Abstract
Advances in surgical techniques and laparoscopic instruments have resulted in the development of laparoscopic pancreatic surgery. Total pancreaticoduodenectomy is performed for treating benign and borderline pancreatic disease involving the whole pancreas. Here, we report a case of metastatic renal cell carcinoma in the pancreas, treated by laparoscopic pylorus-preserving total pancreaticoduodenectomy. A 59-year-old woman was diagnosed with metastatic renal cell carcinoma. Multiple metastatic lesions were found on routine follow-up. She had a history of radical video-assisted right-nephrectomy for renal cell carcinoma (conventional type, pT1) in November 2003, without any recurrence. However, in 2014, a routine health checkup revealed multiple enhancing lesions throughout the pancreas. Positron emission tomography showed a suspicious 4-cm lesion in her left thyroid. Laparoscopic pylorus-preserving total pancreaticoduodenectomy with splenectomy was performed, along with simultaneous left total thyroidectomy with central compartment node dissection for metastatic renal cell carcinomas. The total operation time was 441 min, with an estimated blood loss of 150 ml; no transfusion was administered. Her hospital stay was 12 days. The histopath report confirmed metastatic renal cell carcinoma in the pancreas and left thyroid. Based on literature reviews, we further tried to estimate the oncologic outcome of total pancreatectomy in multiple pancreatic metastasis of renal cell carcinoma. Laparoscopic pylorus-preserving total pancreaticoduodenectomy is feasible and safe, even in cases of metastatic renal cell carcinoma.
Keywords: Renal cell carcinoma, Pancreas metastasis, Pancreatectomy, Laparoscopic, Survival
INTRODUCTION
Pancreatic metastases from other primary cancers are uncommon, accounting for less than 5% of pancreatic cancers. Primary cancers reported to metastasize to the pancreas include renal cell carcinoma (RCC), lung cancer, colon cancer, and breast cancer; among these, RCC is the most frequent primary cancer.1 As pancreatic metastases of RCC are usually slow growing, with tumor-free intervals >10 years, they are asymptomatic in more than 50% of cases and are usually incidental findings during long-term follow-ups.2 Although uncommon, when the primary cancer metastasizes only to the pancreas, the pancreatic resection of the isolated metastasis is proven to improve long-term patient survival.3
Here, we report what we believe to be the first case of laparoscopic total pancreatectomy for metastatic cancer from RCC, which occurred 11 years after initial nephrectomy for RCC. In addition, we review the literatures to provide rationales and oncologic insight for total pancreatectomy in multiple pancreatic metastasis of RCC.
CASE
Patient presentation
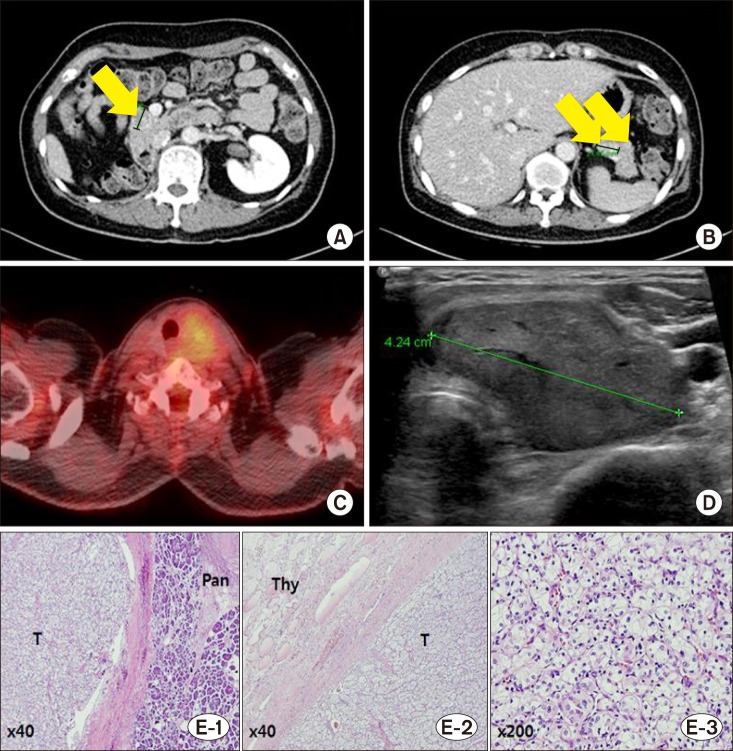
