Abstract
Inflammatory bowel disease (IBD) is a heterogeneous group of chronic diseases with a rising prevalence in the pediatric population, and up to 25% of IBD patients are diagnosed before 18 years of age. Adolescents with IBD tend to have more severe and extensive disease and eventually require graduation from pediatric care toadult services. The transition of patients from pediatric to adult gastroenterologists requires careful preparation and coordination, with involvement of all key players to ensure proper collaboration of care and avoid interruption in care. This can be challenging and associated with gaps in delivery of care. The pediatric and adult health paradigms have inherent differences between health care models, as well as health care priorities in IBD. The readiness of the young adult also influences this transition of care, with often times other overlaps in life events, such as school, financial independence and moving away from home. These patients are therefore at higher risk for poorer clinical disease outcomes. The aim of this paper is to review concepts pertinent to transition of care of young adults with IBD to adult care, and provides resources appropriate for an IBD pediatric to adult transition of care model.
Keywords: Inflammatory bowel disease, Adolescents, Young adults, Transition care, Transition to adult care
Core tip: The process of transition of a young adult with inflammatory bowel disease (IBD) to adult care should be well coordinated and incorporate all key players to ensure proper collaboration and avoid interruption in care. An early, regular assessment of the adolescent readiness for transition is important. The adolescent patient should be seen without the parent or caregivers in order to build self-reliance. Pediatric gastroenterologists need to discuss and introduce the concept of transition with the patient and family early and identify adult gastroenterologists with unique interests in young adults with IBD. The adult gastroenterologist should be prepared for the transition with advanced communication with the referring pediatric team, consider further training in adolescent health, and review health priorities and targets of care early with the young adult.
INTRODUCTION
Inflammatory bowel disease (IBD) is a heterogeneous group of diseases that includes both ulcerative colitis (UC) and Crohn’s disease (CD). In the United States, nearly 1.5 million Americans are affected by this chronic disease, and approximately 30% of CD and 20% of UC patients have disease onset prior to the age of 20[1,2]. Population-based studies demonstrate a rising incidence of pediatric IBD over the last decade and the projected prevalence of pediatric onset of disease is about 10000 new cases annually[2,3].
Similar to other chronic diseases such as cystic fibrosis (CF) and diabetes, children with IBD eventually require a transfer of care to an adult gastroenterologist. This transition from pediatric to adult care carries potential challenges, given the inherent differences between pediatric and adult health care models, disease characteristics and phenotype, and treatment strategies. There are two key elements to this healthcare transition. One is the transition of care from the primary caregiver or guardian to the patient, and the other is the transfer of responsibility from the pediatric gastroenterologist to an adult provider[4]. Without both elements, the process of transition will inevitably fail and result in poorer patient and disease outcomes.
This paper highlights the need for a structured transition process for IBD patients that graduate from pediatric to adult gastroenterology care and provides an overview of this process.
DIFFERENCES IN PEDIATRIC AND ADULT HEALTH CARE MODELS
The pediatric healthcare model is family-focused and requires parental involvement for knowledge, understanding, guidance and consent[5,6]. Pediatric specialists have also received baseline training in pediatric care and are appropriately sensitive to child-specific psychosocial needs. The delivery of care is usually designed to include a multi-disciplinary team of providers and medical staff.
Conversely, the adult care model promotes independence and individualized care[5,6]. Medical care is often carried out by a single provider. The focus of care is on the disease, with less attention on growth and puberty, and psychological development. The familiarity of the adult subspecialists on adolescent developmental milestones and its impact on disease is often limited.
Alongside these differences in models of health care, the pediatric patient is often also involved in other transitions, including possible graduation, new employment, financial independence, and moving away from family and home. These potential overlapping events may also affect health care models, including sudden new and unfamiliar assignment to a local adult healthcare provider, less oversight by caregiver or parent, economic barriers and access to healthcare and pharmacological therapies, and possible noncompliance or adherence to treatment.
