer 2 for measurement of TAG in 40 randomly selected cases.
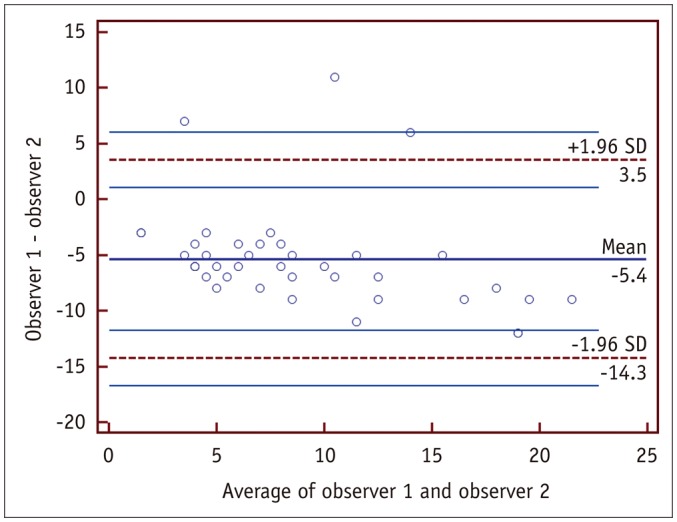
Mean difference of TAG measured by two raters was -5.4 HU/10 mm. HU = Hounsfield units, SD = standard deviation, TAG = transluminal attenuation gradient
Comparison of Parameters in All Groups
The comparison of TAG, and length and depth of MB among the three groups (MB without dynamic compression, MB with systolic compression < 50%, and MB with systolic compression ≥ 50%) is shown in Table 2. The mean TAG value was the lowest in patients with MB with systolic compression ≥ 50% (-19.9 ± 8.7 HU/10 mm) (Fig. 2), slightly higher in patients with MB with systolic compression < 50% (-14.0 ± 4.8 HU/10 mm), and the highest in patients with MB without systolic compression (-9.6 ± 6.2 HU/10 mm) (Fig. 3). Conversely, patients with MB with systolic compression ≥ 50% showed greater lesion-length than the patients in the other two groups; and the lesion-length was the shortest in patients with MB without systolic compression. Similarly, bridge thickness was the greatest in patients with MB with systolic compression ≥ 50%; whereas, it was the lowest in patients with MB without systolic compression. The three indices showed significant differences between the groups. In addition, persistent diastolic compression (compression extent was < 50% in all cases) was also noted in 42 (29.2%, 42/144) MB cases. The TAG of MB with diastolic compression was significantly lower than the TAG of MB without diastolic compression (-21.4 ± 4.8 HU/10 mm vs. -12.7 ± 8 HU/10 mm, p < 0.001). In all lesions with persistent diastolic compression, 38.1% (16/42) were associated with systolic compression < 50%; whereas, 61.9% (26/42) were associated with systolic compression ≥ 50%.
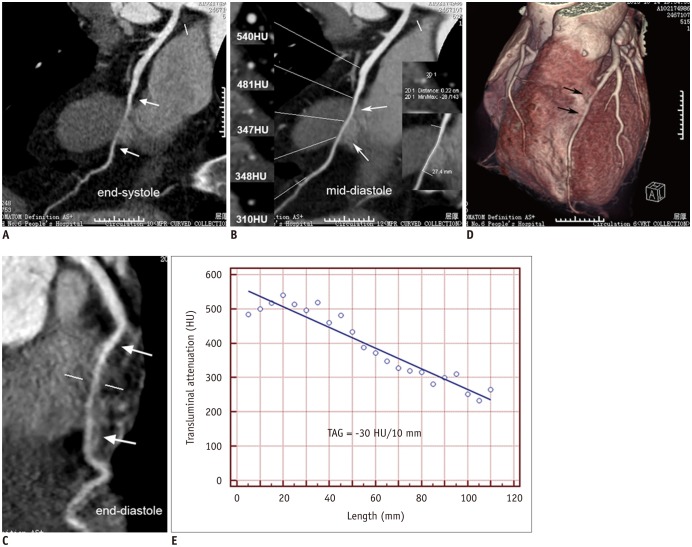
Fig. 2. Representative case of MB with dynamic compression.
