Abstract
Background
Acute diarrhoea is one of the main causes of morbidity and mortality among children in low‐income countries. Glucose‐based oral rehydration solution (ORS) helps replace fluid and prevent further dehydration from acute diarrhoea. Since 2004, the World Health Organization (WHO) has recommended the osmolarity of less than 270 mOsm/L (ORS ≤ 270) versus greater than 310 mOsm/L formulation (ORS ≥ 310). Polymer‐based ORS (for example, prepared using rice or wheat) slowly releases glucose and may be superior to glucose‐based ORS.
Objectives
To compare polymer‐based oral rehydration solution (polymer‐based ORS) with glucose‐based oral rehydration solution (glucose‐based ORS) for treating acute watery diarrhoea.
Search methods
We searched the following sources up to 5 September 2016: the Cochrane Infectious Diseases Group (CIDG) Specialized Register, the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library 2016, Issue 9), MEDLINE (1966 to 5 September 2016), EMBASE (1974 to 5 September 2016), LILACS (1982 to 5 September 2016), and mRCT (2007 to 5 September 2016). We also contacted researchers, organizations, and pharmaceutical companies, and searched reference lists.
Selection criteria
We included randomized controlled trials (RCTs) of people with acute watery diarrhoea (cholera and non‐cholera associated) that compared polymer‐based and glucose‐based ORS (with identical electrolyte contents).
Data collection and analysis
Two review authors independently assessed the search results and risk of bias, and extracted data. In multiple‐treatment arms with two or more treatment groups, we combined outcomes as appropriate and compared collectively with the control group.
Main results
Thirty‐five trials that included 4284 participants met the inclusion criteria: 28 trials exclusively included children, five included adults, and two included both adults and children.
Polymer‐based ORS versus glucose‐based ORS (osmolarity ≤ 270)
Eight trials (752 participants) evaluated this comparison, and seven trials used rice as a polymer source. Polymer‐based ORS may decrease mean stool output in the first 24 hours by 24 mL/kg (mean difference (MD) −24.60 mL/kg, 95% CI −40.69 to −8.51; one trial, 99 participants, low quality evidence). The average duration of diarrhoea may be reduced by eight hours (MD −8.24 hours, 95% CI −13.17 to −3.30; I² statistic = 86%, five trials, 364 participants, low quality evidence) with polymer ORS but results are heterogeneous. Limited trials showed no observed difference in the risk of unscheduled use of intravenous fluid (RR 0.66, 95% CI 0.43 to 1.02; I² statistic = 30%; four trials, 376 participants, very low quality evidence), vomiting (very low quality evidence), and hyponatraemia (very low quality evidence).
Polymer‐based ORS versus glucose‐based ORS (osmolarity ≥ 310)
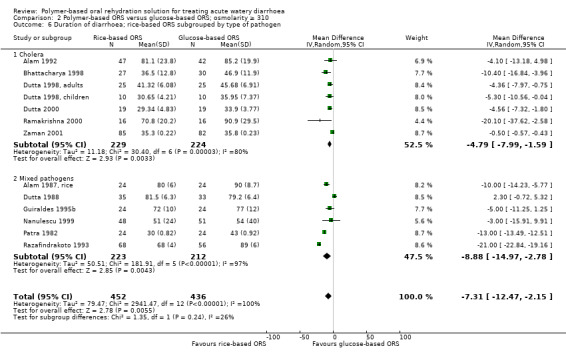
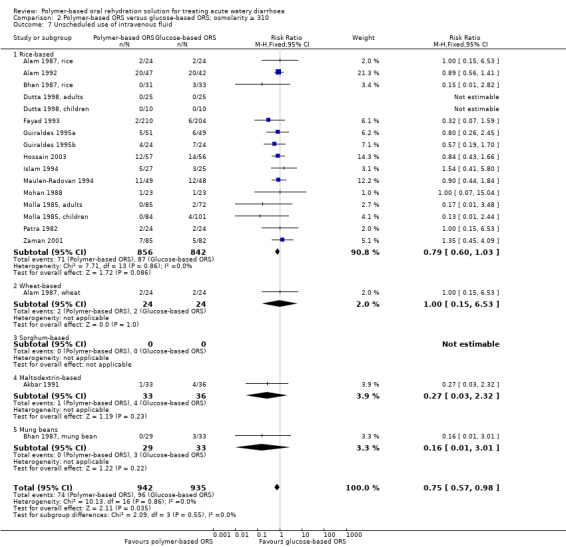
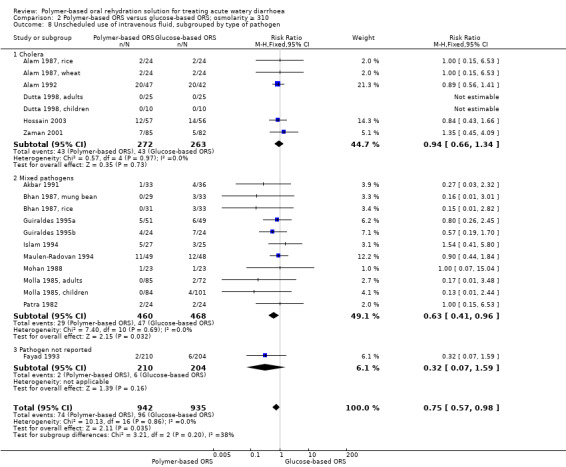
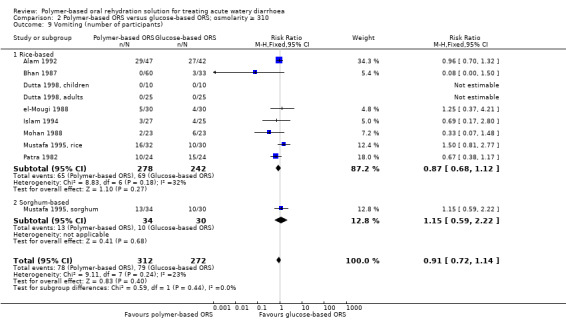
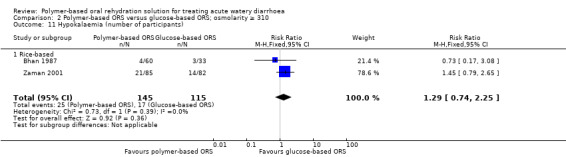
Twenty‐seven trials (3532 participants) evaluated this comparison using a variety of polymers. On average, polymer ORS may reduce the total stool output in the first 24 hours by around 65 mL/kg (MD −65.47 mL/kg, 95% CI −83.92 to −47.03; 16 trials, 1483 participants, low quality evidence), and may reduce the duration of diarrhoea by around eight hours (MD −8.57 hours; SD −13.17 to −4.03; 16 trials, 1137 participants, low quality evidence) with substantial heterogeneity. The proportion of participants that required intravenous hydration was low in most trials with fewer in the polymer ORS group (RR 0.75, 95% CI 0.57 to 0.98; 19 trials, 1877 participant, low quality evidence) . Subgroup analysis by type of pathogen suggested an effect on unscheduled intravenous fluid in those infected with mixed pathogens (RR 0.63, 95% CI 0.41 to 0.96; 11 trials, 928 participants, low quality evidence), but not in participants positive for Vibrio cholerae (RR 0.94, 95% CI 0.66 to 1.34; 7 trials, 535 participants, low quality evidence). No difference was observed in the number of patients who developed vomiting (RR 0.91, 95% CI 0.72 to 1.14; 10 trials, 584 participants, very low quality evidence), hyponatraemia (RR 1.82, 95% CI 0.52 to 6.44; 4 trials, 385 participants, very low quality evidence), hypokalaemia (RR 1.29, 95% CI 0.74 to 2.25; 2 trials, 260 participants, low quality evidence), or persistent diarrhoea (RR 1.28, 95% CI 0.68 to 2.41; 2 trials, 885 participants, very low quality evidence).
