Abstract
Aim of the study
Inflammasome, a large complex of NOD-like receptors (NLRs), drives tumor growth and progression. The present study aimed at exploring the alteration in expression of urinary inflammasome-related microRNAs (miRNAs) in bladder cancer (BC). Our previous report demonstrated the up-regulation of NLRs genes (NLRP3, NLRP4, NLRP9 and NAIP) in urine sediments of patients harboring BC. The expression levels of miRNAs targeting these NLRs (miR-146a-5p, miR-106a-5p, miR-17-5p, miR-223-3p, miR-141-3p, miR-19a-3p, miR-145-5p, miR-185-5p) were assayed in the same patient cohort.
Materials and methods
Forty-six subjects affected by BC, 28 healthy controls (CTR0) and 31 subjects with histologically confirmed bladder inflammation (CTR1) were recruited. Total RNA was extracted from urine sediment and resulting cDNA was used for amplification by real-time polymerase chain reaction. MiRNA expression levels were evaluated and compared among selected groups. Patients were further stratified according to tumor stage, grade and risk of recurrence and progression. Moreover, non-muscle invasive low-grade and high-grade (HG) BC patients were compared.
Results
MiR 141-3p and miR-19a-3p expression decreased in CTR1 with respect to both BC and CTR0. In contrast, miR-146a-5p was up-regulated in BC compared with CTR0. MiR106a-5p, miR17-5p and miR19a-5p were significantly up-regulated in HG, high-risk (HR) and non-muscle invasive HG BC patients, while miR-185-5p was significantly higher in muscle invasive tumors, according to T stage stratification.
Conclusion
The increased expression of miRNAs targeting NLRs in HG and HR BC patients is in accordance with the decrease in NLR mRNAs observed in our previous report. These data corroborate the direct role of NLR genes and respective regulatory miRNAs in BC making these inflammasome-related molecules a reliable non-invasive tool for BC diagnosis.
Keywords: miRNA, bladder cancer, inflammasome, NOD-like receptors, urine sediment, inflammation
Introduction
Bladder cancer (BC) is the second most frequent urological malignancy and it is the fourth and ninth most common cancer in men and women, respectively, in the Western world.1
About 75% of newly diagnosed BC cases are non-muscle invasive (NMI): of these, ~70% are confined to the mucosa (stage Ta), 20% involves submucosa (stage T1) and 10% are carcinoma in situ (CIS) lesions.2 Regarding prognosis, 30%–80% of NMIBC will recur and 1%–45% of cases will progress to muscle invasive form within 5 years.3 The risk of recurrence and progression increases with the stage, the grade of malignancy, the size and number of lesions and the presence of the CIS.4 Cancer mortality is significantly affected by progression rates of high-risk (HR) NMIBC and by cure rates of muscle invasive ones. BC is diagnosed by cystoscopy in addition to urinary cytology and histological evaluation of the resected tissue. However, cystoscopy is an invasive, painful and potentially infectious procedure. Although voided urine cytology represents the gold standard for the non-invasive diagnosis of BC, its low sensitivity (16%) for low-grade (LG) tumors is the main limitation; on the other hand, sensitivity rises up to 84% for high-grade (HG) BC.5 Among various malignancies, BC is intimately linked to inflammation. Transitional cells carcinoma owns high immunogenic potential and this intrinsic feature lends BC to immunotherapy.6 Tumor microenvironment is regulated by several factors such as NOD-like receptors (NLRs) that play a pivotal role in the cytokine production.6 NLR family accounts for the recognition of intracellular ligands7 by pathogen-associated molecular patterns. They are responsible for the formation of inflammasomes8 that regulate the production of inflammation-related cytokines with direct effects on tumor formation and progression.9 Many efforts have been made to confirm the involvement of NLR inflammasomes in tumorigenesis.10,11 Other factors involved in the development and maintenance of the neoplastic state are the microRNAs (miRNAs).12 MiRNAs are non-coding RNAs of about 22 nucleotides, regulating genes by pairing to target regions within the 3′UTR of messenger RNAs.
MiRNA expression is altered in several urologic malignancies, validating their pivotal role to cancer development, progression and metastasis.13 As an example, the expression of miR-200 has been found down-regulated in urine sediments from patients with BC and the ablation of tumor tissue restored the same expression levels of healthy controls.14 Similar findings were obtained for miR-125b and miR-126 that discriminate at the urine level BC subjects from healthy controls with high sensitivity and specificity.15 Expression profiling studies of miRNAs reported a significant deregulation of miR-21 and miR-205 in tissue samples from patients with BC; moreover, a miR-21/miR-205 ratio differentiates an invasive from noninvasive bladder tumor phenotype.16 The differential expression of miRNAs between BCa and normal bladder tissue leads to the elucidation of miRNA signatures as promising prognostic markers of BCa.17 For example, a miR-9, miR-182 and miR-200b signature was demonstrated to correlate with tumor aggressiveness in muscle invasive BC.18 Similar tumor features have been associated with four miRNAs signature (let-7c, miR-125b-1, miR-193a and miR-99a).19 MiRNAs exert a transcriptional regulation on NRLP3 inflammasome, and their crucial role in modulating inflammasome activity has been widely estabilished.20 We assayed the expression of NLRP3, NLRP4, NLRP9 and NAIP in urine sediments from patients harboring BC, subjects affected by bladder inflammation and healthy subjects in a previous work.11 We found an overexpression of NLRP3, NLRP4, NLRP9 and NAIP in patients with BC when compared with controls. Further stratification according to tumor stage, grade and risk of recurrence and progression showed NLRP up-regulations in patients with early-stage cancer. NAIP was overexpressed in HR patients compared with controls and in HG patients compared with CTR0 and CTR1. The aim of the present study is to evaluate a panel of miRNAs targeting those NLRs showing altered expression in BCa.11 Our interest was focused in the analysis of correlation between NLRs, their respective miRNAs and BC histology. Evaluating miRNA expression as well as their molecular targets in BC represents the starting point for a new miRNA-based diagnostic and prognostic tools.