A. CPR image of end-systolic phase (35% of R-R interval) showed presence of MB at middle LAD with significant compression (white arrows). B. CPR image of mid-diastolic phase (70% of R-R interval) showed presence of MB at middle LAD (white arrows). MB depth and length were 2.2 and 27.4 mm, respectively. C. CPR image of end-diastolic phase (5% of R-R interval) showed presence of MB at middle LAD (white arrows) with persistent compression. D. VR image confirmed overlay of myocardium at middle LAD (black arrows). E. TAG of MB vessel was -30 HU/10 mm. CPR = curved planar reformation, HU = Hounsfield units, LAD = left anterior descending, MB = myocardial bridge, TAG = transluminal attenuation gradient, VR = volume rendering
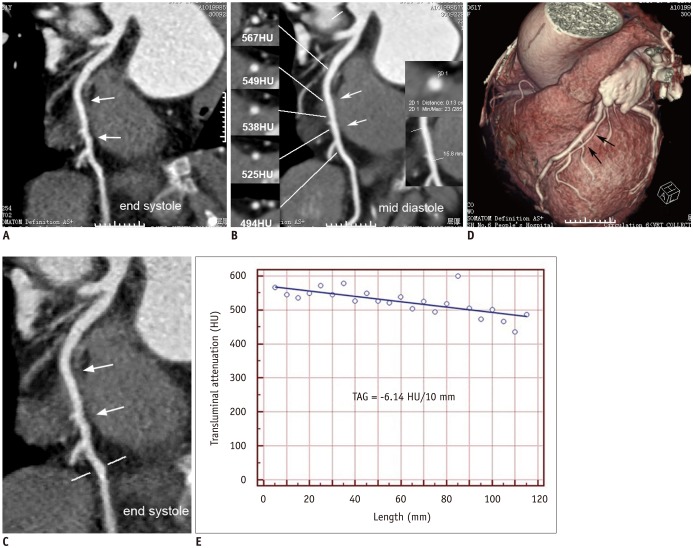
Fig. 3. Representative case of MB with dynamic compression.
A. CPR image of end-systolic phase (35% of R-R interval) showed presence of MB at middle LAD without compression (white arrows). B. CPR image of mid-diastolic phase (70% of R-R interval) showed presence of MB at middle LAD (white arrows). MB depth and length were measured as 1.3 and 15.8 mm, respectively. C. CPR image of end-diastolic phase (5% of R-R interval) showed presence of MB at middle LAD (white arrows). D. VR image confirmed overlay of myocardium at middle LAD (black arrows). D. TAG of MB vessel was -6.14 HU/10 mm. CPR = curved planar reformation, HU = Hounsfield units, LAD = left anterior descending, MB = myocardial bridge, TAG = transluminal attenuation gradient, VR = volume rendering
Diagnostic Performance of CCTA
Receiver operating characteristic curve analysis was performed to determine the optimal cutoff values for identifying systolic compression ≥ 50%. As summarized in Table 3, TAG showed the largest area under the curve, followed by the length and depth of MB (Fig. 4). The best cutoff values were estimated as -18.8 HU/10 mm, 24.6 mm, and 1.5 mm, respectively. At a cutoff value of ≤ 18.8 HU/10 mm as the criterion, TAG yielded higher sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy than the other two parameters (Table 4).
Table 3. ROC Curve Analysis of Variables that were Significant at Univariate Analysis.
| AUC | 95% Confidence Interval | Best Cutoff | P | |
|---|---|---|---|---|
| TAG | 0.778 | 0.702–0.843 | -18.8 HU/10 mm | < 0.001 |
| MB length | 0.663 | 0.579–0.739 | 24.6 mm | < 0.001 |
| MB depth | 0.620 | 0.535–0.699 | 1.5 mm | 0.012 |
AUC = area under curve, HU = Hounsfield units, MB = myocardial bridge, ROC = receiver operating characteristic, TAG = transluminal attenuation gradient
Fig. 4. ROC curve analysis of CCTA-derived parameters for identifying MB with systolic compression ≥ 50%.
