Abstract
Background:
In response to growing concerns regarding the overuse of coronary computed tomography angiography (CCTA) in the clinical setting, multiple societies, including the American College of Cardiology Foundation, have jointly published revised criteria regarding the appropriate use of this imaging modality. However, previous research indicates significant discrepancies in the rate of adherence to these guidelines.
Aim:
To assess the appropriateness of CCTA referrals in a tertiary cardiac center in Bahrain.
Methods:
This retrospective clinical audit examined the records of patients referred to CCTA between the April 1, 2015 and December 31, 2015 in Mohammed bin Khalifa Cardiac Center. Using information from medical records, each case was meticulously audited against guidelines to categorize it as appropriate, inappropriate, or uncertain.
Results:
Of the 234 records examined, 176 (75.2%) were appropriate, 47 (20.1%) were uncertain, and 11 (4.7%) were inappropriate. About 74.4% of all referrals were to investigate coronary artery disease (CAD). The most common indication that was deemed appropriate was the detection of CAD in the setting of suspected ischemic equivalent in patients with an intermediate pretest probability of CAD (65.9%). Most referrals deemed inappropriate were requested to detect CAD in asymptomatic patients at low or intermediate risk of CAD (63.6%).
Conclusion:
This audit demonstrates a relatively low rate of inappropriate CCTA referrals, indicating the appropriate and efficient use of this resource in the Mohammed bin Khalifa Cardiac Center. Agreement on and reclassification of “uncertain” cases by guideline authorities would facilitate a deeper understanding of referral appropriateness.
Key words: Cardiac imaging, coronary computed tomography, coronary computed tomography angiography, coronary computed tomography angiography appropriateness, coronary computed tomography angiography referrals, coronary imaging
INTRODUCTION
Over the past two decades, computed tomography has undergone an accelerated improvement in capabilities relative to other imaging modalities,[1] with various improvements witnessed in terms of scan duration and temporal and spatial resolution. These advances enabled the imaging of small and fast moving structures, essentially overcoming the challenge of imaging the coronary arteries in a beating heart. The ability of coronary computed tomography angiography (CCTA) to noninvasively assess coronary arteries has generated widespread enthusiasm, as reflected by its rapid growth and dissemination.[2]
However, despite the proven value of CCTA in evaluating numerous medical conditions,[2,3,4] there have been growing concerns regarding its overuse in the clinical setting, which is not only associated with a significant financial strain on health services, but also the potential to expose patients to unnecessary radiation. The typical radiation dose for a CCTA study varies widely – from < 1 mSv in a FLASH mode CCTA,[5] through 2–3 mSv for “Step-and-Shoot” protocol[6] to a median dose of 12 mSv for a helical CCTA.[7]
Consequently, effort has been made to maximize the rational utilization of this growing imaging modality by The American College of Cardiology Foundation in coordination with multiple specialty and sub-specialty societies, which have jointly published revised CCTA appropriate use criteria (AUC) in 2010.[3]
Nevertheless, evidence still exists of suboptimal use of this modality in various institutions, with previous data suggesting that the rate of inappropriate use varies between 5% and 25%.[8]
The present study sought to audit the appropriateness of CCTA scans conducted at a tertiary cardiac center in the Kingdom of Bahrain.
METHODS
This study was designed as a retrospective audit of medical records of patients referred for CCTA in the Mohammed bin Khalifa Cardiac Center.
Study population
This study planned to examine all eligible records of patients referred to coronary CT in the time period from April 1, 2015 to December 31, 2015; this period was purposefully chosen to be prior to all physicians' knowledge of the audit to avoid the potential for Hawthorne effect.
Data collection and analysis
Pertinent patient data was directly entered into an Excel spreadsheet (Microsoft Corp., Redmond, WA, USA) from two sources:
CT scan records for identifying details of patients referred to coronary CT, along with details of the CT scan procedure
Patient medical records for additional details regarding referred patients, including family history, previous test results, reason for referral to CT, contraindications to imaging and coronary artery disease (CAD) risk scores.
Patient records were irrevocably anonymized by removing or replacing all potentially identifiable data.
After the information was extracted from the aforementioned sources, each case was meticulously audited against the guidelines to assess appropriateness. To ensure applicability of results, all scoring systems and definitions used are either recommended or referenced by the guidelines.