Authors' conclusions
Polymer‐based ORS shows advantages compared to glucose‐based ORS (at ≥ 310 mOsm/L). Comparisons favoured polymer‐based ORS over ORS ≤ 270 but analysis was underpowered.
15 April 2019
No update planned
Other
This is not a current research question
Keywords: Adult, Child, Humans, Infant, Acute Disease, Cholera, Cholera/complications, Dehydration, Dehydration/etiology, Dehydration/therapy, Diarrhea, Diarrhea/complications, Diarrhea/therapy, Fluid Therapy, Fluid Therapy/methods, Oryza, Polymers, Polymers/therapeutic use, Randomized Controlled Trials as Topic, Rehydration Solutions, Rehydration Solutions/chemistry, Rehydration Solutions/therapeutic use
Plain language summary
Food‐based oral rehydration solution for acute diarrhoea
What is polymer‐based ORS and how might it help
Acute diarrhoea is a common cause of death and illness in developing countries. Oral rehydration solutions (ORS) have had a massive impact worldwide in reducing the number of deaths related to diarrhoea.
The original ORS was based on glucose and had an osmolarity of ≥ 310 mOsm/L (ORS ≥ 310). Glucose‐based ORS with a lower osmolarity was later introduced in attempts to improve efficacy, and is considered better at reducing the amount and duration of diarrhoea. Most ORS is in the form of a sugar–salt solution, but over the years people have tried adding a variety of compounds ('glucose polymers') such as whole rice, wheat, sorghum, and maize. The aim is to slowly release glucose into the gut and improve the absorption of the water and salt in the solution.
This review updates a Cochrane Review published in 2009, and assesses the available evidence on the use of polymer‐based ORS (both rice and non‐rice based) versus glucose‐based ORS.
What the research says
Cochrane researchers examined the available evidence up to 5 September 2016. Thirty‐five trials including 4284 participants met the inclusion criteria: 28 trials included children; five included adults; and two included both. Most trials compared polymer‐based ORS with a sugar–salt ORS with a particular strength (ORS ≥ 310), which is slightly more salty than the currently agreed best formula (≤ 270 mOsm/L). The trials' methodological quality varied.
In people given polymer‐based ORS versus sugar‐salt ORS ≤ 270 mOsm/L there was insufficient evidence to show that one is better than the other (low tovery low quality of evidence).
In those given polymer‐based ORS versus sugar‐salt ORS ≥ 310 mOsm/L, there was a lower amount of stool and shorter time of diarrhoea in the polymer‐based ORS group. No difference was observed between the two groups regarding the number of people who needed a drip to be rehydrated. Adverse events were similar (low tovery low quality of evidence).
Summary of findings
Summary of findings for the main comparison. 'Summary of findings' table 1.
| Polymer‐based ORS compared to glucose‐based ORS ≤ 270 mOsm/L for treating acute watery diarrhoea | |||||
| Patient or population: adults and children with acute watery diarrhoea Settings: primary and secondary healthcare services Intervention: polymer based ORS Comparison: glucose‐based ORS ≤ 270 mOsm/L | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Glucose‐based ORS | Polymer‐based ORS | ||||
| Total stool output during first 24 hours | The mean stool output in the control group was 102 mL/kg |
The mean stool output in the intervention group was 24.60 mL/kg lower (40.69 to 8.51 lower) | — | 99 (1 trial) | ⊕⊕⊝⊝ low1,2,3 |
| Duration of diarrhoea | The mean duration in the control groups ranged from 33.9 to 90.9 hours | The mean duration of diarrhoea in the intervention groups was 8.24 hours shorter (13.17 to 3.30 hours shorter) | — | 364 (5 trials) | ⊕⊕⊝⊝ low4,5,6 |
| Unscheduled use of intravenous fluid | 9 per 100 | 6 per 100 (3 to 10) | RR 0.66 (0.43 to 1.02) | 376 (4 trials) | ⊕⊝⊝⊝ very low4,6,7 |
| Vomiting | 35 per 100 |
20 per 100 (8 to 47) |
RR 0.56 (0.24 to 1.34) |
63 (1 trial) |
⊕⊝⊝⊝8,9,10 very low |
| Hyponatraemia | 23 per 100 |
18 per 100 (8 to 40) |
RR 0.88 (0.43 to 1.82) |
145 (3 trials) |
⊕⊝⊝⊝1,7,11 very low |
| The assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Abbreviations: CI: confidence interval; GRADE: Grading of Recommendations Assessment, Development and Evaluation; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | |||||
1Downgraded by 1 for serious risk of bias: the method of allocation concealment was unclear, and there was no blinding. 2Downgraded by 2 for indirectness: this single study was from a single setting in a paediatric clinic in Romania. The findings may not be broadly applicable to elsewhere. 3No serious imprecision: the result is both clinically important and statistically significant. 4Downgraded by 1 for serious risk of bias: only 1 study had adequate allocation concealment and the rest were unclear. No study was completely blinded. 5No serious heterogeneity: although statistical heterogeneity between studies was high, almost all trials favoured polymer ORS but there was heterogeneity in the magnitude of the effect. 6Downgraded by 1 serious indirectness: only 1 of these studies was conducted in a primary care setting. Most trials were in hospital settings. 7Downgraded by 1 for imprecision: the trials are small and the 95% CI is wide and includes clinically important effects and no effect. 8Downgraded by 1 for serious risk of bias. The allocation sequence and concealment were both unclear and there was no blinding. 9Downgraded by 1 for indirectness: this single study was from a single setting in a hospital in Thailand. The findings may not be broadly applicable to elsewhere. 10Downgraded by 1 for imprecision: the trial is small and the 95% CI is wide and includes clinically important effects and no effect. 11Downgraded by 1 for indirectness: all three trials were done in hospital setting. The findings may not be broadly applicable to elsewhere.
