Abstract
A 50-year-old man with intractable anal pain attributed to proctalgia fugax underwent insertion of a sacral nerve stimulator via the right S3 vertebral foramen for pain control with good symptomatic relief. Thirteen months later, he presented with signs of sepsis. Computed tomography (CT) and magnetic resonance imaging (MRI) showed a large presacral abscess. MRI demonstrated increased enhancement along the pathway of the stimulator electrode, indicating that the abscess was caused by infection introduced at the time of sacral nerve stimulator placement.
The patient was treated with broad spectrum antibiotics, and the sacral nerve stimulator and electrode were removed. Attempts were made to drain the abscess transrectally using minimally invasive techniques but these were unsuccessful and CT guided transperineal drainage was then performed. Despite this, the presacral abscess progressed, developing enlarging gas locules and extending to the pelvic brim to involve the aortic bifurcation, causing hydronephrosis and radiological signs of impending sacral osteomyelitis. MRI showed communication between the rectum and abscess resulting from transrectal drainage. In view of the progressive presacral sepsis, a laparotomy was performed with drainage of the abscess, closure of the upper rectum and formation of a defunctioning end sigmoid colostomy. Following this, the presacral infection resolved.
Presacral abscess formation secondary to an infected sacral nerve stimulator electrode has not been reported previously. Our experience suggests that in a similar situation, the optimal management is to perform laparotomy with drainage of the presacral abscess together with simultaneous removal of the sacral nerve stimulator and electrode.
Keywords: Sacral nerve stimulator, Presacral abscess, Proctalgia fugax
Sacral nerve stimulation is the implantation of a permanent pulse generator that delivers controlled electrical impulses via an electrode placed in contact with the sacral nerve roots, the S3 nerve root being the most common. It is of proven value in the treatment of urinary and faecal incontinence, urinary non-obstructive retention, and chronic pelvic and anal pain including proctalgia fugax.1 We report the case of a 50-year-old man having severe anal pain attributed to proctalgia fugax for 7 years. Treatments with caudal epidural injection and ganglion impar block had been unsuccessful. He was referred to a tertiary centre for chronic pain management, where a temporary trial of S3 nerve stimulation was successful in controlling his anal pain. A permanent nerve stimulator was then implanted with the electrode being sited adjacent to the right S3 nerve root with good symptomatic relief.
The patient presented 13 months later with symptoms and signs of sepsis including poor appetite, weight loss, night sweats, pyrexia, leucocytosis and elevated C-reactive protein. Computed tomography (CT) showed a chronic presacral abscess and magnetic resonance imaging (MRI) demonstrated enhancement along the pathway of the implanted electrode, indicating that the presacral abscess was caused by infection introduced at the time of sacral nerve stimulator implantation. This complication of sacral nerve stimulator implantation is extremely rare and has not been reported previously in the medical literature. We discuss our investigation and management of this case, and give our recommendation for optimal management of this rare complication.
Case history
A 49-year-old man was referred to a tertiary pain centre with a 7-year history of intractable anal pain that had been attributed to proctalgia fugax. He had been investigated with sigmoidoscopy, examination of the rectum under anaesthesia and anorectal MRI; no abnormality had been found. He had been treated with amitriptyline, pregabalin, slow release morphine, oxycodone, caudal epidural injection and ganglion impar block without significant improvement in his symptoms. A temporary right-sided S3 sacral nerve stimulator was implanted, which gave excellent relief from his anal pain. In view of this, a permanent right-sided S3 nerve stimulator was implanted using antibiotic prophylaxis. There were no signs of local infection and good control of anal pain was achieved.
Thirteen months later, the patient was admitted again with a three-week history of poor appetite, weight loss, night sweats and pyrexia. Blood tests showed a haemoglobin level of 104g/l, an international normalised ratio of 1.2, a white cell count of 22.6 × 109/l, a platelet count of 546 × 109/l and a C-reactive protein level of 167mg/l, indicating severe infection.
