Abstract
Background:
Iliopsoas (IP) muscle atrophy is a known consequence of open IP tenotomy, but the severity of IP muscle atrophy that occurs after arthroscopic labral-level IP tenotomies has not been documented.
Purpose:
To document the severity of muscle atrophy that occurs in the iliacus, psoas, and adjacent hip musculature after arthroscopic labral-level IP tenotomy.
Study Design:
Case series; Level of evidence, 4.
Methods:
Twenty-eight patients who had magnetic resonance arthrograms (MRAs) obtained prior to and 3 months to 5 years after arthroscopic labral-level IP tenotomies are the basis of this report. The pre- and postoperative MRAs of each patient were examined in consensus by 2 musculoskeletal radiologists who graded the postoperative muscle atrophy from 0 (no fatty infiltration) to 4 (>75% fatty infiltration) and noted any compensatory muscle hypertrophy or abnormal IP tendon morphology. Patients also were assessed with the Byrd 100-point modified Harris Hip Scoring system (MHHS) preoperatively and at the time of their postoperative MRA.
Results:
Postoperative MRAs were obtained on average 1.7 years (range, 3 months to 5 years) after hip arthroscopy. None of the patients had muscle atrophy on their preoperative MRAs. In contrast, 89% of patients had iliacus and psoas muscle atrophy on their postoperative MRAs, but only 2 (7%) developed grade 4 atrophy, and the majority (64%) had either grade 1 (n = 15) or no atrophy (n = 3). In addition, there were no significant differences in the MHHS of the patients with mild (grades 0-1), moderate (grades 2-3), or severe (grade 4) postoperative atrophy. Postoperative MRAs also demonstrated low-grade atrophy (grades 1-2) in the quadratus femoris (n = 5) and rectus femoris (n = 1) muscles, and 16 patients (57%) had distortion of the tendon, but none had a gap in their tendon.
Conclusion:
A majority of patients (89%) developed IP muscle atrophy after arthroscopic labral-level IP tenotomies, and although this percentage was similar (89% vs 90%) to that reported with lesser trochanteric IP tenotomies, the patients did not (1) develop atrophy of the gluteus maximus and vastus lateralis muscles, (2) have chronic IP tendon disruption, or (3) develop the severity of IP atrophy (55% grade 4 vs 7% grade 4) that has been reported after arthroscopic lesser trochanteric IP tenotomies.
Keywords: hip arthroscopy, iliopsoas tenotomy, muscle atrophy
Iliopsoas (IP) tenotomy is often performed for the treatment of painful snapping and impingement of the tendon.3,8,9,11–13,17,18,20,22 In the past, open tenotomies and fractional lengthenings were performed to treat these problems.1,10,14,16,21 With the advent of hip arthroscopy, arthroscopic labral-level and lesser trochanteric tenotomies have replaced open procedures and currently are the operative treatment of choice for painful snapping and impingement of the tendon.3,8,9,11–13,17,18,20,22 Although IP muscle atrophy is a known consequence of open IP tenotomies,1,10,14,16,21 to date, only 2 studies have described the occurrence of this phenomenon after arthroscopic IP tenotomies: one after arthroscopic lesser trochanteric tenotomies15 and the other describing volumetric changes in the IP muscle-tendon unit (MTU) after labral-level tenotomies.7 To our knowledge, there are no studies that have documented the severity of the postoperative muscle atrophy that occurs in the individual muscles (eg, iliacus, psoas) and adjacent hip musculature (eg, quadratus femoris, vastus lateralis) after arthroscopic labral-level IP tenotomy. Thus, the goal of this study was to document the severity of muscle atrophy that occurs in the iliacus, psoas, and adjacent hip musculature after arthroscopic labral-level IP tenotomy. Our hypothesis was that arthroscopic labral-level tenotomies would result in less severe atrophy of the iliacus, psoas, and adjacent hip musculature than that reported for arthroscopic lesser trochanteric IP tenotomies.
Methods
The study was performed in compliance with HIPAA (Health Insurance Portability and Accountability Act) regulations, with approval from the institutional review board, and with a waiver of informed consent. From a review of the senior author’s (J.S.K.) database of 1285 hip arthroscopies performed between August 2004 and July 2015, we identified 125 patients who had a labral-level arthroscopic IP tenotomy performed for the treatment of painful snapping or impingement of their tendon. The medical records of these 125 patients and the Department of Radiology’s PACS (picture archiving and communication system) were reviewed to identify patients who had both pre- and postoperative magnetic resonance arthrograms (MRAs) of their hip performed. From this review, we identified 28 patients who had MRAs obtained 3 months to 5 years after their labral-level arthroscopic IP tenotomy. In all patients, the second hip MRA was performed for the evaluation of “hip pain” and specific diagnoses, which included recurrent IP tendon tears (n = 2 patients who acutely lost their postoperative hip flexor power), gluteal tendon tear (n = 1), lateral femoral cutaneous nerve injury (n = 1), and fatigue fracture with hip pain and weakness after a fall (n = 1). These 28 patients are the basis of this study. Thus, the inclusion criteria for this study were (1) arthroscopic labral-level IP tenotomy performed by the senior author for the treatment of painful snapping or impingement of the tendon and (2) a pre- and postoperative hip MRA performed at our institution and available for review.
Surgical Technique
All 28 patients included in this study had their arthroscopic labral-level IP tenotomy performed by the senior author, and the same surgical technique was utilized in all cases. All the hip arthroscopies were performed with the patient in the supine position using a minimum of 3 portals (anterior, anterolateral, and posterolateral) as described by Byrd.8 Thus, the central and peripheral compartments were evaluated, labral tears were excised or repaired, and osteoplasties were performed to treat bony impingement as indicated. The arthroscopic procedures performed in these patients are summarized in Table 1.
TABLE 1.