Materials and methods
Patients
Seventy-seven patients with macroscopic or microscopic hematuria and/or irritative symptoms with negative urine culture were enrolled. All patients underwent transurethral bladder resection and histological confirmation of BC was obtained for 46 subjects (BC group), whereas a diagnosis of bladder inflammation was achieved for the remaining 31 patients (CTR1 group). Bladder inflammation was established according to the presence of lymphocytes and neutrophils infiltration without tumoral cells. A third group consisting of 28 healthy controls was included (CTR0). BC patients were stratified according to the degree of bladder wall infiltration, as reported by tumor, node, metastasis classification system (Ta, T1, T2), to the degree of histological differentiation according to the World Health Organization Grading 2004 (LG, HG)21 and to the risk of recurrence and progression according to the European Organization for Research and Treatment of Cancer risk criteria (LG, low-grade; HG, high-grade).22 Specifically, LR tumors included primary, solitary, Ta, papillary urothelial neoplasm of low malignant potential, LG, smaller than 3 cm, no CIS; HR tumors included T1 tumor or HG tumor or CIS or multiple and recurrent and large (>3 cm) Ta, LG tumors; intermediate risk were considered all tumors not defined in the two previous categories. Patients with NMIBC were further stratified in NMI LG (TaLG and T1LG) and NMI HG subtypes (TaHG and T1HG). The Ethics Committee of the University of Perugia approved the study protocols and all subjects signed an informed consent. The investigation conformed to the principles outlined in the Declaration of Helsinki (1997).
Sample collection and processing
Voided urine was collected in sterile cups. Urine was kept at 4°C and processed within 4 h. Samples were centrifuged (2,000× g, 10 min, 4°C) and cell pellets were washed twice with 1X calcium-free phosphate-buffered saline. 300 µL lysis and stabilization buffer (Total RNA Extraction Kit; Norgen Biotek Corp, Thorold, ON, Canada) were added to lyse cells and stabilize nucleic acids before RNA extraction.
RNA extraction
Total RNA including miRNAs was extracted with Total RNA Extraction Kit according to the manufacturer’s instructions. RNA was quantified with Qubit RNA HS Assay Kit (Life Technologies, Carlsbad, CA). RNA was stored at −80°C until use.
Reverse transcription and real-time PCR
Total RNA 7.5 ng were reverse transcribed with miR-CURY LNA™ Universal RT miR polymerase chain reaction (PCR), polyadenylation and complementary DNA (cDNA) synthesis kit (Exiqon, Vedbaek, Rudersdal, Denmark) according to the manufacturer’s protocol. RNA spike-in control UniSp6 was added to the RT mix (total volume 10 µL) as a positive cDNA synthesis control. Real-time PCR assays were performed with miRCURY LNA specific PCR primer set and ExiLENT SYBR® Green Master Mix (Exiqon system) on a Stratagene Mx3005P instrument (Agilent Technology, Santa Clara, CA, USA). cDNA 4 µL diluted 1:20 with nuclease-free water were used in a total reaction volume of 10 µL. UniSp6 positive control was amplified for each sample and outliers (samples with UniSp6 Ct beyond a value of 26) were discarded. Melting curve analysis was carried out, each sample was run in triplicate and results were averaged; no-template controls were included in the analysis. RNU6 was used to normalize data. The −ΔCt method was used to calculate the relative expression of the target genes as follows: −ΔCtmiRNA=− (CtmiRNA − CtRNU6).
Selection of candidate miRNAs
miRNAs predicted to target NLRs analyzed in our previous study (NLRP3, NLRP4, NLRP9, NAIP) were selected using PicTar, TargetScan, miRanda and DIANA microT algorithms. MiR-146a-5p, miR-106a-5p, miR-17p, miR-223-3p, miR-141-3p, miR-19a-3p, miR-145-5p, miR-185-5p were selected after further matching with literature data on cancer-related miRNAs. Experimentally validated and computationally predicted miRNA targets are reported in Table 1. Validated targets are marked with asterisks.
Table 1.
Summary of miRNAs and related mRNA targets
| ID | Accession | Previous IDs | mRNA targets |
|---|---|---|---|
| miR-146a-5p | MIMAT0000449 | hsa-miR-146; hsa-miR-146a | NLRP3 |
| miR-106a-5p | MIMAT0000103 | hsa-miR-106a | NLRP3 |
| miR-17-5p | MIMAT0000070 | hsa-miR-17-5p; hsa-miR-17 | NLRP3*,38 |
| miR-223-3p | MIMAT0000280 | hsa-miR-223 | NLRP3*,35 |
| miR-141-3p | MIMAT0000432 | hsa-miR-141 | NLRP3; NLRP4 |
| miR-19a-3p | MIMAT0000073 | hsa-miR-19a | NLRP9 |
| miR-145-5p | MIMAT0000437 | hsa-miR-145 | NAIP*,45 |
| miR-185-5p | MIMAT0000455 | hsa-miR-185 | NAIP |
Note:
Validated interactions.