Summary of findings 2. 'Summary of findings' table 2.
| Polymer‐based ORS compared to glucose‐based ORS ≥ 310 mOsm/L for treating acute watery diarrhoea | |||||
| Patient or population: adults and children with acute watery diarrhoea Settings: primary and secondary healthcare services Intervention: polymer based ORS Comparison: glucose‐based ORS ≥ 310 mOsm/L | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Glucose‐based ORS | Polymer‐based ORS | ||||
| Total stool output during first 24 hours | The mean stool output in the control groups ranged from 81 to 366 mL/kg |
The mean stool output in the intervention groups was 65.47 mL/kg lower (47.03 to 83.92 lower) | — | 1483 (16 trials) | ⊕⊕⊝⊝ low1,2,3,4 |
| Duration of diarrhoea | The mean duration in the control groups ranged from 24.3 to 90.9 hours | The mean duration of diarrhoea in the intervention groups was 8.47 hours shorter (12.86 to 4.08 hours shorter) | — | 1187 (16 trials) | ⊕⊕⊝⊝ low1,2,3,4 |
| Unscheduled use of intravenous fluid | 102 per 1000 | 79 per 1000 (61 to 103) | RR 0.75 (0.57 to 0.98) | 1877 (19 trials) | ⊕⊕⊝⊝ low1,3,4,5 |
| Unscheduled use of intravenous fluid in those with mixed pathogen | 101 per 1000 |
63 per 1000 (31 to 60) |
RR 0.63 (0.49 to 0.96) |
928 (11 trials) | ⊕⊕⊝⊝ low1,3,4,5 |
| Unscheduled use of intravenous fluid in those with Cholera | 159 per 1000 |
150 per 1000 (105 to 213) |
RR 0.94 (0.66 to 1.34) |
535 (7 trials) | ⊕⊕⊝⊝ low1,3,4,5 |
| Vomiting | 313 per 1000 |
250 per 1000 (197 to 313) |
RR 0.91 (0.72 to 1.14) |
584 (10 trials) |
⊕⊝⊝⊝ very low1,3,5,6 |
| Hyponatraemia | 16 per 1000 |
30 per 1000 (9 to 104) |
RR 1.82 (0.52 to 6.44) |
385 (4 trials) |
⊕⊝⊝⊝ very low1,3,5,6 |
| Hypokalaemia | 148 per 1000 |
191 per 1000 (110 to 333) |
RR 1.29 (0.74 to 2.25) |
260 (2 trials) |
⊕⊕⊝⊝ low1,6,8,9 |
| Development of persistent diarrhoea | 17 per 1000 |
21 per 1000 (6 to 78) |
RR 1.28 (0.68 to 2.41) |
885 (2 trials) |
⊕⊝⊝⊝6,10,11 very low |
| The assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). Abbreviations: CI: confidence interval; GRADE: Grading of Recommendations Assessment, Development and Evaluation; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | |||||
1Downgraded by 1 for serious risk of bias: most trials were at high risk of selection bias due to a lack of allocation concealment, and most were at high risk of detection or reporting bias due to a lack of blinding. 2No serious inconsistency: although there is considerable heterogeneity between studies, all studies favoured polymer ORS but there was heterogeneity in the magnitude of this effect. Not downgraded. 3Downgraded by 1 for indirectness: most trials were from hospital settings not primary healthcare or community settings. 4No serious imprecision: the meta‐analysis is adequately powered. The result is statistically significant and clinically important. 5No serious inconsistency: statistical heterogeneity was low. 6Downgraded by 1 for serious imprecision: the 95% CI is wide and includes both clinically important effects and no effect. 7Downgraded by 1 for imprecision: the trial is small and the 95% CI is wide. 8No serious inconsistency: statistical heterogeneity was low but there was heterogeneity in the magnitude of this effect. Not downgraded 9No serious indirectness. One trial was in a hospital and the other in a rural treatment centre 10Downgraded by 1 for serious risk of bias. Only one trial had adequate allocation sequence and concealment, the other one was unclear. There was no blinding in both trials. 11Downgraded by 1 for indirectness. Both trials were conducted in a hospital setting.
Background
Description of the condition
Acute diarrhoea is defined as three or more loose bowel movements in a 24‐hour period (WHO/icddr,b 1995), and is one of the principal causes of morbidity and mortality among children in low‐income countries. Kosek 2003, a review of 27 prospective studies from 20 countries published from 1990 to 2000, estimated the incidence of diarrhoea as 3.8 episodes per child per year for children under 11 months of age and 2.1 episodes per child per year for children aged one to four years. It has a negative impact on quality of life and can result in considerable healthcare costs. Most of these diarrhoeal illnesses occur in low‐income countries and are mainly caused by infection. The cause is mainly viral in children aged under five years, while both bacterial and viral pathogens are implicated in adults (Casburn‐Jones 2004). Other causes of acute diarrhoea are disordered motility, such as irritable bowel syndrome, intake of certain drugs, or ileal bile acid malabsorption.