A 59-year-old asymptomatic woman was admitted to our pancreaticobiliary surgery department, for multiple pancreatic lesions incidentally found during a routine follow-up. She had a prior history of radical right nephrectomy for RCC (conventional type, pT1). On a follow-up computed tomography (CT) scan 11 years after her nephrectomy, multiple pancreatic masses suggestive of metastasis from RCC were found, the largest of which were 2.1 cm and 2 cm on the pancreas tail and head, respectively (Fig. 1). Positron emission tomography (PET) with F-18 fluorodeoxyglucose (18-FDG) revealed multiple pancreatic tumors with minimal FDG uptake, as well as a left thyroid tumor with similar FDG uptake as the pancreatic tumors (Fig. 1C). Fine needle aspiration biopsy report was consistent with thyroid metastasis from RCC (Fig. 1D).
Fig. 1. Preoperative computed tomography scans and microscopy images of a metastatic renal cell carcinoma (RCC) in the pancreas and thyroid. Multiple, variable-sized (range, 0.7 cm-2 cm) contrast-enhancing nodules are visible in the pancreas head (A), body and tail (B). An 18-F fluorodeoxyglucose (FDG) positron emission tomography scan shows mild FDG uptake in the left thyroid (C), and a neck ultrasonography scan reveals an approximately 4-cm solid hypoechoic mass in the left thyroid gland (D). Metastatic RCC was confirmed in the pancreas (E-1), and thyroid (E-2). Note the characteristic appearance of RCC with clear cytoplasm arranged in nests (E-3). T, tumor; Pan, pancreas; Thy, thyroid.
Operation
Laparoscopic total pancreatectomy combines laparoscopic pylorus-preserving pancreaticoduodenectomy and laparoscopic subtotal distal pancreatectomy with splenectomy.4,5 Left total thyroidectomy was performed through a 6-cm transverse skin incision on the anterior neck. The operation lasted 7 hours 21 minutes, with an estimated intraoperative blood loss of approximately 150 ml. Pathologic examination revealed multiple nodules in the pancreas, with a maximum size of 1.7 cm×1.1 cm; a 3.7-cm nodule was also found in the left thyroid. Both these nodules were consistent with RCC metastasis (Fig. 1E).
Postoperative course
The patient's postoperative recovery was uneventful. She discharged on postoperative day 12, without complications. During five months of follow-up, there was no evidence of local recurrence or distant metastasis.
Literature review
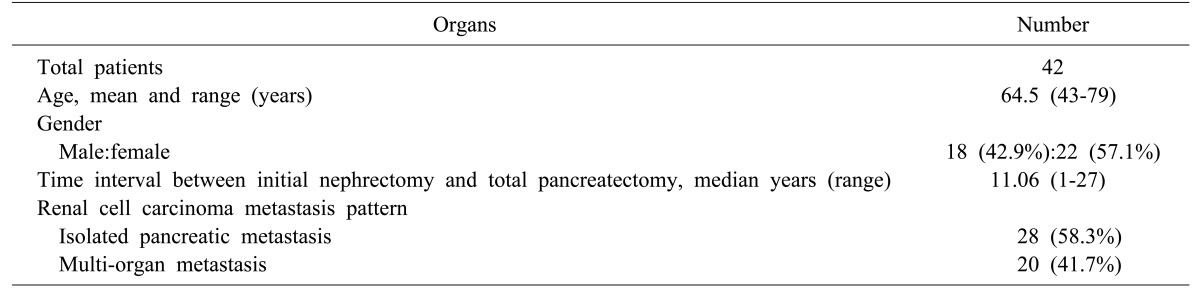
We searched PubMed for reported cases of total pancreatectomy for multiple pancreatic metastasis of RCC, using the keywords “renal cell carcinoma” and “total pancreatectomy”. A total of 30 case reports written in English, describing 50 patients, were identified.1,2,3,6,7,8,9,10,11,12,13,14,15,16,17 Patient demographics and presentations are listed in Table 1. Of note, 28 patients (58.3%) had extrapancreatic multi-organ metastasis of RCC.11,12,13,14,15,16
Table 1. Patient demographics and presentation.