Statistical analysis
GraphPad Prism 6.0 (GraphPad Software, Inc., San Diego, CA, USA) was employed to calculate statistical significance among groups. A P<0.05 was considered statistically significant. Logistic regression analysis was performed to evaluate the association of selected miRNAs with BC. Prediction models were based on miRNA expression values (−ΔCts). Univariate logistic regression analysis was made for each miRNA and thereafter, multivariate logistic models were built. The association between miRNAs and disease-free survival of patients was evaluated through Kaplan–Meier analysis. Groups were compared using the log-rank test.
Results
Expression levels of selected miRNAs in BC, CTR0 and CTR1 groups\
Patient data and hematological parameters are reported in Table 2. As can be seen, the absence of statistically significant differences allowed us to exclude other inflammatory processes in our cohort of patients. Median follow-up was 25.3 months (ranged from 18 to 38 months). Analysis of miRNA expression in urine sediment showed decreased levels of miR-141-3p in CTR1 with respect to both BC and CTR0 (fold changes 3.26 and 0.21, respectively). Similar results were observed for miR-19a-3p (fold changes 3.25 and 0.4, Figure 1). In contrast, the expression of miR-146a-5p significantly increased in BC compared with CTR0 (fold change 3.78, P=0.005) (Figure 1). Finally, a slight decrease of miR-146-5p was noticed in CTR1 compared with BC (fold change 3.22, Figure 1). The other miRNAs did not change in expression in the groups under analysis (Figure 1).
Table 2.
Hematological and clinical parameters of enrolled subjects
| Variables | Group I (BC, n=46) |
Group II (CTR1, n=28) |
Group III (CTR0, n=31) |
P-value I vs II |
P-value I vs III |
P-value II vs III |
|---|---|---|---|---|---|---|
| Degree of bladder wall infiltration | ||||||
| Ta | 26 | |||||
| T1 | 14 | |||||
| T2 | 6 | |||||
| Tumor grade | ||||||
| Low | 18 | |||||
| High | 28 | |||||
| Risk of recurrence and progression | ||||||
| Low | 17 | |||||
| High | 29 | |||||
| Age (years) | ||||||
| Median | 65 | 62 | 64 | 0.45 | 0.68 | 0.7 |
| Range | 45–84 | 63–81 | 47–82 | |||
| SD | 9.46 | 10.2 | 12.57 | |||
| Gender | ||||||
| Male | 37 | 24 | 25 | 0.33 | 0.9 | 0.27 |
| Female | 9 | 4 | 6 | |||
| Median | 8.15 | 7.02 | 7.64 | 0.36 | 0.49 | 0.87 |
| Range | 2.21–18.99 | 5.06–10.74 | 3.55–12.28 | |||
| SD | 3.47 | 2.38 | 2.77 | |||
| Median | 4.85 | 4.61 | 4.28 | 0.68 | 0.79 | 0.48 |
| Range | 1.04–12.59 | 2.49–6.3 | 1.82–9.02 | |||
| SD | 2.15 | 1.78 | 2.49 | |||
| Median | 2.35 | 1.52 | 1.68 | 0.16 | 0.13 | 1.00 |
| Range | 0.97–15.19 | 0.6–4.05 | 0.56–3.33 | |||
| SD | 2.35 | 1.07 | 1.12 | |||
| Median | 0.545 | 0.57 | 0.555 | 0.86 | 0.61 | 0.46 |
| Range | 0.25–1.15 | 0.14–1.33 | 0.31–1.71 | |||
| SD | 0.221 | 0.229 | 0.428 |
Abbreviations: BC, patients with bladder cancer; CTR1, subjects with bladder inflammation; CTR0, healthy controls; SD, standard deviation; mmc, cubic milliliter.
Figure 1.
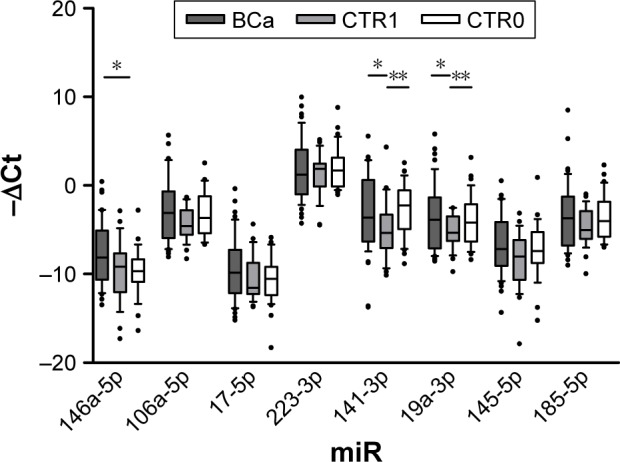
Expression levels expressed as −ΔCt (median with range and interquartile range) of selected miRNAs.
Notes: *P<0.05; **P<0.01.
Stratification of patients with BC
To investigate whether the expression levels of selected miRNAs were related to histological differentiation of BC, patients were stratified according to tumor stage, grade, risk of recurrence and progression. Moreover, miRNA expression in urine sediment from patients with HG BC was compared with NMI LG and NMI HG BC.
Tumor stage
Expression analysis of urine sediment form patients stratified according to T stage showed miR-185-5p significantly up-regulated in muscle invasive (T2) with respect to NMI cancer (Ta, fold change 15.1). Data are shown in Figure 2.
Figure 2.