Arthroscopic Procedures Performed
| Procedurea | No. of Patients |
|---|---|
| Labral-level iliopsoas tenotomy | 28 |
| Debridement of labral tear | 22 |
| Repair of labral tear | 5 |
| Osteoplasty for FAI | 18 |
| Loose body removal | 5 |
| Torn ligamentum teres excision | 3 |
| Microfracture | 2 |
| Partial synovectomy | 1 |
| Total | 84 |
aPatients often had more than 1 arthroscopic procedure performed. FAI, femoroacetablur impingement.
All 28 patients had an arthroscopic labral-level release of the IP tendon performed to treat painful snapping or impingement of the tendon. The details of the arthroscopic labral-level tendon release technique utilized in this study have been previously described.20 In brief, after arthroscopic treatment of concomitant central compartment pathology was completed, an anterior capsulotomy was made with a radiofrequency ablation device directly under the IP tendon. The tendon was then freed from any capsular adhesions and released with a combination of the radiofrequency ablation device and a beaver blade (Figure 1). Care was taken to only cut the tendinous portion of the IP MTU, thus leaving the muscle fibers intact. In all cases, the tendon release was verified by identifying both edges and ends of the tendon via the anterior capsulotomy (Figure 1B).
Figure 1.
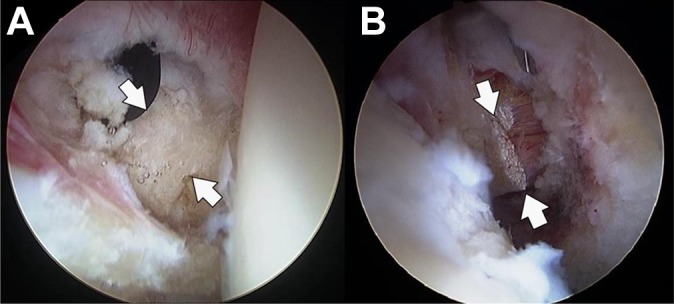
Arthroscopic views of the right hip showing the exposure and release of the iliopsoas tendon at the level of the labrum. (A) Prior to the release, an anterior capsulotomy was performed to expose and define (arrows indicate the edges of the tendon) the borders of the tendon. (B) The tendon was then released with a combination of the radiofrequency device and a beaver blade. Care was taken to only release the tendinous portion of the iliopsoas muscle-tendon unit, which, based on a prior study, leaves 60% of the muscle-tendon unit (the muscular portion) intact.2,6
Rehabilitation Protocol
All patients were enrolled in the same 3-phase rehabilitation program. The goals of phase 1 (surgery to week 4) were pain control, hip protection, and initial range of motion and leg control exercises. Phase 2 (postoperative weeks 4-10) focused on gait, functional movements, and performing a single-leg stance for longer than 15 seconds. Goals for phase 3 included returning to sport- and work-related activities with good leg control and no pain and improving hip flexor strength, with a goal of achieving hip flexor strength equal to 90% of the contralateral side.
Imaging
All MRAs were performed at our institution by 1 of our 8 musculoskeletal radiologists. The details of the protocol for the MRAs of the hip are provided in the Appendix. In summary, imaging included coronal T1-weighted, coronal T2-weighted, sagittal T1-weighted, oblique axial T1-weighted, axial T2-weighted with fat suppression, and axial T1-weighted images. MRA was performed after intra-articular administration of approximately 12 mL of a solution consisting of 5 mL nonionic iodinated contrast, 5 mL sterile saline, 5 mL of 0.5% ropivacaine, 5 mL 1% preservative-free lidocaine, and 0.1 mL of gadolinium contrast. Injection of the intra-articular contrast was performed via an anterolateral approach utilizing fluoroscopic guidance.
Each pre- and postoperative MRA was evaluated in consensus by 2 faculty musculoskeletal radiologists with 15 and 16 years of experience in interpreting musculoskeletal magnetic resonance examinations. Thus, a finding was considered positive if both readers agreed on its presence, and the grade of atrophy assigned was based on the consensus agreement of the radiologists regarding the percentage of fatty infiltration present. The musculoskeletal radiologists were blinded as to the clinical results (postoperative modified Harris Hip Scores [MHHS]) but not patient identifiers, as the pre- and postoperative magnetic resonance examinations had to be compared in the same patient. The reviewers compared the pre- and postoperative MRAs to determine whether the postoperative study revealed (1) muscle edema with new intramuscular high T2 signal intensity, (2) muscle atrophy (graded 0-4), (3) compensatory muscle hypertrophy, (4) abnormal signal within the IP tendon (increased signal on T1 or T2 sequences), or (5) abnormal IP tendon morphology. These parameters were selected and analyzed because they had been the data points in a prior study that assessed muscle atrophy after arthroscopic lesser trochanteric IP tenotomies.15 We used a previously described magnetic resonance grading scale19 for assessing the muscle atrophy observed on each patient’s MRA. With this scale, findings are graded from 0 to 4: grade 0 = no fat, grade 1 = muscles containing some fatty streaks, grade 2 = fatty infiltration with more muscle tissue than fat, grade 3 = fatty infiltration with equal amounts of fat and muscle, and grade 4 = fatty infiltration with more fat than muscle.15,19 This scale was also used in the prior clinical study that assessed the magnetic resonance appearance of the hip muscles after lesser trochanteric IP tenotomies.15
The IP tendon was considered distorted if it was thickened or irregular in contour, and it was considered disrupted if a gap was seen between the tendon and the lesser trochanter. A tendon could be both disrupted and distorted if a gap was seen distally but the tendon was distorted above the gap.
