Abstract
Background
Ischemic stroke is often a sequel of atherosclerotic risk factors. Carotid intima-media thickness (CIMT) is a surrogate marker of early atherosclerotic changes.
Purpose
It was hypothesized that CIMT is associated with ischemic stroke in adults across all ages.
Methods
A case control study was performed on 163 diagnosed cases of first-time ischemic stroke and age-(±1 SD) and gender-matched healthy control attendants reporting at a tertiary care hospital. Data were collected on atherosclerotic risk factors for ischemic stroke. CIMT from both the carotids was measured using carotid vascular Doppler. The demographic profile and CIMT with atherosclerotic risk factors of cases and controls across different age groups were compared using unpaired t test if they passed the test of normality, else the Mann-Whitney test was used. OR for vascular risk factors for the development of stroke was calculated. The relationship of CIMT to atherosclerotic risk factors was analyzed by using Spearman correlation and regression analysis. The level of significance was set at 0.05.
Results
Age-specific value of CIMT was significantly higher in stroke cases than in age-matched controls across all age groups. Right CIMT, along with the history of hypertension (HTN; OR 2.3), are important risk factors for ischemic stroke in the younger age group (20–40 years). With increasing age along with the history of HTN and right CIMT (OR >7), presence of plaque (OR 6.3) and daily smoking (OR 5.1) are also significant risk factors. CIMT is significantly related to the daily alcohol and smoking intake and the presence of plaques. Right CIMT is positively related to increasing age in normal population (R2 = 0.041; p < 0.001).
Conclusions
Right CIMT and comorbid HTN are significant risk factors associated with the development of ischemic stroke across all adult age groups.
Keywords: Cerebrovascular accidents, Vascular risk, Atherosclerosis
Introduction
Stroke is often a sequel of modifiable risk factors like diabetes mellitus (DM), hypertension (HTN), smoking, and hyperlipidemia [1] which induces pathological changes of atherosclerosis in blood vessels. The reduction in diameter of vessels due to hypertrophy or entropic inner modeling provokes the development of cerebro-and cardiovascular diseases [2]. The progression of carotid intima-media thickness (CIMT) is a marker of early vascular wall damage, appearing in the process of atherosclerosis [3].
CIMT is safe, reliable, and inexpensively measured. It has recently been seen as a strong predictor of future vascular events such as myocardial infarction and stroke [4] and to evaluate the success of anti-lipidemic drug intervention [5]. More recently, it has been utilized in epidemiologic studies to detect subclinical vascular disease and assess its relation to cardiovascular disease (CVD) risk factors and stroke [6, 7, 8]. A positive association exists between CIMT and the risk of subsequent cardiovascular events including stroke, independent of all major risk factors, in Asian populations [9, 10] and in the western world [11, 12, 13].
Case control studies for the assessment of risk factors of stroke in India is limited and done in smaller group of stroke patients [14]. At the moment, there is no consensus on the role of increased CIMT in the occurrence of ischemic stroke in adults across all age groups. In this study, we investigate the hypothesis that CIMT is associated with stroke development in adults across all age groups.
Methods
The case control study was done on 163 diagnosed cases of ischemic stroke based on CT and MRI findings, 163 age-matched control (±1 SD), and gender. The study period was between August 2012 and July 2013. The study was approved by the HIHT University Ethical Committee vide reference number HIHT/PHARMA/E-1/2011/91, and confers to their guidelines. After taking written and informed consent of the patients (if unconscious: caregiver) and control volunteers, the data were collected by interview method. The data collected included demographic profile, prior history of atherosclerotic disease, diabetes, HTN, and history of smoking and alcohol. Patients with stroke of more than 2 weeks, patients on hypolipedemic drugs for more than 1 year, and peripheral vascular disease were excluded. Electrocardiography was done to quantify the cardiac function. Carotid vascular Doppler was performed for vascular correlates IMT from both the carotids. Other investigation performed was total serum cholesterol. The control group was also investigated for similar tests.