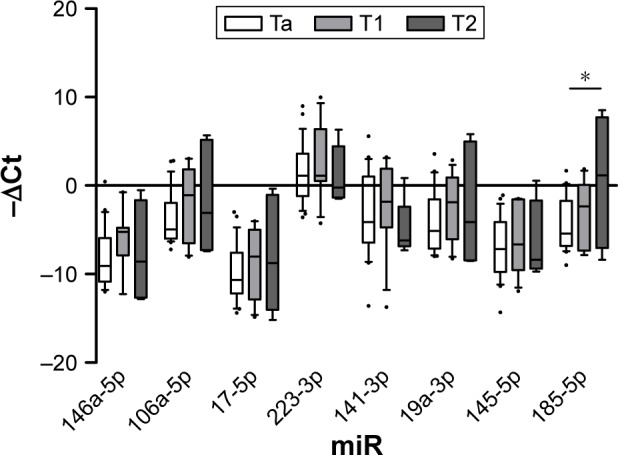
Expression levels expressed as −ΔCt (median with range and interquartile range) of selected miRNAs.
Notes: Comparisons were made according to tumor stage. *P<0.05.
Tumor grade
According to tumor grade, expression levels of miR-106a-5p, miR-17-5p, miR-19a-3p and miR-185-5p were significantly increased in urine sediment from patients with HG tumors (fold changes 4.05, 6.01, 4.53 and 4.98, respectively, Figure 3).
Figure 3.
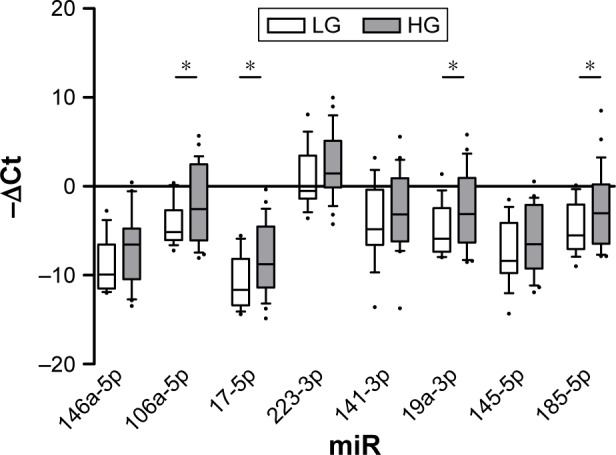
Expression levels expressed as −ΔCt (median with range and interquartile range) of selected miRNAs.
Notes: Comparisons were made according to histological grade. *P<0.05.
Abbreviations: HG, high-grade; LG, low-grade.
Risk of recurrence and progression
MiRNA expression analysis after stratification according to risk of recurrence and progression reported increased levels of miR-106a-5p, miR-17-5p, miR-19a-3p and miR-185-5p in HR versus LR tumors, as observed in HG versus LG tumors (fold changes 4.47, 5.9, 5.14 and 4.51, respectively). Moreover, miR-223-3p expression increased concomitantly to increasing risk of recurrence and progression (fold change 5.59, Figure 4).
Figure 4.
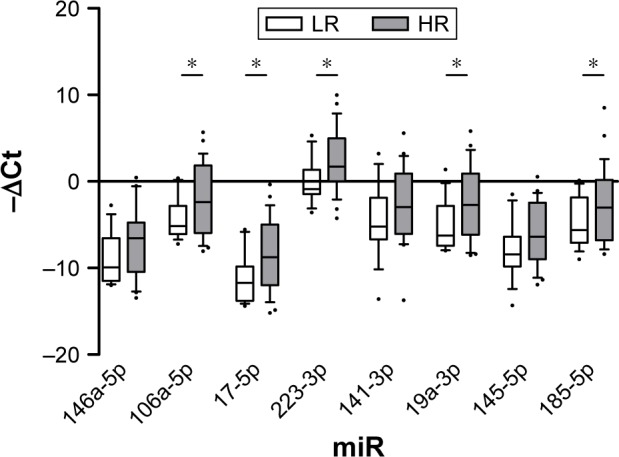
Expression levels expressed as −ΔCt (median with range and interquartile range) of selected miRNAs.
Notes: Comparisons were made according to risk of recurrence and progression. *P<0.05.
Abbreviations: HR, high-risk; LR, low-risk.
NMI LG vs NMI HG cancer
Given the peculiar expression level of miRNAs in HG and muscle invasive tumor, we set out to examine whether miRNAs targeting NLRs inflammasomes distinguish patients with NMI LG from those harboring NMI HG BC (Figure 5). Results confirmed the up-regulation of miR-106a-5p, miR-17-5p and miR-19a-3p highlighted in both grade and risk-based stratifications (fold changes 3.96, 4.8 and 4.56, respectively). Moreover, miR-146a-5p showed an up- regulation in NMI HG tumors (fold change 6.15, Figure 5).
Figure 5.
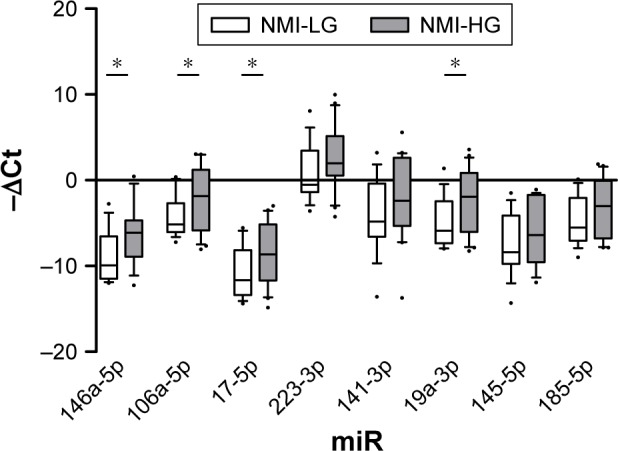
Expression levels expressed as −ΔCt (median with range and interquartile range) of selected miRNAs.
