Abstract
Objective To investigate the difficulties doctors face in discussing treatment options with patients with acute, life threatening illness and major comorbidities.
Design Observational study of doctor-patient interviews based on a standardised clinical scenario involving high risk surgery in a hypothetical patient (played by an actor) with serious comorbidities.
Participants 30 trainee doctors 3-5 years after graduation.
Main outcome measures Adequacy of coverage of various aspects was scored from 3 (good) to 0 (not discussed).
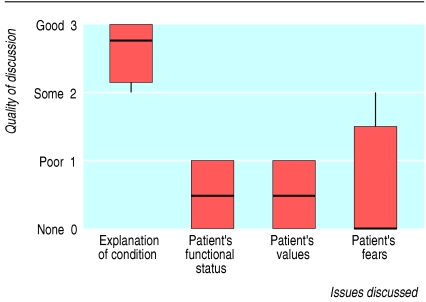
Results The medical situation was considered to be well described (median score 2.7 (interquartile range 2.1-3.0)), whereas the patient's functional status, values, and fears were poorly or minimally addressed (scores 0.5 (0.0-1.0), 0.5 (0.0-1.0), and 0.0 (0.0-1.5), respectively; all P < 0.001 v score for describing the medical situation). Twenty nine of the doctors indicated that they wished to include the patient's family in the discussion, but none identified a preferred surrogate decision maker. Six doctors suggested that the patient alone should speak with his family to reach a decision without the doctor being present. The doctors were reluctant to give advice, despite it being directly requested: two doctors stated that a doctor could not give advice, while 17 simply restated the medical risks, without advocating any particular course. Of the 11 who did offer advice, eight advocated intervention.
Conclusions Doctors focused on technical medical issues and placed much less emphasis on patient issues such as functional status, values, wishes, and fears. This limits doctors' ability to offer suitable advice about treatment options. Doctors need to improve their communication skills in this difficult but common clinical situation.
Introduction
Doctors are increasingly confronted by major, life threatening illness in patients who have serious comorbidities. Decision making in these circumstances poses major difficulties, and doctors perceive that they are poorly prepared for this task.1 The task is made harder by the need to reach decisions about an acute illness or crisis quickly, often within minutes, and by the probability that the doctor who must make the decision has never previously met the patient.
The choices are usually stark. Withholding treatment almost always results in the patient's death (although not always quickly), while intervention is likely to result in considerable complications and a protracted course, often culminating in death. Neither option represents a good or obvious choice. Withholding treatment without the agreement of a patient or relatives is liable to generate complaint, but mentioning a treatment that the doctor may feel to be inappropriate may encourage patients and families to demand it.
Despite recognition that this is a common problem, for which doctors are poorly prepared, there has been little research of doctors' discussions when confronted by difficult choices for a patient close to the end of life. We therefore conducted this study of junior doctors' behaviour in such a situation.
Participants and methods
Clinical scenario—We designed a “no win” scenario in which a decision not to operate would result in death (leaking abdominal aortic aneurysm), while comorbidities (end stage cardiac, respiratory, and renal disease) would make it highly likely that intervention would result in serious complications and prolonged stay in intensive care, probably culminating in death. An actor was briefed to take the role of the patient with very limited functional status, who was struggling to live alone after the death of his wife and who had been considering death before his aorta ruptured. For the interviews, the actor lay on a trolley in a hospital gown, wearing an oxygen mask and displaying obvious discomfort on movement. The actor was instructed to specifically ask for advice in the event that the interviewing doctor did not offer it.
Participants—Using the same actor and scenario on a weekly basis over four weeks, we invited 30 junior doctors in training (3-5 years after graduation) to speak to the “patient” about his condition and treatment options. The doctors were aware that they were speaking to an actor and were told that the aim of the study was to see what they discussed when faced with a potential major intervention in a high risk patient.
Recording of interviews—Only the actor and doctor were present for each interview. No time limit was set—we instructed the doctors to take their leave when they were satisfied that the interview had reached a natural conclusion. We recorded the interviews on audiotape, and subsequently transcribed the recording. To maintain anonymity, the doctors were not identified on the audiotape or on the transcript. After transcription the tapes were erased on the instruction of the ethics committee.
Scoring of transcripts—Four specialists (three intensive care consultants and one nephrologist) independently reviewed the transcripts (that is, without discussion between them). They had agreed on the aspects of the interviews to be scored before the study. These included explanation of the medical condition and the interventional or non-interventional options and exploration of the patient's prior functional status, values, and fears. In addition, the response to the request for advice was to be noted. Each of the aspects was scored on a four point scale (from 0 (not discussed) to 3 (good discussion)) by each reviewer.
Statistical analysis— We determined a median score for each aspect reviewed by each of the four specialists and combined these scores to provide an overall median (interquartile range) score for each aspect. We compared the combined scores for the different aspects by applying the sign test to the paired differences. We determined inter-rater reliability for the specialists using Kendall's coefficient of concordance.