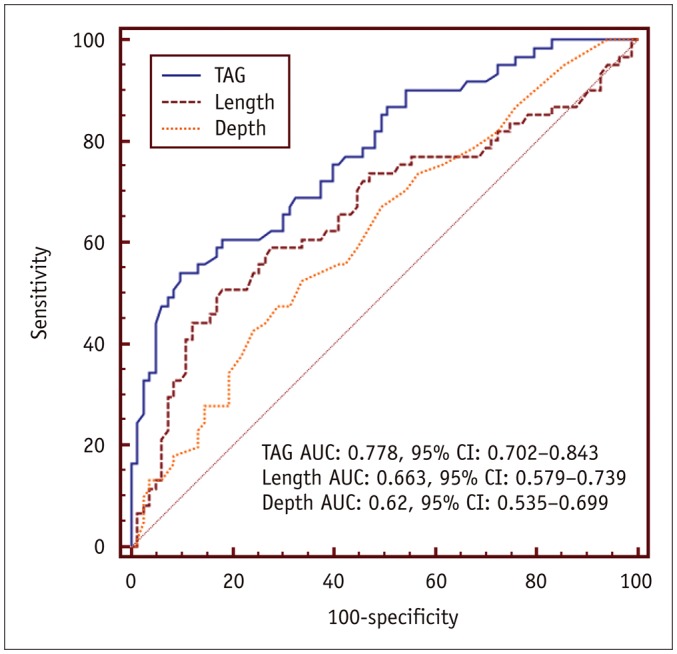
TAG showed largest AUC and best diagnostic performance compared with MB depth and MB length (TAG vs. depth, p = 0.01; TAG vs. length, p = 0.057; length vs. depth, p = 0.475). AUC = area under curve, CCTA = coronary computed tomography angiography, CI = confidence interval, MB = myocardial bridge, ROC = receiver operating characteristic, TAG = transluminal attenuation gradient
Table 4. Diagnostic Performance of CCTA for Indicating Significant Systolic Compression.
| Sensitivity, % (95% CI) | Specificity, % (95% CI) | Positive Predictive Value, % (95% CI) | Negative Predictive Value, % (95% CI) | Diagnostic Accuracy, % (95% CI) | |
|---|---|---|---|---|---|
| TAG of MB ≤ -18.8 HU/10 mm | 54.1 (40.9–66.9) | 90.4 (81.9–95.8) | 80.5 (65.1–91.2) | 72.8 (63.1–81.1) | 75.0 (67.9–82.1) |
| MB length > 24.6 mm | 50.8 (37.7–63.9) | 81.9 (72.0–89.5) | 67.4 (52.0–80.5) | 69.4 (59.3–78.3) | 68.8 (61.2–76.4) |
| MB depth > 1.5 mm | 52.5 (39.3–65.4) | 66.3 (55.1–75.3) | 53.3 (40.0–66.3) | 65.5 (54.3–75.5) | 60.4 (52.4–68.4) |
CCTA = coronary computed tomography angiography, CI = confidence interval, HU = Hounsfield units, MB = myocardial bridge, TAG = transluminal attenuation gradient
DISCUSSION
The main finding of our study was that systolic compression could be ruled out based on the intracoronary TAG derived from the diastolic phase. In addition, with the optimal cutoff value (≤ -18.8 HU/10 mm) as a criterion, the MB with systolic compression ≥ 50% could be differentiated from those with mild systolic compressions.
Myocardial bridging is an incidental finding associated with an excellent five-year survival rate of 97% (16); however, emerging evidence suggests that MBs are associated with myocardial ischemia and infarction, which are related with direct compression, especially at the systolic phase (2,3,4,5). The degree of systolic compression may substantially affect further therapeutic strategy and outcome (17). Therefore, the diagnosis of dynamic compression is of clinical importance.
Previously reported findings on the morphological features that predict dynamic compression are controversial, due to variations in the anatomical properties such as the length and thickness of MB among the studies (10,15,18).