Note: *P<0.05.
Abbreviations: NMI-HG, non-muscle invasive high-grade; NMI-LG, non-muscle invasive low-grade.
Evaluation of prognostic power of miRNAs
MiRNAs from urine sediment displayed the expression level based on histological differentiation of BC. Based on previous results, miRNAs seemed to have the prognostic power to predict histological outcome. On the basis of these premises, logistic regression analysis was performed and results are shown in Table 3.
Table 3.
Univariate and multivariate logistic regression analyses of variables predicting the outcome of disease
| Logistic regression analysis | microRNA ID | P-value | (%) SN | (%) accuracy |
|---|---|---|---|---|
| HG vs LG BC | miR-17-5p | 0.045 | 76.92 | 57.14 |
| HR vs LR BC | miR-17-5p | 0.028 | 81.48 | 61.9 |
| miR-19a-3p | 0.049 | 82.14 | 60.47 | |
| NMI-LG vs NMI-HG | miR-17-5p | 0.04 | 70 | 63.89 |
| BC | miR-17-5p + miR-106a-5p + miR-19a-3p | 0.017 | 76.92 | 80.77 |
Abbreviations: BC, bladder cancer; HG, high-grade; HR, high-risk; LG, low-grade; LR, low-risk; NMI-HG, non-muscle invasive high-grade; NMI-LG, non-muscle invasive low-grade; SN, sensitivity.
HG vs LG tumor
According to the grade of histological differentiation, miR17-5p showed statistical significance in the univariate analysis. Sensitivity and accuracy were 76.92% and 57.14%, respectively (Table 3). In the multivariate logistic regression analysis, the combination of variables under analysis did not show any relevant finding (data not shown).
HR vs LR BC
Logistic regression analysis was performed to verify the ability of selected miRNAs in discriminating HR from LR BC. Results from the univariate analysis displayed high sensitivity and accuracy in predicting high risk of recurrence and progression for miR-17-5p (81.48% sensitivity, 61.90% accuracy) and for miR-19a-3p (82.24% sensitivity, 60.47% accuracy) (Table 3). Multivariate logistic regression analysis did not show any significant result (data not shown).
NMI LG vs NMI HG BC
When patients with NMI LG versus NMI HG tumor were analyzed by means of logistic regression, only miR-17-5p gave an acceptable model (70% sensitivity, 63.89% accuracy) (Table 3). In the multivariate logistic regression analysis, the combination of miR-106a-5p, miR-17-5p, miR-19a-3p and miR-146a-5p gave the best model in terms of sensitivity and accuracy (76.92% and 80.77%, respectively) (Table 3).
We also analyzed the association between miRNAs and disease-free survival of patients through Kaplan–Meier analysis. The optimal cut-off value for each miRNA was calculated by ROC analysis and used to dichotomize expression levels (high and low groups). No significant association between miRNA expression and disease-free survival was recorded (data not shown).
Discussion
Genome-wide miRNA expression signatures have been used to precisely identify aberrant miRNAs expression signatures in BC.23 Moreover, emerging evidence demonstrated that miRNAs play a pivotal role in the regulation of immunological functions and the prevention of autoimmunity. Several NLRs were validated as specific targets of selected miRNAs, while others were only predicted through algorithms (Table 1). In the present study, we evaluated inflammation-related miRNAs targeting NLRs known to be altered in BC. In our previous report, we observed an enhanced expression of NLRP3, NLRP4, NLRP9 and NAIP messenger RNAs (mRNAs) in urine sediments from patients with BC with respect to healthy controls. Furthermore, we highlighted the up-regulation of NLRP3, NLRP4 and NLRP9 in both Ta and LG tumors after stratifying by T stage, grade and risk of recurrence and progression of BC.11 In contrast, NLRP4 and NLRP9 were over-expressed in NMI LG tumors; these results suggested the potential role of inflammasomes in the early development of BC, when an innate immunity reaction occurs in the early stage of tumorigenesis. In the same study, the authors reported that NAIP mRNA level was significantly higher in patients with HG tumors than healthy controls and patients with bladder inflammation. Same results were obtained when HR patients were analyzed, suggesting an essential role of NAIP in BC progression.