Clinical Evaluation
All 28 hips included in this study were examined by the senior author and assessed with Byrd’s 100-point MHHS prior to arthroscopy and at the time of their postoperative MRA. Hip flexor strength also was assessed by the senior author via manual muscle testing at the clinic visit just prior to each patient’s postoperative MRA. At these visits, maximum active hip flexion strength was determined for both hips in the following manner. The patient was seated at the end of the examining table with his or her arms crossed over the chest. Each patient was then instructed to forcibly flex his or her hip against the manual resistance applied by the senior author, and hip flexor strength was rated from 0 to 5 (using the standard manual muscle testing scale) based on the maximum resistance generated by the patient prior to release of muscle resistance. Isolated testing of IP muscle strength was not performed. Operative notes, operative hip sheets (drawings), intraoperative photos, and pre- and postoperative clinical notes were available for review for all 28 patients.
Statistical Analysis
Results were expressed by descriptive methods (eg, mean, range), and the Student t test was used to compare paired samples (eg, patient age, sex). A chi-square test was used to compare grades of atrophy with level of tenotomy, and a 1-way analysis of variance was used to assess the effect of the different grades of atrophy on the clinical outcomes. P ≤ .05 was considered statistically significant. Generalized estimating equation models were used to compare the iliacus atrophy grade, psoas atrophy grade, and IP distortion. The statistical power of the study was limited by the number of patients who met the inclusion criteria and by the number of patients who developed grade 4 atrophy postoperatively. There were too few patients with grade 4 atrophy to draw any valid conclusions regarding correlations between the atrophy observed and the hip flexor strength or the MHHS of patients who were measured just prior to their postoperative MRA.
Results
The study population consisted of 3 men and 25 women with a mean age of 31.5 years (range, 15-56 years). Average length of time from IP release to the postoperative MRA was 1.7 years (range, 3 months to 5 years). As noted previously, the study population included only those patients who had a labral-level IP tenotomy performed by the senior author and both pre- and postoperative MRAs performed at our institution. This resulted in a study group with a wide range in age (15-56 years) and in the interval between the pre- and postoperative MRA (3 months to 5 years). In addition, since the postoperative MRAs were not obtained at standard intervals, the length of time from tenotomy to the development of postoperative atrophy could not be determined.
In all patients, the second hip MRA was performed for the evaluation of “hip pain” and to assess the hip for the specific diagnoses of recurrent IP tendon tears (n = 2 patients who acutely lost their postoperative hip flexor power), a gluteal tendon tear (n = 1), a lateral femoral cutaneous nerve injury (n = 1), and suspected fatigue fracture with hip pain and weakness after a fall (n = 1). The diagnoses from the second MRA included new degenerative cartilage loss in 18 (64%) patients, recurrent labral tears in 11 (39%) patients, persistent cam and/or pincer deformities in 9 (32%) patients, intra-articular bodies in 4 (14%) patients, peritrochanteric bursitis in 3 (11%) patients, and ligamentum teres tears in 2 (7%) patients.
MRA Findings
None of the patients had hip muscle atrophy evident on their preoperative MRAs. Twenty-five of 28 patients (89%) developed muscle atrophy after their arthroscopic labral-level IP tenotomy. Atrophy was most commonly observed in the psoas (89%) and quadratus femoris (18%) muscles but was also seen in the iliacus (8%) and rectus femoris (4%) muscles (Table 2).
TABLE 2.
Percentage of Labral-Level Tenotomy Patients Who Had Hip Muscle Atrophy Seen on Posttenotomy Magnetic Resonance Arthrography
| Muscle | Patients, n (%) | Grade of Atrophya |
|---|---|---|
| Iliacus | 8 (8) | 2 (1.3) |
| Psoas | 25 (89) | 4 (1.5) |
| Quadratus femoris | 5 (18) | 2 (1.2) |
| Rectus femoris | 1 (4) | 2 (2.0) |
| Tensor fascia lata | 0 | 0 |
| Vastus lateralis | 0 | 0 |
| Vastus medialis | 0 | 0 |
| Gluteus maximus | 0 | 0 |
aData presented as highest grade (mean) of muscle atrophy seen on postoperative magnetic resonance images.
The psoas was the only muscle that developed grade 4 atrophy. The highest grade of atrophy seen in the iliacus and the quadratus and rectus femoris muscles was grade 2. There was no atrophy of the tensor fascia lata, vastus medialis, vastus lateralis, or gluteus maximus muscles observed on the postoperative MRAs of these patients (Figure 2).
Figure 2.
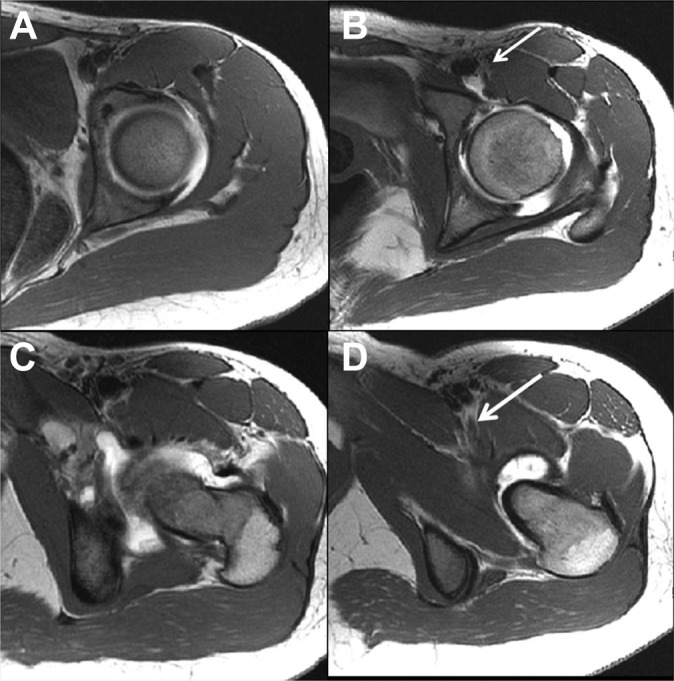
Pre- and postoperative axial T1-weighted hip magnetic resonance arthrography (MRA) images of a 16-year-old female with left hip pain. (A and C) Preoperative images demonstrated no muscle atrophy. (B and D) Postoperative images demonstrated grade 4 atrophy of the psoas muscle above the level of the acetabular rim (arrow, B) and grade 1 atrophy below the level of the acetabular rim (arrow, D). The postoperative MRA was performed 13 months after the patient’s labral-level iliopsoas tenotomy, and her modified Harris Hip Score at that time was 82.5 points.