Although CCTA is well recognized as a useful imaging modality in the diagnosis of various cardiac diseases (19), the functional evaluation by CT mainly focuses on the hemodynamic assessment of atherosclerotic coronary diseases (20). In this study, we examined TAG non-invasively derived from CCTA as an additional parameter that may help to determine the systolic compression measured during the diastolic phase. The result indicated that TAG showed the highest specificity, positive predictive value, negative predictive value, and diagnostic accuracy. There are two underlying mechanisms that might contribute to our findings. The first is diastolic filling dysfunction. Previous studies revealed that systolic vessel compression by MB sustains until mid-to-late diastole, which induces hemodynamic disturbance and filling dysfunction in both, the systolic and diastolic phases (12,21). The second mechanism is downstream-flow limitation resulting from the constriction of the proximal vessel and blood-flow filling dysfunction by the myocardial compression (22). Thus, TAG may gradually decrease from the proximal to the distal length of the coronary artery.
Transluminal attenuation gradient showed high specificity (90.4%) for identifying significant dynamic compression with a cutoff value of -18.8 HU/10 mm, however, the sensitivity (54.1%) was low. In addition, the negative predictive value (72.8%) was lower than the positive predictive value (80.5%). Thus, this phenomenon could be attributed to the diastolic blood-flow filling. For this small subgroup of patients, diastolic blood-flow filling dysfunction induced by systolic constriction was not obvious. Therefore, MB with moderate or severe compression could show a higher TAG value than expected. In addition, TAG is a parameter with functional significance; whereas, dynamic compression is an anatomic feature. Previous studies have indicated that the extent of MB compression does not necessarily correlate with inducible myocardial ischemia (23), which could partly explain the lower sensitivity value compared to specificity. Furthermore, the potential clinical value of TAG for the assessment of MB lies in the exclusion of significant compression with high specificity, since myocardial perfusion defect was not noted in MB with systolic compression < 50% (24).
Additionally, the clinical value of TAG derived from diastolic phase can be translated into the further application of this novel parameter in patients scanned in the prospective acquisition mode. Traditionally, assessment of the extent of compression by CCTA requires high-spatial resolution images in both systolic and diastolic phases (10), which are available only in retrospective ECG-gated acquisition with increased radiation dose (9,11,25). Based on our current findings, prospective acquisition with single cardiac phase and low radiation dose is a potential method for non-invasive prediction of significant compression of MB with TAG alteration.
The major limitation of our study was that the functional tests such as myocardial perfusion imaging or fractional flow reserve (FFR) (26) were not applied as a routine investigation for evaluation of MBs. Therefore, we were unable to validate the TAG value for identifying the hemodynamic significance of MB. It is commonly accepted that the stenotic extent sometimes mismatches the findings from myocardial perfusion imaging or FFR (26). The 50% systolic compression does not necessarily lead to myocardial ischemia and is responsible for the chest discomfort. Thus, the clinical relevance of TAG should be carefully interpreted before confirmation by other functional tests. Second, the use of 128-detector CT TAG depends on the time-density curve of the transluminal contrast agent and scanning time. A wider detector row scanner or dual-source CT system enables single-beat imaging of the entire coronary artery. Thus, further large-sample studies employing CCTA and ICA are needed to confirm the diagnostic accuracy of our findings. Third, the compression extent was determined at the end-systolic and end-diastolic phases, in which the image quality was compromised due to the application of dose modulation technique (full dose during 40–70% of R-R interval). Therefore, accurate assessment of the exact compression extent was not feasible on CCTA. In addition, the tube voltage and current varied between the patients due to body habitus. Thus, heterogeneous tube settings might also affect the measurement results of TAG. Finally, a recent study revealed that the intraluminal attenuation of coronary vessels gradually decreased along with a decrease in diameter (27). Therefore, further studies are required to test the value of TAG for prediction of systolic compression of MB based on vessel caliber.
In conclusion, TAG derived from the diastolic phase could exclude systolic compression of MB. In addition, with the cutoff value of -18.8 HU/10 mm, TAG was a superior predictor of MB with systolic compression ≥ 50%, as compared with the length and depth of MB. The TAG of MB with persistent diastolic compression was significantly lower than the TAG without diastolic compression.