The guidelines take into account a plethora of clinical information regarding each case referred to CCTA to characterize it into one of 93 clinical scenarios where coronary CT could be potentially used; each scenario is associated with a numerical score ranging from 1 to 9, which is derived from available clinical evidence and an independent technical panel of experts using a modified Delphi technique.[3] The three possible characterizations of appropriateness are appropriate (7–9), uncertain (4–6), and inappropriate (1–3).
Cases where the CT scan and/or patient records were inadequate to yield an indication from the guidelines were excluded. Since this audit sought to establish the appropriateness of CCTA use, noncontrast CT scans ordered to calculate the coronary calcium score were not included. All cases were consistent with assumptions the guidelines make regarding the quality standards of CCT imaging.
Statistical analysis
Continuous variables are presented as median (Q1, Q3), whereas categorical variables are presented as frequency (% of n). Differences in the clinical characteristics of the analysis sample based on the AUC group were analyzed using the Chi-square test for categorical variables and Kruskal–Wallis test for continuous variables. Statistical significance was defined as a P < 0.05. Statistical analysis was performed using SPSS version 21.0 (IBM Corp., Chicago, Illinois, USA).
RESULTS
Study group characteristics
The audit initially identified 315 records of patients referred to coronary CT in the specified time frame. Of these records, 81 records were excluded collectively due to the cancellation of the CT scan (48 records) or insufficient information in the databases to yield an appropriate score from the guidelines (33 records); the remaining 234 records constituted the analysis sample.
The majority of cancelled scans were aborted by the attending cardiologists in light of a high calcium score from a preceding noncontrast coronary CT. Other reasons for cancellation include evidence of renal insufficiency and nonideal factors for imaging, such as the inability of patients to hold their breath.
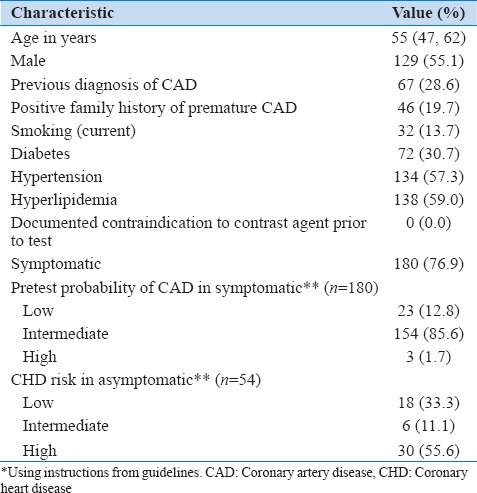
The clinical characteristics of the analysis sample are illustrated in Table 1. The median age of the analysis sample was 55 years (range 15–84 years), with 55.1% of records belonging to male patients.
Table 1.
Clinical characteristics of analysis sample (n=234)
One patient was noted to have developed an anaphylactic reaction to contrast agent.
Reasons for referral
Overall, detection of CAD was by far the most common reported reason for referral to CCTA, with 174 (74.4%) of referrals falling into this category. The other reasons for referral are results of previous tests (20.5%), evaluation of cardiac structure and function (3.0%), and postrevascularization (2.1%).
Appropriateness of referrals
Figure 1 illustrates the proportion of referrals that fall into each AUC category.
Figure 1.
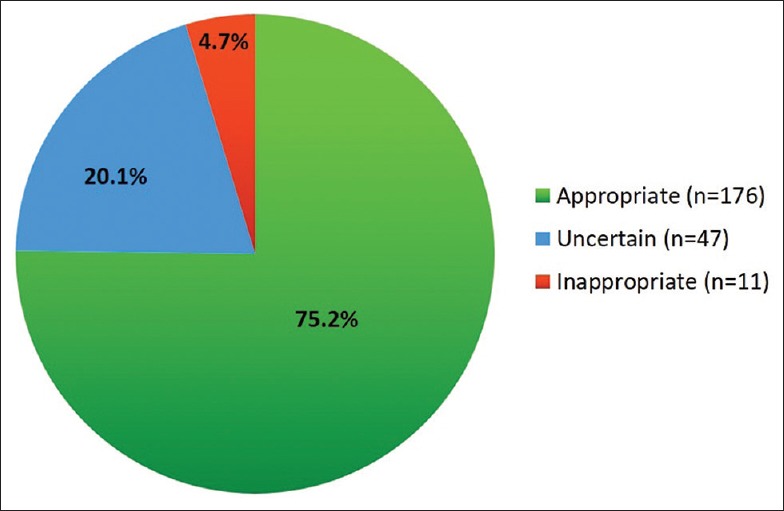
Pie chart illustrating the proportion of referrals that fall into each appropriate use criteria category
Table 2 compares the reasons for referral according to AUC category. Among referrals deemed appropriate (n = 176, 75.2%), the most common indication by far was CAD detection in patients with suspected ischemic equivalent with an intermediate pretest probability of CAD (116 cases, 65.9%). Prior test results constituted the second most common indication for referrals that were deemed appropriate (38 cases, 21.6%).
