Abstract
Objectives
To assess how staff at Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics address potential developmental delays and parent developmental concerns in children <5 years.
Methods
A web-based survey of Oregon WIC staff in non-administrative roles assessed staff interactions with parents regarding concerning child development/behavior, perceptions of connectedness with local developmental resources, and knowledge of typical child development.
Results
Staff (n=153) responses indicated knowledge of typical child development, frequent interactions with families about child development, and frequent noticing of developmental concerns. However, most staff reported being less than very well connected to developmental resources. Open-ended responses suggested staff frequently make direct referrals to Early Intervention, public health nurses, and others who can further assess developmental concerns.
Conclusions
Although it is outside the primary scope of their work, developmental and behavioral concerns are frequently raised and addressed by WIC staff. Findings suggest that strengthening existing referral processes and enhancing continuity of care between WIC and developmental providers may improve child outcomes and reduce disparities.
Keywords: child development, developmental delay, community health, WIC
INTRODUCTION
Developmental disabilities are common in early childhood, affecting one in six U.S. children.1 Prevalent developmental conditions include speech/language delays, gross and/or fine motor delays, autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD) cerebral palsy, and genetic conditions such as Down syndrome. For children with these conditions, early access to community-based diagnosis and therapy services is key to maximizing long-term child development and functioning. Conversely, untreated developmental disabilities can adversely impact a child’s long-term developmental trajectory, physical health, and can adversely burden families.2–5
Low-income and racial and ethnic minority children are at risk for under-identification and treatment of developmental disabilities.6 Poor and/or minority children with developmental delays are less likely to participate in Part C Early Intervention,7,8 which provides free evaluations and services for young children with developmental delays, and are more likely to have unmet therapy needs.9 These patterns of under-identification and service use are also true for specific developmental conditions: for instance, ASD, which affects one in 68 U.S. children,10 is less commonly identified in early childhood for families that are low-income, Latino, or black.10 Low-income and racial and ethnic minority children with ASD also receive lesser quality care after diagnosis.11 Similarly, racial and ethnic minority children with ADHD are less likely to be diagnosed with the condition in early childhood or to receive any treatment once diagnosed.12 As a result, resources are needed to connect children at risk for unidentified developmental disabilities to community support and therapy services that can help them and their families.6
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is an important resource for low-income families during early childhood. As a prevention-focused public health nutrition program, WIC serves over half of all infants born in the U.S. each year. Children are able to participate in the program until age five if their household remains income eligible. Children ages two to four make up the single largest group of program participants representing 33.7% of WIC’s caseload.13 Racial and ethnic minority children are disproportionately represented in WIC: 40% are of Latino ethnicity and about 40% identify as races other than white.14 As a result, WIC staff work with a population that may be largely underserved in health and developmental care. Low-income families interact with WIC not only to receive supplemental foods but also to receive health and growth screenings, nutrition education, lactation support, and referrals to appropriate health and community resources. Many parents attend WIC classes that link nutrition with parenting issues such as strategies for dealing with picky eaters and how to involve kids with shopping and cooking activities. WIC staff frequently live in the same communities as WIC families and may be of similar racial, ethnic, and sociodemographic background; as a result they are often trusted community members.
Consequently, it is likely that WIC staff interact frequently with families around the topic of child development; however, little is known about how WIC staff interact with families when either staff or parents identify possible developmental conditions, or how staff address these concerns. Many WIC staff are paraprofessionals and not all dietetics programs include training on typical child development or community resources for children experiencing developmental delays. Though part of WIC’s federal mandate is to provide referrals and access to other health-related and public assistance programs,15 this mandate does not specifically include counseling on child development. As a result, staff may have varied ability or motivation to identify and take action on parent developmental concerns.
The present study was part of a larger statewide assessment of developmental needs within WIC. As part of that project, we surveyed a statewide sample of WIC staff to assess their knowledge of signs of possible developmental delays and community resources for families identifying developmental concerns. Our primary research questions were: (1) How often do WIC staff engage with parents about developmental concerns? (2) How well can WIC staff identify signs of developmental delay? and (3) How connected are WIC staff with medical and community resources for children with developmental disabilities?
METHODS
Study Sample and Design
In 2015 we conducted a web-based survey of Oregon WIC staff. To be included in the study sample, staff had to hold a clinical position at any WIC office in Oregon as of September 2015; clinical positions were defined as those separate from administrative staff that regularly had direct contact with families (e.g., registered dietitian, certifier). All eligible staff were sent an email link to complete the survey and received a coffee gift card as a participation incentive. Of the 191 eligible staff contacted, 153 were successfully surveyed thereby achieving a response rate of 80%. Of the 34 WIC programs in the state, 33 clinics had at least one staff member complete the survey. The largest site made up 12.7% of the total staff survey sample. Oregon Health & Science University’s Institutional Review Board approved the study protocol.