Carotid Measurements
The CIMT measurements were made using Doppler with a 0.75 MHz linear superficial probe in B-mode. All readings were taken and interpreted by the same investigator. The point of measurement was taken 1 cm proximal to the carotid bulb at the site of maximum thickness, avoiding the plaque area. The ultrasound machine used had a sensitivity range of 0.1 mm, that is, each division was equivalent to 0.1 mm.
Other Investigations
The total serum cholesterol in inter-digestive period was measured in both cases and controls by NABL accredited reference laboratory of the hospital.
Statistical Analysis
All calculations were performed using SPSS software version 17. The demographic profile and CIMT with atherosclerotic risk factors of cases and controls were compared using unpaired t test if they passed the test of normality, else the Mann-Whitney test was used. CIMT across different age groups was compared among cases and controls using unpaired test. OR of various vascular risk factors including CIMT, HTN, DM, presence of plaque, smoking, and alcohol are calculated for the development of stroke. The presence of plaque and IMT in the right and left carotids are presented as frequency. The cases were analyzed for the IMT and its strength of relation to HTN, total cholesterol, daily smoking, daily alcohol, and presence of plaque using Spearman correlation. The level of significance was set at 0.05.
Results
The study was conducted on 163 patients, diagnosed cases of ischemic stroke (CT scan suggestive of non-hemorrhagic infarction). There were more number of males (78%) presenting with ischemic stroke as compared to females (22%). Thirty-two percent of ischemic stroke cases were having a H/O HTN. This was followed by those having DM with HTN (21.5%) and 14/163 had a H/O earlier stroke. More than 50% of ischemic stroke patients were daily smokers (Table 1a).
a.
Ischemic stroke patients and controls a Demographic distribution
| Parameters | Cases (n = 163) | Controls (n = 163) | p value |
|---|---|---|---|
| Demographic factors | |||
| Males, n (%) | 127 (78) | 123 (75.4) | |
| Females, n (%) | 36 (22) | 39 (24) | |
| Age, years, mean ± SD | 58.43±9.1 | 57.09±8.7 | ns# |
| Average BMI, kg/m2 | 26.24±3.71 | 26.91±3.9 | ns# |
| Past history of diseases, n (%) | |||
| HTN | 52 (32.0) | 11 (6.7) | <0.001 |
| DM | 7 (4.0) | 13 (7.9) | ns |
| DM with HTN | 35 (21.5) | 6 (3.6) | <0.001 |
| CVA | 14 (8.5) | 0 | – |
| Addiction habits, n (%) | |||
| Daily smoking | 95 (58) | 50 (30.6) | <0.001 |
| Daily alcohol | 39 (24) | 43 (26.3) | ns |
| Blood investigations, n (%) | |||
| Total serum cholesterol, >220 mg/dL | 19 (12.0) | 29 (17.9) | ns# |
t test and chi-square test; ns, non-significant. CVA, cerebrovascular accident; HTN, hypertension; DM, diabetes mellitus.
b.
CMIT distribution
| CIMT, mm | Cases (n = 163) | Controls (n = 163) | p value |
|---|---|---|---|
| Right IMT | 0.77±0.36 | 0.56±0.13 | <0.0001 |
| Left IMT | 0.73±0.29 | 0.57±0.14 | <0.0001 |
| Right IMT with DM | 0.88±0.12 | 0.53±0.13 | 0.06 |
| Left IMT with DM | 0.93±0.11 | 0.59±0.11 | 0.003 |
| Right IMT with HTN | 0.75±0.16 | 0.60±0.10 | <0.0001 |
| Left IMT with HTN | 0.72±0.18 | 0.59±0.12 | 0.006 |
| Right IMT with DM and HTN | 0.76±0.2 | 0.58±0.11 | 0.06 |
| Left IMT with DM and HTN | 0.70±0.18 | 0.71±0.12 | 0.15 |
| Right IMT in daily smokers | 0.78±0.13 | 0.55±0.09 | <0.0001 |
| Left IMT in daily smokers | 0.70±0.15 | 0.56±0.1 | <0.0001 |
Values are mean ± SD; p < 0.05 is significant; t test.