Description of the intervention
Since the 1980s, efforts to reduce the number of deaths from diarrhoea have been based on several interventions, including the improvement of water quality and sanitation, promotion of breastfeeding, and the introduction of treatment programmes that include oral rehydration therapy (Claeson 1990). The World Health Organization (WHO) introduced the oral rehydration solution (ORS) in 1979, and it rapidly became the cornerstone of programmes for the control of diarrhoeal diseases (Claeson 1990). The osmolarity of the original formulation is 310 mOsm/L (referred to as ORS ≥ 310) and consists of glucose (111 mmol/L), sodium (90 mmol/L), potassium (20 mmol/L), chloride (80 mmol/L), and citrate (10 mmol/L) or bicarbonate (30 mmol/L). The ORS was shown to improve signs of dehydration, including thirst, sunken eyeballs, sunken fontanelles, poor skin turgor, or a decreased or absence of urine output (WHO/icddr,b 1995). It was considered to be both safe and effective (Santosham 1991), and mainly responsible for the decrease in case‐fatality rates from acute dehydrating diarrhoea (Victora 2000). In 2004, the WHO recommended a different formulation in which the glucose and sodium content were each reduced to 75 mmol/L to give a total osmolarity of 245 mOsm/L (referred to as ORS ≤ 270) (WHO 2004). The ORS ≤ 270 reduces stool volume, shortens the duration of diarrhoea, and decreases the need for unscheduled intravenous therapy compared with ORS ≥ 310 (Hahn 2002).
How the intervention might work
The physiological basis for the use of ORS ≥ 310 was the co‐transport of glucose and sodium across the intestinal membrane (Santosham 1991). While this glucose‐based ORS is effective in replacing the fluid from acute diarrhoea and thus prevents further dehydration, it neither reduces stool loss nor shortens the duration of illness (Santosham 1991). Increasing the glucose concentration to greater than 111 mmol/L increases the osmotic load of the solution, which may further aggravate the fluid loss and induce hypernatraemia (Hunt 1992). In recent years, the WHO has recommended an ORS with 75 mmol/L of sodium, 75 mmol/L of glucose, and a total osmolarity of 245 mmol/L (ORS ≤ 270).
The biochemical basis for the use of a polymer‐based ORS is the presence of starch in rice, wheat, sorghum, and some fruits and vegetables (Carpenter 1988; Pizarro 1991). Even during diarrhoea, the digesting enzyme (amylase) is present in large amounts in the small intestine, so this starch is slowly broken down into glucose molecules. This glucose in turn provides the carrier molecules for co‐transport of sodium and water across the intestinal epithelium, without the corresponding osmotic penalty that results if the quantity of glucose is further increased by the use of ORS ≥ 310.
Why it is important to do this review
New ORS formulations have been evaluated in attempts to improve the efficacy of ORS ≥ 310 (Molla 1985; Fontaine 1998; Hoekstra 2004). Glucose polymer‐based ORS (referred to as polymer‐based ORS) may contain whole rice (amylopectins), as in rice‐based ORS or rice syrups (maltodextrins). The difference is that the latter contains only a small amount of amino acids and protein. Other sources of polymers are wheat, sorghum, and maize (high amylase‐resistant starch). In these polymer‐based solutions, the glucose is slowly released after digestion and is absorbed in the small bowel, which enhances the reabsorption of water and electrolyte secreted into the bowel lumen during diarrhoea (Carpenter 1988; Pizarro 1991). Although ORS ≥ 310 is no longer recommended, it remains unknown whether a polymer‐based ORS is indeed more effective than a glucose‐based ORS (that is, ORS ≥ 310 or ORS ≤ 270).
A Cochrane Review of rice‐based ORS for treating diarrhoea concluded that it significantly reduced the mean 24‐hour stool output in adults and children with cholera or cholera‐like diarrhoea, but results were inconclusive for infants and children with non‐cholera diarrhoea (Fontaine 1998). In this Cochrane Review, we have updated the evidence on the use of polymer‐based ORS (both rice‐based ORS and non‐rice based ORS) and expanded the primary outcome measures to include the number of participants who required unscheduled use of intravenous fluid therapy. Other primary outcome measures focus on the duration of diarrhoea and the stool output in the first 24 hours since these are considered crucial in the management of these patients and the first 24 hours is the time period of greatest stool loss. Our Cochrane Review also aims to provide more insights into whether polymer‐based ORS is more effective than glucose‐based ORS, and to inform future research.
Patients are dehydrated during the first six to eight hours, but once rehydrated, feeding is initiated and stool losses are replaced volume per volume with the ORS. The effect of feeding a rice‐based or starch‐based food as soon as the participants are rehydrated could confound the effects of glucose polymer‐based ORS (Alam 1992).
Objectives
To compare polymer‐based oral rehydration solution (polymer‐based ORS) with glucose‐based oral rehydration solution (glucose‐based ORS) for treating acute watery diarrhoea.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs).
Types of participants
Infants, children, and adults with acute watery diarrhoea (cholera and non‐cholera associated) and mild, moderate, or severe dehydration, as defined by the trial authors.
We excluded trials that included participants who were unable to drink or take in oral fluids, those in shock, and those with bloody diarrhoea or dysentery.
Types of interventions
Intervention
Polymer‐based oral rehydration solution (polymer‐based ORS): ORS in which glucose was replaced by a commercial or a local preparation of a polymer (for example, rice, wheat, maltodextrins, maize, sorghum, or corn), the electrolyte composition remaining unchanged between the two solutions.
Control
Glucose‐based ORS: ORS that contains glucose as a carbohydrate source with either 90 or 60 to 75 mmol/L of sodium.
Types of outcome measures
Primary outcomes
Total stool output (g/kg) during the first 24 hours after randomization.
Total stool output (g/kg) from randomization to cessation of diarrhoea.
Duration of diarrhoea (hours) from randomization until cessation of diarrhoea.
Secondary outcomes
Unscheduled intravenous fluid therapy.
Cases of vomiting.
Adverse events
All adverse events including hyponatraemia (serum sodium level ≤ 130 mmol/L) (low sodium), hypokalaemia (≤ 3 mol/L) (low potassium), and development of persistent diarrhoea.
Search methods for identification of studies
We included all relevant trials regardless of language or publication status (published, unpublished, in press, and ongoing).
Electronic searches
We searched the following databases using the search terms and strategy described in Appendix 1: the Cochrane Infectious Diseases Group Specialized Register (up to 5 September 2016); the Cochrane Central Register of Controlled Trials (CENTRAL), published in the Cochrane Library (2016, Issue 9); MEDLINE (1966 to 5 September 2016); EMBASE (1974 to 5 September 2016); and LILACS (1982 to 5 September 2016). We also searched themetaRegister of Controlled Trials (mRCT) using 'diarrhoea' and 'oral rehydration solution' as search terms (2007 to 5 September 2016).
