Abstract
Background
No studies of Health Coach Interventions for knee OA sufferers that include patients’ perspectives have been published. The study assesses current clinical practice and primary care professionals’ advice from the patients’ perspective, in order to obtain a participative design for a complex intervention based on coaching psychology. Moreover, wants to analyse the experiences, perceptions, cognitive evaluation, values, emotions, beliefs and coping strategies of patients with knee osteoarthritis, and secondly the impact of these factors in the Self-management of this condition.
Methods
It is an interpretative qualitative study. The study included patients with diagnosis of knee osteoarthritis (OA) from 4 primary health care centres in Barcelona. A theoretical sampling based on a prior definition of participants’ characteristics was carried out. Ten semi-structured interviews with knee OA patients were carried out. A content thematic analysis was performed following a mixed-strategy text codification in Lazarus framework and in emerging codes from the data.
Results
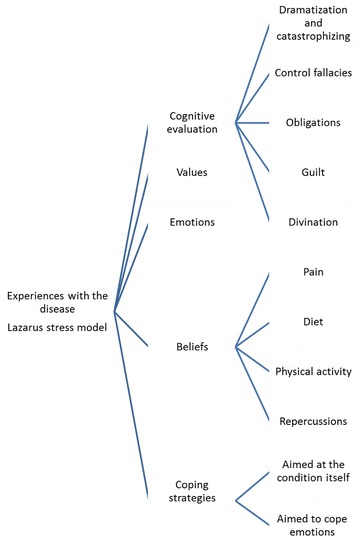
The results are structured in two blocks: Experiences and perceptions of informants and Experiences of knee osteoarthritis according to the Lazarus model. Regarding experiences and perceptions of informants: Some participants reported that the information was mostly provided by health professionals. Informants know which food they should eat to lose weight and the benefits of weight loss. Moreover, participants explained that they like walking but that sometimes it is difficult to put into practice. Regarding experiences of knee osteoarthritis according Lazarus model: Cognitive evaluation is influenced by cognitive distortions such as obligation, guilt, dramatization and catastrophism. Values: Family is the value most associated with wellbeing. Helping others is another recurring value. Emotions: Most participants explain that they feel anxiety, irritability or sadness. Beliefs: To some, physiotherapy helps them feel less pain. However, others explain that it is of no use to them. Participants are aware of the association overweight– pain. Coping strategies: The strategies for coping with emotions aim to reduce psychological distress (anxiety, sadness, anger) and some are more active than others.
Conclusions
The study highlights that patients with knee osteoarthritis require a person-centered approach that provides them with strategies to overcome the psychological distress caused by this condition.
Electronic supplementary material
The online version of this article (doi:10.1186/s12891-017-1584-3) contains supplementary material, which is available to authorized users.
Keywords: Lifestyle, Knee osteoarthritis, Qualitative research, Health coaching, Primary health care, Interviews
Background
Clinical guidelines for knee osteoarthritis (OA) recommend non-pharmacological first-line management which should include weight loss, healthy eating habits, physical activity (PA), Self-management of pain, information-education and orthoses [1]. In particular, they recommend the education of patients even if current evidence remains inconclusive [2–4]. Indeed, non-pharmacological recommendations frequently lack precision regarding contents, duration, intensity and frequency and might result in the suboptimal care of OA patients observed in several studies [4].
Based on personal living experiences with the disease, the interactions with health professionals and the treatments received, the informants have identified various elements to take into account in the design, contents and format of a new intervention for knee OA implemented in Primary Health Care [5]. The impact of knee OA can be profound on self-esteem [6], it limits daily activity, causes a feeling of loss [7] and decreases work productivity. These effects could be mitigated if the health services provided more information on the disease and on how to manage it self-efficiently [8]. Moreover, taking into consideration the beliefs and expectations of patients can contribute to improve the interventions [9].
The theoretical foundation of Health Coaching (HC) is linked to the theoretical-conceptual framework of behavioural change [10] and has been defined as a behavioural intervention to facilitate the establishment and achievement of health promotion objectives, modify behaviours, reduce harmful habits, improve self-management of chronic conditions and increase health related quality of life [11].
Health Coaching (HC) can improve quality of life, change attitudes, decrease unhealthy habits, treatment adherence, self-management and pain in chronic patients [12–19] and also promote healthy eating and PA [20]. In order to live with knee OA, patients use coping strategies that are determined by their values, emotions and beliefs. These categories define the key components that knee OA sufferers perceive as important for the design of a coaching intervention [5].
No studies of HC interventions for knee OA sufferers that include patients’ perspectives have been published. The Medical Research Council has established a methodology for the development of complex interventions that consists of several phases and uses qualitative and quantitative methods [21, 22]. The first phase of this methodology aims at identifying the contextual factors that shape the theories of how the intervention works and might affect implementation, the modelling process and outcomes.
The objectives of this study were:
To identify current practice and advice of primary care professionals from the patients’ perspective in order to achieve a participative design of a complex intervention based on coaching psychology
To further understand the experiences, perceptions, cognitive evaluation, values, emotions, beliefs and coping strategies of patients with knee OA and the influence of all these factors in the Self-management of this condition.
Methods
Design
We conducted an interpretative qualitative study [23] to further our understanding of the phenomenon as experienced by the individual living with knee OA. The study also looked for patient related factors that could facilitate or restrict the implementation of the intervention (acceptability, adequacy, feasibility, integration within other programs, location, schedule and duration).
Conceptual framework of the study: Lazarus stress model
The Lazarus stress coping model [24, 25] has been used to understand stressful life events. This framework is adequate for our research when we consider knee OA as a potential stressful factor. The level of distress and wellbeing of people are determined by their coping strategies.
A growing body of studies stresses the importance of psychological factors in the pain process. The Lazarus stress model has been transferred to the chronic pain field to study these factors. This model suggests that when there is a potentially stressful event, anxiety levels depend on the cognitive evaluation of pain stimulus and the strategies used to cope with it. Psychological pain factors which have recently appeared in the literature are analysed from the perspective of the Lazarus model [26].
The Lazarus model includes the following variables:
Cognitive Evaluation: process that determines the consequences that a particular event will generate in an individual.
Values: Values convey what is important for the individual and determine what is at stake in a particular stressing situation.
Emotions: Lazarus enumerates the following emotions: anger, envy, jealousy, anxiety-horror, guilt, shame, relief, hope, sadness-depression, gratefulness, compassion, happiness-joy, pride and love [27].