DIFFERENCES IN PEDIATRIC AND ADULT INFLAMMATORY BOWEL DISEASE
There are reported differences in pediatric and adult disease phenotype and behavior. Goodhand and colleagues[7] conducted a retrospective case-control of 100 adolescents matched with 100 adults with IBD, and described a more complex and aggressive disease phenotype among the adolescents. Specifically, adolescents with IBD were more likely to have extensive CD with ileocolonic involvement as compared to adults with disease restricted to only ileum or colon alone (69% vs 28%). Adolescents were also more likely to have perianal disease as compared to adults, 33% vs 16%. There was a higher incidence of pancolitis among adolescents with UC (67%) as compared to adults (39%) who had disease limited mostly to the left colon. There were also differences in therapies, with adolescents more likely than adults to require immunomodulator therapy (53% vs 13%) and biologic agents (20% vs 8%), which also suggests more severe disease.
Vernier-Massouille et al[8] described the natural history of patients with pediatric onset of disease and found that these patients were more likely to have upper gastrointestinal involvement, extraintestinal manifestations, and higher risk for steroid dependence and stricturing and penetrating disease. Among the pediatric IBD patients, 44% required surgery at some point from the time of diagnosis, with a 34% risk within the first 5 years of diagnosis. Adolescents were also more likely to require hospital admission (14%-46%) and more likely to miss appointments (0-20%) compared to adults[7]. Hartman and colleagues reported that nutritional impairment and weight loss occurred in up to 85% of IBD children, which further affects patient growth and development[9].
Mental health disorders are also more common and there is a lowered self-esteem, increased depression and anxiety, behavioral problems, body image distortion, and impaired social competence described among adolescents diagnosed with IBD[10]. In a meta-analysis review, Greenley et al[11] described higher rates of depressive disorders among young IBD patients compared to other chronic conditions. The negative impact of depression and anxiety on medical adherence has also been well described[12].
Because of the more severe disease phenotype, need of chronic medications and multiple psychomedical co-morbidities such as malnutrition, delayed growth, and underlying depression or anxiety, there needs to be uninterrupted care and management of IBD as the move toward adulthood is made, to ensure improved outcomes.
TRANSITION OF CARE IN OTHER CHRONIC DISEASES
Transition of care should not be mistaken by a simple transfer of care, which is a “planned movement of patient and their medical records from one provider to another at a distinct point in time”[13]. The transition of care is a “purposeful planned movement of adolescents and young adults with chronic physical and medical conditions from child-centered to adult-oriented health care systems”[14]. The transition process should be well-coordinated and incorporate all key players to ensure proper collaboration and avoid interruption in care. Unlike a transfer, which is a single event, the transition is a gradual process that allows the young adult to acquire behavioral skills and knowledge to assume full responsibility for their health care needs and management of their disease.
The medical providers that are involved should understand the rationale for the transition process, have the knowledge and skills to facilitate this process, and also know when the transition is indicated. Because the transition period is a vulnerable time, it is important to have a structured program in place, which can have a positive effect on the clinical and medical, as well as psychological outcomes for the patient.
There are several examples of transition of care with other chronic diseases, such as cystic fibrosis (CF), type 1 diabetes and congenital heart disease. Pediatricians have long been aware of the need and challenges of ensuring that CF patients receive appropriate services as they move into adult care. CF pediatricians and other medical providers have been leaders in the development of models for transitional care for over 20 years[15]. Examples of different CF-transition models include: CF-trained pediatrician to continue to provide the health service for life; pediatrician to transfer the care to adult physicians at “CF centers”; and lastly the pediatrician to transfer the care to both a designated local chest physician and with joint care at a designated CF center[15]. Regardless of the adopted model, the transition process is made clear to the patient and the provided care is appropriate for the needs of the patient. There is convincing evidence of improved survival of CF patients, despite no medical cure, and attributed in part to the improvement and proactive care provided during childhood and with the appropriate, purposeful transition to adult care[15].