Survey Development
Given that there were no existing scales for assessing the relationship between WIC and developmental providers, all survey items were created by the study team, which included WIC staff, through an iterative process. The goal was to develop survey items that would be easily understood by staff filling various WIC positions requiring direct contact with families.
Measures
The survey consisted of 21 structured items assessing staff interactions with parents regarding child development or behavioral concerns, staff perceptions of connectedness with local developmental resources, staff knowledge of typical child development, staff comfort levels with children with developmental disabilities, and open-ended questions about interactions with families.
Frequency of interactions with parents
To quantify staff interactions with parents regarding concerning child development or behavior we presented staff with two questions: (1) In your job at WIC, about how often do you have significant concerns about a child’s learning, development, or behavior? (2) About how often do parents at WIC ask you questions about their child’s learning, development, or behavior? Response options to both questions were “more than once per week,” “between once per week and once per month,” “less than once per month,” and “never.” In analyses, we dichotomized outcomes as “more than once per week” and “less than once per week.”
Child development knowledge items
In order to assess staff knowledge of typical child development, participants were presented with a hypothetical scenario about a two-year child displaying 11 behaviors that ranged from typical for age (e.g., “he does not recognize any letters or numbers”) to those that were concerning for a developmental condition (e.g., “he does not respond to his name when his mom calls”). Staff were asked to answer whether they were “not very concerned” or “yes, concerned” about each behavior. Specific behaviors studied spanned a range of physical, social, and feeding behaviors, and were adapted from validated parent-reported development questionnaires, including the Ages and Stages-3 Questionnaire,16 the Modified Checklist for Autism in Toddlers – Revised with Follow-up,17 and the Center for Disease Control and Prevention’s (CDC) “Learn the Signs. Act Early” parent checklist.18 Total number of correct responses to the item set were used as a measure of knowledge of early childhood development.
Community connections
We used two survey items to identify how connected staff perceived their WIC office to be with local developmental resources. The first, asked “How connected is your WIC office to your county Early Intervention/Early Childhood Special Education program (EI/ECSE)?” EI/ECSE is a combined program in Oregon. This question was rated on a four-point scale: “not very connected,” “somewhat connected,” “very connected,” and “do not know.” Responses were dichotomized as “very connected” and “less than very connected,” which included the other three response options. The second question on connections to developmental resources asked “Which of the following best describes your WIC office’s connection with pediatric healthcare providers in your area?” Response options included: “well connected with almost all,” “well connected with some but not others,” “poorly connected with most,” and “do not know.” Responses were re-categorized into two groups: “well connected with almost all” and “less than well connected,” which included the other three response options.
Open-ended questions
With the intent of obtaining a richer understanding of staff experiences, we asked staff who shared that they had noticed a concerning behavior in a child to respond to three open-ended questions. Questions read: (1) “Tell us about a time you noted a concern and shared it with the family. What happened?” (2) “How can WIC help parents be more aware of whether their child’s development is on track?” and (3) “In your opinion, how can WIC reduce challenges for families whose children have developmental conditions?”
Statistical Analysis
Descriptive statistics were used to assess the study population by individual and WIC clinic characteristics (Table 1). To investigate WIC staff understanding of early childhood development, mean, median, and overall proportion of correct responses and standard deviations were calculated for the previously described case vignette.
Table 1.
Study sample characteristics
| Overall Percentage or Mean (SD) | |
|---|---|
|
| |
| Individual Characteristics | N=153 |
|
| |
| Position type | |
|
| |
| Certifiera (n=83) | 60.6 |
| RD (n=25) | 18.3 |
| RN (n=5) | 3.7 |
| Coordinatorb (n=24) | 17.5 |
|
| |
| Years worked at WIC | |
|
| |
| Mean number of years | 12.5 (8.8) |
| Range of work years | 0–43 |
|
| |
| Spanish-English bilingual | |
|
| |
| No (n=93) | 60.8 |
| Yes (n=60) | 39.2 |
|
| |
| Age | |
|
| |
| Staff age | 45.1 (12.3) |
| Range of staff age | 21–72 |
|
| |
| Race | |
|
| |
| White (n=114) | 88.4 |
| Black/African American (n=2) | 1.6 |
| American Indian/Alaska Native (n=6) | 4.7 |
| Asian (n=2) | 1.6 |
| Multiple race/other (n=5) | 3.9 |
|
| |
| Latino/Hispanic ethnicity | |
|
| |
| Latino/Hispanic (n = 33) | 24.6 |
| Not Latino/Hispanic (n=101) | 75.4 |
|
| |
| Clinic Characteristics | |
|
| |
| Urbanicity of WIC clinic | |
|
| |
| Metropolitan area (n=94) | 68.6 |
| Nonmetropolitan area, adjacent to metro area (n =32) | 23.4 |
| Nonmetropolitan area, nonadjacent to metro area (n=11) | 8.0 |
Abbreviations: RD, registered dietitian; RN, registered nurse; SD, standard deviation; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
WIC staff authorized to assess program eligibility, determine nutrition risk, and prescribe supplemental foods.