Searching other resources
Researchers, organizations, and pharmaceutical companies
To help identify unpublished and ongoing trials, we conducted a communications or website search (1 May 2006 to 5 September 2016) with individual researchers working in the field of general paediatrics and gastroenterology, and the following organizations who may be funding a similar study: the World Health Organization (WHO) through Dr. Shin Young Soo, Regional D, Waterborne and Parasitic Diseases, WHO Regional Office for the Western Pacific, Manila, Philippines; INCLEN (www.inclen.org); USAID (www.usaid.gov); the Asian Development Bank (www.adb.org); and the World Bank (www.worldbank.org). We also searched United Laboratories Philippines (www.unilab.com.ph) and Abbott International (www.abbott.com.ph) (pharmaceutical companies who manufacture ORS) for any unpublished or ongoing trials.
Reference lists
We checked the reference lists of all studies identified by the above methods.
Data collection and analysis
Selection of studies
Two review authors (GVG and LFD) independently screened the literature search results by title or abstract. We retrieved the full‐text reports of studies that either one or both review authors considered potentially relevant and trials with unclear treatment allocation. We independently assessed the inclusion criteria of these trials using a standard eligibility form. We resolved any disagreements through discussion, or if necessary, we consulted a third review author (MLM Gonzales). We scrutinized trial reports to ensure we detected that the result has not been previously published. We listed the excluded studies and the reasons for exclusion in the 'Characteristics of excluded studies' section. We constructed a PRISMA diagram to illustrate the study selection process (Figure 1).
1.
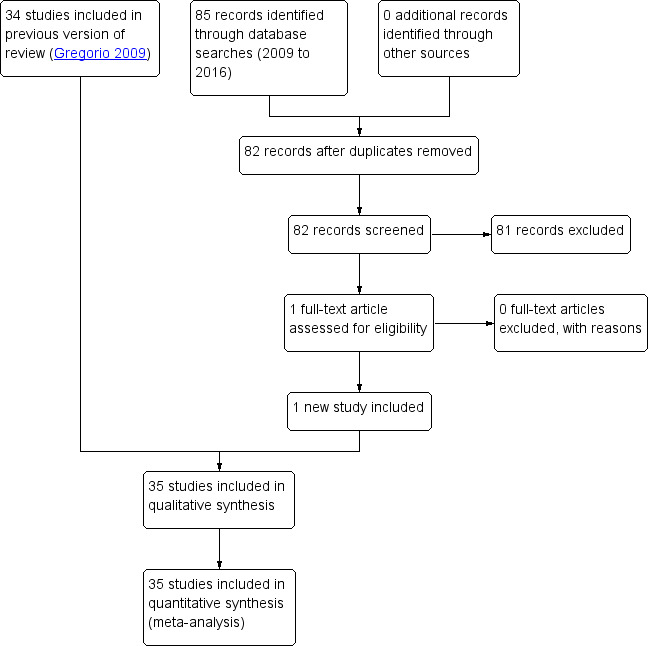
Study flow diagram.
Data extraction and management
Two review authors (GV Gregorio and EG Martinez or MLM Gonzales) independently extracted data from the included trials using pretested data extraction forms. We extracted the number of participants who were randomized and the number of participants analysed for all outcomes for each treatment arm in each trial to determine loss to follow‐up, whether loss was comparable across treatments, and to determine the type of analysis used. Since the primary outcome measures were continuous, we extracted arithmetic means and standard deviations (SDs) for each treatment group and noted the number of participants in each group. In trials with multiple interventions (two or more different polymer‐based ORS that were used as treatment groups), we pooled the means and SDs of the different polymer‐based ORS across the treatment arms.
For dichotomous outcome measures, we recorded the number(s) of participants that experienced the event and the number of participants analysed in each treatment group. In the meta‐analysis, for multiple treatment arms, we combined the number of participants that experienced the outcome in two or more experimental interventions as appropriate and compared collectively with the control group.
We resolved any disagreements about data extracted by referring to the trial report and through discussion, or, if necessary, we consulted a third review author. Where data were insufficient or missing, we attempted to contact the trial authors for clarification. GV Gregorio entered the data into Review Manager 5 (RevMan 5) (RevMan 2014).
Assessment of risk of bias in included studies
Two review authors (GV Gregorio and LF Dans or MLM Gonzales) independently assessed the risk of bias (methodological quality) of each trial using a prepared 'Risk of bias' assessment form. We assessed the generation of allocation sequence and allocation concealment as either 'high', 'low', or 'unclear'. We also noted who was blinded, such as the trial participants, care providers, or outcome assessors, and classified the inclusion of randomized participants in the analysis as either adequate if greater than 90% or inadequate if 90% or less. We used the results of the assessment to perform a sensitivity analysis. In the case of unclear or missing information, we attempted to contact the trial authors. We resolved disagreements by discussion between the review authors (Figure 2).
2.
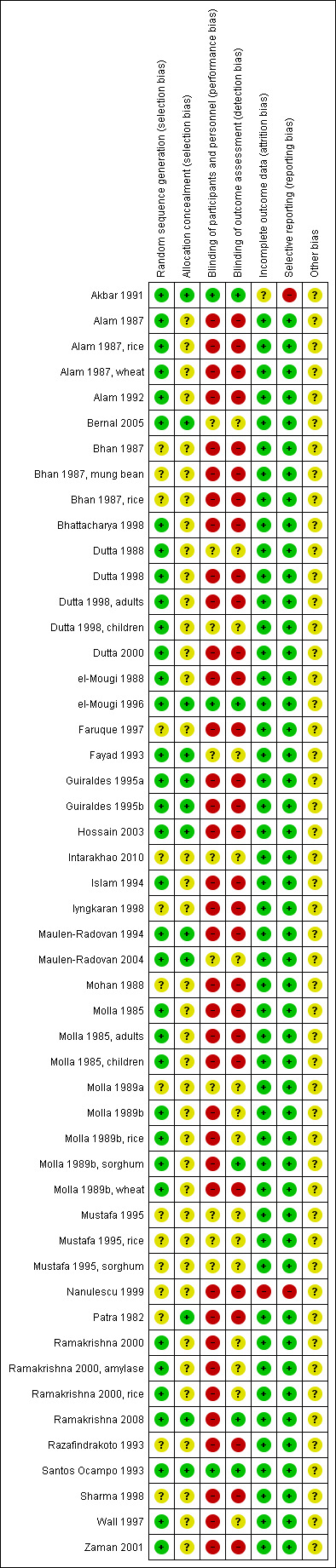
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Measures of treatment effect
The primary outcome measures included: (1) total stool output in the first 24 hours from randomization (g/kg), (2) total stool output from randomization to cessation of diarrhoea (g/kg); and (3) duration of diarrhoea during the study period (hours). We extracted the arithmetic mean and standard deviation (or medians and ranges) values and the number of participants analysed in each treatment group.