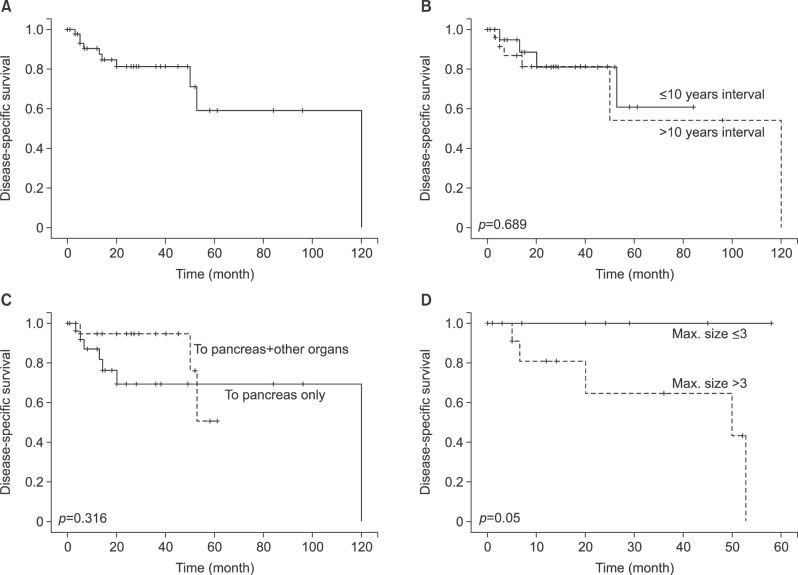
The mean overall disease-specific survival of patients who underwent total pancreatectomy for multiple pancreatic metastasis of RCC was 84.4 months (95% confidential interval [CI]:61.9-106.9) (Fig. 2A). The time interval from initial nephrectomy to total pancreatectomy (within 10 years vs. over 10 years: mean 64.3 months [95% CI: 48.0-80.6] vs. mean 80.1 [95% CI: 43.1-117.1], p=0.689) and metastatic pattern of RCC (pancreas only vs. pancreas+others: mean 86.7 months [95% CI: 62.1-111.4] vs. 53.8 months [95% CI: 47.2-60.6], p=0.316) did not influence oncologic outcomes (Fig. 2B and C). However, analysis revealed that the maximum tumor size influenced the oncologic outcome, and tumor size over 3 cm was associated with adverse oncologic outcomes in patients with total pancreatectomy for multiple pancreatic metastasis (p=0.050, Fig. 2D).
Fig. 2. Literature review-based oncologic outcomes of total pancreatectomy for metastatic renal cell carcinoma, showing overall disease-specific survival (A), and long-term oncologic outcomes according to time interval (10 years) (B), metastasis pattern (C), and maximum tumor size (D).
DISCUSSION
RCC is the most frequent primary cancer metastasizing to the pancreas. Due to the long time interval between primary RCC and metastasis,9 a long-term and meticulous follow-up is required. Literature reviewed by us showed that the median time interval between the primary RCC resection and pancreatic metastasis was 11 years, ranging from 1 to 27 years. In the present case, the multiple pancreatic metastases were identified 11 years after the initial nephrectomy for RCC. The duration to pancreatic metastasis from initial nephrectomy for RCC was not associated with negative oncologic outcomes (Fig. 2B), suggesting that careful follow-up and proper aggressive surgical approach are important in treating multiple pancreatic metastasis of RCC.