Beliefs: cognitive configurations created individually or culturally shared. They are pre-existing notions of reality that can be used as a perceptual lens.
Coping Strategies: constantly changing cognitive and behavioural efforts developed to manage specific external and/or internal demands that are evaluated as excessive or overwhelming for the resources of the individual.
Social Support: coping resource whereby we have somebody that provides emotional, informative and/or tangible support.
Participants: The study included symptomatic knee OA patients, with clinical and radiographic OA grades 1–3 in the Kellgren-Lawrence classification, selected from four primary health care centres (PHCC) in Barcelona. Participants were recruited by the general practitioners in each PHCC between February and April 2015.
Sampling and participant selection strategy
A theoretical sampling based on a prior definition of participants’ characteristics was carried out to obtain optimal variety and discursive wealth [28]. Patients with knee OA living in the metropolitan area of Barcelona were selected in accordance to a priori defined profiles. We took the following variables into account: gender, age, number of years with knee OA, employment status, household and relevant health problems.
Patients with knee OA were recruited by their general practitioner or nurse, who explained the study and suggested the participation.
Techniques to generate information
Face to face individual Interviews were conducted by the first author, a specialist in this technique, in the PHCC of the participants, and lasted from 30 to 60 min. The interview guide followed five sequences (impact of knee OA; interaction with health professionals, physiotherapists and social workers; coping strategy; recommendations toward the design of the intervention; and use of information technology techniques - ICTs) (Additional file 1). The interviewer used open, non-directive formulation consistent with the participant’s language. Observational field notes that included contextual characteristics, atmosphere and relevant non-verbal expressions were produced. Ten patients with knee OA were invited to participate, all of them accepted and data saturation was reached (Table 1).
Table 1.
Sociodemographic characteristics of participants with knee OA
| Code | Gender | Age (years) | Years since onset knee osteoarthritis | Employment status | Household size | Relevant health problems |
|---|---|---|---|---|---|---|
| M1_CR | Female | 60 | 16 | Housewife | Partner | Haemophilia and Depression |
| H2_CR | Male | 84 | 14 | Retired (building) | Partner | Silicosis, vascular problem in one leg |
| H3_CR | Male | 58 | 20 | Disabled (graphic design) | Partner | Pain in lower limbs |
| H4_SA | Male | 85 | 6 | Retired (factory) | Alone (widower) | Diabetes, bladder cancer (operated) |
| M5_U | Female | 66 | 16 | Disabled (cleaning) | Alone (divorced) | Polyarthritis, anxiety |
| M6_U | Female | 62 | 15 | Housewife | Partner | Polyarthritis, anxiety symptoms, high blood pressure |
| M7_U | Female | 67 | 5 | Retired | Partner | Knee prosthesis, carpal tunnel |
| M8_VR | Female | 75 | 3 | Housewife | Grandson | Knee prosthesis and breast cancer |
| M9_VR | Female | 83 | <1 | Housewife | Alone (widow) | High blood pressure |
| M10_VR | Female | 67 | 17 | Retired | Alone (single) | Diabetes and depression |
Data analysis
All interviews were recorded and transcribed literally and systematically by trained personnel. After successive readings of the transcriptions, researchers reached preanalytical intuitions. A content thematic analysis was performed [24, 25]. Next, the following analytical steps were carried out: a) identification of the relevant texts; b) fragmentation of the text in units of meaning; c) a mixed-strategy text codification in Lazarus categories and in emerging codes from the data; d) creation of categories grouping the codes by the criterion of analogy; e) analysis of each category; and f) elaboration of a new text with the results. These results were subsequently discussed with the whole research team and, after careful deliberation and exchanges of findings, consensus was reached.
The following procedures were performed to improve rigour [29]: triangulation of analysis by four researchers; and comparison of findings with the original data.
Results
The results are structured in two blocks: Experiences and perceptions of informants and Experiences of knee osteoarthritis according to the Lazarus model.
Experiences and perceptions of informants
- Experiences and perceptions in patients’ interactions with health professionals (General Practitioner and nurse), physiotherapists and social workers The following subcategories emerged from the informants’ discourses:
-
Information-education on knee osteoarthritisSome participants reported that the information was mostly provided by their family doctors, who explained the repercussions of knee OA, the progression of the disease and also provided some advice. However, a participant told that sometimes she did not understand the information provided. Others were not satisfied with the information received, in particular by specialists; they considered that it amounted practically to nothing and that the interaction was limited to prescribing painkillers and to referring them for diagnostic tests.Do you feel that the professionals of the health centre have provided enough information on knee osteoarthritis?. . No, they just prescribe painkillers. And I cannot take strong painkillers because I have a large hernia and they prescribe paracetamol, which is useless. M9_VRNone of the participants received materials on these issues, and some said it would be useful for them to have this information although they did not specify which type of materials they expected. The patients’ expectations aimed to obtain more information on their condition, prognosis and treatment”.
-
Professional advice on diet and weightAdvice on losing weight was mentioned by most participants. Informants are aware that they are overweight, they know which food they should eat to lose weight and the benefits of weight loss. Some explained that they take care of their weight, but that putting on weight comes very easy to them. They find it difficult to modify behaviours, mainly because of lack of discipline and because of the food they love. They emphasized the difficulty of sustaining a healthy weight, they had lost weight with the help of dieticians, endocrinologists and acupuncture and have again put it on.“…I’m very strict …You tell me “take this list: Monday this, Tuesday that,..” and I will do it… don’t give me anything ambiguous for me to plan between 5 possible first courses, 5 possible second courses.. no. H4_SASome had received leaflets about diets to help them achieve weight loss.
-
Professional advice on physical activityParticipants explained that health professionals tell them to walk. They explained that they like it and they walk even if it is difficult, because if they move they feel better.Some receive positive feedback for exercising in water to reduce impact on the joints,“Aguagym? Yesyesyes, it’s wonderful. I go twice a week, and then I feel so relaxed, because I leave the swimming pool, I have a shower…and such, I then feel so relaxed …” M1_CRand others use the stationary bicycle. They explained that they would feel more motivated if they could exercise in a group.