Although posttenotomy muscle atrophy was observed in 25 (89%) of 28 patients, only 2 (7%) patients developed grade 4 atrophy, and the majority of patients (64%) only had grade 1 (n = 15) or no atrophy (n = 3) (Table 3). The percentage of patients with low-grade (0-1) atrophy was significantly higher than the percentage of patients with high-grade (grade 3-4) atrophy (P < .012). None of the patients had MRA evidence of posttenotomy compensatory hypertrophy in any of the adjacent hip musculature (eg, gluteus maximus, quadratus or rectus femoris, tensor fascia lata, vastus lateralis) (Figure 3).
TABLE 3.
Number of Labral-Level Tenotomy Patients With Each Grade of Atrophya
| Grade of Atrophy | P Valueb | |||||||
|---|---|---|---|---|---|---|---|---|
| Site of Release | Patients | 4 | 3 | 2 | 1 | 0 | χ2 | Fisher |
| Labral level | No. | 2 | 2 | 6 | 15 | 3 | <.012 | <.013 |
aThe number of patients with low-grade (grade 0-1) atrophy was significantly higher than the number of patients with high-grade (grade 3-4) atrophy (P < .012).
bComparison of the total number of patients with low grade (grade 0-1) atrophy (n = 18) with the total number of patients with high grade (grade 3-4) atrophy (n = 4).
Figure 3.

Pre- and postoperative axial T1-weighted magnetic resonance arthrography (MRA) images of a 33-year-old woman with posttenotomy left hip pain. (A and C) Preoperative images show no muscle atrophy, while (B and D) postoperative images demonstrate grade 2 atrophy of the iliopsoas muscle at the acetabular rim (arrow, B) and grade 1 atrophy of the quadratus femoris muscle (arrow, D). The postoperative MRA was performed 12 months after the patient’s labral-level iliopsoas tenotomy, and her modified Harris Hip Score at that time was 67 points.
MRA Iliopsoas Tendon Findings
Postoperative abnormalities within the IP tendon were frequently observed, including abnormal intratendinous T1 and T2 signal and distortion of the tendon. Twelve (43%) patients had increased T1 signal within the residual portion of the IP tendon, and 4 (14%) had increased T2 signal.
Sixteen (57%) patients had evidence of distortion of their IP tendon when the pre- and posttenotomy MRAs were compared. Twelve (43%) of the labral-level patients had no posttenotomy distortion, and none of the tendons in these patients had intratendinous T1 or T2 signal. None of the 28 labral-level patients had disruption (a gap) in the IP tendon observed on their posttenotomy MRAs.
Correlation of MRA Findings and Hip Function
As noted above, all 28 hips included in this study were assessed with the Byrd 100-point MHHS prior to their arthroscopic, labral-level tenotomy and at the time of their postoperative MRA. The fact that there was no edema within the iliacus or psoas muscles even when the posttenotomy MRA was performed only 6 months after the tenotomy suggests that the MRA changes observed in the muscles were established and not part of an acute, ongoing process.
To assess the effect of the severity of atrophy on clinical outcomes, patients were grouped based on the highest grade of atrophy observed in either their iliacus or psoas muscles, and the MHHS scores of each group were compared. The results of these comparisons and the demographic data (eg, age and length of time to the second MRA) for each patient are summarized in Table 4.
TABLE 4.
Comparison of Individual Patients’ Grade of Postoperative Atrophy and Their MHHS and Hip Flexor Strength at the Time of Their Second MRAa
| ID | Age, y | Sex | Grade of Atrophyb | Preop MHHS | Time to MRA 2, mo | Hip Score at MRA 2 | Strength at MRA 2c |
|---|---|---|---|---|---|---|---|
| 19 | 16 | F | 4 | 38.5 | 10 | 82.5 | 5 |
| 23 | 17 | F | 4 | 45.1 | 41 | 81.4 | 5 |
| Mean | 16.5 | 41.8 | 81.95 | ||||
| 17 | 25 | F | 3 | 46.2 | 8 | 45.1 | 4 |
| 22 | 39 | F | 3 | 39.6 | 11 | 81.4 | 4 |
| 10 | 20 | F | 2 | 72.6 | 39 | 84.7 | 5 |
| 20 | 42 | F | 2 | 41.8 | 5 | 59.4 | 4 |
| 26 | 29 | F | 2 | 59.4 | 10 | 68.2 | 5 |
| 27 | 31 | F | 2 | 50.6 | 24 | 79.2 | 5 |
| 30 | 33 | F | 2 | 45.1 | 11 | 56.1 | 5 |
| 32 | 26 | F | 2 | 41.8 | 20 | 67.1 | 4 |
| Mean | 30.6 | 49.6 | 67.6 | ||||
| 3 | 20 | F | 1 | 38.5 | 3 | 81.4 | 5 |
| 6 | 35 | F | 1 | 39.6 | 32 | 47.3 | 4 |
| 9 | 15 | F | 1 | 45.1 | 41 | 84.7 | 5 |
| 12 | 50 | F | 1 | 33.0 | 31 | 72.6 | 4 |
| 13 | 39 | F | 1 | 45.1 | 11 | 81.4 | 5 |
| 14 | 21 | M | 1 | 57.2 | 36 | 81.4 | 5 |
| 15 | 24 | M | 1 | 42.9 | 12 | 42.9 | 4 |
| 18 | 44 | F | 1 | 53.9 | 10 | 35.2 | 4 |
| 21 | 30 | F | 1 | 41.8 | 6 | 49.5 | 3 |
| 24 | 18 | F | 1 | 59.4 | 23 | 91.3 | 5 |
| 25 | 56 | F | 1 | 38.5 | 5 | 56.5 | 3 |
| 29 | 49 | F | 1 | 39.6 | 3 | 46.2 | 4 |
| 31 | 32 | F | 1 | 29.7 | 19 | 33 | 3 |
| 33 | 38 | F | 1 | 23.1 | 6 | 53.9 | 4 |
| 34 | 31 | F | 1 | 44 | 5 | 73.7 | 5 |
| 5 | 35 | M | 0 | 57.2 | 15 | 69.3 | 5 |
| 7 | 41 | F | 0 | 38.5 | 24 | 90.2 | 5 |
| 11 | 26 | F | 0 | 41.8 | 3 | 63.9 | 4 |
| Mean | 33.6 | 42.7 | 64.1 |
aThere was no significant difference in the average scores of the 18 patients with mild (grades 0-1) and the 8 patients with moderate (grades 2-3) postoperative iliopsoas atrophy (P = .64). Hip flexor strength testing at the time of the second MRA indicated that there was no correlation with a patient’s hip flexor strength and the grade of muscle atrophy observed on their postoperative MRA. F, female; M, male; MHHS, modified Harris Hip Score; MRA, magnetic resonance arthrography.