Table 2.
Reported reasons for coronary computed tomography angiography referral according to appropriate use criteria category attributed to analysis sample records (n=234)
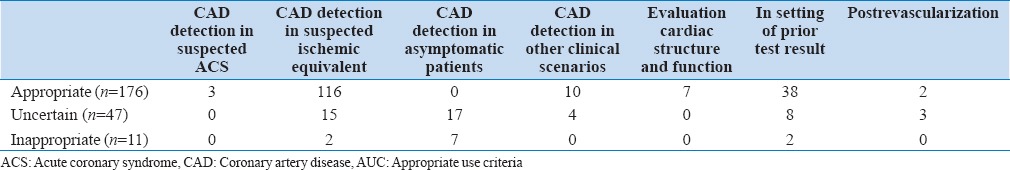
In contrast, referrals deemed inappropriate (n = 11, 4.7%) were predominantly requested to detect CAD in asymptomatic patients at low or intermediate risk of CAD (seven cases, 63.6%). The remainder of referrals deemed inappropriate fall into two equally contributing categories: CAD detection in suspected ischemic equivalent in patients at high risk of CAD (two cases, 18.2%) and periodic repeat testing in setting of prior test results in stable or asymptomatic patients (two cases, 18.2%).
Of referrals that fall into the uncertain category (n = 47, 20.1%), the most common indications were detection of CAD in asymptomatic patients at high risk of CAD (17 cases, 36.2%) and detection of CAD in suspected ischemic equivalent in patients at low risk of CAD (15 cases, 31.9%).
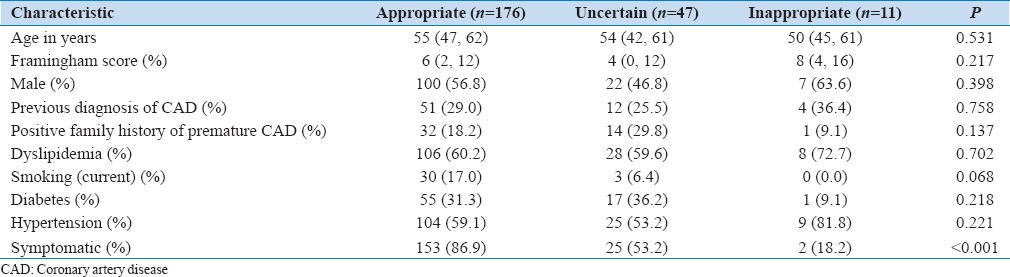
Table 3 illustrates the differences in clinical characteristics of records according to AUC category. In general, clinical characteristics are relatively similar in all groups, with the only statistically significant difference being symptomatic state (P < 0.001).
Table 3.
Comparison of clinical characteristics of records according to appropriate use criteria category
DISCUSSION
This is the first reported study in Bahrain which sought to assess CCTA referral patterns according to the latest 2010 AUC guidelines. This study analyzed the records of patients referred to CCTA in a 9-month period, making it robust against the short-term temporal trends in CCTA referral patterns.
In general, the results demonstrate favorable referral patterns, with a relatively high rate of appropriate use and a rate of inappropriate use that is comparable to the lowest rates reported in studies using the same guidelines[9,10,11] [Figure 2].
Figure 2.