Results
The four reviewers showed fair inter-rater reliability (Kendall's coefficient of concordance for explanation of condition 0.54, of functional status 0.82, of values 0.65, of fears 0.49, of interventional option 0.56, and of non-interventional option 0.58; all P < 0.0001). The reviewers considered the medical condition to be well described generally (median score 2.7 (interquartile range 2.1-3.0), whereas the patient's functional status, values and wishes, and fears were generally not addressed or were only poorly covered (median scores 0.5 (0.0-1.0), 0.5 (0.0-1.0), and 0.0 (0.0-1.5), respectively; fig 1).
Fig 1.
Quality of 30 junior doctors' discussions of treatment options for a patient with acute, life threatening illness and serious comorbidities. (Figure shows median, interquartile range, and range of scores)
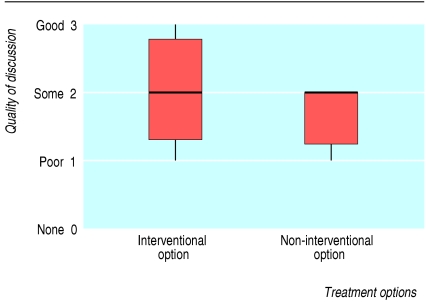
The interventional (surgical) option was not significantly better described than the non-interventional option (median scores 2.0 (1.25-2.75) and 2.0 (1.25-2.0) respectively; fig 2). The explanation of the interventional option often did not describe the likely postoperative course but remained focused on the immediate surgical risk. Explanation of the consequences of non-intervention was often limited to the probability of death.
Fig 2.
Quality of 30 junior doctors' explanations of treatment options for a patient with acute, life threatening illness and serious comorbidities. (Figure shows median, interquartile range, and range of scores)
All but one doctor indicated that they wished to involve the family in discussions, but none identified a preferred surrogate decision maker. Six doctors (20% (95% confidence interval 6% to 34%)) suggested that the patient should speak with his family alone to help them to arrive at a decision (without the doctor being present to explain the medical situation). The doctors were reluctant to give advice, despite it being requested: two (6% (0 to 14%)) stated that a doctor could not give advice (stated reasons were “My job as a doctor is to give you the options,” “I can't answer that, because I am not you,” “I have given you the options, you'll have to decide”), while 17 (57% (39% to 75%)) simply restated the medical risks without offering advice. Of the 11 (36% (18% to 53%)) who did give advice, eight (72%) advocated intervention.
Discussion
This study showed that the junior doctors explained the medical situation reasonably well but generally did not consider the extent to which disease was affecting the life of the patient. Nor did they consider the treatment options in the context of the patient's fears or hopes. They focused on the disease rather than approaching the problem as a composite of the disease and the person.
Patients consider it to be important for doctors to give attention to patient values rather than just to the disease process.2 This is not a new issue. The eminent physician William Osler (1849-1919) wrote: “It's more important to know what sort of person this disease has, than what sort of disease this person has.” This view is probably even more pertinent today, with the advance of medical specialisation, the ageing population, and the vastly increased range of possible treatments that can be offered.
Proper informed consent requires a balanced presentation of the available treatment options. Our analysis of the junior doctors' presentation of the interventional and non-interventional options indicates that there is plenty of room for improvement.
Limitations of this study
Our actor was placed in the appropriate context and played the part of a sick patient in pain. However, the actor was younger than the patient he played and was obviously not in shock. It is therefore possible that important non-verbal cues were absent and that the interviewing doctors reacted differently than they would have done in the real clinical context. On direct questioning after the interview, the doctors said that they thought the situation was realistic, but some of those who had asked the patient about his functional limitation expressed surprise that he had reported such severe limitation.
To facilitate description of the communication process, we chose to score elements of the communication. Evaluation of the effectiveness of communication is highly subjective, however, and our reviewers showed substantial variation in their scoring.3 The use of four reviewers, who each discuss the issues frequently in their routine clinical practice, was designed to rate the interviews as effectively as possible. While all simulations have some limitations, we believe that our study usefully identified areas where educational efforts should be directed.
Giving advice
Most of the doctors in our study were unwilling to offer advice. This may have been because of uncertainty about the clinical situation, since the doctors surveyed were all trainees, but the comments made by some suggest that they think giving advice is inappropriate. Recent teaching has emphasised respect for patient autonomy and has suggested that the doctor's role should be limited to providing information.4 Informal discussion with trainees confirms that local medical school teaching clearly conveys this message. Recent discussion in the medical ethics literature has recognised that a role limited to delivery of information may have substantial limitations, particularly for patients who are unable or unwilling to make a decision.5 An approach that includes a spectrum of options—ranging from simple provision of information for autonomous patient choices to a beneficent, paternalistic manner—may be more appropriate in response to the vastly different personalities of patients presenting with the same serious disease.6
The findings of Heyland et al support the idea that different patients have different requirements.7 They ascertained patients' preferred role in end of life decisions and found that 10% wished to leave all decisions to their doctor, 9% wished their doctor to decide for them after seriously considering their opinion, 32% felt the decision should be shared between the doctor and the patient, and 24% reported they wished to make the decision after seriously considering their doctor's opinion. Only 16% stated that they wished to make the decision alone. If these findings are generally applicable, then at least 75% of patients faced with an end of life decision want their doctor to offer a recommendation. However, Johnston and Pfeifer have reported that only 50% of doctors believed it was appropriate to offer advice.8 We found that only 36% of our doctors gave advice even when advice was directly requested.