bHighest grade of atrophy observed in the iliacus and/or psoas muscles.
cMaximum active hip flexion strength was determined for both hips with patient seated at the end of the examining table. Each patient was then instructed to forcibly flex his or her hip against the manual muscle resistance applied by the examiner (senior author), who rated the strength from 0-5 based on the manual muscle testing scale.
Only 2 patients had grade 4 atrophy, and their MHHS at the time of their second MRA averaged 82 points (range, 81.4-82.5). Two patients had grade 3 and 6 patients had grade 2 atrophy, and their MHHS averaged 67.7 points and ranged from 45 to 85 points. Fifteen patients had grade 1 and 3 patients had no atrophy observed on their second MRA, and their MHHS averaged 64.1 points and ranged from 33 to 91 points. There was no significant difference in mean scores of the 18 patients with mild (grades 0-1) and the 8 patients with moderate (grades 2-3) postoperative IP atrophy (P = .64). The scores of the 2 patients with grade 4 atrophy were 14 points higher than the mean scores of the patients with mild or moderate atrophy, but there were too few patients with grade 4 atrophy to draw any valid conclusions regarding their scores and the amount of atrophy observed.
Similarly, the results of the hip flexor strength testing prior to the postoperative MRA also did not predict the grade of IP muscle atrophy observed on the postoperative MRAs. Both patients with grade 4 atrophy had 5+ hip flexor strength, and the patients with 4− to 4+ hip flexor power were spread equally between the 18 patients with mild (grade 0-1) and the 8 patients with moderate (grade 2-3) atrophy. The 3 patients with the most (grade 3) hip flexor weakness were all in the grade 1 atrophy group. However, there were too few patients with grade 4 atrophy to draw any valid conclusions regarding their hip flexor strength and the amount of atrophy observed.
Discussion
Currently, arthroscopic labral-level and lesser trochanteric IP tenotomies are the operative treatment of choice for painful snapping and impingement of the tendon.3,8,9,11–13,17,18,20,22 Although IP muscle atrophy is a known consequence of open IP tenotomies,1,10,14,16,21 to date, only 2 studies have described the occurrence of this phenomenon after arthroscopic tenotomies: one after arthroscopic lesser trochanteric IP tenotomies15 and the other that analyzed volumetric changes in the IP muscle after labral-level tenotomies.7 However, to our knowledge, there are no studies that have documented the severity (grade) of the postoperative muscle atrophy that occurs in the individual muscles (eg, iliacus, psoas) and adjacent hip musculature after arthroscopic labral-level IP tenotomies. Thus, the goal of this study was to document the severity of postoperative hip muscle atrophy that occurs after arthroscopic labral-level IP tenotomies.
The results of this study indicate that most patients (89%) develop iliacus and psoas muscle atrophy after arthroscopic labral-level IP tenotomies and that the percentage of patients who experience this outcome is similar (89% vs 90%) to that which has been reported with lesser trochanteric IP tenotomies15 (Table 5).
TABLE 5.
Comparison of the Percentage of Labral-Level Tenotomy Patients (Current Study) and Lesser Trochanteric Tenotomy Patients15 Who Had Hip Muscle Atrophy Seen on Posttenotomy Magnetic Resonance Arthrography
| Muscle | LL Patients (%) | Grade of Atrophya | LT Patients (%)15 | Grade of Atrophya | P Value, χ2 |
|---|---|---|---|---|---|
| Iliacus | 8 | 2 (1.3) | 65 | 4 (1.9) | .001 |
| Psoas | 89 | 4 (1.5) | 85 | 4 (2.9) | >.05 |
| Quadratus femoris | 18 | 2 (1.2) | 10 | 3 (1.8) | |
| Rectus femoris | 4 | 2 (2.0) | 5 | 3 (2.5) | |
| Tensor fascia lata | 0 | 0 | 0 | 0 | |
| Vastus lateralis | 0 | 0 | 5 | 2 (1.5) | |
| Vastus medialis | 0 | 0 | 0 | 0 | |
| Gluteus maximus | 0 | 0 | 25 | 2 (1.3) | .001 |
aData presented as highest grade and (average grade) of muscle atrophy seen on postoperative magnetic resonance arthrography images. LL, labral level; LT, lesser trochanter.