Our study showed that miR-146a-5p, miR-141-3p and miR-19a-3p were differentially expressed in urine sediments from patients harboring BC, subjects with bladder inflammation and age-matched healthy controls. Down-regulation of miR-19 in CTR1 group compared with both BC and CTR0 subjects is a relevant finding since pro-inflammatory responses through miR-19a-dependent mechanisms have been recently clarified.24 MiR-19a-3p is predicted to target NLRP9 and its increased expression, together with NLRP4, has been reported in less malignant tumors in our previous work.11 Moreover, miR-19a-3p significantly decreases the SOCS3 mRNA level with consequent enhanced IFN-α and IL-6 signal transduction.24 The regulation of SOCS molecules by miR-19a and its involvement in inflammatory processes has been also reported in multiple myeloma cells.25 Down-regulation of miR-19a in post-digital rectal examination urine sediments from patients harboring prostate cancer has also been shown in our previous study.26 MiR-146a-5p is aberrantly expressed in thyroid,27 prostate28 and gastric cancers.29 Increased miR-146a-5p expression seems to inhibit cell proliferation, migration and invasion.29 Targeting of STAT by miR-146a has been reported by Hou et al, who analyzed its effects on the IFN-α signaling pathway in hepatocytes infected by hepatitis B virus.30 In patients with BC, a genetic variant of miR-146a-5p is associated with high risk of recurrence.31 According to the recent literature, our results showed increased expression of miR-146a-5p in BC compared with CTR0, while no significant modifications in CTR1 subjects compared with both BC and CTR0 groups were recorded. These results seem to be in contrast with the up-regulation of NLRs in BC patients reported in our previous work.11 Nonetheless, miR-146a-3p could exert a prominent role in carcinogenesis beyond controlling inflammation. This could be especially true since a validated interaction between miR-146a-5p and its NLR target mRNA has not yet been validated. In fact, miR-146-a-5p levels in BC patients did not differ significantly from CTR1 group, which instead occurs for miR-19a-3p and miR-141-3p. Studies on miR-141 have shown its involvement in different autoimmune diseases, such as systemic lupus erythematosus,32 inflammatory bowel disease,33 psoriasis34 and other immune-related diseases. Although its role in different cancers is well known as well,14 no significant modifications in miR-141 expression between BC patients and controls has been reported in our study. Regarding T stage stratification, miR-223-3p, miR-17-5p and miR-185-5p up-regulation in both NMI and muscle invasive BC has been described.35 In our study, only an increased expression of miR-185–5p in T2 tumors (Figure 2) was found compared with both Ta and T1 ones, while neither miR-223-3p nor miR-17-5p showed significant alterations between muscle invasive versus NMI tumors. Besides NLRP3, other genes have demonstrated to be specifically targeted by miR-223-3p. In particular, ZEB1 was proven to be suppressed by miR-223–3p in BC cell lines treated with Ginkgolide B.36 Furthermore, SEPT6 was reported to be specifically targeted by miR-223-3p in prostate cancer cell lines.37 Among miRNAs involved in inflammation, miR-17-5p deserves particular attention as member of miR-17/92 cluster involved in tumorigenesis, immune diseases, cardiovascular diseases, neurodegenerative diseases and aging.14 MiR-17 has been recently discovered to destabilize the thioredoxin-interacting protein mRNA, which is responsible for the activation of the NLRP3 inflammasome, causing Caspase-1 cleavage and IL-1β secretion.38 Tazi et al identified the Mirc1/Mir17–92 cluster as a potential negative regulator of autophagy-related genes in cystic fibrosis macrophages.39 In our analysis, miR-17-5p was significantly up-regulated in HG (Figure 3), HR (Figure 4) and NMI HG tumors (Figure 5). Similar pattern of expression was reported for miR-106a-3p and miR-19-a-3p (Figures 3–5). Large-scale miRNA microarray studies established the oncogenic nature of miR-106a for colon, pancreas and prostate carcinomas.40 High levels of circulating miR-106a have been associated with risk of aggressive lung cancer41 and gastric cancer together with miR-17–5p.42 Moreover, chemoresistance and poor survival of patients with ovarian cancer were associated with the up-regulation of miR-106a.43 Similarly, a recent study outlined the oncogenic properties of miR-19a demonstrating its overexpression in BC tissue. A correlation between miR-19a levels and cancer aggressiveness was also outlined.44 In the present study, increased expression of miR-106a-5p, miR-17-5p and miR-19a-3p was associated with HG and HR BC. Therefore, the prognostic value of selected miRNAs was assessed; miR-17-5p seemed to discriminate HG from LG BC with 76.92% sensitivity and 57.14% accuracy. Furthermore, miR-170-5p was able to predict HR patients compared with LR counterparts. Similar results were observed for miR-19a-3p (82.24% sensitivity, 60.47% accuracy). Finally, the accuracy of selected miRNAs in discriminating NMI LG from NMI HG patients was investigated: again, in the univariate model, miR-17-5p performed the best (56.25% specificity, 70% sensitivity, 63.89% diagnostic accuracy). The combination of miR-106a-5p, miR-17-5p, miR-19a-3p and miR 146a-5p outperformed miR-17-5p (+6.92% sensitivity, +16.88% accuracy). Our results highlight a correlation between miRNA expression levels and disease severity. The molecular recognition of patients harboring HG tumors exerts a crucial importance in clinical practice. Inflammasome components and their regulatory pathways could allow the recognition of those BC subtypes with unfavorable prognosis needing both early diagnosis and surgical therapy. Moreover, as future perspective, they may become novel targets to develop a targeted immunotherapy because of their role in cancer immunity.
Conclusion
Our study showed that miR-146a-5p, miR-141-3p and miR-19a-3p are differentially expressed in urine sediments from patients harboring BC, subjects with bladder inflammation and age-matched healthy controls. Furthermore, increased expression of miR-106a-5p, miR-17-5p and miR-19a-3p was associated with HG and HR BC. According to T stage stratification, only miR-185-5p was significantly higher in muscle invasive tumors with respect to NMI ones.
The increased expression of miRNAs targeting NLRs in HG and HR BC is in accordance with the decrease in NLR mRNAs involved in tumorigenesis and progression of BC. Our data highlight the pivotal role of NLRs in BC and confirm the hypothesis that their regulation is mediated by miRNA. Then, these inflammasome-related molecules may be used as potential candidates for non-invasive diagnostic tool of BC. However, the potential ability of urine miRNAs for the prediction of tumor stage and grade needs further investigations because the accuracy obtained in the present study does not allow their clinical use as diagnostic tools compared with more achievable urine cytology.
