To the Editor:
Modern management of asthma requires a comprehensive diagnostic approach and assessment of exacerbations. The former is based on medical history, physical examination, and demonstration of airway instability by bronchial challenges or peak expiratory flow (PEF) monitoring (1). Though measuring the PEF is useful to assess the natural variability of bronchial tone, it is effort dependent, needs cooperation by the patient, may alter airway caliber, and requires a long period of observation (2, 3). In addition, its sensitivity is less than that of bronchial challenges (4) and similar to symptoms (5). Symptoms and use of rescue drugs and PEF monitoring are used for risk prediction, though they weakly correlate with each other and clinical outcomes (6–9), and are usually applied retrospectively, thus precluding prediction of adverse events in real life (10).
Here we provide evidence that home monitoring of inspiratory resistance (Rinsp) by a newly developed noninvasive technology based on forced oscillation technique (FOT) with great sensitivity to assess lung function (11–13) may be a reliable tool to diagnose asthma and predict acute deterioration of airway function.
Ten nonsmokers with mild asthma and 10 healthy control subjects (Table 1) had FOT measured at home for 2 minutes twice a day for 6 consecutive months with a portable FOT device (11). Baseline lung function was normal in the healthy subjects but consistent with mild airflow obstruction in the subjects with asthma, as suggested by an FEV1/slow vital capacity below lower limits of normality and FEV1 as %predicted near normal. The lack of significant differences in Rinsp between groups was presumably the result of the mild peripheral airflow obstruction in asthma, high variability of the measurement, and limited number of subjects in the study. An intuitive user interface provided visual and acoustic feedbacks to the subjects. Artifacts due to glottis closure and anomalous breaths were automatically discarded by the device's software. The data were encrypted and transmitted through the Internet to a central server for storage and further analysis. For each measurement, the mean and standard deviation of Rinsp were used to build time series of its coefficients of variation (CVRINSP) at 2, 4, 8, 16, and 32 consecutive days. Risk predictors for acute deterioration of airway function were estimated from the conditional probability that an increase of Rinsp greater than or equal to twice the predicted respiratory resistance (14) occurred within the next 4, 7, 15, or 30 days given the CVRINSP values observed in the previous 8 days. The trial was approved by the Ethical Committee of the S. Luigi Hospital (Orbassano, Torino, Italy).
TABLE 1.
MAIN ANTHROPOMETRIC AND BASELINE LUNG FUNCTION DATA
| Variables | Subjects with Asthma | P Value | Control Subjects |
| Sex, M/F | 7/3 | 0.08 | 3/7 |
| Age, yr | 35 ± 15 | 0.07 | 47 ± 11 |
| BMI, kg·m−2 | 25 ± 4 | 0.37 | 23 ± 2 |
| FEV1, L | 3.00 ± 0.38 | 0.80 | 3.08 ± 0.69 |
| FEV1, %pred | 87 ± 11 | 0.01 | 108 ± 14 |
| FEV1/SVC, %pred | 85 ± 9 | 0.05 | 93 ± 6 |
| TLC, %pred | 102 ± 11 | 0.23 | 109 ± 11 |
| RV, %pred | 109 ± 34 | 0.86 | 103 ± 20 |
| Rinsp, cmH2O·s·L−1 | 3.51 ± 1.11 | 0.14 | 2.88 ± 0.45 |
Definition of abbreviations: BMI = body mass index; Rinsp = inspiratory resistance at 5 Hz; RV = residual volume; SVC = slow vital capacity; TLC = total lung capacity.
Data are mean ± SD.
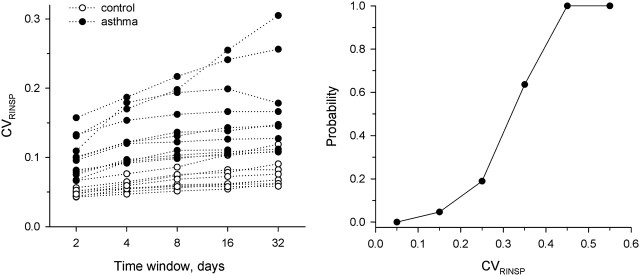
At all time scales (2, 4, 8, 16, and 32 d), CVRINSP was significantly larger in subjects with asthma than in healthy subjects (P < 0.001) (Figure 1, left panel). A time window of only 4 days provided 90% sensitivity and specificity for morning or evening CVRINSP with respect to the diagnosis of the disease.