The cases had the mean value of right CIMT higher than the age-matched controls (0.77 ± 0.36 vs. 0.56 ± 0.13 mm), and the difference was highly significant (p < 0.0001). Statistically significant difference was also observed when groups were analyzed with risk factors such as HTN and smoking. When the left CIMT value was compared, the case group was found to have higher values (0.73 ± 0.29 mm) compared to controls 0.57 ± 0.14 mm (p < 0.001). This difference was also present when groups were analyzed with risk factors such as HTN, diabetes, and smoking. The difference was found to be statistically significant (Table 1b).
When CIMT was compared among different age groups (20–40; >40-<60; >60 years), the cases had a significantly higher value than age-matched controls (p < 0.05; p < 0.01; p < 0.001; Table 2).
Table 2.
Baseline characteristics of cases and controls across different age groups
| Parameters | Cases (n = 163) |
Controls (n = 163) |
||||
|---|---|---|---|---|---|---|
| 20–40 years (n = 16) | >40–60 years (n = 60) | ≥60 years (n = 87) | 20–40 years (n = 17) | >40–60 years (n = 60) | ≥60 years (n = 89) | |
| Age, years, mean ± SD | 33.53±5.2 | 49.5±4.5 | 69±9.0 | 37.3±5.0 | 47.93±4.5 | 65.58±6.0 |
| Right CIMT, mm, mean ± SD | 0.67±0.12* | 0.71±0.16### | 0.83±0.12^^^ | 0.55±0.08 | 0.55±0.1 | 0.69±0.06 |
| Left CIMT, mm, mean ± SD | 0.71±0.11* | 0.69±0.17## | 0.76±0.17^^^ | 0.57±0.09 | 0.56±0.09 | 0.60±0.1 |
| Right CIMT ≥ age group-specific cut-off | 4 | 18 | 22 | 2 | 5 | 4 |
| Left CIMT ≥ age group-specific cut-off | 6 | 20 | 27 | 4 | 5 | 6 |
Comparison between 20–40 years.
p < 0.05; comparison between 40–60 years.
p < 0.01
p < 0.001; comparision between ≥60 years.
p < 0.001; t test.
In the absence of a well-defined population cut-off value for CIMT, we used control mean IMT plus 2 SDs for each of the age groups [14]. The age group-specific cut-off IMT value thus calculated was 0.71 mm for 20–40 years; 0.74 mm for >40-<60 years, and 0.82 mm for >60 years. Such a value would include 95% of age-specific controls. It gave an average specificity of >90%, with a sensitivity of 35%. The positive predictive value was 87%, and the negative predictive value was 60%.
The age-wise analysis of the left and right CIMT showed that the mean CIMT values increased from younger to older age groups. Comparing the mean IMT values with corresponding age-specific controls showed that the cases had a significantly higher value than controls, both with right and left carotid arteries. The frequency of subjects with more than age-specific IMT values were almost equally represented in both the right and left CIMT (Table 2).
Risk assessment for the development of stroke with atherosclerotic covariates shows that right CIMT and H/O HTN were important risk factors among the young population with the OR of developing stroke being ∼2.5 times the control. However, this was non-significant, may be due to the small size of the sample. With increase in the age (40–60 years), HTN becomes the most important risk factor (OR 6.9; p < 0.01) followed by CIMT and H/O plaques (OR 4.7; p < 0.05), and daily smoking (OR 3.7; p < 0.01) for the development of ischemic stroke. In older adults (>60 years), odds of developing ischemic stroke is increased with higher IMT (>0.82 mm) in the carotids and H/O HTN (OR >7) followed by H/O plaques and daily smoking (p < 0.01) as compared to age-matched controls. Right CIMT and H/O HTN are significant risk factors associated with the development of ischemic stroke across all age groups (Table 3).
Table 3.