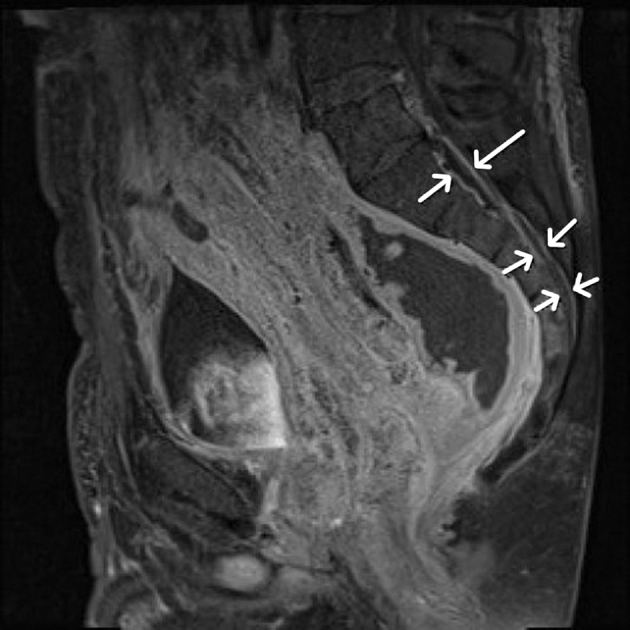
The patient was treated with broad spectrum antibiotics and CT was performed, which demonstrated a chronic abscess in the presacral region extending from the S2 vertebra downwards, measuring 9cm craniocaudally, 6cm transversely and 5.6cm anteroposteriorly (Fig 1). Inflammatory changes were seen in the rectum anteriorly. MRI showed the sacral nerve stimulator electrode extending from the right sacral foramen to the presacral space and penetrating the mesorectal fascia (Figs 2 and 3). MRI also demonstrated increased enhancement of the S2/S3 and S3/S4 intervertebral discs (Fig 4) as well as along the stimulator electrode, indicating infection arising from stimulator implantation. In addition, there was leptomeningeal enhancement and a rim enhancing epidural abscess (Fig 5).
Figure 1.
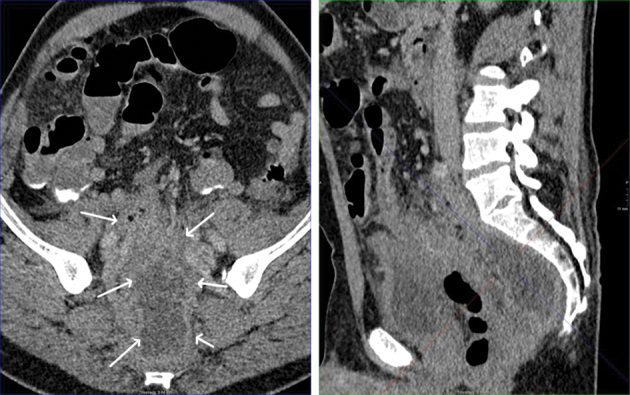
Reformatted oblique and sagittal computed tomography showing presacral abscess (arrows)
Figure 2.

Sagittal and axial computed tomography showing stimulator electrode passing through the sacral foramina
Figure 3.

Transverse computed tomography showing the stimulator electrode adjacent to the presacral abscess (arrow)
Figure 4.
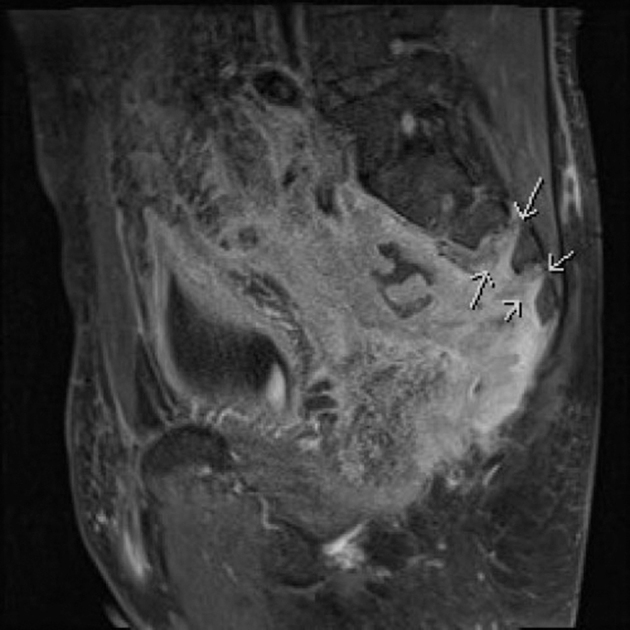
Sagittal magnetic resonance imaging showing increased enhancement of the S2/S3 and S3/S4 intervertebral discs, and associated large presacral abscess
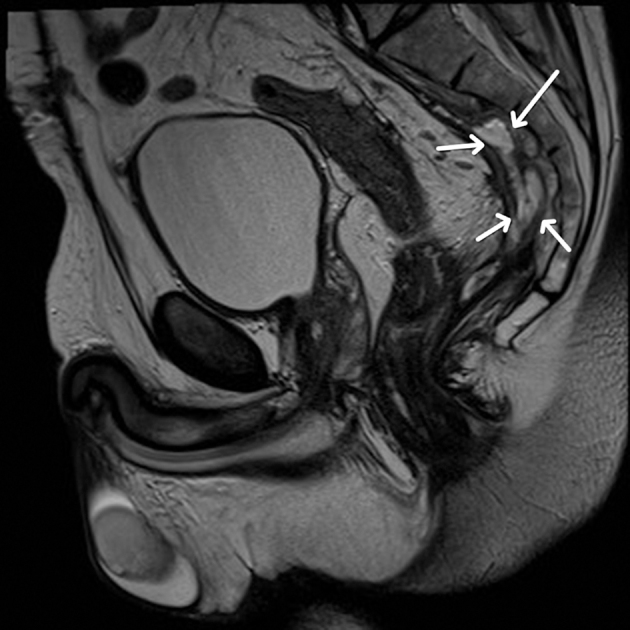
Figure 5.