Individual who acts as local program representative with the state WIC program and partner organizations. Depending on the clinic, this individual may also take on the responsibilities of a certifier.
Descriptive statistics were used to assess the frequency of WIC staff developmental concerns and connectedness outcomes, including frequency of noticing concerns, frequency of being asked about concerns, and connectedness with developmental resources. Bivariate analyses including Pearson Chi-square tests, and multivariable logistic regression were then used to examine the associations of individual respondent and WIC clinic characteristics with each of these outcomes (Table 2). Multivariable models included all factors shown in Table 2 as covariates. To assess whether staff who had frequent developmental concerns were more strongly connected with developmental resources than other staff, we used bivariate analyses to identify the proportions, along with 95% confidence intervals, of staff who noticed and were asked concerns with those who were connected to developmental resources. All analyses were conducted with Stata 13.1 (College Station, Texas).
Table 2.
Staff experiences with child development and behavior concerns, by individual and clinic characteristic
| Staff noticed DB concerns >1 per week (n=42) |
Staff asked about DB concerns >1 per week (n=60) |
Staff felt < very connected with EI/ECSE (n=105) |
Staff felt < well connected with pediatric healthcare providers (n=114) |
|
|---|---|---|---|---|
| Overall % of staff with outcome (95% CI) | 27.6 (21.0–35.4) | 39.5 (31.9 – 47.5) | 69.3 (61.4 – 76.2) | 74.3 (66.7 – 80.7) |
|
| ||||
| Individual Characteristics, % of staff with outcome (95% CI) | ||||
|
| ||||
| Years of Work at WIC | ||||
|
| ||||
| 5 years or less (n=38) | 26.3 (14.6 – 42.8) | 34.2 (20.8 – 50.8) | 79.0 (62.8 – 89.3) | 76.3 (60.0 – 87.4) |
| More than 5 years (n=100) | 27.0 (19.1 – 36.7) | 39.0 (29.8 – 49.0) | 68.3 (58.5 – 76.7) | 74.0 (64.4 – 81.7) |
| P-valuea | 0.910 | 0.651 | 0.246 | 0.757 |
|
| ||||
| Position | ||||
|
| ||||
| Certifier (n=83) | 19.3 (12.1 – 29.4) | 39.8 (29.7 – 50.8) | 73.5 (62.4 – 82.0) | 79.3 (69.0 – 86.8) |
| RD (n=25) | 56.0 (36.1 – 74.2) | 44.0 (25.8 – 63.9) | 76.0 (55.2 – 89.1) | 52.0 (32.6 – 70.9) |
| RN (n=5) | 40.0 (8.1 – 83.4) | 20.0 (2.1 – 74.8) | 60.0 (16.6 – 91.9) | 60.0 (16.6 – 91.9) |
| Coordinator (n=24) | 21.7 (9.1 – 43.6) | 17.4 (6.5 – 39.0) | 66.7 (45.5 – 82.8) | 79.2 (57.9 – 91.3) |
| P-valuea | 0.003 | 0.157 | 0.804 | 0.042 |
|
| ||||
| Spanish-English Bilingual | ||||
|
| ||||
| No (n=93) | 30.4 (21.8 – 40.7) | 43.5 (33.6 – 53.9) | 66.7 (56.4 – 75.6) | 72.8 (62.7 – 81.0) |
| Yes (n=60) | 23.3 (14.2 – 35.9) | 33.3 (22.5 – 46.3) | 73.3 (60.6 – 83.1) | 76.7 (64.1 – 85.8) |
| P-valuea | 0.339 | 0.211 | 0.383 | 0.596 |
|
| ||||
| Clinic Characteristics, % of staff with outcome (95% CI) | ||||
|
| ||||
| Urbanicity | ||||
| Metropolitan area (n=94) | 29.8 (21.3 – 39.9) | 44.7 (34.8 – 55.0) | 74.5 (64.6 – 82.4) | 75.5 (65.7 – 83.3) |
| Nonmetropolitan area, adjacent to metro area (n=32) | 21.9 (10.6 – 29.8) | 25.0 (12.8 – 43.1) | 60.6 (42.9 – 75.9) | 78.1 (60.2 – 89.4) |
| Nonmetropolitan area, non-adjacent to metro area (n=11) | 18.2 (4.2 – 52.9) | 18.2 (4.2 – 52.9) | 72.7 (39.6 – 91.6) | 54.6 (25.5 – 80.8) |
| P-valuea | 0.576 | 0.034 | 0.430 | 0.290 |
P-value for Pearson Chi-square test
Abbreviations: CI, confidence interval; DB, developmental/behavioral, EI/ECSE, Early Intervention/Early Childhood Special Education; RD, registered dietitian; RN, registered nurse; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Analyses of Open-Ended Questions
Responses to open-ended questions were initially reviewed by the entire study team for major thematic content, and a list of preliminary codes were developed. Subsequently two team members independently coded all staff responses according to the initial coding framework; discrepancies were resolved by mutual discussion between the coders and a third team member. When necessary new codes were added to the framework. For the first open-ended question, a table was created to display a representative quotation illustrating the theme’s content and relative frequency (Table 3). Themes from the other two questions are not presented in tables but are discussed.