We learnt from the current literature review that long-term survival of total pancreatectomy in patients with multiple pancreatic metastasis of RCC was 84.4 months. Compared to oncologic outcomes following surgical resection of multiple hepatic metastasis from colorectal cancer,18 the survival of patients who underwent total pancreatectomy for multiple pancreatic metastasis of RCC appears to be double than those who underwent hepatectomy due to liver metastasis of colon cancer, thus providing an oncologic rationale to favor aggressive surgical intervention even in multiple pancreatic metastasis. Further analysis revealed no significant survival differences with other organ involvement in RCC as well as pancreas (Fig. 2C), supporting our approach of simultaneous thyroidectomy for thyroid metastasis of RCC.
Although kidney cancer was once considered resistant to chemotherapy and radiation therapy,19 recent reports have shown that tyrosine kinase inhibitor-targeted therapy markedly improves the prognosis of patients with metastatic RCC.20 In our study, metastatic RCC larger than 3 cm showed poor prognosis for total pancreatectomy (Fig. 2D).
Our study specifically dealt with several cases of total pancreatectomy due to multiple metastasis of RCC. In addition, the literature review indicated that tumor size less than 3 cm has an adverse effect on oncologic outcomes in patients with total pancreatectomy for metastatic RCC. However, these cases were published from 1972 to 2014 at various centers, and some important clinicopathological variables were not reported. Considering the small patient number, a larger, multi-center study is needed to investigate prognostic factors and rationales of total pancreatectomy in the relevant patient population.
References
- 1.Hijioka S, Hifumi M, Mekky MA, Takekuma Y, Kawaguchi T, Yokomizo H, et al. Total pancreatectomy for metastatic renal cell carcinoma with marked extension into the main pancreatic duct. Intern Med. 2010;49:557–562. doi: 10.2169/internalmedicine.49.2943. [DOI] [PubMed] [Google Scholar]
- 2.Benhaim R, Oussoultzoglou E, Saeedi Y, Mouracade P, Bachellier P, Lang H. Pancreatic metastasis from clear cell renal cell carcinoma: outcome of an aggressive approach. Urology. 2015;85:135–140. doi: 10.1016/j.urology.2014.09.034. [DOI] [PubMed] [Google Scholar]
- 3.Aimoto T, Uchida E, Yamahatsu K, Yoshida H, Hiroi M, Tajiri T. Surgical treatment for isolated multiple pancreatic metastases from renal cell carcinoma: report of a case. J Nippon Med Sch. 2008;75:221–224. doi: 10.1272/jnms.75.221. [DOI] [PubMed] [Google Scholar]
- 4.Choi SH, Hwang HK, Kang CM, Yoon CI, Lee WJ. Pylorus- and spleen-preserving total pancreatoduodenectomy with resection of both whole splenic vessels: feasibility and laparoscopic application to intraductal papillary mucin-producing tumors of the pancreas. Surg Endosc. 2012;26:2072–2077. doi: 10.1007/s00464-011-2113-3. [DOI] [PubMed] [Google Scholar]
- 5.Kim DH, Kang CM, Lee WJ. Laparoscopic-assisted spleen-preserving and pylorus-preserving total pancreatectomy for main duct type intraductal papillary mucinous tumors of the pancreas: a case report. Surg Laparosc Endosc Percutan Tech. 2011;21:e179–e182. doi: 10.1097/SLE.0b013e31821e9e2d. [DOI] [PubMed] [Google Scholar]
- 6.Alzahrani MA, Schmulewitz N, Grewal S, Lucas FV, Turner KO, McKenzie JT, et al. Metastases to the pancreas: the experience of a high volume center and a review of the literature. J Surg Oncol. 2012;105:156–161. doi: 10.1002/jso.22009. [DOI] [PubMed] [Google Scholar]