-
Experiences with the different treatments providedInformants mentioned painkillers and non-steroidal anti-inflammatory agents, usually prescribed by health professionals. They are anxious about the side effects of these medications.“I avoid taking pills…I have some, in case one day it hurts too much….” M5_UDepending on the situation, they choose to take paracetamol, NSAIDs, sometimes with a “gastric protection agent”, or bear the pain without taking any tablets.Gels and creams are well accepted by participants, but they complained that the public health system does not cover this type of treatment; they also complain about (the) long waiting times for local injections.Some participants had also had physiotherapy with mostly positive results on the short and medium term. In general, they complained about the long waiting lists to access these services.One informant explained a positive experience with magnesium supplements. They did not comment on the opinions of professionals on alternative therapies.Two participants have a knee prosthesis and they evaluate them positively. Most consider that prosthesis is the best option in the long term although they leave it for when their condition is unsustainable. The youngest participants explained that in this case the health professionals recommend to wait and to bear the condition. Two participants expressed the need for research in this area.“in November 2011 they were about to give me a prosthesis, I had the day of admission, for the operation and everything, but in the preoperative stage, the last person you talked to is the anaesthetist, and he really scared me he told me you are very young and the average duration of the prosthesis is 10 years, and there is more rejection in the second…and I didn’t do it,” H3_CR“Well, if some people need the operation, they don’t want to suffer more then, explain, tell him to not be afraid, that the operation no no… My experience of the operation is very positive…” M8_VR
-
-
Experiences of knee osteoarthritis according to the Lazarus model (Fig. 1 )
We have used the Lazarus Stress Model for a structured analysis of the patients’ experiences. This model explains that when faced with a potentially stressing event, people respond with different levels of stress and emotions. This response depends basically on two factors: cognitive evaluation (where according to Beck cognitive distortion takes place) and coping strategies. In summary, emotions depend on how the person evaluates the situation and which behaviours and thoughts does she use to manage this situation. However, this model also includes two additional cognitive variables of a more static nature that determine the other: beliefs and values. Consequently, based on their beliefs and personal values, individuals will evaluate and cope with a particular situation with different degrees of stress. An outline of the model can be found in Fig. 1.
This model can be applied in this study, since knee osteoarthritis is a potentially stressing condition.-
A.Cognitive evaluationDifferent cognitive distortions bias the cognitive evaluation of participants. For instance:Within the distortion “obligations”, the concept of helping those around them is the most used.“I have to do the shopping, I have to do the housework to my family” M7_UIn relation to guilt, they feel guilty about not following the advice on diet and PA and for not meeting the expectations of the people closest to them.“I feel bad when I eat something forbidden”. M6_UDramatization and catastrophizing are observed when participants refer to pain and they label it as terrible, as greatly affecting them, etc.“… Terrible, terrible. But in 1998 it was less painful, I think that because I still had my house and was busy with my children, but since I came here, in 2001, uyy, this has been terrible” M10_VRThe control fallacies are conveyed in verbalisations such as lack of time or putting on armour to protect themselves from being hurt.“ until now I went swimming, but lately I had to quit due to family problems, I don’t have time ” “I know many thin women that have bad arthritis” M6_UThe divination of thought usually focuses on the feelings of the loved ones (they think they know what their family members think about them).“… For me it’s not a trauma or anything, people should see that … people are very nosey, they like to ask; there she is with the bad knee.. you have to explain, otherwise …” M1_CR
-
B.ValuesValues are compromises that express what is important for the person. Family is the main answer to the question of what makes them happy and the value most associated with wellbeing. Helping others is another recurring value.Some of them prioritize the needs of others over their own needs, which they associate with the importance of the family.“And most of all not being in much pain, because I have things to do, … help my daughter, … help my mother…”. M1_CRThey lose sight of self-care. Another important value is filling time.“Being busy the whole day!! I spend cleaning … cleaning here and there… It does not even hurt.. M10_VRThe absence of “occupation” takes them back to dejection and sadness thoughts and emotions and feelings of uselessness.The value of autonomy, being physically independent and not needing canes and crutches; it is essential to help the family, others and to be busy.“It makes me sad because it limits me, it limits me a lot, I cannot do what I would do”. M8_VRAll participants mention self-demand (overcoming personal frontiers) and discipline by action (following medical recommendations) or by omission (neglecting to follow these recommendations). They consider themselves demanding in relation to their values and to the important aspects of their life. Prevention of knee OA was not considered a priority.
-
C.EmotionsMost participants explain that they feel anxiety, irritability or sadness. Anxiety affects them differently: in some the diet is affected, in others it increases ruminative thoughts. In most cases, and even if not directly articulated, the low mood status is enhanced by the lack of acceptance of the aging process. They feel nostalgia for the activities they could do “before the arthrosis”, which in fact were activities they carried out in their youth. Indeed, knee osteoarthritis represents a “mourning process” for the participants.Fear takes place when someone in their immediate environment had been seriously disabled as a consequence of osteoarthritis. In these cases, we observed a keener interest for prevention.“I had my mother sitting in a chair for many years as a result of arthrosis. That’s what I fear most” M8_VRParticipants find happiness in small things related to their values: housework, since it signifies autonomy; helping others; and spending time with the family.
-
D.BeliefsBeliefs are cognitive configurations individually created or culturally shared, pre-existing concepts of reality that act as a perceptual lens.
-
Beliefs on painTo some, physiotherapy helps them feel less pain. However, others explain that it is of no use to them.“No… Because when I’m doing physiotherapy it hurts even more, and when physiotherapy finishes it goes on hurting. It doesn’t work for me”. M1_CRPatients believe that physiotherapy is useful when they are doing it and are aware that when they stop physiotherapy the pain comes back. Only one participant explained that he consistently practices the exercises daily because he believes that it is key to improve pain. For some, the pain of knee OA hinders the practice of physical activity because of the belief that it can increase the pain.Another shared belief on pain is “that it must be borne”, possibly related to some Judeo-Christian values of sacrifice, be it as acceptance (coping strategy) or some resignation (negative emotion).To cope with pain, patients choose as a first option looking for distractions, secondly they prefer to bear it and lastly they take medication.