Table 3. Frequencies of types of responses that occur after staff note and share developmental concerns with families.
Tell us about a time you noted a [developmental/behavioral] concern and shared it with the family. What happened?
| Type of response to staff sharing concern | Quote exemplifying response type | Frequency |
|---|---|---|
| Staff actions | ||
| Referral to community agency (e.g. Early Intervention, Public Health Nurse) or parent was offered extra resources/screenings | “I noticed that I could not understand any of the child’s speech. I asked if the parent could interpret the conversation. She could not. The child was new to WIC and was 4 [years] old. I told her we could direct her to Early Childhood Development and Head Start for speech therapy that would be no cost to the family. She was thrilled. Next visit He was using words and was in therapy with hearing services. Super feeling to help!” | 60 |
| Referral to Primary Care Provider | “Yesterday; I got a 3 year old acting up, crying for no apparent reason. Behaving with fear just by standing next to her to get her weight and height. Mom says she is afraid all the time, mom had to quit her job because child does not wanted to leave her side. Child does not verbally articulate what is happening, just cry and seem anxious. Mom says she is not concerned; I referred the mom to her doctor and look for help if possible.” | 25 |
| Staff attempt to assess family’s willingness to address concern | “I asked ‘tell me, what has the doctor said about the patient’s behavior?’ That usually opens the flood gates of how the parent had been concerned, talked to the doctor, the doctor didn’t do anything. I did a county health nurse referral. The county health nurse helped get the child the help that was needed.” | 29 |
| Staff confirm concerns noted in another setting | “Noticed 9 month old twin babies not having good head control or able to sit without a lot of support. Encouraged the family to talk to [doctor] about it. Mentioned that [doctor] already did, but they didn’t think it was that serious. Helped them understand the importance of having follow up.” | 8 |
| Staff felt unequipped to bring up concern | “I felt inappropriate by approaching. I didn’t feel as though I had the right skills to broach that topic.” | 2 |
| Parent responses | ||
| Parents appreciated staff’s concern | “The parent was unaware of any [developmental disability] and was not receptive to the possibility. Many times the parents have been receptive.” | 21 |
| Parent said they accept concern or have a neutral reaction | “Mom was receptive, stated she has noticed the same thing but wasn’t sure if it was just her being too worried. Referral given to [Early Intervention] and encouraged her to discuss with [doctor].” | 18 |
| Parent dismissed or denied concerning behavior | “Depending on the parents, sometimes they don’t want to see the problem, and other[s are] very open to find out if the child has a problem.” | 15 |
| Parent decide to wait and see it concerning behavior continues or have other neutral reaction | “I expressed my concern and told her she should keep an eye out for it and if she saw it again she should tell her doctor.” | 6 |
| Parent initiated concern by sharing it with staff | “Most of the time, the parent is usually the one mentioning the concern.” | 8 |
RESULTS
Among, the 153 WIC staff surveyed, 60.6% were certifiers, 18.3% were registered dietitians (RD), 17.5% were clinic coordinators, and 3.7% were registered nurses (RN). Overall, the median time staff reported working at WIC was 12 years, with individual years ranging from zero to 43. A majority of staff surveyed were white (88.4%) and not Latino/Hispanic (75.4%); slightly more than a third reported speaking Spanish (39.2%). Mean staff age was 45.1 years old (Standard Deviation [SD]=12.3; Table 1). 68.6% of respondents worked at a WIC local clinic in a metropolitan area per the U.S. Census Rural-Urban Continuum Codes designation.19
Descriptive frequencies of the child development knowledge items indicated that WIC staff correctly answered most of the questions, attaining an average score 81.8% (SD=22.0%). In other words, on average, staff correctly answered 8.9 (SD=2.4) out of 11 possible items (median=10). There were no differences in staff knowledge of typical child development by position type.