The dichotomous outcomes included: (1) unscheduled use of intravenous fluid; (2) vomiting; (3) hyponatraemia; (4) hypokalaemia (low potassium levels); and (5) development of persistent diarrhoea (diarrhoea of more than 10 days' duration from onset). We recorded the number of participants who experienced the episode and the total number of participants in each group.
Unit of analysis issues
We used the weighted mean difference to combine continuous data that were summarized by arithmetic means and standard deviations data. If the included trials reported data using geometric means, this may have indicated that the data was skewed. Thus, we extracted the standard deviation on the log scale using the generic inverse variance method and reported it on the natural scale. We reported the medians and ranges in a table.
Dealing with missing data
We attempted to contact the trial authors for any insufficient or missing data. If there was discrepancy in the number of participants randomized and the number of participants analysed in each treatment group, we reported the percentage loss to follow‐up in each group. We performed an intention‐to‐treat analysis.
Assessment of heterogeneity
We evaluated the presence of statistical heterogeneity among the interventions by inspecting the forest plot and by performing a Chi² test for heterogeneity using a P value of 0.10 to determine statistical significance. Also, we used an I² statistic value of 50% as an indication of moderate heterogeneity. If there was statistically significant heterogeneity, we used the random‐effects or DerSimonian and Laird method to combine data (DerSimonian 1986); otherwise we applied a fixed‐effect model.
Assessment of reporting biases
We assessed the presence of publication bias by looking for asymmetry in the funnel plots. We also assessed asymmetry of the funnel plots using the StatsDirect computer programme (StatsDirect 2008), and considered a P value of less than 0.05 on Egger's bias test as significant.
Data synthesis
GV Gregorio analysed the data using RevMan (RevMan 2014), and presented the results with 95% confidence intervals (CI). We determined and reported the percentage of participants lost to follow‐up for all trials based on the number randomized and the number analysed in each treatment group. We based analyses on a complete‐case approach. For the participants who did not adhere to the study protocol, we based their outcome on what the trial author(s) reported (if they performed an intention‐to‐treat (ITT) analysis) or on data we sought from the trial authors (if there was no ITT analysis).
We presented risk ratios (RR) for dichotomous outcomes. We determined continuous outcomes summarized as arithmetic means and SDs data using the mean difference (MD).
We checked the normality of the data by calculating the ratio of the mean over the SD. If the ratio (mean/SD) was less than two, then it was likely that the data were skewed and therefore we did not combine the data in the meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We investigated heterogeneity using subgroup analyses. We subgrouped trials according to the osmolarity of glucose ORS (ORS ≥ 310 or ORS ≤ 270) and type of polymer (rice, wheat, maltodextrins, and sorghum). We also evaluated the effect of the participant age (< 19 years (paediatric) and ≥ 19 years (adult) and of cholera as a pathogen. When there was substantial statistical heterogeneity (that is, I² statistic = 100%), we did not combine the trials in the meta‐analysis.
Sensitivity analysis
We performed sensitivity analyses to assess the robustness of the meta‐analysis by excluding trials of a low methodological quality, that is, those that used an inadequate method of randomization, unconcealed treatment allocation, and inadequate inclusion of randomized participants in the analysis.
Quality of the evidence
We assessed the quality of the evidence using the GRADE approach. We used the GRADEpro Guideline Development Tool (GDT) to prepare the 'Summary of findings' tables (GRADEpro GDT 2014). We considered generation of allocation sequence adequate if the study authors stated that they used a method with unpredictable sequence such as random number table or computer generated random numbers; unclear if trial authors stated that the trial was randomized but gave no further information; or inadequate when allocation was predictable and therefore introduced selection bias.
Allocation concealment was adequate if the investigator or the participant could not predict assignment to the group, such as by using central randomization, identical drug containers, or sealed opaque envelopes; unclear if the trial authors did not describe the method of concealment; or inadequate if the allocation of participant could be predicted.
We considered blinding adequate when the investigator or participant (double blind) did not know whether recruitment was to the intervention or control arms; unclear if the trial authors did not describe the method of blinding; and inadequate if the trial did not use blinding.
We considered follow‐up to be adequate when study authors presented study end points for 90% or more of the participants enrolled at the beginning; inadequate when follow‐up was less than 90%; and unclear when either the number of participants recruited at the beginning of the study or the number of participants who completed the study were unclear.
Results
Description of studies
Results of the search
In the first version of this review, Gregorio 2009, 34 trials met the inclusion criteria. For this review update, we identified 82 original records after we searched the literature up to 5 September 2016. We did not identify any further information regarding unpublished or ongoing clinical trials on polymer‐based oral rehydration solution (ORS) following communication with researchers, an organization, and pharmaceutical companies. After screening the literature search results by title and abstract, we excluded 81 records and assessed one full‐text article for eligibility. Only one new trial met the inclusion criteria of this review, Intarakhao 2010, and thus we included 35 trials in total in this review update. We have presented a PRISMA study flow diagram in Figure 1.
Included studies
Setting
Most trials were conducted in India (10 trials) and Bangladesh (nine trials). Other study centres were in Egypt (three trials) (el‐Mougi 1988; Fayad 1993; el‐Mougi 1996); Chile (two trials) (Guiraldes 1995a; Guiraldes 1995b); Mexico (two trials) (Maulen‐Radovan 1994; Maulen‐Radovan 2004); and one trial each was done in Australia (Wall 1997), Colombia (Bernal 2005), Madagascar (Razafindrakoto 1993), Malaysia (Iyngkaran 1998), Pakistan (Islam 1994), the Philippines (Santos Ocampo 1993), Romania (Nanulescu 1999), Sudan (Mustafa 1995), and Thailand (Intarakhao 2010). All but two trials were conducted in hospital settings. One trial was conducted in a paediatric clinic (Nanulescu 1999), and one in a rural treatment centre (Zaman 2007).