However, although the percentage of lesser trochanteric patients with posttenotomy psoas atrophy was similar to that of the labral-level patients in the current study (85% vs 89%), the percentage of patients with iliacus atrophy (Table 5) was significantly higher (65% vs 8%) in the lesser trochanteric group (P < .001), and the severity of atrophy (percentage of patients with grade 4 atrophy) was much greater (55% vs 7%) in the lesser trochanteric patients (Table 6).
TABLE 6.
Comparison of the Number of Patients With Each Grade of Atrophy for Labral-Level Tenotomy Patients (Current Study) and for Lesser Trochanteric Tenotomy Patients15 a
| Grade of Atrophy | P Valueb | |||||||
|---|---|---|---|---|---|---|---|---|
| Site of Release | Patients | 4 | 3 | 2 | 1 | 0 | χ2 | Fisher |
| Labral-Level | No. | 2 | 2 | 6 | 15 | 3 | <.012 | <.013 |
| Lesser-Trochanter15 | No. | 11 | 2 | 4 | 1 | 2 | ||
aThe incidence of atrophy was similar (∼90%) in both groups, but there was a significant difference in the severity of atrophy which was significantly greater in the lesser trochanteric tenotomy patients as 11 (55%) of the lesser trochanteric tenotomy patients had grade 4 atrophy compared with 2 (7%) in the labral-level tenotomy group, and only 3 (15%) of the lesser trochanteric tenotomy patients had low (0-1) grade compared with 18 (64%) of the labral-level tenotomy patients.
bComparisons of the total number of labral-level patients (n = 2) with the total number of lesser trochanteric patients with grade 4 atrophy (n = 11) and the total number of labral-level patients (n = 18) with the total number of lesser trochanteric patients with grade 0-1 atrophy (n = 3).
Specifically, in the study by Hain et al,15 11 (55%) of the lesser trochanteric patients developed grade 4 atrophy of their iliacus and/or psoas muscles after tenotomy at the lesser trochanter, whereas only 2 (7%) of the labral-level patients in the current study developed grade 4 atrophy. This difference was statistically significant (P < .013). Similarly, the percentage of labral-level patients with low-grade (0-1) atrophy was significantly higher (64%) than that reported in lesser trochanteric patients (7%; P < .012).
The results of a magnetic resonance imaging (MRI) study that assessed volumetric changes in the IP muscle of 18 patients who had labral-level IP tenotomies support the results of the current study.7 These authors reported that MRIs obtained at least 1 year postoperatively demonstrated that the IP muscle of the operated side was 25% (volumetrically) smaller than the control side. However, they analyzed the iliacus and psoas as a single MTU, and thus, they could not determine the relative atrophy of each muscle belly or of the adjacent hip musculature, as was done in the current study.
The difference in the severity of atrophy that occurs after labral-level and lesser trochanteric tenotomies may be explained in part by the results of Blomberg et al6 and Alpert et al.2 In the study by Alpert et al,2 the authors performed a cross-sectional analysis of the IP tendon at the level of the labrum and found that the tendon made up 47% of the MTU.2 In the study by Blomberg et al,6 the authors performed a cross-sectional analysis of the IP MTU at both the labral and lesser trochanteric levels of arthroscopic IP tenotomies.6 They found that at the labral level, the tendon makes up 40% of the MTU, and at the lesser trochanteric level, the tendon makes up 60% of the MTU. Thus, tenotomies at the labral level leave a significantly greater percentage (60% vs 40%) of the MTU (the muscular portion) intact.6 The authors theorized that the 20% increase in the amount of muscle that remains after a labral-level tenotomy may more effectively tether and limit the amount of tendon separation that occurs and that this phenomenon may contribute to the high rate of recurrent snapping (20%-60%) that has been reported for both arthroscopic11,20 and open labral-level IP tenotomies.1,10,14,16,21
The results of the current study also suggest that the additional 20% of the muscle that is left intact after labral-level tenotomies may more effectively transmit loads to the proximal muscle bellies of the iliacus and psoas muscles, and, thus, limit the amount of muscle atrophy that occurs. The results of Blomberg et al6 may also explain in part the finding that although 25% of the lesser trochanteric patients in the study by Hain et al15 developed gluteus maximus atrophy, none of the labral-level tenotomy patients in the current study did. This may have occurred because the smaller muscle mass left intact after lesser trochanteric tenotomies resulted in a greater loss of the normal opposition to hip extension generated by the iliacus and psoas muscles, and thus, the development of gluteus maximus atrophy.
In the current study, postoperative distortion of the tendon was observed in 57% of patients, but no distortion and no intratendinous signal was seen in 43% of patients. This suggests that the posttenotomy scarring closely followed the original course of the tendon and that those interpreting hip MRIs after arthroscopic IP tenotomies should be aware that the tendon may appear normal on MRAs obtained 6 or more months after the tenotomy.
The relatively normal appearance of the IP tendon on follow-up MRI after arthroscopic tenotomies also has been reported by Arabia et al.4 They evaluated the degree of regeneration that occurred in 19 patients after labral-level tenotomies and found that at a mean of 23 months (range, 6-44 months), regeneration occurred in all patients and that mean postoperative circumference of the tendon at the site of the tenotomy was 84% of its original circumference. The authors concluded that after an arthroscopic labral-level IP tenotomy, patients recover their flexion strength because they regenerate over 80% of the circumference of their original IP tendon. Their conclusion regarding the recovery of full hip flexor strength has been confirmed by the results of numerous studies that have assessed postoperative muscle strength after arthroscopic labral-level and lesser trochanteric IP tenotomies.3,4,9,13,17,18
None of the patients in the current study had evidence of a gap in their IP tendon on their postoperative MRA. In contrast, Hain et al15 reported that 35% of their patients with lesser trochanteric tenotomy had a discrete gap in their tendon 6 or more months after tenotomy. The finding that our labral-level tenotomy patients did not have persistent disruption of their IP tendon may be explained by the study of Bayer and Keene.5 They evaluated the amount of tendon separation that occurred after labral-level and lesser trochanteric arthroscopic IP tenotomies and found that the mean tendon separation after labral-level tenotomies (8.3 ± 2.04 mm) was significantly less (5 mm) than that which occurs after lesser trochanteric tenotomies (13.3 ± 3.01 mm; P < .001). They theorized that the smaller amount of tendon separation that occurs after labral-level tenotomies may explain the higher rates of recurrent snapping that has been reported with open and arthroscopic labral-level tenotomies.1,10,11,13,14,20,21
The smaller amount of tendon separation that occurs after labral-level tenotomies also may explain why none of the patients in the current study had chronic disruption of their IP tendon, In the study by Bayer and Keene,5 tendon separation after labral-level tenotomies never exceeded 12 mm. In contrast, 12 (30%) of their lesser trochanteric patients had tendon separation greater than 14 mm, and separation ranged as high as 22 mm. Perhaps the lesser trochanteric patients with persistent disruption reported in the study by Hain et al15 were those with greater than 14 mm of separation, and this amount of separation was beyond that which would result in spontaneous repair.