WIC staff reported frequent interactions with families about topics related to child development. A majority of staff either noticed concerns or were asked about concerns “more than once per week” and “between once per week and once per month;” very few staff reported “never” having these types of interactions around child development (Figure 1). Overall, 27.6% of staff reported noticing developmental or behavioral concerns in a child more than once per week. On bivariable and multivariable analysis, dietitians were more likely than other types of WIC staff to notice concerns at least weekly (56.0% versus 19.3% for certifier, Chi-square p=0.003, Adjusted Odds Ratio (AOR) 4.83 [95% Confidence Interval [CI] 1.83–12.82]. There were no other significant differences in noticing concerns according to staff or clinic characteristics. 39.5% of staff reported being asked about concerns by a parent more than once per week; clinics that were in non-metropolitan, non-adjacent to metropolitan areas were less likely to have staff be asked about concerns on bivariable but not multivariable analyses (18.2% versus 44.7% in metropolitan areas, Chi-square p=0.03).
Figure 1.
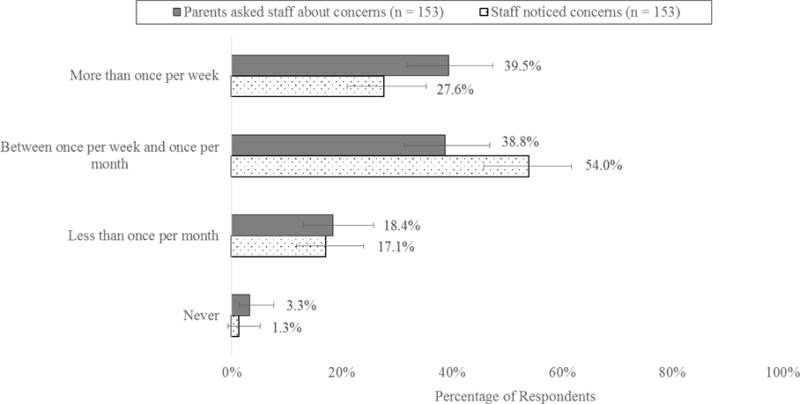
Frequency of WIC staff being asked about developmental concerns and noticing concerning behaviors in a child
When asked about their clinic’s connection to local developmental resources, a majority of staff (69.3%) reported being less than very connected with EI/ECSE and less than well connected with pediatric healthcare providers in their area (74.3%). There were no differences in staff connection with EI/ECSE by staff or clinic characteristics. There was a difference in staff connection with pediatric healthcare providers according to position type: on bivariable and multivariable analyses dietitians had the most connection with pediatric healthcare providers (52.0% <well connected versus 79.3% of certifiers, p=0.04; AOR 4.02 [95% CI 1.51–10.75]).
Since it was possible that a small portion of staff at WIC had more expertise in developmental issues and also had better connections with community resources, we specifically assessed connectedness with community resources among those WIC staff that noted developmental concerns most frequently. Bivariate analyses revealed that among WIC staff who reported noticing concerns more than once per week, 71.4% (55.8%–83.2%) also reported being less than very connected with EI/ECSE and 81.0% (66.0%–90.3%) reported being less than well connected with pediatric healthcare providers (Table 3). Similarly, among staff who reported being asked about concerns more than once per week, 63.3% (50.3%–74.7%) reported being less than very connected with EI/ECSE and 76.7% (64.1%–85.8%) reported being less than well connected with pediatric healthcare providers. Together, these results suggest staff who frequently notice concerns and who are frequently asked about concerns also do not feel connected to resources (i.e., EI/ECSE, pediatric providers) that could further assess developmental and behavioral concerns.