Participants
The 35 eligible trials included 4284 participants: 2304 used polymer‐based ORS and 1980 used glucose‐based ORS. In the individual trials, there was no statistically significant difference in the baseline characteristics between the two groups. Eight trials were on polymer‐based ORS versus ORS ≤ 270 while 27 trials used ORS ≥ 310.
Age
Twenty‐eight trials included children only: 25 trials in children less than five years old; one in children aged one to eight years old (Alam 1987); one in children aged two to ten years old (Dutta 2000); and one trial in children aged five to 15 years old (Zaman 2007). Five trials included adults only (Alam 1992; Bhattacharya 1998; Ramakrishna 2000; Hossain 2003; Ramakrishna 2008), and two trials included both adults and children (Molla 1985; Dutta 1998). The two trials that included both adults and children randomized and reported the outcomes separately for each group (Dutta 1998; Molla 1985).
Pathogen
In terms of the aetiology of diarrhoea, only eight trials randomized exclusively Vibrio cholerae‐positive participants (Molla 1989a; Alam 1992; Bhattacharya 1998; Dutta 1998; Dutta 2000; Ramakrishna 2000; Zaman 2001; Hossain 2003), while 22 trials included participants with mixed pathogens (both cholera and non‐cholera), and five trials did not report the pathogen (el‐Mougi 1988; Molla 1989b; Fayad 1993; Mustafa 1995; Sharma 1998).
Interventions
There were eight trials that compared polymer‐based ORS with ORS ≤ 270. Seven used rice as polymer source (Wall 1997; Bhattacharya 1998; Iyngkaran 1998; Nanulescu 1999; Dutta 2000; Maulen‐Radovan 2004; Intarakhao 2010), and one trial used amylase‐resistant starch (Ramakrishna 2008).
Twenty‐seven trials compared polymer‐based ORS with glucose‐based ORS ≥ 310 mOsm/L. Eighteen trials used varieties of rice (precooked, uncooked and pop rice), three trials evaluated maltodextrins (Akbar 1991; Santos Ocampo 1993; el‐Mougi 1996), one trial used amylase‐resistant starch (Ramakrishna 2000) and another used plantain flour (Bernal 2005). One trial each had rice‐based ORS in one trial arm and at least another polymer group: wheat (Alam 1987; Alam 1987, wheat); mung beans (Bhan 1987; Bhan 1987, mung bean); sorghum (Mustafa 1995, sorghum) ;and wheat, millet, maize, sorghum, and potatoes (Molla 1989b). In trials with more than one polymer group, they were reported separately. Overall, 22 trials used rice as a polymer source.
Feeding was started immediately after hydration in 26 trials, while in seven trials the onset of refeeding was unclear (Patra 1982; Molla 1985; Bhattacharya 1998; Dutta 1998; Iyngkaran 1998; Dutta 2000; Ramakrishna 2000). Only one trial withheld feeding in the first 24 hours (Molla 1989b). In another trial, Alam 1992, the participants were randomized into the rice‐ and glucose‐based ORS and further stratified as with and without food intake. In Alam 1992, we only used the data on participants with food intake in this review.
Outcomes reported
Most of the 35 trials reported the total stool output in the first 24 hours (25 trials), total stool output from randomization to discharge (18 trials), duration of diarrhoea (27 trials), and unscheduled use of intravenous fluid (19 trials). However, some of these outcomes were measured and reported in different units by the different studies and therefore we could not use all the data in the meta‐analyses (Table 3; Table 4). Furthermore, we did not include the data in the meta‐analyses if they were skewed: data for total stool output in 24 hours (Molla 1989a; Santos Ocampo 1993; Maulen‐Radovan 2004; Bernal 2005); on duration of diarrhoea (Santos Ocampo 1993; Mustafa 1995; Wall 1997); and total stool output from randomization to discharge (Santos Ocampo 1993).
1. Total stool output during the first 24 hours reported in different units.
| Trial | Unit of reporting total stool output during the first 24 hours |
| ORS ≤ 270 | |
| Bhattacharya 1998 | Mean (SD) L |
| Ramakrishna 2008 | Median (range) |
| Dutta 2000 | Mean (SD) L |
| Maulen‐Radovan 2004 | Geometric mean (95% CI) but during maintenance phase |
| ORS ≥ 310 | |
| Akbar 1991 | Median (range) |
| el‐Mougi 1996 | Geometric mean (95% CI) |
| Fayad 1993 | Geometric mean (95% CI) but during maintenance phase |
| Hossain 2003 | Median (range) |
| Ramakrishna 2000 | Mean (SD) but reported only in g |
| Sharma 1998 | Mean (SD) in g |
Abbreviations: SD: standard deviation; CI: confidence interval; ORS: oral rehydration solution.
2. Duration of diarrhoea reported in different units.
| Trial | Unit of reporting duration of diarrhoea |
| ORS ≤270 | |
| Iyngkaran 1998 | Reported only as shorter for rice ORS |
| Ramakrishna 2008 | Median (range) |
| ORS ≥310 | |
| Akbar 1991 | Median (hours) |
| el‐Mougi 1996 | Geometric mean (95% CI) |
| Fayad 1993 | Mean (SD) but during maintenance phase |
| Hossain 2003 | Median (range) |
| Molla 1989b | Not reported as patients were observed only for 24 hours |
Abbreviations: CI: confidence interval; SD: standard deviation; ORS: oral rehydration solution.
A few trials reported the number of participants with vomiting (11 trials) (Patra 1982; Bhan 1987; el‐Mougi 1988; Mohan 1988; Alam 1992; Islam 1994; Mustafa 1995, rice; Mustafa 1995, sorghum; Dutta 1998, adults; Dutta 1998, children; Iyngkaran 1998); hyponatraemia (six trials) (Dutta 1988; Guiraldes 1995a; Bhattacharya 1998; Dutta 2000; Zaman 2001; Ramakrishna 2008); hypokalaemia (two trials) (Bhan 1987; Zaman 2007); and development of persistent diarrhoea (two trials) (Fayad 1993; Faruque 1997).