Clinical Outcomes
As noted previously, each patient studied was examined by the senior author and assessed using the Byrd MHHS system preoperatively and at the time of their postoperative MRA. The postoperative MHHS obtained at the time of the second MRA was not predictive of the severity (grade) of the atrophy that was observed on the MRAs. Patients with no atrophy, mild to moderate (grades 2-3) atrophy, and grade 4 atrophy had similar MHHS scores (see Table 4).
Similarly, the results of hip flexor strength testing also did not predict the posttenotomy grade of IP muscle atrophy that was observed on postoperative MRA. Both patients with grade 4 atrophy had 5+ hip flexor strength, and the patients with 4− to 4+ hip flexor power were spread equally between those with mild (grades 0-1) and moderate (grades 2-3) atrophy. The 3 patients with grade 3 hip flexor strength were all in the grade 1 atrophy group.
Strengths and Limitations
The strengths of this study are that it is a consecutive series of patients who had (1) arthroscopic labral-level tenotomies performed by 1 surgeon at 1 institution, (2) pre- and posttenotomy MRAs performed and interpreted by 2 musculoskeletal radiologists at the same institution, (3) pre- and posttenotomy clinical outcomes prospectively evaluated with the Byrd MHHS, and (4) imaging obtained up to 5 years (mean, 1.7 years) after arthroscopic labral-level and lesser trochanteric IP tenotomies documenting the development and persistence of muscle atrophy and distortion of the IP tendon. Based on the results of prior studies,4,11,12,20 the results of this study suggest that if a surgeon chooses a labral-level IP tenotomy over a lesser trochanteric tenotomy to treat painful impingement or snapping of the tendon, he or she can anticipate that there will be less postoperative muscle atrophy and no persistent gap in the tendon. However, the results of prior studies suggest that a “trade-off” for choosing a labral-level tenotomy over a lesser trochanteric tenotomy to treat painful snapping of the tendon is a significantly higher rate of recurrent snapping of the tendon (22% vs 1%) after labral-level IP tenotomies.3,4,9,11,12,20
The limitations of this study are (1) all the patients had repeat MRAs for the evaluation of recurrent hip pain, so we do not know whether our findings would apply to patients that are asymptomatic after IP tenotomy; (2) we could not determine the contribution of the IP tenotomy to the postoperative atrophy observed since there was no control group of patients who had hip arthroscopy performed without IP tenotomies; (3) we could not determine when the postoperative atrophy occurred; (4) the true incidence of atrophy could not be determined because this is not a consecutive series of symptomatic and asymptomatic patients; and (5) the statistical power of the study was limited by the number of patients who met the inclusion criteria and by the number of patients who developed grade 4 postoperative atrophy.
Conclusion
A majority of patients (89%) developed IP muscle atrophy after arthroscopic labral-level IP tenotomies, and although this percentage was similar (89% vs 90%) to that reported with lesser trochanteric IP tenotomies,15 the patients did not develop atrophy of the gluteus maximus and vastus lateralis muscles (25% in lesser trochanteric patients), have chronic IP tendon disruption (35% in lesser trochanteric patients), or develop the severity of IP atrophy (55% grade 4 vs 7% grade 4) that has been reported after arthroscopic lesser trochanteric IP tenotomies.15
Appendix
Protocol for the Magnetic Resonance Arthrograms (MRAs) of the Hips in This Study
The protocol for the MRAs of the hip for these studies included the following: coronal T1-weighted with fat suppression (repetition time [TR] 700 ms, echo time [TE] 8 ms, echo train length [ETL] = 2, matrix 288 × 224, field of view [FOV] = 18 cm, slice thickness = 4 mm with 0.4-mm interslice gap), coronal T2-weighted with fat suppression (TR 4600 ms, TE 80 ms, ETL = 19, matrix 320 × 224, FOV = 18 cm, slice thickness = 4 mm with 0.4-mm interslice gap), sagittal T1-weighted with fat suppression (TR 700 ms, TE 8 ms, ETL = 2, matrix 228 × 224, FOV = 18 cm, slice thickness = 4 mm with 0.4-mm interslice gap), oblique axial T1-weighted with fat suppression (TR 700 ms, TE 8 ms, ETL = 2, matrix 288 × 224, FOV = 18 cm, slice thickness = 4 mm with 0.4-mm interslice gap), axial T1-weighted (TR 650 ms, TE 18 ms, ETL = 2, matrix 228 × 224, FOV = 18 cm, slice thickness = 4 mm with 0.4-mm interslice gap), and axial T2-weighted with fat suppression (TR 4000 ms, TE 80 ms, ETL = 19, matrix 18 × 18, FOV = 18 cm, slice thickness = 4 mm with 0.4-mm interslice gap) performed after the intra-articular administration of approximately 12 mL of a solution consisting of 5 mL nonionic iodinated contrast, 5 mL sterile saline, 5 mL of 0.5% ropivacaine, 5 mL 1% preservative-free lidocaine, and 0.1 mL of gadolinium contrast. Injection of the intra-articular contrast was performed via an anterolateral approach utilizing fluoroscopic guidance.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: The research presented was supported under NIH awards UL1TR000427 and TL1TR000429.