Analysis of responses to the open-ended question “Tell us about a time you noted a [developmental or behavioral] concern and shared it with the family. What happened?” elicited numerous descriptions of clinical encounters with children having developmental delays including speech and motor delays, as well as behavioral disturbances. We coded both staff actions and parent responses to staff actions (Table 3). The most frequent staff action was described as making a direct referral to a community resource such as EI/ECSE or a county health nurse who could further assess a child’s development. Staff would also frequently refer to the child’s primary care provider for developmental concerns. Some staff attempted to assess a parent’s readiness to address the developmental concern before making a recommendation; several noted that motivational interviewing skills they learned for nutrition counseling were useful in this setting. WIC staff also noted that they often served as another voice to confirm a parent’s concerns or to confirm concerns that another community member had raised about a child’s development. Per staff reports, parents had varying responses to staff’s actions. They frequently appreciated WIC staff’s concern and often were grateful for referral resources. Nonetheless, some parents had a more neutral or wait-and-see attitude. Parents frequently would dismiss or deny a WIC staff member’s stated concern. Sometimes, parents were the ones to initiate a concern with WIC staff.
Analysis of the final two open-ended questions provided ideas for potential next steps for WIC. When asked how WIC can help parents be aware of typical child development, an overwhelming majority of staff responded with a call for more educational resources for staff as well as for parents, and many staff reported wanting to establish better connections with developmental and medical resources. One staff noted, “More trainings on specific age-appropriate development [are] needed for WIC staff so that they are approaching parents appropriately and making appropriate comments and not scaring parents. Offering more [parent] classes around child development is also needed!” Several staff, however, pointed out that developmental education may be out of WIC’s scope; for instance, one staff wrote “I feel as though our staff are spread thin with what they are already asked to do. If development is something WIC is expected to incorporate then they either need to refer or hire specialists.” As far as suggestions for how to make WIC visits comfortable for children with developmental disabilities, many staff proposed coordinating with other agencies to have joint appointments or to share information, such as height and weight, which may have recently been collected and could be challenging to collect again. Some staff additionally recommended having remote appointments, offering transportation, and customizing appointments by skipping optional procedures to make visits shorter or scheduling more difficult visits during quieter clinic times.
DISCUSSION
In this statewide sample, we found that developmental and behavioral concerns and conditions are a frequent topic of conversation among families and staff in WIC clinics: nearly four in 10 WIC staff were asked about a child’s development at least once per week, and nearly three in 10 noticed a developmental concern about a child at least once per week. Given that the majority of WIC staff in our study could distinguish many instances of typical versus delayed development in young children, it is likely that many of the developmental concerns raised by WIC staff are well founded.
Though developmental concerns were prevalent, WIC staff felt poorly connected to local developmental resources: almost 70% felt less than very connected with their county EI/ECSE office, and 74% felt less than well connected with most pediatric healthcare providers. Those WIC staff that fielded the most developmental concerns also felt poorly connected to primary care and community developmental resources. This study’s qualitative data revealed WIC staff often reach out to local developmental agencies such as EI/ECSE and primary care when they are concerned about a child’s development or behavior. However, their frequent referrals to these agencies did not engender perceptions of connectedness, which may reflect poor cross-system coordination of care.
Study results confirm that WIC is currently an important site for the early identification of developmental disabilities for low-income families; however, WIC staff may need more support to effectively refer children with developmental conditions and to improve continuity of care once EI/ECSE services are initiated. The current study shows that although WIC’s primary mission is to provide public health nutrition services and not to diagnose or address childhood developmental delays, WIC staff nonetheless spend significant time engaging with families on this topic in the course of delivery of standard WIC services. As a result, WIC staff and families may benefit from additional support for developmental issues—this kind of support could come in the form of family handouts, trainings for current staff, co-located personnel to handle developmental concerns, or even in the form of improved partnerships with community developmental resources.
Several prior efforts have been made in WIC clinics to improve developmental care, though it is unclear whether these efforts would thrive in the absence of research funding. Guerrero et al. (2013) conducted a large-scale “train the trainer” intervention in which Los Angeles WIC paraprofessional staff were trained to deliver parent education about normative child development and early identification of developmental delays in children, and delivered parent-centered messages about how to talk with primary care providers about potential developmental delays. The education program was broadly acceptable to parents, WIC staff, and primary care providers.20 Another program in Los Angeles also conducted a pilot test of co-locating a developmental specialist in WIC offices who could screen families who were identified as at risk for developmental delays based on a single developmental surveillance item incorporated into WIC nutritional assessments.21 Similarly, the CDC recently funded a study to distribute its “Learn the Signs. Act Early” program materials for the early detection of autism and other developmental disabilities via an interactive phone app that was piloted with Georgia WIC parents and staff.22 Though parents reported an app would be convenient, it is unclear whether large-scale deployment of the app would be effective in teaching WIC parents about child development.