Similarly, among young adults with type 1 diabetes mellitus who underwent a structured transition of care as opposed to those only referred to an adult care provider by a referral letter or simple transfer, had improved attendance in clinic and hemoglobin A1c (HbA1c) levels[16].
TRANSITION OF CARE IN INFLAMMATORY BOWEL DISEASE
Emerging adulthood, defined as the first period of adult life from age 18 to 25, is often considered an unstable period between adolescence and full adulthood[13]. In IBD, as with other chronic diseases, “emerging adulthood” may be a longer period of time by default of the chronic disease. The emotional dynamics of the chronic disease and close dependence (excessive or appropriate) could contribute to the adolescents’ difficulty progressing to the age appropriate emotional maturity and independence. The emerging adults with IBD (EAI) coined by Trivedi and Keefer[13], have an increased risk for disease progression, including stricturing and penetrating disease, and other complications of disease[17]. Studies have also demonstrated a higher economic burden among EAIs, including increased all-cause total health care costs in both UC and CD[18,19] as well as the highest utilization of emergency services of any adult sub-population[20]. Poorer adherence to treatment plans and attendance to clinic visits are also reported to be the lowest among EAIs[21].
Although there are several described models of transition of care in IBD implemented in clinics in the United States and other Westernized countries, an ideal model for a structured transition program in IBD has yet to be defined. There is also suggestion that a “transition program may either be a physical clinic with a dedicated, multidisciplinary group of care providers or a conceptual element of the care provided in a more traditional clinic setting”[4].
Hait et al[6] conducted a survey of adult gastroenterologists to determine which patient competencies are necessary for a successful transition to an adult practice. The study concluded that adult providers have identified a deficiency in the young adults’ knowledge of disease, medical history and medications, and also reported that pediatric gastroenterologists need to improve communication with patients and referring providers. Less than half of the adult gastroenterologists in the survey reported competency with adolescent developmental and mental health issues, despite 89% who believed this was important. The study also concluded that adult gastroenterologists may benefit from additional formalized training in adolescent issues.
A United Kingdom study[22] of adult and pediatric gastroenterologists surveyed to identify the needs of adolescents with IBD and barriers to a successful transition, concluded that 80% of pediatric providers were more likely to consider a structured transition process to be very important, as compared to 47% among adult providers (P = 0.001). Similar to the prior study, more adult vs pediatric gastroenterologists identified deficiencies in preparation of adolescents for transition of care, including lack of disease knowledge about disease condition and treatments (79% vs 42% respectively, P = 0.001).
Trivedi and Keefer[13] describe three primary adult provider skill sets for the care of an EAI patient, which includes: “(1) understand the natural history, disease phenotype, complications and treatment options for IBD; (2) appreciate nutrition, growth, and radiation exposure concerns; and (3) recognize the convergence and divergence of traditional pediatric and adult care models in IBD”. The authors also describe “expanded skill sets” which is crucial in the care and management of EAIs, and incorporates a good understanding of adverse effects of IBD treatments, implications of disease and therapies on sexual, fertility and reproductive systems, issues related to unemployment and disability, and understanding of health insurance and coverage plans[13].
ORGANIZING A TRANSITION PROGRAM IN INFLAMMATORY BOWEL DISEASE
The North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) has published recommendations regarding the transition of patients with childhood onset of IBD to adult care[23]. The NASPGHAN recommendation to the pediatric gastroenterologist is to begin the process of transition when the patient enters early to middle adolescence and: (1) see the adolescent patient without their parents or caregivers in order to build independence and self-reliance; (2) discuss and introduce the subject and the benefits of a transition to an adult gastroenterologist early on to the patient and family; (3) select an experienced adult gastroenterologist knowledgeable and interested in the unique needs of young adults with IBD; and (4) provide all appropriate medical records and summaries to the adult gastroenterologist in advance, to ensure confidence in the patient and family that the pediatric and adult providers are working together. The NASPGHAN Medical Summary Form can be found in Appendix A of this medical position statement[23].