Sagittal magnetic resonance imaging showing increased leptomeningeal enhancement (upper 2 arrows), rim enhancing epidural abscess (lower 4 arrows) and presacral abscess
The sacral nerve stimulator and electrode were removed under general anaesthesia. At that time, rectal examination showed a hard indurated posterior rectal wall. There was no fluctuant abscess that could be drained without imaging. Attempts were then made to drain the presacral abscess using minimally invasive techniques. Initially, transrectal ultrasonography guided drainage was attempted following bowel preparation with MoviPrep® (Salix, Raleigh, NC, US); 400ml of serous fluid was aspirated at two different points. Microbiological analysis of the fluid found that it contained Klebsiella oxytoca sensitive to both gentamicin and piperacillin/tazobactam as well as Enterococcus faecium sensitive to linezolid. A guidewire was passed into the collection and balloon dilation was performed. However, a drainage catheter could not be inserted owing to patient intolerance. A drain was then placed transperineally into the presacral abscess under CT guidance (Fig 6). Although some purulent fluid was drained, the patient did not improve significantly.
Figure 6.
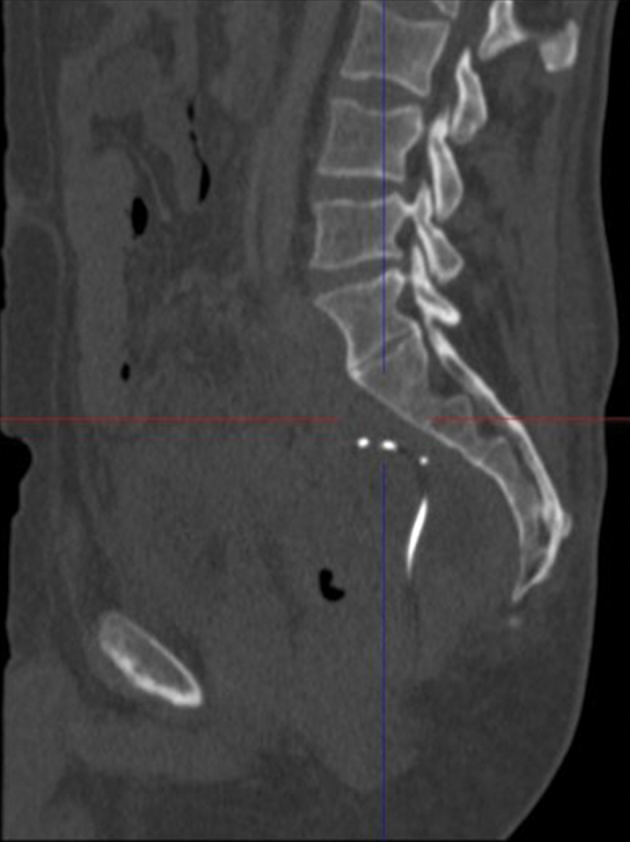
Sagittal computed tomography showing transperineal drainage catheter
Three weeks later, CT demonstrated a progressing presacral collection containing more gas locules extending cranially to the aortic bifurcation and encasing the iliac arteries. Hydronephrosis had developed, indicating ureteric compression at the pelvic brim caused by the inflammatory mass. MRI showed a thick walled, enhancing presacral collection with a connection from the superior aspect of the rectum extending into the presacral collection in the position of the attempted transrectal drain implantation. There was induration and inflammation of the sacral periosteum, indicating impending sacral osteomyelitis.