Any effort to design an intervention in the WIC setting must take into account three key priorities; first, that WIC’s mission is primarily nutritional in nature; second, that any potential intervention must be sustainable within the limited funding constraints of WIC and what is allowable activity to be covered by the program’s funding;23 and third, that WIC staff have limited training and time to conduct developmental assessments. As a result, interventions that require significant auxiliary funding (e.g., co-location of specialized developmental providers in WIC) or extensive staff training and time (e.g., teaching WIC staff to screen and refer for developmental conditions) may not be sustainable outside of the research context. There is a strong need for effective yet low-intensity interventions that WIC can sustain. Future potential WIC-specific interventions might include designing standard workflows for addressing parent developmental concerns when they arise, or developing a centralized developmental assessment and referral resource for staff and family developmental concerns. For example, a state WIC program could refer to regional developmental specialists who could field parent concerns, conduct in-depth risk assessments, and connect families with appropriate community agencies. In states where developmental screening and assessment is a Medicaid quality metric, like in Oregon,24 Medicaid programs and Accountable Care Organizations may be interested in cooperating with this type of effort. Another potential option might be to train specific staff that field the most developmental concerns in assessment and referral resources. Results from our study suggest that training dietitians might be particularly beneficial, since they encounter the most parent concerns and have the strongest connections with primary care, likely because they see a higher-risk population than WIC certifiers. Further research on whether such interventions are feasible, sustainable, and efficacious are needed.
The study had a number of limitations. First, all activities were per staff report; there was no direct measurement of frequency of interaction with families around specific topics. Second, there was no formal item assessing frequency of referral to healthcare or community resources; thus there is no objective measure of how often these type of referrals occur, or whether they were truly appropriate. WIC staff training may differ by state, and WIC family demographics may also vary; therefore, findings may not be generalizable to some state WIC programs. The measure of connectedness with pediatric healthcare providers (“well-connected with all”) may be a relatively high bar; however, it is worth noting that over 25% of WIC staff did feel connected with all pediatric healthcare providers in their area, which suggests this standard is feasible. The study did not clarify to what extent developmental referral services provided by WIC staff were unique versus duplicative of other referrals for developmental disabilities (e.g., from primary care). However, parents may be more likely to take action on developmental concerns when they hear consistent messages across settings. Although the eleven items used to measure child development knowledge were adapted from validated parent-report measures, the items as a set were not validated against a more comprehensive measure of child development knowledge. As a result, it is difficult to know if the scores that staff achieved indicate strong overall developmental knowledge. Finally, this study focused on developmental disabilities and the link between WIC with developmental disability providers, such as EI and primary care. However, families may present with a broad spectrum of developmental and behavioral observations that do not meet Part B or C eligibility criteria, but that would nonetheless benefit from community help and support. Connecting WIC with other community supports, where they exist, is of critical importance for supporting child development across the spectrum from typical development to developmental disability. The Help Me Grow program is one example of a statewide framework that can connect parents with developmental questions to appropriate resources, increasing parent engagement in early childhood.25
CONCLUSIONS
This statewide study is the only one to-date assessing staff needs for child development resources in WIC. Study findings reveal that WIC staff already interact with families around developmental concerns in the context of nutritional assessment and counseling. These results point to a need for creation of WIC-specific resources for developmental and behavioral concerns in early childhood.
Acknowledgments
We acknowledge all of the Oregon WIC staff for their helpful participation and feedback. We also acknowledge Shon Tyler for his assistance with data analysis.
Funding: This project was funded by the National Institute of Mental Health, grant number: K23MH095828.
Footnotes
Disclosure: The authors have no conflicts of interest to disclose.