Acquiring the skills necessary for transitioning to the adult setting should also not be limited to a single encounter and therefore a healthcare transition plan is needed. NASPGHAN has created a “Healthcare Provider Transitioning Checklist” for patients and providers that can be utilized to help evaluate the readiness of the adolescents to transition of care. It also provides information to the healthcare provider to better understand these goals and improve ways to help the adolescent best achieve appropriate readiness for transition. It is recommended that the process begins in early adolescence, age 12-14 years[24].
A regular assessment of the adolescent readiness for transition is important. These assessments help identify areas where the adolescent may need further disease education to achieve independence and competence in transition-relevant skills.
The evaluation of readiness is difficult to measure and there have been several clinical instruments used to guide this process. One example is the Transition Readiness Assessment Questionnaire (TRAQ)[25], which is a patient-reported assessment of health and skills needed for management of medications, tracking health issues and talking with healthcare providers. Benchimol et al[26] also developed a portable medical record for the patient called the MyHealth Passport for IBD, which allows patients and parents to answer questions about disease course, medical and treatment history. Both TRAQ and MyHealth Passport for IBD are available online for download and can be utilized in clinic and provided to all patients.
Morisky et al[27] Adherence Scale may also be used as a clinical instrument tool to identify patients with potential adherence problems. It can be used to monitor treatment adherence once therapies are initiated, as well as identify or address any potential adherence problems early and guide health care providers to provide reinforcement and clinical advice for better outcomes.
Seattle Children’s Hospital Inflammatory Bowel Disease Center recently developed a readiness tool for the Pediatric-to-Adult IBD Transition Clinic. This form is available through the electronic medical record system and can be printed out at the time of the clinic encounter. The form contains separate age appropriate lists of questions to the adolescent patient, all pertaining to their diagnosis, treatment plan and general knowledge about IBD and patient’s individual health care access. The goal of the structured interaction between the IBD team member and the patient is to emphasize the importance of knowing these answers firsthand and prepares the patient for the next age appropriate list of questions on future visits.
Lastly, the PHQ-9 Depression Screening Tool[28] is also another useful instrument that has incorporated the DSM-IV diagnostic criteria for depression and can be applied in clinic along with the transition readiness and adherence tools. Based on the severity score, treatment recommendations and appropriateness for anti-depressants, psychotherapy or support alone can be considered.
The transition of care is usually undertaken after completion of the developmental milestones and appropriate assessment for readiness of the adolescent. This is usually a transition target age of 18 or 19. The transition of care is not usually recommended when the adolescent is hospitalized or with acute bowel disease flare, but rather when the young adult is able to manage his or her disease largely independent of caregivers and professional staff, and is overall at baseline or stable with their disease and current treatment or management of disease. Certainly, there are exceptions to this particularly when the EAI has medical refractory disease and warrants special consideration such as enrollment into a clinical trial or options of treatment not yet FDA-approved for pediatric patients. Hait et al[29] describe a suggested timeline, noting that this process is not a “rigid protocol” but rather a process that requires tailoring based on the developmental abilities of the adolescent and is more based on emotional and cognitive maturity and competency as opposed to chronological age alone.
IDENTIFICATION OF KEY PLAYERS OR STAKEHOLDERS IN THE TRANSITION OF CARE
The transition of care involves multiple stakeholders invested in their respective roles in a seamless continuation of the adolescent’s health care (Figure 1). Recognizing the important roles of the key players in this multidisciplinary team and enhancing timely communication between them is essential.
Figure 1.