In view of the progression of the presacral collection, despite broad spectrum antibiotics and minimally invasive drainage, bilateral ureteric stents were inserted and a laparotomy was performed. Purulent fluid and necrotic material was removed from the presacral space, and wide bore drains were inserted presacrally. The rectum was divided above the pelvic brim using a surgical stapler and then oversewn. A sigmoid end colostomy was constructed to defunction the rectum so as to minimise the risk of reinfection of the presacral region with faecal organisms. The patient made a good recovery and subsequent MRI showed progressive resolution of the presacral collection (Fig 7).
Figure 7.
Sagittal magnetic resonance imaging showing progressive resolution of presacral abscess at 5 months following laparotomy and drainage (arrows)
Discussion
Sacral nerve stimulation has been found to be an effective treatment for chronic idiopathic anal pain.1,2 Implantation of permanent sacral nerve stimulators is associated with an infection rate of approximately 11% despite antibiotic prophylaxis,3 with infection developing from one month to more than a year after implantation.4 Infection usually presents as cellulitis over the site of the pulse generator, and requires removal of the stimulator and electrode. Pain can, however, be the sole presenting symptom of sacral nerve stimulator infection.5
There have been no previous reports of presacral abscess formation complicating sacral nerve stimulator implantation. In our case, MRI demonstrated enhancement along the pathway of the stimulator electrode, indicating that the presacral abscess developed as a result of infection introduced at the time of sacral nerve stimulator implantation. The infection was severe with leptomeningeal involvement, an epidural abscess and a large presacral abscess.
Once the diagnosis had been made, broad spectrum antibiotics were given according to microbiological advice, and the sacral nerve stimulator and electrode were removed. Attempts were then made to drain the presacral abscess using minimally invasive techniques, initially ultrasonography guided transrectal catheter placement. When this proved unsuccessful, CT guided transperineal drainage was performed. Although CT showed that the transperineal drainage catheter was in a good position within the presacral abscess and some purulent material was drained, the presacral abscess progressed as evidenced by the development of more gas locules, involvement of the aortic bifurcation, compression of the ureters at the pelvic brim and development of radiological signs of impending sacral osteomyelitis. This may have been because transrectal drainage attempts resulted in a persistent communication between the rectum and presacral collection, allowing reinfection of the presacral region with faecal organisms.
In view of the progressive presacral collection and proven communication with the rectum, the safest approach was to perform a laparotomy with drainage of the presacral collection, construct a defunctioning sigmoid colostomy and close the rectal stump. Following this, MRI indicated resolution of the presacral collection. Unfortunately, the patient’s chronic anal pain has returned.
Our experience suggests that laparotomy with drainage of the presacral abscess, performed at the time of removal of the sacral nerve stimulator and electrode, would have been a better management option than to attempt drainage using minimally invasive techniques after removal of the sacral nerve stimulator and electrode. It is likely that this would have avoided the need for colostomy formation.
Conclusions
Presacral abscess formation is a rare complication of sacral nerve stimulator implantation that has not been described previously. The optimal management appears to be laparotomy and drainage of the presacral abscess at the time of removal of the sacral nerve stimulator and electrode.
References
- 1.Chiarioni G, Asteria C, Whitehead WE. Chronic proctalgia and chronic pelvic pain syndromes: new etiologic insights and treatment options. World J Gastroenterol 2011; : 4,447–4,455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falletto E, Masin A, Lolli P et al. Is sacral nerve stimulation an effective treatment for chronic idiopathic anal pain? Dis Colon Rectum 2009; : 456–462. [DOI] [PubMed] [Google Scholar]
- 3.Guralnick ML, Benouni S, O’Connor RC, Edmiston C. Characteristics of infections in patients undergoing staged implantation for sacral nerve stimulation. Urology 2007; : 1,073–1,076. [DOI] [PubMed] [Google Scholar]
- 4.Wexner SD, Hull T, Edden Y et al. Infection rates in a large investigational trial of sacral nerve stimulation for fecal incontinence. J Gastrointest Surg 2010; : 1,081–1,089. [DOI] [PubMed] [Google Scholar]
- 5.Elkattah R, Chiles L, Bird E, Huffaker RK. Pain as the sole presenting symptom of infected sacral nerve stimulation implantable pulse generator. Open Access J Sci Technol 2015; : 1–3. [Google Scholar]