References
- 1.Möhlenkamp S, Hort W, Ge J, Erbel R. Update on myocardial bridging. Circulation. 2002;106:2616–2622. doi: 10.1161/01.cir.0000038420.14867.7a. [DOI] [PubMed] [Google Scholar]
- 2.Akdemir R, Gunduz H, Emiroglu Y, Uyan C. Myocardial bridging as a cause of acute myocardial infarction: a case report. BMC Cardiovasc Disord. 2002;2:15. doi: 10.1186/1471-2261-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SS, Jeong MH, Kim HK, Kim MC, Cho KH, Lee MG, et al. Long-term clinical course of patients with isolated myocardial bridge. Circ J. 2010;74:538–543. doi: 10.1253/circj.cj-09-0648. [DOI] [PubMed] [Google Scholar]
- 4.Gowda RM, Khan IA, Ansari AW, Cohen RA. Acute ST segment elevation myocardial infarction from myocardial bridging of left anterior descending coronary artery. Int J Cardiol. 2003;90:117–118. doi: 10.1016/s0167-5273(02)00518-1. [DOI] [PubMed] [Google Scholar]
- 5.Nakanishi R, Rajani R, Ishikawa Y, Ishii T, Berman DS. Myocardial bridging on coronary CTA: an innocent bystander or a culprit in myocardial infarction? J Cardiovasc Comput Tomogr. 2012;6:3–13. doi: 10.1016/j.jcct.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Gawor R, Kuśmierek J, Płachcińska A, Bieńkiewicz M, Drożdż J, Piotrowski G, et al. Myocardial perfusion GSPECT imaging in patients with myocardial bridging. J Nucl Cardiol. 2011;18:1059–1065. doi: 10.1007/s12350-011-9406-8. [DOI] [PubMed] [Google Scholar]
- 7.Lee YS, Moon DH, Shin JW, Park SW, Park SJ, Lee HK. Dipyridamole TI-201 SPECT imaging in patients with myocardial bridging. Clin Nucl Med. 1999;24:759–764. doi: 10.1097/00003072-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Hwang JH, Ko SM, Roh HG, Song MG, Shin JK, Chee HK, et al. Myocardial bridging of the left anterior descending coronary artery: depiction rate and morphologic features by dual-source CT coronary angiography. Korean J Radiol. 2010;11:514–521. doi: 10.3348/kjr.2010.11.5.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirai N, Horiguchi J, Fujioka C, Kiguchi M, Yamamoto H, Matsuura N, et al. Prospective versus retrospective ECG-gated 64-detector coronary CT angiography: assessment of image quality, stenosis, and radiation dose. Radiology. 2008;248:424–430. doi: 10.1148/radiol.2482071804. [DOI] [PubMed] [Google Scholar]
- 10.Leschka S, Koepfli P, Husmann L, Plass A, Vachenauer R, Gaemperli O, et al. Myocardial bridging: depiction rate and morphology at CT coronary angiography--comparison with conventional coronary angiography. Radiology. 2008;246:754–762. doi: 10.1148/radiol.2463062071. [DOI] [PubMed] [Google Scholar]
- 11.Machida H, Tanaka I, Fukui R, Shen Y, Ishikawa T, Tate E, et al. Current and novel imaging techniques in coronary CT. Radiographics. 2015;35:991–1010. doi: 10.1148/rg.2015140181. [DOI] [PubMed] [Google Scholar]
- 12.Bourassa MG, Butnaru A, Lespérance J, Tardif JC. Symptomatic myocardial bridges: overview of ischemic mechanisms and current diagnostic and treatment strategies. J Am Coll Cardiol. 2003;41:351–359. doi: 10.1016/s0735-1097(02)02768-7. [DOI] [PubMed] [Google Scholar]
- 13.Steigner ML, Mitsouras D, Whitmore AG, Otero HJ, Wang C, Buckley O, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010;3:179–186. doi: 10.1161/CIRCIMAGING.109.854307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi JH, Min JK, Labounty TM, Lin FY, Mendoza DD, Shin DH, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging. 2011;4:1149–1157. doi: 10.1016/j.jcmg.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Kim PJ, Hur G, Kim SY, Namgung J, Hong SW, Kim YH, et al. Frequency of myocardial bridges and dynamic compression of epicardial coronary arteries: a comparison between computed tomography and invasive coronary angiography. Circulation. 2009;119:1408–1416. doi: 10.1161/CIRCULATIONAHA.108.788901. [DOI] [PubMed] [Google Scholar]