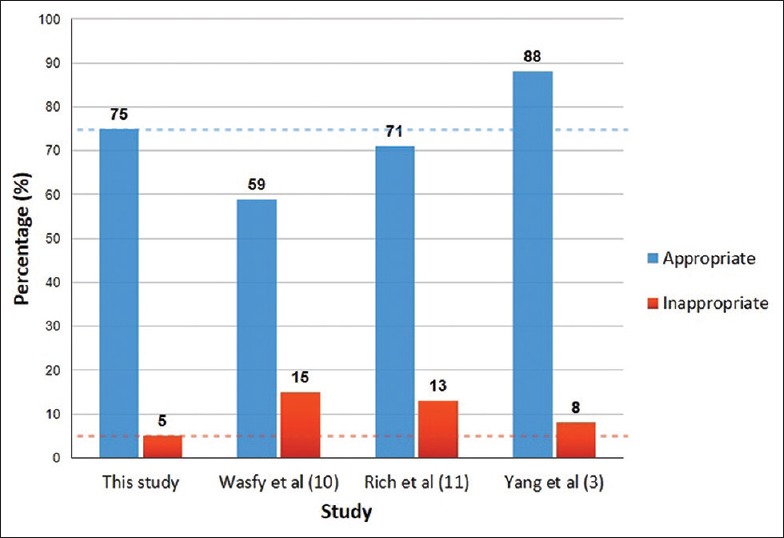
Bar chart comparing coronary computed tomography angiography referrals in this study to those reported in other studies using the 2010 appropriate use criteria guidelines
These results indicate proper, relatively efficient utilization of CCTA scans in the Mohammed bin Khalifa Cardiac Center that is largely in line with published guidelines.
As evident from the clinical characteristics of the study sample, patients who were referred to CCTA were predominantly symptomatic with a low or intermediate risk of CAD. This further reinforces the appropriateness of the referrals as patients in this category are likely to benefit from the high-negative predictive value that CCTA offers, providing an effective method of ruling out CAD and avoiding the risks of invasive angiography.[12] Hence, it is not surprising that the detection of CAD in symptomatic patients was identified as the most common appropriate indication for referral to CCTA, both by this study and in similar studies.[13,14]
Referrals that fall into inappropriate AUC category also showed resemblance to those reported in similar studies; “CAD detection in asymptomatic patients with low- or intermediate-risk of CHD” constituted the majority of inappropriate indications in this study and most studies which reported this statistic.[11,13,14] This striking similarity can possibly reflect universal physician misconceptions regarding the utilization of CCTA in this particular patient group. If so, intervention in the form of a quality improvement program is likely to be beneficial, as interventions aiming to rectify previously assessed inappropriate CCTA referrals were proven to be efficacious in significantly lowering the rates of inappropriate CCTA scans.[8,13] This study has demonstrated a statistically significant higher proportion of asymptomatic patients compromising the inappropriate AUC group relative to other groups (P < 0.001), indicating that paying particular heed to asymptomatic patients' clinical situation prior to their referral to CCTA may also be efficacious in decreasing inappropriate referrals.
Interestingly, this study revealed that a considerable proportion of referrals were deemed “uncertain” by guidelines, echoing a universal pattern seen in similar studies.[9,10,13,14,15] This is a significant obstacle; one fifth of referrals analyzed fall into this category, making it impossible to appreciate or act on the appropriateness of these referrals. This highlights the need to reach a consensus on such cases to refine and update the current guidelines, which will facilitate a better understanding on the appropriateness of CCTA referrals and provide valuable guidance on how inappropriate scans can be minimized.
Study limitations
This study was conducted with the underlying assumption that all pertinent data that physicians' used to make a clinical decision is documented in the databases. Any information not documented could have resulted in misclassification. Considering the relatively thorough documentation of patient information in the databases analyzed and the exclusion of cases with clearly insufficient data, the effect of this assumption on data accuracy is expected to be limited.
While the guidelines take into account a multitude of clinical parameters to yield an appropriateness score, they did not take into consideration the type of scan mode or radiation dose associated with CCTA imaging; although the variation in radiation dose for spiral CT imaging may not vary significantly between hospitals to warrant special consideration, the “Flash” scan mode of the DSCT scanner used in Mohammed bin Khalifa Cardiac Center is associated with a radiation dose of < 1 mSV.[5] Ideally, this relatively low-radiation dose should be taken into account as part of the benefit-to-risk analysis. Taking this into consideration would potentially lower the already small proportion of referrals deemed “inappropriate” by this audit.
CONCLUSION
This audit provides evidence of appropriate and efficient use of CCTA in the Mohammed bin Khalifa Cardiac Center, identifying limited room for improvement. Setting up a continuous quality improvement system that incorporates AUC guidelines is recommended to maintain and further enhance current CCTA referral patterns. Reaching a consensus on “uncertain” scenarios in the guidelines is required to gain a deeper understanding of the appropriateness of CCTA referrals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Dr. Leena Sulaibeekh and the CT department staff for their assistance in data collection. We would also like to thank the Sheikh Mohammed bin Khalifa Cardiac Centre staff for their assistance in making this research possible.