References
- 1.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in U.S. children, 1997–2008. Pediatrics. 2011;127(6):1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- 2.Herlihy LE, Brooks B, Dumont-Mathieu T, et al. Standardized screening facilitates timely diagnosis of autism spectrum disorders in a diverse sample of low-risk toddlers. J Dev Behav Pediatr. 2014;35(2):85–92. doi: 10.1097/DBP.0000000000000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vohra R, Madhavan S, Sambamoorthi U, et al. Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism. 2014;18(7):815–826. doi: 10.1177/1362361313512902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogers SJ, Vismara LA. Evidence-based comprehensive treatments for early autism. J Clinical Child Adolesc. 2008;37(1):8–38. doi: 10.1080/15374410701817808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vismara LA, Rogers SJ. Behavioral treatments in autism spectrum disorder: what do we know? Annu Rev of Clinl Psycho. 2010;6:447–468. doi: 10.1146/annurev.clinpsy.121208.131151. [DOI] [PubMed] [Google Scholar]
- 6.Perrin JM, Anderson LE, Van Cleave J. The rise in chronic conditions among infants, children, and youth can be met with continued health system innovations. Health Affair. 2014;33(12):2099–2105. doi: 10.1377/hlthaff.2014.0832. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg SA, Zhang D, Robinson CC. Prevalence of developmental delays and participation in Early Intervention services for young children. Pediatrics. 2008;121(6):e1503–e1509. doi: 10.1542/peds.2007-1680. [DOI] [PubMed] [Google Scholar]
- 8.Feinberg E, Silverstein M, Donahue S, et al. The impact of race on participation in Part C Early Intervention services. J Dev Behav Pediatr. 2011;32(4) doi: 10.1097/DBP.0b013e3182142fbd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magnusson D, Palta M, McManus B, et al. Capturing unmet therapy need among young children with developmental delay using national survey data. Acad Pediatr. 2016;16(2):145–153. doi: 10.1016/j.acap.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Christensen DL, Baio J, Braun KV, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. Morbidity and mortality weekly report Surveillance summaries (Washington, DC: 2002) 2016;65(3):1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Magaña S, Parish SL, Rose RA, et al. Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellect Dev Disabil. 2012;50(4):287–299. doi: 10.1352/1934-9556-50.4.287. [DOI] [PubMed] [Google Scholar]
- 12.Morgan PL, Hillemeier MM, Farkas G, et al. Racial/ethnic disparities in ADHD diagnosis by kindergarten entry. J Child Psychol Psyc. 2014;55(8):905–913. doi: 10.1111/jcpp.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Department of Agriculture. WIC Participant and Program Characteristics 2014 (Summary) 2015 http://www.fns.usda.gov/sites/default/files/ops/WICPC2014-Summary.pdf. Accessed February 15, 2017.
- 14.Thorn B, Tadler C, Huret N, et al. WIC Participant and Program Characteristics 2014. Alexandria, VA: 2015. (Insight policy research under contract no. AG-3198-C-11-0010). [Google Scholar]
- 15.Special Supplemental Nutrition Program for Women, Infants and Children; Subpart C - Participant Eligibility. 2016. 50 Fed Reg 6121 (Feb 13, 1985) (to be codified at 246 C.F.R. pt. 246.7).
- 16.Squires J, Twombly E, Bricker D, et al. ASQ-3 user’s guide. Baltimore, MD: Paul H. Brookes Publishing Co.; 2009. [Google Scholar]
- 17.Robins DL, Casagrande K, Barton M, et al. Validation of the Modified Checklist For Autism in Toddlers, Revised with Follow-up (M-CHAT-R/F) Pediatrics. 2014;133(1):37–45. doi: 10.1542/peds.2013-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Learn the signs. Act early. https://www.cdc.gov/ncbddd/actearly/. Accessed March 2, 2017.
- 19.U.S. Census Bureau. Rural-urban continuum codes. 2013 http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed December 15, 2016.
- 20.Guerrero AD, Inkelas M, Whaley SE, et al. A WIC-based curriculum to enhance parent communication with healthcare providers. J Commun Health. 2013;38(5):958–964. doi: 10.1007/s10900-013-9706-9. [DOI] [PubMed] [Google Scholar]
- 21.Early Developmental Screening and Intervention Initiative. Roles for the Women, Infants and Child (WIC) Program in promoting quality developmental care for young children: a report on lessons learned and options. 2011 [Google Scholar]
- 22.Muñoz D, Arriaga RI. Low-income parents’ values involving the use of technology for assessing health information. Proceedings of the International Conference on Human-Computer Interaction (Interact) 2015 [Google Scholar]
- 23.Special Supplemental Nutrition Program for Women, Infants and Children; Subpart A = General Purpose and Scope. 50 Fed Reg 6121 (Feb 13, 1985) (to be codified at 246 C.F.R. pt. 246.1).
- 24.Oregon Health Authority. Oregon Health Authority Measure Sets. http://www.oregon.gov/oha/analytics/CCOData/2016%20Measures.pdf. Accessed Febrary 15, 2017.
- 25.Hughes MP, Joslyn ABA, Wojton M, et al. Connecting vulnerable children and families to community-based programs strengthens parents’ perceptions of protective factors. Infant Young Child. 2016;29(2):116–129. [Google Scholar]