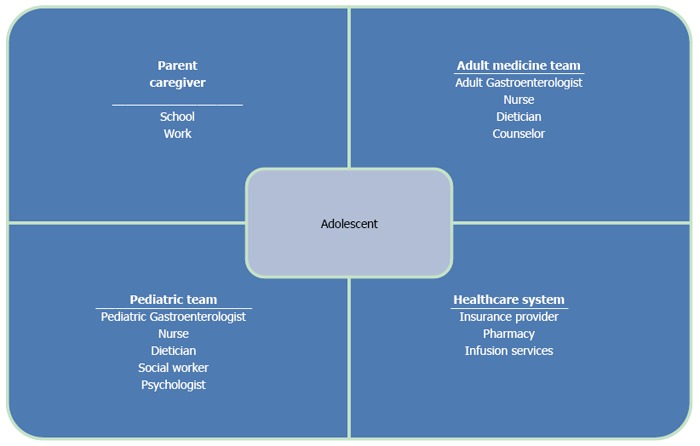
Transition of care involves multiple stakeholders invested.
GOALS AND BARRIERS IN THE PRACTICE FOR A SUCCESSFUL TRANSITION OF CARE
Escher JC identified three goals in the process of transition in IBD: “(1) to get the patient ready for transfer, having attained specific skills and knowledge; (2) to get the parents ready for transfer; and (3) to get the adult gastroenterologist ready and well informed at the time of transfer”[30].
The Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART) developed and validated by Schwartz and colleagues[31,32] has identified seven major inter-related components of patients, parents and providers which impacts transition readiness and potential targets of intervention including: patient development, knowledge, skills/efficacy to managing health, beliefs/expectations of the transition process, transition goals, relationships among patients, parents and providers, and psychosocial functioning regarding conditions and emotions related to the transition process; as well as pre-existing factors which are less modifiable but may still influence the transition process including socio-demographics/culture, insurance/access, health status, risks and problems due to complications of disease, and neurocognition/IQ. These components are either barriers or facilitators of a successful transition of care and further validated in a different study that described that SMART components including patient developmental maturity, parental involvement and degree of provider support influenced the success of transition of care and outcomes that included healthcare utilization, health and quality of life[33].
Achieving the goals of a successful transition of care program may be difficult due to limitations of resources or access to clinics with a structured program, poor readiness or preparation for the young adult to transition, limited communication between the referring pediatric gastroenterologists to the receiving adult providers, and suboptimal training in adolescent medicine for adult gastroenterologists[4,22,34-38].
Other factors may also impede the success of IBD transition of care. As we assess and track the readiness of the patient for the transition, there may be reluctance by parent, caregiver or even the pediatric gastroenterology team. This reluctance or inability to “let go” by other key players involved in this process certainly also impacts the transition.
Because there is no standardized age for transition of care, a heterogeneity in milestones achieved by the young adult, such as high school or college graduation, vocation, employment, marriage or pregnancy to name a few, may also impact the transition process. A lack of IBD centers and few adult gastroenterologists in the local area with special interests in the care and management of IBD patients is another barrier towards a successful transition of care for a young adult. Leung and colleagues summarized practical guidelines to aide not only adolescents through the transition process, but recommendations were also outlined for both pediatric and adult gastroenterologists even when a structured IBD transition clinic is unavailable[39].
Early preparation and good communication is essential in the transition process, but despite this, another limitation is the differences in health priorities among all key stakeholders[40]. These differences in priorities or targets of care needs to be identified and discussed early in the transition in order to help both the EAI and the adult gastroenterologist understand and best achieve them. It is also important to acknowledge that healthcare goals such as achieving clinical and mucosal remission, dysplasia surveillance and preventative health care, are usually different than pediatric care goals such as psychosocial development, growth and nutrition[13]. A close professional and educational relationship between pediatric and adult IBD providers is key to understanding the various management goals, priorities and perhaps “styles” of practice, along the adolescent’s continuum of IBD care.
Lastly, the variation in health care systems and access of care in the United States and other countries further complicates this process. Among both adult and pediatric gastroenterologists, lack of funding, time, support of services, training and too few of IBD transition of care patients were the top five obstacles experienced in their local setting which impacted the ability to deliver transition of care services[22].