REFERENCES
- 1.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, et al. Assessment of coronary artery disease by cardiac computed tomography: A scientific statement from the American Heart Association Committee on cardiovascular imaging and intervention, council on cardiovascular radiology and intervention, and committee on cardiac imaging, council on clinical cardiology. Circulation. 2006;114:1761–91. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 2.Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, et al. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: A report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Catheter Cardiovasc Interv. 2010;76:E1–42. doi: 10.1002/ccd.22495. [DOI] [PubMed] [Google Scholar]
- 3.Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology foundation appropriate use criteria task force, the society of cardiovascular computed tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular imaging, the society for cardiovascular angiography and interventions, and the society for cardiovascular magnetic resonance. J Cardiovasc Comput Tomogr. 2010;4:407.e1–33. doi: 10.1016/j.jcct.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Hadamitzky M, Freissmuth B, Meyer T, Hein F, Kastrati A, Martinoff S, et al. Prognostic value of coronary computed tomographic angiography for prediction of cardiac events in patients with suspected coronary artery disease. JACC Cardiovasc Imaging. 2009;2:404–11. doi: 10.1016/j.jcmg.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Achenbach S, Marwan M, Ropers D, Schepis T, Pflederer T, Anders K, et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010;31:340–6. doi: 10.1093/eurheartj/ehp470. [DOI] [PubMed] [Google Scholar]
- 6.Stolzmann P, Leschka S, Scheffel H, Krauss T, Desbiolles L, Plass A, et al. Dual-source CT in step-and-shoot mode: Noninvasive coronary angiography with low radiation dose. Radiology. 2008;249:71–80. doi: 10.1148/radiol.2483072032. [DOI] [PubMed] [Google Scholar]
- 7.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–7. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 8.Chaudhuri D, Montgomery A, Gulenchyn K, Mitchell M, Joseph P. Effectiveness of quality improvement interventions at reducing inappropriate cardiac imaging: A Systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2016;9:7–13. doi: 10.1161/CIRCOUTCOMES.115.001836. [DOI] [PubMed] [Google Scholar]
- 9.Wasfy MM, Brady TJ, Abbara S, Nasir K, Hoffmann U, Cury RC, et al. Comparison of cardiac computed tomography examination appropriateness under the 2010 revised versus the 2006 original appropriate use criteria. J Cardiovasc Comput Tomogr. 2012;6:99–107. doi: 10.1016/j.jcct.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Rich ME, Utsunomiya D, Simprini LA, Weigold WG, Weissman G, Taylor AJ. Prospective evaluation of the updated 2010 ACCF cardiac CT appropriate use criteria. J Cardiovasc Comput Tomogr. 2012;6:108–12. doi: 10.1016/j.jcct.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Yang T, AM, Van Slooten A, Mahan M, Ananthasubramaniam K. The impact of appropriate use of coronary cardiac computed tomography on downstream resource utilization and patient management. Int J Cardiovasc Res. 2015;4 DOI 10.4172/2324-8602.1000240. [Google Scholar]
- 12.Abidov A, Gallagher MJ, Chinnaiyan KM, Mehta LS, Wegner JH, Raff GL. Clinical effectiveness of coronary computed tomographic angiography in the triage of patients to cardiac catheterization and revascularization after inconclusive stress testing: Results of a 2-year prospective trial. J Nucl Cardiol. 2009;16:701–13. doi: 10.1007/s12350-009-9117-6. [DOI] [PubMed] [Google Scholar]
- 13.Chinnaiyan KM, Peyser P, Goraya T, Ananthasubramaniam K, Gallagher M, Depetris A, et al. Impact of a continuous quality improvement initiative on appropriate use of coronary computed tomography angiography. Results from a multicenter, statewide registry, the Advanced Cardiovascular Imaging Consortium. J Am Coll Cardiol. 2012;60:1185–91. doi: 10.1016/j.jacc.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 14.Murphy MK, Brady TJ, Nasir K, Gazelle GS, Bamberg F, Truong QA, et al. Appropriateness and utilization of cardiac CT: Implications for development of future criteria. J Nucl Cardiol. 2010;17:881–9. doi: 10.1007/s12350-010-9252-0. [DOI] [PubMed] [Google Scholar]
- 15.Carpeggiani C, Marraccini P, Morales MA, Prediletto R, Landi P, Picano E. Inappropriateness of cardiovascular radiological imaging testing; a tertiary care referral center study. PLoS One. 2013;8:e81161. doi: 10.1371/journal.pone.0081161. [DOI] [PMC free article] [PubMed] [Google Scholar]