- 16.Kramer JR, Kitazume H, Proudfit WL, Sones FM., Jr Clinical significance of isolated coronary bridges: benign and frequent condition involving the left anterior descending artery. Am Heart J. 1982;103:283–288. doi: 10.1016/0002-8703(82)90500-2. [DOI] [PubMed] [Google Scholar]
- 17.Schwarz ER, Gupta R, Haager PK, vom Dahl J, Klues HG, Minartz J, et al. Myocardial bridging in absence of coronary artery disease: proposal of a new classification based on clinical-angiographic data and long-term follow-up. Cardiology. 2009;112:13–21. doi: 10.1159/000137693. [DOI] [PubMed] [Google Scholar]
- 18.Ishikawa Y, Akasaka Y, Suzuki K, Fujiwara M, Ogawa T, Yamazaki K, et al. Anatomic properties of myocardial bridge predisposing to myocardial infarction. Circulation. 2009;120:376–383. doi: 10.1161/CIRCULATIONAHA.108.820720. [DOI] [PubMed] [Google Scholar]
- 19.Kim YJ, Yong HS, Kim SM, Kim JA, Yang DH, Hong YJ, et al. Korean guidelines for the appropriate use of cardiac CT. Korean J Radiol. 2015;16:251–285. doi: 10.3348/kjr.2015.16.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang D, Lee JM, Koo BK. Physiologic assessment of coronary artery disease: focus on fractional flow reserve. Korean J Radiol. 2016;17:307–320. doi: 10.3348/kjr.2016.17.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corban MT, Hung OY, Eshtehardi P, Rasoul-Arzrumly E, McDaniel M, Mekonnen G, et al. Myocardial bridging: contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. J Am Coll Cardiol. 2014;63:2346–2355. doi: 10.1016/j.jacc.2014.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herrmann J, Higano ST, Lenon RJ, Rihal CS, Lerman A. Myocardial bridging is associated with alteration in coronary vasoreactivity. Eur Heart J. 2004;25:2134–2142. doi: 10.1016/j.ehj.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Soran O, Pamir G, Erol C, Kocakavak C, Sabah I. The incidence and significance of myocardial bridge in a prospectively defined population of patients undergoing coronary angiography for chest pain. Tokai J Exp Clin Med. 2000;25:57–60. [PubMed] [Google Scholar]
- 24.Uusitalo V, Saraste A, Pietilä M, Kajander S, Bax JJ, Knuuti J. The functional effects of intramural course of coronary arteries and its relation to coronary atherosclerosis. JACC Cardiovasc Imaging. 2015;8:697–704. doi: 10.1016/j.jcmg.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Sun Z, Ng KH. Prospective versus retrospective ECG-gated multislice CT coronary angiography: a systematic review of radiation dose and diagnostic accuracy. Eur J Radiol. 2012;81:e94–e100. doi: 10.1016/j.ejrad.2011.01.070. [DOI] [PubMed] [Google Scholar]
- 26.Ko BS, Cameron JD, Leung M, Meredith IT, Leong DP, Antonis PR, et al. Combined CT coronary angiography and stress myocardial perfusion imaging for hemodynamically significant stenoses in patients with suspected coronary artery disease: a comparison with fractional flow reserve. JACC Cardiovasc Imaging. 2012;5:1097–1111. doi: 10.1016/j.jcmg.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Park EA, Lee W, Park SJ, Kim YK, Hwang HY. Influence of coronary artery diameter on intracoronary transluminal attenuation gradient during CT angiography. JACC Cardiovasc Imaging. 2016;9:1074–1083. doi: 10.1016/j.jcmg.2015.10.028. [DOI] [PubMed] [Google Scholar]