-
Beliefs on dietParticipants are aware of the association overweight– pain. The impossibility of losing weight is one of the most common beliefs amongst women with knee OA. They attribute this impossibility to menopause, age and other factors unrelated to the quality and amount of food intake. Anxiety surrounding food is another factor related to the difficulty in losing weight. Most participants believe that the dieting recommendations are not effective for their particular case. They pointed out that the leaflets with standard advice are of no use to them.“He gave me some paper, but I don’t follow it because it’s bad for me. However, him and another one have insisted that I should not put on weight ” M5_U
-
Beliefs on PAParticipants believe that PA is positive. When they are more active they feel better and their mood improves. The most common PA are walking and Aqua gym.“In water you can do any exercise” “outside water no”. M1_CRThe main limitations for being physically active were knee pain and in some cases negative emotions.
-
Beliefs on OAParticipants explain that OA is a chronic disease and that professionals have told them that it cannot be cured. Beliefs on the possibilities of a cure for knee OA emerge in the interviews, whereas at a conscious level participants are aware that no cure exists yet. However, they mention hope and the need to find a curative treatment.“I think that everything but death has a cure”. M10_VRPatients need to translate the medical indications into something practical in their daily lives. Resignation when faced with knee OA has a strong emotional impact and generates sadness, anger and anxiety. Some patients talked about acceptance with a resigned face and non-verbal signs of negative emotions.
-
-
E.Coping strategiesThe coping strategies aim either at emotions or at the condition itself.The strategies for coping with emotions aim to reduce psychological distress (anxiety, sadness, anger) and some are more active than others. Amongst the most active we highlight looking for distractions, for social support (more emotional than practical). Other patients use strategies to avoid thinking about their problem and being surrounded by family to feel better (one of the most commonly used strategies) such as praying or counting to 10 to calm down.“I spoil myself with a latte”. M8_VR“I wake up around 10 a.m. First thing I drink lukewarm water with lemon, eh, I have breakfast after half an hour, and I make my beds, clean the floor, sweep the apartment, I do, I prepare lunch.. and in the afternoon I get out. ” H3_CR“Mm.. little things, then you understand, how can I explain it.. look, right now I’m enjoying the tablet and my husband with the ball and me with the tablet is no problem at all ” M6_U.“I get it out of my mind” (referring to the disease of the daughter). M8_VRThe most commonly reported strategy is acceptance or resignation.“If you accept it your attitude changes” H3_CRWhereas for some acceptance is a negative concept, others assert that when you accept your condition you change your attitude for the better.The strategies for the condition (chronic and without a lasting solution) aim at reducing the deterioration and the pain (taking medication, walking, cold, rubs, rest and exercise.“When it’s very painful I take ibuprofen or naproxen”. M7_U“Walking at my pace is very relaxing for me”. H3_CR“And I rub it with wasps’ poison” M8_VR“ if you join a gym, whether you believe it or not it’s super positive for the brain ” M10_VR)They learn to pace activities so that the pain does not increase, and to “say no” to avoid being overloaded with obligations. Not all strategies are equally used. Some patients never learn to say “no” or to pace efforts. The strategies aimed at the condition can also be used for the emotions (the calming effect of exercise).
-
A.
Fig. 1.
Lazarus theoretical model applied to knee osteoarthritis
II-Recommendations for the design of the coaching psychology intervention (Table 2)
Table 2.
Recommendations for the coaching intervention – barriers and facilitators
| Barriers in the management of knee osteoarthritis | |
| Result | Contributions |
| Difficulty for translating theory into practice | Strategies and techniques to take action |
| Difficulties in sustaining a healthy diet | Indications and recommendations for a healthy diet |
| To facilitate simple menus | |
| To facilitate healthy menus | |
| Techniques to control stress (anxiety) | |
| Motivation strategies to implement a healthy diet and make it sustainable over time | |
| Pain associated with physical activity | Techniques to manage pain |
| Indications and recommendations to carry out physical activity | |
| Motivation strategies to start and sustain physical activity | |
| Fear | Strategies to overcome fears |
| Facilitators in the management of knee osteoarthritis | |
| Result | Contributions |
| Holistic Vision | Holistic vision focused on individual needs |
| Lack of individualisation | Taking into account the person within the group |
| Physiotherapy to reduce pain | Include physiotherapy exercises in the intervention |
| Strategies to sustain the practice of these exercises | |
| They would like to have more information | To provide information on the disease, its repercussions and advice on how to live with it |
| Learning to say “no” | Assertiveness strategies |
| Social support | To offer space for participants to talk about their particular situation |
| To offer the possibility of continuity of contact between participants at the end of the intervention (WhatsApp, phone, etc.) | |
| Self-care | To provide strategies for the patient to have time for him/herself |
| Learning to calm down | Strategies to control stress |
| Mindfulness | |
| Breathing and relaxation techniques | |
| Acceptance | Work with acceptance and differentiating it from resignation |
| Values | The patients’ most important values will be used to motivate and to generate change in the participants (family, autonomy, discipline) |
Reference framework
Participants pointed out that even within a group intervention there is a need for a holistic, person-centered approach that does not just focus on arthrosis. They underlined the community aspect and the need to be made aware of the resources of the neighbourhood.
“To help us know what’s in there, in this neighbourhood there is nothing to do. Things like aqua gym and such” M7_U
On the other hand, they highlighted the relevance of a participative design that allows sharing experiences and improvement proposals. In their opinion, sharing makes people feel more involved in the activities and it implies more consistency in relation to learning and implementing what they have learned. However, some participants think that they might feel uncomfortable within a group. They also mentioned the importance of working with cultural and socioeconomic sensitivity.
Participants accepted and were open to the proposal of having a health psychologist as coach because they believed it is a professional trained to listen to and solve needs related to their disease.
“I’m happy, because it’s working well with the doctor, and now with you, and if there are things to do for no, to slow down a bit the arthritis, then fantastic…·”. M7_U
None of the participants manifested that they wanted another type of professional to conduct the Health Coaching.
Contents/components
Participants emphasized the need to translate theory into practice for behavioural change. In general, they proposed to encourage the strengths of individuals and to promote strategies to live with a more positive, problem-solving attitude.
“We need to cheer up people that feels down, teach them that they have to move even if they are in pain. Because I also have pain, eh?” M8_VR
Participants also expressed the need to learn to say “no” to be able to focus on self-care. In relation to diet, they explained that they need to learn how to prepare restrictive diets and how to combine foods with nutrients. In relation to PA, they wanted to know the activities most suited to their financial, practical and health needs. With regard to pain, they wanted to know how to channel thoughts toward more positive attitudes.
Use of TICs
Most participants mentioned the regular use of smartphones, tablets and computers. They knew how to use messaging apps and were open to work using these technologies.