Age group wise strength of association of vascular risk factors in ischemic stroke cases as compared to matched controls
| Parameters | OR (95% CI) |
|||||
|---|---|---|---|---|---|---|
| 20–40 years | p value | >40–60 years | p value | ≥60 years | p value | |
| Right CIMT, mm | 2.3 (0.38–16) | ns | 4.7 (1.6–13.7) | 0.004 | 7.1 (3.3–21.8) | 0.0002 |
| Left CIMT, mm | 1.9 (0.43–8.2) | ns | 5.5 (1.9–15.8) | 0.001 | 6.2 (2.4–16.6) | 0.0001 |
| H/O plaques | – | – | 4.7 (1.7–17.9) | 0.02 | 6.3 (2.9–19.3) | <0.0001 |
| H/O DM | – | – | 0.47 (0.28–2.7) | ns | 0.98 | ns |
| H/O HTN | 2.3 (0.36–15) | ns | 6.9 (1.8–25.2) | 0.002 | 7.5 (3.5–18.6) | <0.0001 |
| H/O DM with HTN | – | – | 3.8 (1.2–9.2) | 0.02 | – | – |
| H/O daily smoking | – | – | 3.7 (1.7–8) | 0.001 | 5.1 (2.5–10.1) | 0.0006 |
| H/O daily alcohol | 0.46 (0.22–0.97) | 0.49 (0.24–0.99) | ns | |||
CIMT, carotid intima-medial thickness; HTN, hypertension; DM, diabetes mellitus; ns, non-significant.
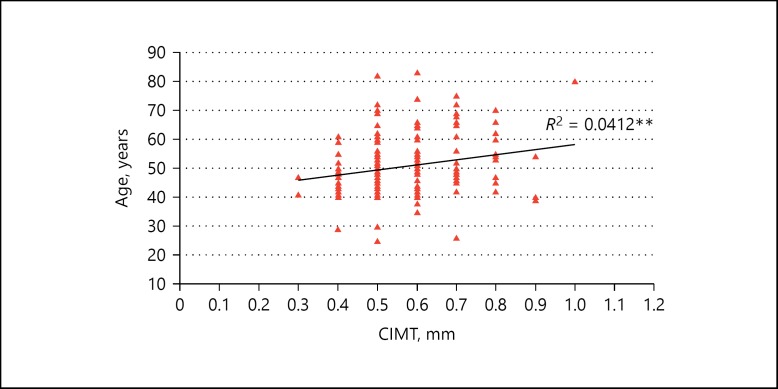
The presence of ischemic stroke was correlated with age, IMT of both the carotids, and presence of plaque. No significant correlation of WHR, presence of plaque, daily smoking, daily alcohol consumption and S T were observed. Cholesterol with IMT of both the carotids was observed in cases after controlling for age and BMI as duration and amount of consumption were not recorded. However, age was positively related and would explain 4% of the prediction (R2 = 0.041; p ≤ 0.001) of right CIMT in the control population (Fig. 1).
Fig. 1.
Relation of carotid intima-media thickness with increasing age in the normal population.
Discussion
The current CVD risk stratification tools for the general population are focused on life time modifiable risk factors such as DM, HTN, and dyslipidemia, which in long term may contribute to atherosclerotic changes in arterial thickness [15]. CIMT is a surrogate marker for the early detection of atheromatous changes and is easily accessed by non-invasive B-mode ultrasound [16]. Consideration of both right and left carotids could improve the prediction by assuring the true presence of large parameters [17].
In this study, both the carotids were measured for the IMT and were found to be significantly higher in cases (0.77 ± 0.36 and 0.73 ± 0.29 mm) than in controls (0.56 ± 0.13 and 0.57 ± 0.14 mm; p < 0.001), which persisted in different age groups. Difference between stroke cases and controls were also observed by Sahoo et al. [14], who reported significantly higher mean CIMT (0.782 ± 0.19 mm) than in controls (0.594 ± 0.98 mm; p < 0.0001) but in south Indian population. Similar to our study, the difference persisted across all age groups. Mukherjee et al. [18] reported a significantly higher CIMT values among stroke cases as compared to controls, but the mean values were lower (0.66 vs. 0.32 mm) than our study; however, the sample size was small and the controls were not matched with the cases.