- 7.Chang YH, Liaw CC, Chuang CK. The role of surgery in renal cell carcinoma with pancreatic metastasis. Biomed J. 2015;38:173–176. doi: 10.4103/2319-4170.137771. [DOI] [PubMed] [Google Scholar]
- 8.Hatori T, Kimijima A, Fujita I, Furukawa T, Yamamoto M. Duodenum-preserving total pancreatectomy for pancreatic neoplasms. J Hepatobiliary Pancreat Sci. 2010;17:824–830. doi: 10.1007/s00534-009-0225-0. [DOI] [PubMed] [Google Scholar]
- 9.Hiotis SP, Klimstra DS, Conlon KC, Brennan MF. Results after pancreatic resection for metastatic lesions. Ann Surg Oncol. 2002;9:675–679. doi: 10.1007/BF02574484. [DOI] [PubMed] [Google Scholar]
- 10.Jovine E, Biolchini F, Cuzzocrea DE, Lazzari A, Martuzzi F, Selleri S, et al. Spleen-preserving total pancreatectomy with conservation of the spleen vessels:: operative technique and possible indications. Pancreas. 2004;28:207–210. doi: 10.1097/00006676-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Kanai T, Aoki A, Okazeri S, Shimada H, Masamura S, Saikawa Y, et al. Successful aggressive treatment against multiple intra-abdominal metastases from renal cell carcinoma 18 years after nephrectomy. Jpn J Clin Oncol. 1992;22:216–220. [PubMed] [Google Scholar]
- 12.Kassabian A, Stein J, Jabbour N, Parsa K, Skinner D, Parekh D, et al. Renal cell carcinoma metastatic to the pancreas: a single-institution series and review of the literature. Urology. 2000;56:211–215. doi: 10.1016/s0090-4295(00)00639-7. [DOI] [PubMed] [Google Scholar]
- 13.Law CH, Wei AC, Hanna SS, Al-Zahrani M, Taylor BR, Greig PD, et al. Pancreatic resection for metastatic renal cell carcinoma: presentation, treatment, and outcome. Ann Surg Oncol. 2003;10:922–926. doi: 10.1245/aso.2003.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Minni F, Casadei R, Perenze B, Greco VM, Marrano N, Margiotta A, et al. Pancreatic metastases: observations of three cases and review of the literature. Pancreatology. 2004;4:509–520. doi: 10.1159/000080248. [DOI] [PubMed] [Google Scholar]
- 15.Niess H, Conrad C, Kleespies A, Haas F, Bao Q, Jauch KW, et al. Surgery for metastasis to the pancreas: is it safe and effective? J Surg Oncol. 2013;107:859–864. doi: 10.1002/jso.23333. [DOI] [PubMed] [Google Scholar]
- 16.Schauer M, Vogelsang H, Siewert JR. Pancreatic resection for metastatic renal cell carcinoma: a single center experience and review of the literature. Anticancer Res. 2008;28:361–365. [PubMed] [Google Scholar]
- 17.Tuech JJ, Lefebure B, Bridoux V, Albouy B, Lermite E, Le Pessot F, et al. Combined resection of the pancreas and inferior vena cava for pancreatic metastasis from renal cell carcinoma. J Gastrointest Surg. 2008;12:612–615. doi: 10.1007/s11605-007-0295-8. [DOI] [PubMed] [Google Scholar]
- 18.Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–722. doi: 10.1097/01.sla.0000160703.75808.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kothari G, Foroudi F, Gill S, Corcoran NM, Siva S. Outcomes of stereotactic radiotherapy for cranial and extracranial metastatic renal cell carcinoma: a systematic review. Acta Oncol. 2015;54:148–157. doi: 10.3109/0284186X.2014.939298. [DOI] [PubMed] [Google Scholar]
- 20.Larkin J, Paine A, Foley G, Mitchell S, Chen C. First-line treatment in the management of advanced renal cell carcinoma: systematic review and network meta-analysis. Expert Opin Pharmacother. 2015;16:1915–1927. doi: 10.1517/14656566.2015.1058359. [DOI] [PubMed] [Google Scholar]