There are also additional logistical issues during the transition process and questions of concern include: Who is in charge for the management of the patient in transition? Where should the transition clinic be established - the pediatric or adult clinic? When can multiple providers all be available to meet with the patient and parents/caregivers at the same time? Finally, which gastroenterologist, pediatric or adult, can bill for the clinic visit?
CONCLUSION
As we begin to consider IBD as a disease that begins in childhood and continues into adulthood, we face the same challenges for transitioning of care as other chronic diseases. This is a process that requires careful coordination and collaboration from key stakeholders of a multidisciplinary team including first and foremost the patient, as well as parents/caregiver and providers. Although a number of transition clinic models currently exist, there is paucity of data and gap in knowledge for the care and management of this vulnerable young population. The developmental maturity and core competency of the EAI, early preparation and good communication by the pediatrician and an expanded skill set and training for the adult gastroenterologist will allow for a smoother transition and best impact clinical outcomes.
Larger, prospective studies are needed to help standardize transition care practices. Data-driven assessment of strategies aimed to optimize competency and development, communication, education, and adherence will ultimately help improve clinical outcomes in the IBD transition of care.
ACKNOWLEDGMENTS
The authors would like to acknowledge Teresa Wachs RN, CCM, BC for her tremendous dedication, support, advocacy and care of our Transition of Care patients, as well as her contribution in the development of the Seattle Children’s Hospital IBD Readiness Tool for the Pediatric to Adult Transition Clinic.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The authors declare that there are no conflicts of interests regarding the publication of this paper.
Peer-review started: February 1, 2017
First decision: March 19, 2017
Article in press: May 4, 2017
P- Reviewer: Gow KW, Lakatos PL, Sangkhathat S S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
References
- 1.Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.e42; quiz e30. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Kelsen J, Baldassano RN. Inflammatory bowel disease: the difference between children and adults. Inflamm Bowel Dis. 2008;14 Suppl 2:S9–11. doi: 10.1002/ibd.20560. [DOI] [PubMed] [Google Scholar]
- 3.Malaty HM, Fan X, Opekun AR, Thibodeaux C, Ferry GD. Rising incidence of inflammatory bowel disease among children: a 12-year study. J Pediatr Gastroenterol Nutr. 2010;50:27–31. doi: 10.1097/MPG.0b013e3181b99baa. [DOI] [PubMed] [Google Scholar]
- 4.Philpott JR. Transitional care in inflammatory bowel disease. Gastroenterol Hepatol (N Y) 2011;7:26–32. [PMC free article] [PubMed] [Google Scholar]
- 5.Bollegala N, Nguyen GC. Transitioning the Adolescent with IBD from Pediatric to Adult Care: A Review of the Literature. Gastroenterol Res Pract. 2015;2015:853530. doi: 10.1155/2015/853530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hait EJ, Barendse RM, Arnold JH, Valim C, Sands BE, Korzenik JR, Fishman LN. Transition of adolescents with inflammatory bowel disease from pediatric to adult care: a survey of adult gastroenterologists. J Pediatr Gastroenterol Nutr. 2009;48:61–65. doi: 10.1097/MPG.0b013e31816d71d8. [DOI] [PubMed] [Google Scholar]
- 7.Goodhand J, Dawson R, Hefferon M, Tshuma N, Swanson G, Wahed M, Croft NM, Lindsay JO. Inflammatory bowel disease in young people: the case for transitional clinics. Inflamm Bowel Dis. 2010;16:947–952. doi: 10.1002/ibd.21145. [DOI] [PubMed] [Google Scholar]
- 8.Vernier-Massouille G, Balde M, Salleron J, Turck D, Dupas JL, Mouterde O, Merle V, Salomez JL, Branche J, Marti R, et al. Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology. 2008;135:1106–1113. doi: 10.1053/j.gastro.2008.06.079. [DOI] [PubMed] [Google Scholar]