“Whatsapp yes. My friend in Italy, I will show you, that I have a friend in Italy, that friend I mentioned from Italy. Whatsapp yes and gmail too… Let’s see, Nicoletta… Every day or every night, “good night”, “”, “bon giorno” “#italiano#” “#italiano#”. M5_U.
Location, schedule and duration and frequency
In relation to location, they consider that activities should take place in any community site that is close and accessible (libraries, schools, Primary Health Care Centre, community and sports centres, parks). Moreover, with the use of different locations more people gets to know the resources and participation is enhanced.
With regard to schedule, they point out that arrangements are generally more difficult for working people, more so since the financial crisis. They suggest schedules that include morning and afternoon. As regards duration and frequency, they propose weekly frequency during 5–6 weeks, duration around 2–2.5 h.
Discussion
In relation to interaction with professionals, participants acknowledged that even though they received advice on health behaviours for the management of knee OA and other conditions, adherence to this advice is difficult. They expressed fear and ambivalence in relation to surgical and pharmacological treatments and suggested that professionals should focus on the needs of the patients, on alleviating pain and on delaying the progression of the disease. These results coincide with various studies that indicate that patients and health professionals felt that OA should receive more attention and better consistency of care, with more emphasis on self-management to help patients manage their condition more effectively and appropriately [8, 30]. Indeed, patient information and education are considered core treatments for OA in evidence-based clinical guidelines. Patients should then use this information to implement changes and for decision-taking regarding treatment [31–34].
Similarly to other qualitative studies, patients explained that knee OA affects the whole body and their lives on many levels [35]. The symptoms experienced illustrate a diversity of problems that represented a major concern for many participants in our study: knee pain, stiffness, difficulties in daily activities, reduction of work, instability, weakness, lack of mobility and psychological impact. Patients with knee osteoarthritis often suffer from obesity/overweight (90%), hypertension (40%), depression (30%) and diabetes (15%), resulting in a decreased quality of life [36]. However, most patients can differentiate when the pain is due to knee osteoarthritis or other conditions.
With regard to psychological impact, we should highlight that most questionnaires that evaluate knee OA and its treatment do not include this factor, probably because there was no involvement of knee OA patients in its design [34]. In this study, participants mentioned the need for research in this area. Indeed, research projects should plan their agendas working with those that should benefit from that research [33]. Since they are best placed to reflect on their experience of an illness, it is essential to collect their opinions to build evidence about their priorities [37] and to enhance the relevance of research. A strength of our study is that we take into account patients’ perspectives. The study protocol [5] explains that the integral management of the patient is paramount in the treatment of knee osteoarthritis. Accordingly, the design of the coaching intervention takes into account other factors such as associated diseases, environment and personal circumstances, all of which are considered during the sessions.
Patients explained that translating theory into practice and modifying behaviour is difficult. They request a holistic vision from professionals, based on their needs and not only on their health problems [38]. The person-centered approach model involves being an active agent for change and a non-directive role of the professional; it is based on unconditional acceptance, empathy and authenticity [39, 40]. Including the patient-centered context in complex interventions implies reflection on how to support optimal health and provision of care by means of reflecting on the patient’s history [41].
The Lazarus [24, 25, 27] model used in the analysis is useful to detect cognitive evaluations and stress coping strategies. Acceptance is one of the key facilitators for coping with different situations [42–44] such as knee osteoarthritis. Working toward acceptance through HC can help patients improve the self-management.
Our findings point at the various difficulties for participants to follow dietary advice: lack of individualisation, anxiety, and prioritizing other aspects of their lives, in particular the people closest to them [30]. Some studies have shown that HC helps people achieve dietary objectives [45–47]. Also in agreement with other studies and despite a positive attitude in relation to PA, we have found barriers to their implementation such as pain, PA habits prior their current condition, lack of social support and lack of acceptance to their current situation [48–50]. According to various authors, HC provides strategies to start and sustain PA levels appropriate to the conditions of individuals [19, 51–56]. Another main result of our study is the importance that participants attach to mood, a key element for setting in motion their internal resources, also observed in previous investigations [34, 57–59]. In summary, health coaching, which originates within the framework of behavioural change, can help people increase their quality of life, their self-efficacy (a determinant factor of behavioural change), their perception of self-control and to reduce stress [30, 60].
Strengths and weaknesses
This research investigates the experiences of patients with mild to moderate knee OA. These experiences constitute an essential information toward the design and implementation of a complex intervention that will be acceptable, adequate, feasible, integrated within other programs, and appropriate in relation to location, schedule and duration. This article corresponds to Phase 1 or Modelling Phase of the MRC framework; the results have been used to design a HC intervention in knee OA intervention [61, 62].
Most participants in our research have suffered from knee OA for long time, are extremely familiar with this condition, understand available interventions and resources and have developed effective coping strategies. Participants spoke extensively about their problems, so that the data obtained were rich and diverse. The theoretical sample was successful in achieving diversity in age, gender, number of years since onset of disease, employment status, treatment modalities and multimorbidity. We should underscore that the mean age of participants in this study is older than the mean age found in the literature. This is a qualitative study that aims to achieve maximum plurality of discourse (minimum age 58 years, maximum age 85). Although the average age in experimental studies on knee osteoarthritis is 62 years of age, the electronic medical records of primary care centres in Barcelona reveal that the mean age of most patients that consult for this condition is closer to 70, the age group most represented in this study.
Nevertheless, the results of our study have been limited because no adults in the pre-diagnostic phase were included and the immigrant population, which might have different experiences, was not represented. The coaching group sessions with a participative strategy could be useful in case of proactive participants and volunteers but not for other profiles. This is a common characteristic of many intervention studies that require voluntary participation. This issue is worth exploring in depth during a qualitative study (phase 3). Further studies should include their discourses. Therefore, caution is needed before transferring these results to other settings and populations. However, the similarity with other studies with people from other origins and cultures suggests its applicability [7–9]. The rigour procedures used (in-depth-description of the context, theoretical sample design, audio-taping transcription, saturation, triangulation of analysis and reflexivity) have ensured the reliability of the findings in our setting.
Conclusions
This study analyses the experiences of patients that suffer from knee OA. Their discourses have been extremely useful for the modelling of the second phase of this study, a clinical trial to compare current treatment with the HC intervention.