Figure 1.
(Left panel) Long-term variability of the Rinsp characterized by the coefficient of variation (CVRINSP) of individual subjects measured in the morning in individual subjects with asthma (solid symbols) and healthy subjects (open symbols) plotted against time windows. (Right panel) conditional probability computed on an individual basis that a given CVRINSP calculated over the past 8 days is associated with an increase in Rinsp greater than or equal to twice the predicted respiratory resistance within the next week. Each point of the prediction curve is the average probability of an interval centered on that point.
The occurrence of an acute deterioration of airway function within 1 week was predicted by computing CVRINSP over a period of only 8 days with a probability of 100% when CVRINSP was greater than 0.44 (Figure 1, right panel), but not by the average Rinsp.
There are several reasons for CVRINSP to be highly accurate for both diagnosis and prediction of acute deterioration of airway function in asthma. First, Rinsp is the most sensitive functional parameter of airway caliber (11–15) and is unaffected by lung volume history (3). Second, our technology allows accurate measurements of lung function over mid-tidal inspiration, thus avoiding the artifacts of expiratory flow limitation or glottis closure on resistance. Third, unlike the recommended analysis of PEF (1), the variability of Rinsp in the present study was estimated from the CV. The advantages of this approach stem from the concept that fluctuations in biological signals often follow power-law distributions, thus carrying more useful information than mean values (10, 16–20). For clinical practice, it is remarkable that a time window of only 4 days (Figure 1, left panel) was highly sensitive and specific to distinguish subjects with asthma from normal subjects. Nevertheless, future studies should address the role of average Rinsp in addition to CVRINSP for diagnostic and prognostic purposes.
Even though the number of subjects enrolled was low, the results are encouraging and might open new horizons in the field. Spirometry, or indeed any other lung function tests, cannot capture the fundamental characteristic of the disease: namely, the changes in lung function over time. Home monitoring of lung function by FOT does so in only a few days and can be easily and noninvasively performed by the patient. In addition, the analysis of the fluctuations of Rinsp can be used to form powerful risk predictors of acute deterioration of airway function and, possibly, asthma exacerbations. Even though this study was limited to voluntary adults, it can be envisaged that this technology may be particularly suitable in pediatrics and occupational medicine, and for prediction of asthma control when treatment regimens are modified.
Acknowledgments
The authors are grateful to the Fondazione Giovanni e Annamaria Cottino for financial support and to Dr. Roberto Torchio for technical assistance.
Footnotes
Author Contributions: C.G. participated in the design of the study, data collection and management, and preparation of the manuscript; A.G. participated in the design of the study, data management, statistical analysis, and preparation of the manuscript; B.S. participated in the statistical analysis and preparation of the manuscript; A.P. participated in the design of the study, statistical analysis, and preparation of the manuscript; V.B. participated in the design of the study and preparation of the manuscript; R.P. participated in the design of the study and preparation of the manuscript; R.L.D. participated in the design of the study, data analysis, and preparation of the manuscript.
Supported by Ministero Italiano della Salute per la Ricerca Finalizzata, Istituto Italiano di Tecnologie del Politecnico di Milano, Fondazione Giovanni e Annamaria Cottino, and National Institutes of Health grant HL-098976.