- 9.Hartman C, Eliakim R, Shamir R. Nutritional status and nutritional therapy in inflammatory bowel diseases. World J Gastroenterol. 2009;15:2570–2578. doi: 10.3748/wjg.15.2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mackner LM, Crandall WV, Szigethy EM. Psychosocial functioning in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:239–244. doi: 10.1097/01.MIB.0000217769.83142.c6. [DOI] [PubMed] [Google Scholar]
- 11.Greenley RN, Hommel KA, Nebel J, Raboin T, Li SH, Simpson P, Mackner L. A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J Pediatr Psychol. 2010;35:857–869. doi: 10.1093/jpepsy/jsp120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray WN, Denson LA, Baldassano RN, Hommel KA. Treatment adherence in adolescents with inflammatory bowel disease: the collective impact of barriers to adherence and anxiety/depressive symptoms. J Pediatr Psychol. 2012;37:282–291. doi: 10.1093/jpepsy/jsr092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trivedi I, Keefer L. The Emerging Adult with Inflammatory Bowel Disease: Challenges and Recommendations for the Adult Gastroenterologist. Gastroenterol Res Pract. 2015;2015:260807. doi: 10.1155/2015/260807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, Slap GB. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- 15.Hewer SC, Tyrrell J. Cystic fibrosis and the transition to adult health services. Arch Dis Child. 2008;93:817–821. doi: 10.1136/adc.2008.143578. [DOI] [PubMed] [Google Scholar]
- 16.Cadario F, Prodam F, Bellone S, Trada M, Binotti M, Trada M, Allochis G, Baldelli R, Esposito S, Bona G, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 2009;71:346–350. doi: 10.1111/j.1365-2265.2008.03467.x. [DOI] [PubMed] [Google Scholar]
- 17.Louis E. Epidemiology of the transition from early to late Crohn’s disease. Dig Dis. 2012;30:376–379. doi: 10.1159/000338129. [DOI] [PubMed] [Google Scholar]
- 18.Bickston SJ, Waters HC, Dabbous O, Tang BI, Rahman M. Administrative claims analysis of all-cause annual costs of care and resource utilization by age category for ulcerative colitis patients. J Manag Care Pharm. 2008;14:352–362. doi: 10.18553/jmcp.2008.14.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kappelman MD, Rifas-Shiman SL, Porter CQ, Ollendorf DA, Sandler RS, Galanko JA, Finkelstein JA. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135:1907–1913. doi: 10.1053/j.gastro.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Trends in ambulatory and emergency room visits for inflammatory bowel diseases in the United States: 1994-2005. Am J Gastroenterol. 2010;105:363–370. doi: 10.1038/ajg.2009.580. [DOI] [PubMed] [Google Scholar]
- 21.Goodhand J, Hedin CR, Croft NM, Lindsay JO. Adolescents with IBD: the importance of structured transition care. J Crohns Colitis. 2011;5:509–519. doi: 10.1016/j.crohns.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 22.Sebastian S, Jenkins H, McCartney S, Ahmad T, Arnott I, Croft N, Russell R, Lindsay JO. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: differing perceptions from a survey of adult and paediatric gastroenterologists. J Crohns Colitis. 2012;6:830–844. doi: 10.1016/j.crohns.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 23.Baldassano R, Ferry G, Griffiths A, Mack D, Markowitz J, Winter H. Transition of the patient with inflammatory bowel disease from pediatric to adult care: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2002;34:245–248. doi: 10.1097/00005176-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 24.NASPGHAN North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Inflammatory Bowel Disease Monographs. Healthcare Provider Checklist for Transitioning a Patient from Pediatric to Adult Care. Accessed website February 09 2015. Available from: http://www.naspghan.org/files/documents/pdfs/medical-resources/ibd/Checklist_PatientandHealthcareProdiver_TransitionfromPedtoAdult.pdf.