Amongst the findings we should highlight the need for a holistic, person-centered approach that takes into account the characteristics and needs of patients and that includes the physical, psychological, social and practical aspects of knee OA.
These patients need empathy in relation to their suffering and psychological distress caused by their condition. They also explain their concern and ambivalence in relation to the use of medicines to control pain and request more research to obtain pharmacological treatment that is more effective and produces less side effects.
Health coaching should emphasize acceptance as a coping strategy. Acceptance is a key factor toward the improvement of quality of life and to decrease the impact of knee OA.
Acknowledgements
We would like to thank all those who participated in this study and took the time to share their experiences; and we would like to the reviewers of this manuscript for their very helpful comments and suggestions.
Funding
The project received a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain), awarded on the 2014 call under the Health Strategy Action 2013–2016, within the National Research Program oriented to Societal Challenges, within the Technical, Scientific and Innovation Research National Plan 2013–2016, with reference PI14/00585, co-funded with European Union ERDF funds. The role of this funding source is only to provide the funds.
Availability of data and materials
All the anonymous text transcription could be available writing the principal investigator. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
VCT, JMQ, EPR, ILG, XM, EBG, MGM, LJF and AB contributed to the conception and design of the study. AB is the scientific director of the project. VC, JM, ILL, EPR and AB did the fieldwork and the triangulation of the analysis. VCT, JMQ, EPR, ILG, XM, EBG, MGM, LJF and AB participated in the interpretation of the final results. VCT, JMQ, EPR, ILG, XM, EBG, MGM, LJF and AB developed the draft manuscript, and read and approved the final manuscript.
Competing interests
The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
Consent for publication
The participants sign the consent form in order to consent to publish the data guaranteeing the confidentiality and anonymity of their data
Ethics approval and consent to participate
This study followed the tenets of the Helsinki Declaration and Good Clinical Research Practice. The family doctors and nurses of all participants provided information about the aim and procedures of the study. All participants signed a written informed consent form at the beginning of the interview. The confidentiality and anonymity of the data was ensured through a code. This code was used to identify the selected verbatim-transcripts.
The project was approved by the Ethics and Clinical Research Committee of the Primary Care Research Institute Jordi Gol (P13/011). The audio and video archives will be eliminated after 5 years.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Interview guide. (DOCX 16 kb)
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s12891-017-1584-3) contains supplementary material, which is available to authorized users.
Contributor Information
Victoria Carmona-Terés, Email: victoriacarmona@copc.cat.
Jenny Moix-Queraltó, Email: jenny.moix@uab.cat.
Enriqueta Pujol-Ribera, Email: epujol@idiapjgol.org.
Iris Lumillo-Gutiérrez, Email: irislumillo@gmail.com.
Xavier Mas, Email: 22716xmg@comb.cat.
Enrique Batlle-Gualda, Email: enrique.batlle@gmail.com.
Milena Gobbo-Montoya, Email: milena.gobbo@gmail.com.
Lina Jodar-Fernández, Email: ljodar74@gmail.com.
Anna Berenguera, Phone: +34 93 482 44 25, Email: aberenguera@idiapjgol.org, http://www.idiapjgol.org.
References
- 1.Mas X, Barraquer ME. Gonalgia. Actualización en Medicina de Familia 3[5] 2013. pp. 249–258. [Google Scholar]
- 2.Pagès-Castellà, A., Muñoz Ortego, J., Prieto-Alhambra, D. Guía artrosis [http://www.ics.gencat.cat/3clics/main.php]. Barcelona: [updated January 25, 2013; Accessed 26 Jan 2013]. At http://www.ics.gencat.cat/3clics/main.php?page=GuiaPage&idGuia=238. 2013.
- 3.Bennell KL, Hunter DJ, Hinman RS. Management of osteoarthritis of the knee. BMJ. 2012;345:e4934. doi: 10.1136/bmj.e4934. [DOI] [PubMed] [Google Scholar]
- 4.Fernandes L, Hagen KB, Bijlsma JW, Andreassen O, Christensen P, Conaghan PG, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72:1125–1135. doi: 10.1136/annrheumdis-2012-202745. [DOI] [PubMed] [Google Scholar]
- 5.Carmona-Teres V, Lumillo-Gutierrez I, Jodar-Fernandez L, Rodriguez-Blanco T, Moix-Queralto J, Pujol-Ribera E, et al. Effectiveness and cost-effectiveness of a health coaching intervention to improve the lifestyle of patients with knee osteoarthritis: cluster randomized clinical trial. BMC Musculoskelet Disord. 2015;16:38. doi: 10.1186/s12891-015-0501-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maly MR, Krupa T. Personal experience of living with knee osteoarthritis among older adults. Disabil Rehabil. 2007;29:1423–1433. doi: 10.1080/09638280601029985. [DOI] [PubMed] [Google Scholar]
- 7.Nyvang J, Hedstrom M, Gleissman SA. It’s not just a knee, but a whole life: a qualitative descriptive study on patients’ experiences of living with knee osteoarthritis and their expectations for knee arthroplasty. Int J Qual Stud Health Well -being. 2016;11:30193. doi: 10.3402/qhw.v11.30193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kao MH, Tsai YF. Illness experiences in middle-aged adults with early-stage knee osteoarthritis: findings from a qualitative study. J Adv Nurs. 2014;70:1564–1572. doi: 10.1111/jan.12313. [DOI] [PubMed] [Google Scholar]