Study by Cupini et al. [19] reported a mean value of CIMT (>1 mm), which was associated with the development of stroke as compared to 0.91 mm in controls; however, the study population was of more than 70 years of age and of different ethnicity. GENIC, a case control study had similar mean IMT values (0.79 mm) in stroke patients compared to our study. The basal characteristics of population were similar to our study, except the study was done on higher age group and only on hypertensive patients [10].
Higher values of CIMT in stroke patients with DM, HTN, and smokers have been previously reported in Caucasian population [20]. Our study also reported a higher value of CIMT among stroke cases with the above co-morbidities, and the difference was statistically significant. Similar results were observed by Sahoo et al. [14], where the difference was significant in the subgroup analysis by risk factors such as HTN, diabetes, and smoking between patients and controls. Study by Das et al. [21] on Asian Indian stroke cases demonstrated an increased IMT with grades of plaque in type II diabetic stroke patients, but in small population of cases of ischemic stroke with age-matched controls. Similar to our study, the CIMT was significantly higher in hypertensive patients and smokers. Study in eastern Indian tertiary care hospital by Saha et al. [22] in 50–60 years of age group also found a higher value of CIMT among ischemic stroke patients with diabetes in both left and right carotids as compared to controls, but the difference was not significant.
Several studies have reported a positive correlation of CIMT, cardiovascular risk and increased incidence of stroke among the western population [23, 24]. Risk assessment of vascular covariates among stroke cases showed that right CIMT, HTN, and smoking were strongly associated with the development of stroke across all age groups in Indian population. Present research showed a very interesting pattern of risk factor transition in age-wise analysis. Both right CIMT and HTN are important risk factors for the development of stroke among younger population with OR more than 2, although statistically non-significant, which may be due to the small number of subjects. With the increase in age, HTN (OR 6.9; p < 0.01) became the important risk factor followed by CIMT and presence of plaque (OR 4.7; p < 0.01). Daily smoking also shows more than 3 times risk of ischemic stroke as compared to age- and gender-matched controls. In older adults (>60 years), the risk increases to >5 times for the above risk factors. The analysis shows that with advancement of age, the risk of stroke due to increased right CIMT becomes less important and covariate such as HTN becomes a more important risk factor, while smoking becomes a contributor for the development of stroke in 4 decades, that is, more than 60 years.
Right CIMT is an important marker, especially for the young population, which may not have developed comorbid risk factors. CIMT (age-specific cut-off 0.71mm [≤40 years]; 0.74mm [40–60 years]; 0.82mm [≥60 years]) of right side may be a significant risk factor for the development of ischemic stroke in Indian population. Cross-sectional study by Salim Hasim in South East Asia also shows a strong association of CIMT (>1.0 mm) and stroke (p = 0.008) in the Indonesian population [25]. A direct correlation exists because IMT is a marker of generalized atherosclerosis which plays an important role in the pathogenesis of cerebrovascular events such as stroke. Rotterdam elderly case control single center study in a subgroup of population of 55 years of age or older also showed an association between common CIMT and the risk of stroke [26]. The differences between their study and our study may be explained by the race of population, age group, limited number of subjects, and the methodology used. In our study, the presence of ischemic stroke was correlated with age, IMT of both the carotids, and presence of plaque but only right CIMT is positively related to increasing age in the normal population (R2 = 0.0412**).
Our results extend their findings by showing that common CIMT has a strong correlation, with the incidence of stroke even in young age group. This implies that common CIMT may be used as a predictor of cerebrovascular events across all age groups in Indian population.
Limitations
It was a single-center study done in a tertiary care hospital. Since our study was not a prospective study, we could not calculate the hazard ratios for CIMT values.
Author's Contribution
Each author has made substantial contribution towards preparing the manuscript and the work reported in it.
Disclosure Statement
The authors declare no conflict of interest. The manuscript is complied with International Committee of Medical Journal Editor's guidelines. This study received funding from Indian Council of Medical Research, and India vide project No. 5/4-5/55/Neuro/2011-NCD-I.