Ethical approval for this study was obtained from the University of Wisconsin Madison Minimal Risk IRB (Health Sciences) (submission ID 2015-0122).
References
- 1. Allen WC, Cope R. Coxa saltans: the snapping hip revisited. J Am Acad Orthop Surg. 1995;3:303–308. [DOI] [PubMed] [Google Scholar]
- 2. Alpert JM, Kozanek M, Li G, Kelly BT, Asnis PD. Cross-sectional analysis of the iliopsoas tendon and its relationship to the acetabular labrum: an anatomic study. Am J Sports Med. 2009;37:1594–1598. [DOI] [PubMed] [Google Scholar]
- 3. Anderson S, Keene J. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36:2363–2371. [DOI] [PubMed] [Google Scholar]
- 4. Arabia WHM, Gómez-Hoyos J, Serna JFL, et al. Regrowth of the psoas tendon after arthroscopic tenotomy: a magnetic resonance imaging study. Arthroscopy. 2013;29:1308–1313. [DOI] [PubMed] [Google Scholar]
- 5. Bayer JL, Keene JS. Comparison of the amount of iliopsoas tendon lengthening that occurs after arthroscopic labral-level and lesser trochanteric tenotomies. http://www.sportsmed.org/apps/aossm_2013/scientific_posters.html. Accessed July 2013.
- 6. Blomberg JR, Zellner BS, Keene JS. Cross-sectional analysis of iliopsoas muscle-tendon units at the sites of arthroscopic tenotomies. Am J Sports Med. 2011;39(suppl):58S–63S. [DOI] [PubMed] [Google Scholar]
- 7. Brandenburg JB, Kapron AL, Wylie JD, et al. The functional and structural outcomes of arthroscopic iliopsoas release. Am J Sports Med. 2016;44:1286–1291. [DOI] [PubMed] [Google Scholar]
- 8. Byrd JWT. Evaluation and management of the snapping iliopsoas tendon. Tech Orthop. 2005;20:45–51. [PubMed] [Google Scholar]
- 9. Contreras ME, Dani WS, Endges WK, De Araujo LC, Berral FJ. Arthroscopic treatment of the snapping iliopsoas tendon through the central compartment of the hip: a pilot study. J Bone Joint Surg Br. 2010;92:777–780. [DOI] [PubMed] [Google Scholar]
- 10. Dobbs M, Gordon E, LuhMann S, Szymanski D, Schoenecker P. Surgical correction of the snapping iliopsoas tendon in adolescents. J Bone Joint Surg Am. 2002;84:420–424. [DOI] [PubMed] [Google Scholar]
- 11. Domb BG, Shindle MK, McArthur B, Voos JE, Magennis EM, Kelly BT. Iliopsoas impingement: a newly identified cause of labral pathology in the hip. HSS J. 2011;7:145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. El Bitar YF, Stake CE, Dunne KF, Botser IB, Domb BG. Arthroscopic iliopsoas fractional lengthening for internal snapping of the hip: clinical outcomes with a minimum 2-year follow-up. Am J Sports Med. 2014;42:1696–1703. [DOI] [PubMed] [Google Scholar]
- 13. Flanum ME, Keene JS, Blankenbaker DG, et al. Arthroscopic treatment of the painful “internal” snapping hip: results of a new endoscopic technique and imaging protocol. Am J Sports Med. 2007;35:770–779. [DOI] [PubMed] [Google Scholar]
- 14. Gruen GS, Scioscia TN, Lowenstein JE. The surgical treatment of internal snapping hip. Am J Sports Med. 2002;30:607–613. [DOI] [PubMed] [Google Scholar]
- 15. Hain KS, Blankenbaker DG, DeSmet AA, Keene JS, Munoz del Rio A. MR appearance and clinical significance of changes in the hip muscles and iliopsoas tendon after iliopsoas tenotomy. HSS J. 2013;9:236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hoskins JS, Burd TA, Allen WC. Surgical correction of internal coxa saltans: a 20-year consecutive study. Am J Sports Med. 2004;32:998–1001. [DOI] [PubMed] [Google Scholar]
- 17. Ilizaliturri VM, Jr, Chaidez C, Villegas P, Briseño A, Camacho-Galindo J. Prospective randomized study of 2 different techniques for endoscopic iliopsoas tendon release in the treatment of internal snapping hip syndrome. Arthroscopy. 2009;25:159–163. [DOI] [PubMed] [Google Scholar]
- 18. Ilizaliturri VM, Jr, Villalobos FE, Jr, Chaidez PA, Valero FS, Aguilera JM. Internal snapping hip syndrome: treatment by endoscopic release of the iliopsoas tendon. Arthroscopy. 2005;21:1375–1380. [DOI] [PubMed] [Google Scholar]
- 19. Khoury E, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscule: sonography versus MR. AJR Am J Roentgenol. 2008;190:1105–1111. [DOI] [PubMed] [Google Scholar]
- 20. Nelson IR, Keene JS. Results of labral-level iliopsoas tenotomies for treatment of labral impingement. Arthroscopy. 2014;30:688–694. [DOI] [PubMed] [Google Scholar]
- 21. Taylor GR, Clarke NM. Surgical release of the “snapping iliopsoas tendon.” J Bone Joint Surg Br. 1995;77:881–883. [PubMed] [Google Scholar]
- 22. Wettstein M, Jung J, Dienst M. Arthroscopic psoas tenotomy. Arthroscopy. 2006;22:907.e1–907.e4. [DOI] [PubMed] [Google Scholar]