- 9.Pouli N, Das NR, Lincoln NB, Walsh D. The experience of living with knee osteoarthritis: exploring illness and treatment beliefs through thematic analysis. Disabil Rehabil. 2014;36:600–607. doi: 10.3109/09638288.2013.805257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michie S. Designing and implementing behaviour change interventions to improve population health. J Health Serv Res Policy. 2008;13(Suppl 3):64–69. doi: 10.1258/jhsrp.2008.008014. [DOI] [PubMed] [Google Scholar]
- 11.Linden A, Butterworth SW, Prochaska JO. Motivational interviewing-based health coaching as a chronic care intervention. J Eval Clin Pract. 2010;16:166–174. doi: 10.1111/j.1365-2753.2009.01300.x. [DOI] [PubMed] [Google Scholar]
- 12.Huffman MH. HEALTH COACHING: a fresh, new approach to improve quality outcomes and compliance for patients with chronic conditions. Home Healthc Nurse. 2009;27:490–496. doi: 10.1097/01.NHH.0000360924.64474.04. [DOI] [PubMed] [Google Scholar]
- 13.Thom DH, Hessler D, Willard-Grace R, DeVore D, Prado C, Bodenheimer T, et al. Health coaching by medical assistants improves patients’ chronic care experience. Am J Manag Care. 2015;21:685–691. [PubMed] [Google Scholar]
- 14.Liddy C, Johnston S, Irving H, Nash K, Ward N. Improving awareness, accountability, and access through health coaching: qualitative study of patients’ perspectives. Can Fam Physician. 2015;61:e158–e164. [PMC free article] [PubMed] [Google Scholar]
- 15.McGloin H, Timmins F, Coates V, Boore J. A case study approach to the examination of a telephone-based health coaching intervention in facilitating behaviour change for adults with Type 2 diabetes. J Clin Nurs. 2015;24:1246–1257. doi: 10.1111/jocn.12692. [DOI] [PubMed] [Google Scholar]
- 16.Thom DH, Ghorob A, Hessler D, De VD, Chen E, Bodenheimer TA. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013;11:137–144. doi: 10.1370/afm.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Varney JE, Weiland TJ, Inder WJ, Jelinek GA. Effect of hospital-based telephone coaching on glycaemic control and adherence to management guidelines in type 2 diabetes, a randomised controlled trial. Intern Med J. 2014;44:890–897. doi: 10.1111/imj.12515. [DOI] [PubMed] [Google Scholar]
- 18.Wayne N, Perez DF, Kaplan DM, Ritvo P. Health coaching reduces HbA1c in type 2 diabetic patients from a lower-socioeconomic status community: a randomized controlled trial. J Med Internet Res. 2015;17:e224. doi: 10.2196/jmir.4871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willard-Grace R, DeVore D, Chen EH, Hessler D, Bodenheimer T, Thom DH. The effectiveness of medical assistant health coaching for low-income patients with uncontrolled diabetes, hypertension, and hyperlipidemia: protocol for a randomized controlled trial and baseline characteristics of the study population. BMC Fam Pract. 2013;14:27. doi: 10.1186/1471-2296-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Hara BJ, Phongsavan P, Venugopal K, Eakin EG, Eggins D, Caterson H, et al. Effectiveness of Australia’s Get Healthy Information and Coaching Service(R): translational research with population wide impact. Prev Med. 2012;55:292–298. doi: 10.1016/j.ypmed.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 21.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50:587–592. doi: 10.1016/j.ijnurstu.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 23.Reeves S, Albert M, Kuper A, Hodges BD. Why use theories in qualitative research? BMJ. 2008;337:a949. doi: 10.1136/bmj.a949. [DOI] [PubMed] [Google Scholar]
- 24.Lazarus RS, Folkman S, Folkman S: Estrés y procesos cognitivos. Barcelona: Martínez Roca; 1986.
- 25.Lazarus RS. Emotions and interpersonal relationships: toward a person-centered conceptualization of emotions and coping. J Pers. 2006;74:9–46. doi: 10.1111/j.1467-6494.2005.00368.x. [DOI] [PubMed] [Google Scholar]
- 26.Moix J. Análisis de los factores psicológicos moduladores del dolor crónico benigno. Anuario de Psicología. 2005;36:37–60. [Google Scholar]
- 27.Lazarus FS. Estrés y emoción. Manejo e implicaciones en nuestra salud. Bilbao: Desclée de Brower; 2000. [Google Scholar]
- 28.Tuckett AG. Qualitative research sampling: the very real complexities. Nurse Res 2004. 2004;12:47–61. doi: 10.7748/nr2004.07.12.1.47.c5930. [DOI] [PubMed] [Google Scholar]
- 29.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 30.Mann C, Gooberman-Hill R. Health care provision for osteoarthritis: concordance between what patients would like and what health professionals think they should have. Arthritis Care Res (Hoboken) 2011;63:963–972. doi: 10.1002/acr.20459. [DOI] [PubMed] [Google Scholar]
- 31.Moe RH, Haavardsholm EA, Grotle M, Steen E, Kjeken I, Hagen KB, et al. Development of a brief multidisciplinary education programme for patients with osteoarthritis. BMC Musculoskelet Disord. 2011;12:257. doi: 10.1186/1471-2474-12-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chard J, Dickson J, Tallon D, Dieppe P. A comparison of the views of rheumatologists, general practitioners and patients on the treatment of osteoarthritis. Rheumatology (Oxford) 2002;41:1208–1210. doi: 10.1093/rheumatology/41.10.1208-b. [DOI] [PubMed] [Google Scholar]
- 33.Tallon D, Chard J, Dieppe P. Relation between agendas of the research community and the research consumer. Lancet. 2000;355:2037–2040. doi: 10.1016/S0140-6736(00)02351-5. [DOI] [PubMed] [Google Scholar]
- 34.Tallon D, Chard J, Dieppe P. Exploring the priorities of patients with osteoarthritis of the knee. Arthritis Care Res. 2000;13:312–319. doi: 10.1002/1529-0131(200010)13:5<312::AID-ANR11>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 35.Sociedad Española de Medicina de Familia y Comunitaria. E, Mas Lodo N, Martín Blázquez M, Raja Casillas M, Izquierdo Zamarriego M, Valles Fernández N, Metola Gómez M. What underlies goalgia in general population? Atención Primaria. 2017;215–219. [PubMed]
- 36.Hunter DJ. Ostheoarthritis: Managing this chronic disease. Sidney: New Agency for Clinical Innovation. 2013.