- 25.Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, Ferris M, Kraemer DF. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14:415–422. doi: 10.1016/j.acap.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Benchimol EI, Walters TD, Kaufman M, Frost K, Fiedler K, Chinea Z, Zachos M. Assessment of knowledge in adolescents with inflammatory bowel disease using a novel transition tool. Inflamm Bowel Dis. 2011;17:1131–1137. doi: 10.1002/ibd.21464. [DOI] [PubMed] [Google Scholar]
- 27.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hait E, Arnold JH, Fishman LN. Educate, communicate, anticipate-practical recommendations for transitioning adolescents with IBD to adult health care. Inflamm Bowel Dis. 2006;12:70–73. doi: 10.1097/01.mib.0000194182.85047.6a. [DOI] [PubMed] [Google Scholar]
- 30.Escher JC. Transition from pediatric to adult health care in inflammatory bowel disease. Dig Dis. 2009;27:382–386. doi: 10.1159/000228578. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37:883–895. doi: 10.1111/j.1365-2214.2011.01282.x. [DOI] [PubMed] [Google Scholar]
- 32.Schwartz LA, Brumley LD, Tuchman LK, Barakat LP, Hobbie WL, Ginsberg JP, Daniel LC, Kazak AE, Bevans K, Deatrick JA. Stakeholder validation of a model of readiness for transition to adult care. JAMA Pediatr. 2013;167:939–946. doi: 10.1001/jamapediatrics.2013.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paine CW, Stollon NB, Lucas MS, Brumley LD, Poole ES, Peyton T, Grant AW, Jan S, Trachtenberg S, Zander M, et al. Barriers and facilitators to successful transition from pediatric to adult inflammatory bowel disease care from the perspectives of providers. Inflamm Bowel Dis. 2014;20:2083–2091. doi: 10.1097/MIB.0000000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zeisler B, Hyams JS. Transition of management in adolescents with IBD. Nat Rev Gastroenterol Hepatol. 2014;11:109–115. doi: 10.1038/nrgastro.2013.254. [DOI] [PubMed] [Google Scholar]
- 35.Wright EK, Williams J, Andrews JM, Day AS, Gearry RB, Bampton P, Moore D, Lemberg D, Ravikumaran R, Wilson J, et al. Perspectives of paediatric and adult gastroenterologists on transfer and transition care of adolescents with inflammatory bowel disease. Intern Med J. 2014;44:490–496. doi: 10.1111/imj.12402. [DOI] [PubMed] [Google Scholar]
- 36.Fishman LN, Ziniel SI, Adrichem ME, Fernandes SM, Arnold J. Provider awareness alone does not improve transition readiness skills in adolescent patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2014;59:221–224. doi: 10.1097/MPG.0000000000000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gray WN, Holbrook E, Morgan PJ, Saeed SA, Denson LA, Hommel KA. Transition readiness skills acquisition in adolescents and young adults with inflammatory bowel disease: findings from integrating assessment into clinical practice. Inflamm Bowel Dis. 2015;21:1125–1131. doi: 10.1097/MIB.0000000000000352. [DOI] [PubMed] [Google Scholar]
- 38.Abraham BP, Kahn SA. Transition of Care in Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y) 2014;10:633–640. [PMC free article] [PubMed] [Google Scholar]
- 39.Leung Y, Heyman MB, Mahadevan U. Transitioning the adolescent inflammatory bowel disease patient: guidelines for the adult and pediatric gastroenterologist. Inflamm Bowel Dis. 2011;17:2169–2173. doi: 10.1002/ibd.21576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cervesi C, Battistutta S, Martelossi S, Ronfani L, Ventura A. Health priorities in adolescents with inflammatory bowel disease: physicians’ versus patients’ perspectives. J Pediatr Gastroenterol Nutr. 2013;57:39–42. doi: 10.1097/MPG.0b013e31828b5fd4. [DOI] [PubMed] [Google Scholar]