Acknowledgments
This work was supported by Fondazione Cassa di Risparmio Terni e Narni. The research was performed in the Department of Surgical and Biomedical Sciences, Via Mazzieri 3, 05100 Terni, University of Perugia, Italy. Ettore Mearini and Giulia Poli share first authorship.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Kirkali Z, Chan T, Manoharan M, et al. Bladder cancer: epidemiology, staging and grading, and diagnosis. Urology. 2005;66(Suppl 6A):4–34. doi: 10.1016/j.urology.2005.07.062. [DOI] [PubMed] [Google Scholar]
- 3.Van Rhijn BW, Burger M, Lotan Y, et al. Recurrence and progression of disease in non-muscle-invasive bladder cancer: from epidemiology to treatment strategy. Eur Urol. 2009;56(3):430–442. doi: 10.1016/j.eururo.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Losa A, Hurle R, Lembo A. Low dose bacillus Calmette-Guerin for carcinoma in situ of the bladder: long-term results. J Urol. 2000;163(1):68–71. [PubMed] [Google Scholar]
- 5.Vrooman OPJ, Witjes JA. Urinary markers in bladder cancer. Eur Urol. 2008;53(5):909–916. doi: 10.1016/j.eururo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Zitvogel L, Kepp O, Galluzzi L, Kroemer G. Inflammasomes in carcinogenesis and anticancer immune responses. Nat Immunol. 2012;13(4):343–351. doi: 10.1038/ni.2224. [DOI] [PubMed] [Google Scholar]
- 7.Motta V, Soares F, Sun T, Philpott DJ. NOD-like receptors: versatile cytosolic sentinels. Physiol Rev. 2015;95(1):149–178. doi: 10.1152/physrev.00009.2014. [DOI] [PubMed] [Google Scholar]
- 8.Henao-Mejia J, Elinav E, Strowig T, Flavell RA. Inflammasomes: far beyond inflammation. Nat Immunol. 2012;13(4):321–324. doi: 10.1038/ni.2257. [DOI] [PubMed] [Google Scholar]
- 9.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G. Inflammation and cancer: how hot is the link? Biochem Pharmacol. 2006;72(11):1605–1621. doi: 10.1016/j.bcp.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 11.Poli G, Brancorsini S, Cochetti G, Barillaro F, Egidi MG, Mearini E. Expression of inflammasome-related genes in bladder cancer and their association with cytokeratin 20 messenger RNA. Urol Oncol. 2015;33(12):505.e1–e7. doi: 10.1016/j.urolonc.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Di Leva G, Garofalo M, Croce CM. MicroRNAs in cancer. Ann Rev Pathol. 2014;9:287–314. doi: 10.1146/annurev-pathol-012513-104715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guancial EA, Bellmunt J, Yeh S, Rosenberg JE, Berman DM. The evolving understanding of microRNA in bladder cancer. Urol Oncol. 2014;32(1):41. doi: 10.1016/j.urolonc.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang G, Chan ES, Kwan BC, et al. Expression of microRNAs in the urine of patients with bladder cancer. Clin Genitourin Cancer. 2012;10(2):106–113. doi: 10.1016/j.clgc.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Snowdon J, Boag S, Feilotter H, Izard J, Siemens DR. A pilot study of urinary microRNA as a biomarker for urothelial cancer. Can Urol Assoc J. 2013;7(1–2):28–32. doi: 10.5489/cuaj.11115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neely LA, Rieger-Christ KM, Neto BS, et al. A microRNA expression ratio defining the invasive phenotype in bladder tumors. Urol Oncol. 2010;28(1):39–48. doi: 10.1016/j.urolonc.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Yoshino H, Seki N, Itesako T, Chiyomaru T, Nakagawa M, Enokida H. Aberrant expression of microRNAs in bladder cancer. Nat Rev Urol. 2013;10(7):396–404. doi: 10.1038/nrurol.2013.113. [DOI] [PubMed] [Google Scholar]
- 18.Pignot G, Cizeron-Clairac G, Vacher S, et al. microRNA expression profile in a large series of bladder tumors: identification of a 3-miRNA signature associated with aggressiveness of muscle-invasive bladder cancer. Cancer. 2013;132(11):2479–2491. doi: 10.1002/ijc.27949. [DOI] [PubMed] [Google Scholar]
- 19.Xu Z, Yu YQ, Ge YZ, et al. MicroRNA expression profiles in muscle-invasive bladder cancer: identification of a four-microRNA signature associated with patient survival. Tumor Biol. 2015;36(10):8159–8166. doi: 10.1007/s13277-015-3559-z. [DOI] [PubMed] [Google Scholar]
- 20.Sutterwala FS, Haasken S, Cassel SL. Mechanism of NLRP3 inflammasome activation. Ann N Y Acad Sci. 2014;1319:82–95. doi: 10.1111/nyas.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacLennan GT, Kirkali Z, Cheng L. Histologic grading of non-invasive papillary urothelial neoplasms. Eur Urol. 2007;51(4):889–898. doi: 10.1016/j.eururo.2006.10.037. [DOI] [PubMed] [Google Scholar]