- 37.Royle J, Oliver S. Consumer involvement in the health technology assessment program. Int J Technol Assess Health Care. 2004;20:493–497. doi: 10.1017/S0266462304001412. [DOI] [PubMed] [Google Scholar]
- 38.Codern-Bove N, Pujol-Ribera E, Pla M, Gonzalez-Bonilla J, Granollers S, Ballve JL, et al. Motivational interviewing interactions and the primary health care challenges presented by smokers with low motivation to stop smoking: a conversation analysis. BMC Public Health. 2014;14:1225. doi: 10.1186/1471-2458-14-1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alharbi TS, Carlstrom E, Ekman I, Jarneborn A, Olsson LE. Experiences of person-centred care - patients’ perceptions: qualitative study. BMC Nurs. 2014;13:28. doi: 10.1186/1472-6955-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Astin F, Horrocks J, Closs SJ. Managing lifestyle change to reduce coronary risk: a synthesis of qualitative research on peoples’ experiences. BMC Cardiovasc Disord. 2014;14:96. doi: 10.1186/1471-2261-14-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Constand MK, MacDermid JC, Dal Bello-Haas V, Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. 2014;14:271. doi: 10.1186/1472-6963-14-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clarke SP, Poulis N, Moreton BJ, Walsh DA, Lincoln NB: Evaluation of a group acceptance commitment therapy intervention for people with knee or hip osteoarthritis: a pilot randomized controlled trial. Disabil Rehabil. 2017;39:663–70. [DOI] [PubMed]
- 43.Trompetter HR, Bohlmeijer ET, Lamers SM, Schreurs KM. Positive psychological wellbeing is required for online self-help acceptance and commitment therapy for chronic pain to be effective. Front Psychol. 2016;7:353. doi: 10.3389/fpsyg.2016.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45:5–31. doi: 10.1080/16506073.2015.1098724. [DOI] [PubMed] [Google Scholar]
- 45.Martin LA, Critelli JW, Doster JA, Powers C, Purdum M, Doster MR, et al. Cardiovascular risk: gender differences in lifestyle behaviors and coping strategies. Int J Behav Med. 2013;20:97–105. doi: 10.1007/s12529-011-9204-3. [DOI] [PubMed] [Google Scholar]
- 46.Somers TJ, Blumenthal JA, Guilak F, Kraus VB, Schmitt DO, Babyak MA, et al. Pain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled study. Pain. 2012;153:1199–1209. doi: 10.1016/j.pain.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deasy C, Coughlan B, Pironom J, Jourdan D, Mcnamara PM. Psychological distress and lifestyle of students: implications for health promotion. Health Promot Int. 2015;30:77–87. doi: 10.1093/heapro/dau086. [DOI] [PubMed] [Google Scholar]
- 48.Ekkekakis P, Vazou S, Bixby WR, Georgiadis E. The mysterious case of the public health guideline that is (almost) entirely ignored: call for a research agenda on the causes of the extreme avoidance of physical activity in obesity. Obes Rev. 2016;17:313–329. doi: 10.1111/obr.12369. [DOI] [PubMed] [Google Scholar]
- 49.Murphy SL, Kratz AL, Williams DA, Geisser ME. The association between symptoms, pain coping strategies, and physical activity among people with symptomatic knee and hip osteoarthritis. Front Psychol. 2012;3:326. doi: 10.3389/fpsyg.2012.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hendry M, Williams NH, Markland D, Wilkinson C, Maddison P. Why should we exercise when our knees hurt? a qualitative study of primary care patients with osteoarthritis of the knee. Fam Pract. 2006;23:558–567. doi: 10.1093/fampra/cml022. [DOI] [PubMed] [Google Scholar]
- 51.Bennell KL, Egerton T, Bills C, Gale J, Kolt GS, Bunker SJ, et al. Addition of telephone coaching to a physiotherapist-delivered physical activity program in people with knee osteoarthritis: a randomised controlled trial protocol. BMC Musculoskelet Disord. 2012;13:246. doi: 10.1186/1471-2474-13-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brodin N, Lohela-Karlsson M, Swardh E, Opava CH. Cost-effectiveness of a one-year coaching program for healthy physical activity in early rheumatoid arthritis. Disabil Rehabil. 2015;37:757–762. doi: 10.3109/09638288.2014.940429. [DOI] [PubMed] [Google Scholar]
- 53.Demmelmaier I, Lindkvist A, Nordgren B, Opava CH. “A gift from heaven” or “This was not for me”. A mixed methods approach to describe experiences of participation in an outsourced physical activity program for persons with rheumatoid arthritis. Clin Rheumatol. 2015;34:429–439. doi: 10.1007/s10067-014-2723-y. [DOI] [PubMed] [Google Scholar]
- 54.Hinman RS, Delany CM, Campbell PK, Gale J, Bennell KL. Physical Therapists, Telephone Coaches, and Patients With Knee Osteoarthritis: Qualitative Study About Working Together to Promote Exercise Adherence. Phys Ther. 2015. [DOI] [PubMed]
- 55.Knittle K, De Gucht V, Hurkmans E, Peeters A, Ronday K, Maes S, et al. Targeting motivation and self-regulation to increase physical activity among patients with rheumatoid arthritis: a randomised controlled trial. Clin Rheumatol. 2015;34:231–238. doi: 10.1007/s10067-013-2425-x. [DOI] [PubMed] [Google Scholar]
- 56.Sahlen KG, Johansson H, Nystrom L, Lindholm L. Health coaching to promote healthier lifestyle among older people at moderate risk for cardiovascular diseases, diabetes and depression: a study protocol for a randomized controlled trial in Sweden. BMC Public Health. 2013;13:199. doi: 10.1186/1471-2458-13-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.DeLongis A, Folkman S, Lazarus RS. The impact of daily stress on health and mood: psychological and social resources as mediators. J Pers Soc Psychol. 1988;54:486–495. doi: 10.1037/0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- 58.Cheng C, Lau HP, Chan MP. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychol Bull. 2014;140:1582–1607. doi: 10.1037/a0037913. [DOI] [PubMed] [Google Scholar]
- 59.Folling IS, Solbjor M, Helvik AS. Previous experiences and emotional baggage as barriers to lifestyle change - a qualitative study of Norwegian Healthy Life Centre participants. BMC Fam Pract. 2015;16:73. doi: 10.1186/s12875-015-0292-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McKenzie SH, Harris MF. Understanding the relationship between stress, distress and healthy lifestyle behaviour: a qualitative study of patients and general practitioners. BMC Fam Pract. 2013;14:166. doi: 10.1186/1471-2296-14-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jagosh J, Bush PL, Salsberg J, Macaulay AC, Greenhalgh T, Wong G, et al. A realist evaluation of community-based participatory research: partnership synergy, trust building and related ripple effects. BMC Public Health. 2015;15:725. doi: 10.1186/s12889-015-1949-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Prufer F, Joos S, Miksch A. What do resource-oriented approaches mean to general practitioners and how can they be facilitated in primary care? a qualitative study. Evid Based Complement Alternat Med. 2013;2013:187641. doi: 10.1155/2013/187641. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the anonymous text transcription could be available writing the principal investigator. The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.