Acknowledgement
Authors are thankful to the Indian Council of Medical Research for funding the study. Authors also acknowledge HIMS, SRH University for providing the facilities for conducting the study. We also acknowledge Ms. Nidhi Mittal, appointed Junior research fellow, for helping us conduct the study.
References
- 1.Libby P. Prevention and treatment of atherosclerosis. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison's Principles of Internal Medicine. ed 16. McGraw-Hill Companies; 2005. pp. 1430–1433. [Google Scholar]
- 2.De Silva DA, Woon FP, Lee MP, Chen CP, Chang HM, Wong MC. South Asian patients with ischemic stroke: intracranial large arteries are the predominant site of disease. Stroke. 2007;38:2592–2594. doi: 10.1161/STROKEAHA.107.484584. [DOI] [PubMed] [Google Scholar]
- 3.Valdueza JM, Schreiber SJ, Roehl JE, Klingebeil R. Neuro-Sonology and Neuroimaging of Stroke. Stuttgart: Ed. Thieme; 2008. pp. 13–53. [Google Scholar]
- 4.Simon A, Megnien JL, Chironi G. The value of carotid intima-media thickness for predicting cardiovascular risk. Arterioscler Thromb Vasc Biol. 2010;30:182–185. doi: 10.1161/ATVBAHA.109.196980. [DOI] [PubMed] [Google Scholar]
- 5.Hunt KJ, Evans GW, Folsom AR, Sharrett AR, Chambless LE, Tegeler CH, Heiss G. Acoustic shadowing on B-mode ultrasound of the carotid artery predicts ischemic stroke: the atherosclerosis risk in communities (ARIC) study. Stroke. 2001;32:1120–1126. doi: 10.1161/01.str.32.5.1120. [DOI] [PubMed] [Google Scholar]
- 6.Hollander M, Bots ML, Del Sol AI, Koudstaal PJ, Witteman JC, Grobbee DE, Hofman A, Breteler MM. Carotid plaques increase the risk of stroke and subtypes of cerebral infarction in asymptomatic elderly: the Rotterdam study. Circulation. 2002;105:2872–2877. doi: 10.1161/01.cir.0000018650.58984.75. [DOI] [PubMed] [Google Scholar]
- 7.Prati P, Tosetto A, Vanuzzo D, Bader G, Casaroli M, Canciani L, Castellani S, Touboul PJ. Carotid intima media thickness and plaques can predict the occurrence of ischemic cerebrovascular events. Stroke. 2008;39:2470–2476. doi: 10.1161/STROKEAHA.107.511584. [DOI] [PubMed] [Google Scholar]
- 8.Vemmos KN, Tsivgoulis G, Spengos K, Papamichael CM, Zakopoulos N, Daffertshofer M, Lekakis JP, Mavrikakis M. Common carotid artery intima-media thickness in patients with brain infarction and intracerebral haemorrhage. Cerebrovasc Dis. 2004;17:280–286. doi: 10.1159/000077338. [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto K, Sera Y, Nakamura H, Ueki Y, Miyake S. Correlation between common carotid arterial wall thickness and ischemic stroke in patients with type 2 diabetes mellitus. Metabolism. 2002;51:244–247. doi: 10.1053/meta.2002.28971. [DOI] [PubMed] [Google Scholar]
- 10.Touboul PJ, Elbaz A, Koller C, Lucas C, Adraï V, Chédru F, Amarenco P. Common carotid artery intima-media thickness and brain infarction: the Etude du Profil Génétique de l'Infarctus Cérébral (GENIC) case-control study: the GENIC investigators. Circulation. 2000;102:313–318. doi: 10.1161/01.cir.102.3.313. [DOI] [PubMed] [Google Scholar]
- 11.Touboul PJ, Labreuche J, Vicaut E, Amarenco P, GENIC Investigators Carotid intima-media thickness, plaques, and Framingham risk score as independent determinants of stroke risk. Stroke. 2005;36:1741–1745. doi: 10.1161/01.STR.0000174490.23495.57. [DOI] [PubMed] [Google Scholar]