When advice was given it was predominantly in favour of intervention. The failure of the doctors to explore the patient's feelings, values, and fears is likely to have contributed to this outcome. Where doctors limit consideration to a disease process, without considering the individuality of the patient who has the disease, it is probable that they will only feel comfortable advocating an interventional course. It is recognised that doctors advocate more life sustaining treatment than elderly people report that they would want, and doctors report that they want less life sustaining treatments for themselves than they would order for elderly patients.9 Hence, doctors should try to compensate for this discrepancy when advising life sustaining treatments in high risk elderly patients. These findings suggest that the training given to doctors on providing advice should be reconsidered.
Involving patients' families
Although all but one of the doctors indicated that they wished to involve the family in discussing treatment options, none identified a preferred surrogate decision maker. In situations where the patient will probably be in no position to make decisions postoperatively and where major complications are likely, it would be wise for a surrogate decision maker to be identified beforehand. Encouraging patients to identify an appropriate surrogate respects their autonomy and can greatly assist decision making should they become incapable.
When patients are uncertain about treatment options, they are unlikely to be in a good position to brief their family about the medical situation and possible treatments in order to reach an informed decision in discussion with them. In our study 20% of the doctors suggested that the patient should speak with their family alone (without the doctor being present to explain) to make a treatment decision. Teaching that highlights the limitations of this approach would be useful.
What is already known on this topic
Doctors are increasingly confronted by major, life threatening illness in patients with serious comorbidities
Little research has been done on how doctors discuss treatment options with patients in this difficult situation
What this study adds
Doctors focused on technical medical issues and placed little emphasis on patient factors such as functional status, values, wishes, and fears
Doctors were reluctant to offer advice about treatment options even when specifically asked for it, and when advice was given it was predominantly in favour of intervention
Doctors need to develop communication skills so that they can better explore their patients' wishes and are therefore better prepared to help patients make decisions when confronted by major illness at the end of life
Conclusions
In response to the results of this study, we are implementing a structured education programme entitled “When enough is enough.” This two hour course aims to assist hospital doctors develop communication skills so that they can better explore their patients' wishes and are therefore better prepared to help their patients make decisions when confronted by major illness at the end of life. The course includes written material, video footage, and interaction with actors.
We believe that discussing treatment options with patients is a vitally important skill for which training can be improved. Medical education is mainly focused on understanding disease. A move towards educating doctors to better understand people has potential to improve patient outcomes considerably.
We acknowledge the efforts of Ruth Clark, who arranged and coordinated the interviews. We also thank all those doctors who participated in the study. Further details of the “When enough is enough” course can be obtained from charliec@barwonhealth.org.au
Contributors: CFC and JWA conceived the study. CFC, JWA, PJS, and DTG assessed the interviews and wrote the article. MJH performed the statistical evaluation and contributed to writing the article. CFC is guarantor for the article.
Funding: This study was supported by a grant from the Department of Human Services, Barwon South West Region, Victoria, Australia. The study design, implementation, and reporting were independent of the funding agency.
Competing interests: None declared.
Ethical approval: The study was approved by the Barwon Health Human Research and Ethics Advisory Committee.
References
- 1.Schwartz CE, Goulet JL, Gorski V, Selwyn PA. Medical residents' perceptions of end-of-life care training in a large urban teaching hospital. J Palliat Med 2003;6: 37-44. [DOI] [PubMed] [Google Scholar]
- 2.Curtis JR, Wenrich MD, Carline JD, Shannon SE, Ambrozy DM, Ramsey PG. Understanding physicians' skills at providing end-of-life care perspectives of patients, families, and health care workers. J Gen Intern Med 2001;16: 68-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thistlethwaite JE. Developing an OSCE station to assess the ability of medical students to share information and decisions with patients: issues relating to inter-rater reliability and use of simulated patients. Educ Health (Abingdon) 2002;15: 170-9. [DOI] [PubMed] [Google Scholar]
- 4.Pochard F, Grassin M, Kentish-Barnes N, Azoulay E. Patient autonomy and the end of life. Crit Care Med 2003;31: 662-3. [DOI] [PubMed] [Google Scholar]
- 5.Schneider C. The practice of autonomy, patients, doctors and medical decisions. Oxford: Oxford University Press, 1998.
- 6.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA 1992;267: 2221-6. [PubMed] [Google Scholar]
- 7.Heyland DK, Tranmer J, O'Callaghan CJ, Gafni A. The seriously ill hospitalized patient: preferred role in end-of-life decision making? J Crit Care 2003;18: 3-10. [DOI] [PubMed] [Google Scholar]
- 8.Johnston SC, Pfeifer MP. Patient and physician roles in end-of-life decision making. End-of-Life Study Group. J Gen Intern Med 1998;13: 43-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carmel S. Life-sustaining treatments: what doctors do, what they want for themselves and what elderly persons want. Soc Sci Med 1999;49: 1401-8. [DOI] [PubMed] [Google Scholar]