To the Editor:
In response to issues raised by Drs. Ley and Collard in their editorial (1) regarding outcome prediction in idiopathic pulmonary fibrosis (IPF), we clarify here certain aspects of our work (2).
The editorial authors repeatedly mention that we identified “serum” biomarkers (1). Plasma is the unclotted cell-free fraction of the blood; serum is obtained after blood is allowed to clot. In our study (2), we identified biomarkers in plasma. Because plasma and serum contain different protein repertoires, we would strongly advocate not using them interchangeably in biomarker discovery or validation.
The editorial authors assert, “biomarker predictors were inconsistently identified in a separate validation cohort,” but fail to discuss the remarkable consistency of our results. Four of the five biomarkers predicted transplant-free survival in both cohorts. More importantly, mortality prediction by our personalized clinical and molecular mortality index (PCMI) was highly consistent between derivation and replication sets, with C-statistics for early mortality exceeding 80% (3). Determining this consistency was possible in this study only because we had two cohorts, unlike all previous peripheral blood biomarker studies in IPF, or as a matter of fact, many recently published clinical risk prediction studies (see examples in References 3–5).
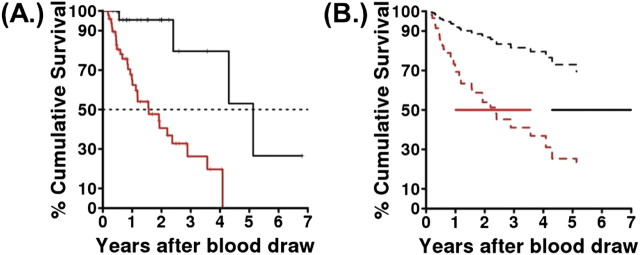
As the editorial authors point out, increased availability of lung transplantation requires that it be addressed in IPF outcome studies. Several data analytic methods can be applied, including the Fine-Gray model cited by the authors, cause-specific incidence models, and multistate models incorporating disease progression, lung transplantation, and mortality (6). In the case of our study, treating lung transplant as a competing risk did not substantially alter the results (Figure 1), highlighting the robustness of PCMI.
Figure 1.
Outcome prediction based on personalized clinical and molecular mortality index (PCMI). Panel A was originally published as Figure 4A in Reference 2. (A) PCMI predicts mortality in idiopathic pulmonary fibrosis. Solid lines show published mortality curves. Red line shows PCMI ≥ 330; black line shows PCMI < 330. Median survival after blood draw was 5.2 and 1.6 years, respectively. (B) Survival curves for mortality with lung transplant as a competing risk. Broken lines are survival curves; solid lines are confidence intervals on the medians from data in Figure 4A; red line shows PCMI ≥ 330; black line shows PCMI < 330 (hazard ratio = 4.37, P = 0.0018). Estimated medians are comfortably within confidence intervals from published analysis.
We agree with the editorial authors that additional studies on molecular biomarkers are needed, but we disagree on what types of studies. Based on the impressive reproducible performance of PCMI in predicting patient outcome at presentation in two cohorts larger than most previously published molecular biomarker studies in IPF, we believe that the question of whether blood proteins contain prognosis-relevant information is largely resolved. Biomarker studies should now be designed to determine the utility of molecular markers in patient management (i.e., transplant prioritization) and to determine whether changes in biomarkers during the course of disease indicate shifts in the patient’s risk profile.
References
- 1.Ley B, Collard HR. Risk prediction in idiopathic pulmonary fibrosis [editorial]. Am J Respir Crit Care Med 2012;185:6–7. [DOI] [PubMed] [Google Scholar]
- 2.Richards TJ, Kaminski N, Baribaud F, Flavin S, Brodmerkel C, Horowitz D, Li K, Choi J, Vuga LJ, Lindell KO, et al. Peripheral blood proteins predict mortality in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2012;185:67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.du Bois RM, Weycker D, Albera C, Bradford WZ, Costabel U, Kartashov A, Lancaster L, Noble PW, Raghu G, Sahn SA, et al. Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011;184:459–466. [DOI] [PubMed] [Google Scholar]
- 4.Collard HR, Calfee CS, Wolters PJ, Song JW, Hong SB, Brady S, Ishizaka A, Jones KD, King TE, Matthay MA, et al. Plasma biomarker profiles in acute exacerbation of idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol 2010;299:L3–L7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kinder BW, Brown KK, McCormack FX, Ix JH, Kervitsky A, Schwarz MI, King TE. Serum surfactant protein-a is a strong predictor of early mortality in idiopathic pulmonary fibrosis. Chest 2009;135:1557–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beyersmann J. Competing risks and multistate models with R. New York: Springer; 2011. [Google Scholar]