- 12.Kitamura A, Iso H, Imano H, Ohira T. Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke. 2004;35:2788–2794. doi: 10.1161/01.STR.0000147723.52033.9e. [DOI] [PubMed] [Google Scholar]
- 13.Hollander M, Hak AE, Koudstaal PJ, Bots ML, Grobbee DE, Hofman A, Witteman JC, Breteler MM. Comparison between measures of atherosclerosis and risk of stroke: the Rotterdam study. Stroke. 2003;34:2367–2372. doi: 10.1161/01.STR.0000091393.32060.0E. [DOI] [PubMed] [Google Scholar]
- 14.Sahoo R, Krishna MV, Subrahmaniyan DK, Dutta TK, Elangovan S. Common carotid intima-media thickness in acute ischemic stroke: a case control study. Neurol India. 2009;57:627–630. doi: 10.4103/0028-3886.57822. [DOI] [PubMed] [Google Scholar]
- 15.Eigenbrodt ML, Bursac Z, Tracy RE, Mehta JL, Rose KM, Couper DJ. B-mode ultrasound common carotid artery intima-media thickness and external diameter: cross-sectional and longitudinal associations with carotid atherosclerosis in a large population sample. Cardiovasc Ultrasound. 2008;6:10. doi: 10.1186/1476-7120-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwee RM, van Oostenbrugge RJ, Hofstra L, Teule GJ, van Engelshoven JM, Mess WH, Kooi ME. Identifying vulnerable carotid plaques by noninvasive imaging. Neurology. 2008;70((24 pt 2)):2401–2409. doi: 10.1212/01.wnl.0000314697.76580.cb. [DOI] [PubMed] [Google Scholar]
- 17.Eigenbrodt ML, Evans GW, Rose KM, Bursac Z, Tracy RE, Mehta JL, Couper DJ. Bilateral common carotid artery ultrasound for prediction of incident strokes using intima-media thickness and external diameter: an observational study. Cardiovasc Ultrasound. 2013;11:22. doi: 10.1186/1476-7120-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mukherjee SC, Basu AK, Bandyopadhyay R, Pal SK, Bandopadhyay D, Mandal SK, Temsusashi Correlation of lipid profile and carotid artery plaque as detected by Doppler ultrasound in ischaemic stroke patients – a hospital-based study. J Indian Med Assoc. 2006;104:325–326. [PubMed] [Google Scholar]
- 19.Cupini LM, Pasqualetti P, Diomedi M, Vernieri F, Silvestrini M, Rizzato B, Ferrante F, Bernardi G. Carotid artery intima-media thickness and lacunar versus nonlacunar infarcts. Stroke. 2002;33:689–694. doi: 10.1161/hs0302.103661. [DOI] [PubMed] [Google Scholar]
- 20.Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337:1521–1526. doi: 10.1016/0140-6736(91)93206-o. [DOI] [PubMed] [Google Scholar]
- 21.Das S, Chakrabarty K, Patnaik M, Roul L, Mohanty J, Singh SC. The relationship of carotid plaque, intima media thickness (IMT), resistivity index (RI) and pulsatility index (PI) in Asian-Indian patients with acute ischemic stroke with and without type 2 DM. Int J Clin Med. 2011;2:561–567. [Google Scholar]
- 22.Saha A, Sinha PK, Paul R, Bandyopadhyay R, Biswas K, Banerjee AK. Study of carotid intima media thickness and its correlation with novel risk factors in ischemic stroke. Neurology Asia. 2011;16:25–31. [Google Scholar]
- 23.O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 24.Petty GW, Brown RD, Jr, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513–2516. doi: 10.1161/01.str.30.12.2513. [DOI] [PubMed] [Google Scholar]
- 25.Harris S. The association of carotid intima-media thickness (cIMT) and stroke: a cross sectional study. New trends in neurosonology and cerebral hemodynamics – an update. Perspect Med. 2012;1:164–166. [Google Scholar]
- 26.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]