References
- 1.World Health Organization/National Heart, Lung, and Blood Institute (US). Global initiative for asthma: global strategy for asthma management and prevention. NIH Publication No. 02.3659. 2007 Jan 1995 (updated 2007; accessed May 14, 2011). Available from: http://www.ginasthma.com
- 2.Quanjer PH, Lebowitz MD, Gregg I, Miller MR, Pedersen OF. Peak expiratory flow: conclusions and recommendations of a Working Party of the European respiratory Society. Eur Respir J 1997;10:2s–8s. [PubMed] [Google Scholar]
- 3.Pellegrino R, Sterk P, Sont JK, Brusasco V. Assessing the effect of deep inhalation on airway calibre: a novel approach to lung function in bronchial asthma and COPD. Eur Respir J 1998;12:1219–1227. [DOI] [PubMed] [Google Scholar]
- 4.Lewis SA, Weiss ST, Britton JR. Airway responsiveness and peak flow variability in the diagnosis of asthma for epidemiological studies. Eur Respir J 2001;8:921–927. [DOI] [PubMed] [Google Scholar]
- 5.Powel H, Gibson PG. Options for self-management education for adults with asthma. Cochrane Database Syst Rev 2002;CD004107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bacharier LB, Strunk RC, Mauger D, White D, Lemanske RF, Sorkness CA. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med 2004;170:426–432. [DOI] [PubMed] [Google Scholar]
- 7.Galant SP, Morphew T, Amaro S, Liao O. Current asthma guidelines may not identify young children who have experienced significant morbidity. Pediatrics 2006;117:1038–1045. [DOI] [PubMed] [Google Scholar]
- 8.Atherton HA, White PT, Hewett G, Howells K. Relationship of daytime asthma symptom frequency to morning peak expiratory flow. Eur Respir J 1996;9:232–236. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Yu C, Holgate ST, Reiss TF. Variability and lack of predictive ability of asthma end-points in clinical trials. Eur Respir J 2002;20:1102–1109. [DOI] [PubMed] [Google Scholar]
- 10.Thamrin C, Stern G. New methods: what do they tell us? Fluctuation analysis of lung function. Eur Respir Mon 2010;47:310–324. [Google Scholar]
- 11.Dellacà R, Gobbi A, Pastena M, Pedotti A, Celli B. Home monitoring of within-breath respiratory mechanics by a simple and automatic forced oscillation technique device. Physiol Meas 2010; 31:N11–N24. [DOI] [PubMed] [Google Scholar]
- 12.Dellacà RL, Pompilio PP, Walker PP, Duffy N, Pedotti A, Calverley PM. Effects of bronchodilatation on expiratory flow limitation and resting lung mechanics in COPD. Eur Respir J 2009;33:329–337. [DOI] [PubMed] [Google Scholar]
- 13.Dellacà RL, Santus P, Aliverti A, Stevenson N, Centanni S, Macklem PT, Pedotti A, Calverley PM. Detection of expiratory flow limitation in COPD using the forced oscillation technique. Eur Respir J 2004;23:232–240. [DOI] [PubMed] [Google Scholar]
- 14.Pasker HG, Schepers R, Clément J, Van de Woestijne KP. Total respiratory impedance measured by means of the forced oscillation technique in subjects with and without respiratory complaints. Eur Respir J 1996;9:131–139. [DOI] [PubMed] [Google Scholar]
- 15.Smith HJ, Reinhold P, Goldman MD. Forced oscillation technique and impulse oscillometry. Eur Respir Mon 2005;31:72–105. [Google Scholar]
- 16.Que CL, Kenyon CM, Olivenstein R, Macklem PT, Maksym GN. Homeokinesis and short-term variability of human airway caliber. J Appl Physiol 2001;91:1131–1141. [DOI] [PubMed] [Google Scholar]
- 17.Frey U, Suki B. Complexity of chronic asthma and chronic obstructive pulmonary disease: implications for risk assessment, and disease progression and control. Lancet 2008;372:1088–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suki B. Fluctuation and power laws in pulmonary physiology. Am J Respir Crit Care Med 2002;166:133–137. [DOI] [PubMed] [Google Scholar]
- 19.Frey U, Brodbeck T, Majumdar A, Taylor DR, Town GI, Silverman M, Suki B. Risk of severe asthma episodes predicted from fluctuation analysis of airway function. Nature 2005;438:667–670. [DOI] [PubMed] [Google Scholar]
- 20.Thamrin C, Stern G, Strippoli M-PF, Kuehni CE, Suki B, Taylor DR, Frey U. Fluctuation analysis of lung function as a predictor of long-term response to β2-agonists. Eur Respir J 2009;33:486–493. [DOI] [PubMed] [Google Scholar]