- 22.Babjuk M, Böhle A, Burger M, et al. EAU guidelines on non-muscle-invasive bladder cancer. Eur Urol. 2011;59:584–594. doi: 10.1016/j.eururo.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Yonghua H, Jiahao C, Xiaokun Z, et al. MicroRNA expression signatures of bladder cancer revealed by deep sequencing. PLoS One. 2011;6(3):e18286. doi: 10.1371/journal.pone.0018286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collins AS1, McCoy CE, Lloyd AT, Stevenson NJ. miR-19a: an effective regulator of SOCS3 and enhancer of JAK-STAT signalling. PLoS One. 2013;8(7):e69090. doi: 10.1371/journal.pone.0069090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pichiorri F, Suh SS, Ladetto M, et al. MicroRNAs regulate critical genes associated with multiple myeloma pathogenesis. Proc Natl Acad Sci U S A. 2008;105(35):12885–12890. doi: 10.1073/pnas.0806202105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egidi MG, Guelfi G, Cochetti G, et al. Characterization of kallireins and microRNAs in urine sediment for the discrimination of prostate cancer from benign prostatic hyperplasia. J Cancer Sci Ther. 2015;7:4. [Google Scholar]
- 27.Graham ME, Hart RD, Douglas S, et al. Serum microRNA profiling to distinguish papillary thyroid cancer from benign thyroid masses. J Otolaryngol Head Neck Surg. 2015;44:33. doi: 10.1186/s40463-015-0083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu B, Huang Y, Niu X, et al. Hsa-miR-146a-5p modulates androgen-independent prostate cancer cells apoptosis by targeting ROCK1. Prostate. 2015;75(16):1896–1903. doi: 10.1002/pros.23068. [DOI] [PubMed] [Google Scholar]
- 29.Li H, Xie S, Liu M, et al. The clinical significance of downregulation of mir-124–3p, mir-146a-5p, mir-155–5p and mir-335–5p in gastric cancer tumorigenesis. Int J Oncol. 2014;45:197–208. doi: 10.3892/ijo.2014.2415. [DOI] [PubMed] [Google Scholar]
- 30.Hou ZH, Han QJ, Zhang C, Tian ZG, Zhang J. miR146a impairs the IFN-induced anti-HBV immune response by downregulating STAT1 in hepatocytes. Liver Int. 2014;34(1):58–68. doi: 10.1111/liv.12244. [DOI] [PubMed] [Google Scholar]
- 31.Wang M, Chu H, Li P, et al. Genetic variants in miRNAs predict bladder cancer risk and recurrence. Cancer Res. 2012;72(23):6173–6182. doi: 10.1158/0008-5472.CAN-12-0688. [DOI] [PubMed] [Google Scholar]
- 32.Wang G, Tam LS, Li EK, et al. Serum and urinary free microRNA level in patients with systemic lupus erythematosus. Lupus. 2011;20(5):493–500. doi: 10.1177/0961203310389841. [DOI] [PubMed] [Google Scholar]
- 33.Pekow JR, Kwon JH. MicroRNAs in inflammatory bowel disease. Inflamm Bowel Dis. 2012;18(1):187–193. doi: 10.1002/ibd.21691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zibert JR, Løvendorf MB, Litman T, et al. MicroRNAs and potential target interactions in psoriasis. J Dermatol Sci. 2010;58(3):177–185. doi: 10.1016/j.jdermsci.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 35.Haneklaus M, Gerlic M, O’Neill LA, Masters SL. miR-223: infection, inflammation and cancer. J Intern Med. 2013;274(3):215–226. doi: 10.1111/joim.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhi Y, Pan J, Shen W. Ginkgolide B inhibits human bladder cancer cell migration and invasion through microRNA-223-3p. Cell Physiol Biochem. 2016;39(5):1787–1794. doi: 10.1159/000447878. [DOI] [PubMed] [Google Scholar]
- 37.Wei Y, Yang J, Yi L, et al. MiR-223–3p targeting SEPT6 promotes the biological behavior of prostate cancer. Sci Rep. 2014;4:7546. doi: 10.1038/srep07546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lerner AG, Upton JP, Praveen PV, et al. IRE1α induces thioredoxin-interacting protein to activate the NLRP3 inflammasome and promote programmed cell death under irremediable ER stress. Cell Metab. 2012;16(2):250–264. doi: 10.1016/j.cmet.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tazi MF, Dakhlallah DA, Caution K, et al. Elevated Mirc1/Mir17–92 cluster expression negatively regulates autophagy and CFTR (cystic fibrosis transmembrane conductance regulator) function in CF macrophages. Autophagy. 2016;12(11):2026–2037. doi: 10.1080/15548627.2016.1217370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Volinia S, Calin GA, Liu CG, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci U S A. 2006;103(7):2257–2261. doi: 10.1073/pnas.0510565103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boeri M, Verri C, Conte D, et al. MicroRNA signatures in tissues and plasma predict development and prognosis of computed tomography detected lung cancer. Proc Natl Acad Sci U S A. 2011;108(9):3713–3718. doi: 10.1073/pnas.1100048108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsujiura M, Ichikawa D, Komatsu S, et al. Circulating microRNAs in plasma of patients with gastric cancers. Br J Cancer. 2010;102(7):1174–1179. doi: 10.1038/sj.bjc.6605608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huh JH, Kim TH, Kim K, et al. Dysregulation of miR-106a and miR-591 confers paclitaxel resistance to ovarian cancer. Br J Cancer. 2013;109(2):452–461. doi: 10.1038/bjc.2013.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feng Y, Liu J, Kang Y, et al. miR-19a acts as an oncogenic microRNA and is up-regulated in bladder cancer. J Exp Clin Cancer Res. 2014;33:67. doi: 10.1186/s13046-014-0067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu X, Wu X, Jiang Q, et al. Downregulation of microRNA-1 and microRNA-145 contributes synergistically to the development of colon cancer. Int J Mol Med. 2015;36(6):1630–1638. doi: 10.3892/ijmm.2015.2364. [DOI] [PubMed] [Google Scholar]