Excluded studies
We excluded 35 trials from the previous version of this review, Gregorio 2009, for the following reasons (see the 'Characteristics of excluded studies' section): the electrolyte composition of the intervention and the control group were not identical or unknown (11 studies); the composition of the treatment group was either unknown or not a polymer (eight studies); the study was not a clinical trial on ORS but on the use of drugs in acute diarrhoea (four trials); the control group used an oral saline solution (one study) or an ORS that did not contain either 90 or 60 to 75 mmol/L sodium (three studies); not a randomized controlled trial (RCT) (one study); no control group (one study); not an efficacy but an effectiveness study (two studies); participants with persistent and not acute diarrhoea (two studies); and two clinical trials did not report the primary or secondary outcome of interest of this review. For this review update we only assessed one full‐text article for eligibility, which met the inclusion criteria of this review (Intarakhao 2010). We did not exclude any other full‐text articles.
Risk of bias in included studies
See Appendix 2 and Figure 2 for a summary of the 'Risk of bias' assessments and the 'Characteristics of included studies' for details of each trial's methods.
Allocation
Of the 35 trials, 24 trials used adequate methods to generate the allocation sequence (computer‐generated or random‐numbers table) and 11 trials used methods that were unclear (Patra 1982; Bhan 1987; Mohan 1988; Molla 1989a; Mustafa 1995; Razafindrakoto 1993; Faruque 1997; Iyngkaran 1998; Sharma 1998; Nanulescu 1999; Intarakhao 2010).
Only 12 trials used an adequate method to conceal allocation (Patra 1982; Bhan 1987; Fayad 1993; Santos Ocampo 1993; Maulen‐Radovan 1994; Guiraldes 1995a; Guiraldes 1995b; el‐Mougi 1996; Hossain 2003; Maulen‐Radovan 2004; Bernal 2005; Zaman 2007). The method was unclear in the other 23 included trials.
Blinding
Three trials performed blinding of the participants, providers, and assessors (Akbar 1991; Santos Ocampo 1993; el‐Mougi 1996). Blinding was difficult or impossible in most trials because of the difference in the appearance of the ORS formulation after reconstitution.
Incomplete outcome data
All but two trials included an adequate (over 90%) number of randomized participants in the analysis. We assessed the number of participants as inadequate in two trials (Akbar 1991; Nanulescu 1999).
Selective reporting
Two trials selectively reported data (Akbar 1991; Nanulescu 1999).
Other potential sources of bias
It was unclear if there were any other potential sources of bias in the included trials.
Effects of interventions
Comparison 1: Polymer‐based ORS versus glucose‐based ORS (≤ 270 mOsm/L)
Eight trials (752 participants) compared polymer‐based ORS with glucose‐based ORS with osmolarity ≤ 270 mOsm/L (see Table 5). Seven trials used rice as a source of polymer. Two trials were conducted in adults (Bhattacharya 1998; Ramakrishna 2008), and the remaining trials were conducted in children (Wall 1997; Iyngkaran 1998; Nanulescu 1999; Dutta 2000; Maulen‐Radovan 2004; Intarakhao 2010). Two studies only included participants with V. cholerae (Bhattacharya 1998; Dutta 2000), while the other six studies included participants with mixed infections.
3. Polymer ORS ≤ 270 mOsm/L summary of trial characteristics.
| Trial | Type of polymer ORS | Age of participants | Cause of diarrhoea | Level of dehydration | Malnutrition | Country | Year of study |
| Wall 1997 | Rice ORS | 1 month to 5 years | Rotavirus | Mild and moderate | Not stated | Australia | Not stated |
| Bhattacharya 1998 | Rice ORS | Adult males | Vibrio cholerae | Severe | Not stated | India | 1993 to 1996 |
| Iyngkaran 1998 | Rice ORS | < 6 months | Mixed pathogen | Mild and moderate | Not stated | Malaysia | Not stated |
| Nanulescu 1999 | Rice ORS | 1 to 12 months | Mixed pathogens | Mild and moderate | Included those with weight for age > 80% of 50th percentile | Northern Romania | 1995 to 1996 |
| Dutta 2000 | Cooked rice | 2 to 10 years | V. cholerae | Severe | Not stated | India | 1995 to 1998 |
| Maulen‐Radovan 2004 | Premixed rice | 3 to 24 months | Rotavirus (43%) | Mild, moderate, and severe | Excluded those with severe malnutrition | Mexico | 1994 to 1995 |
| Ramakrishna 2008 | Amylase‐resistant starch | 12 to 65 years | Mixed pathogens | Moderate and severe | Not stated | India | 2003 to 2005 |
| Intarakhao 2010 | Rice ORS | 9 months to 5 years old | Rotavirus (60%) | Mild and Moderate | Not stated | Thailand | 2007 to 2008 |
Abbreviation: ORS: oral rehydration solution.
Stool output
Mean stool volume in the first 24 hours was lower with polymer‐based ORS in the only study (Nanulescu 1999) that assessed this (MD −24.60 mL/kg, 95% CI −40.69 to −8.51; 1 trial, 99 participants, Analysis 1.1).
1.1. Analysis.
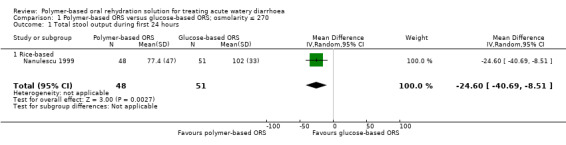
Comparison 1 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≤ 270, Outcome 1 Total stool output during first 24 hours.
Duration of diarrhoea
On average across five trials, the mean duration of diarrhoea was around eight hours shorter with polymer‐based ORS (MD −8.24 hours, 95% CI −13.17 to −3.30; 5 trials, 364 participants, Analysis 1.2). There was substantial statistical heterogeneity between trials in the size of the effect which ranged from three hours shorter to 13 hours shorter (Chi² test P < 0.00001, I² statistic = 86%).
1.2. Analysis.
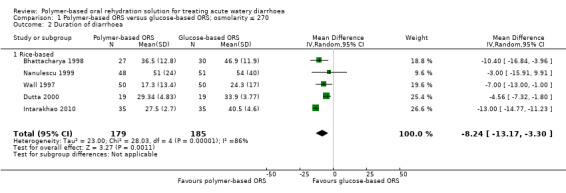
Comparison 1 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≤ 270, Outcome 2 Duration of diarrhoea.
Unscheduled use of intravenous fluid
The number of participants that needed intravenous rehydration was lower with polymer‐based ORS but the 95% CI includes the possibility of both important effects and no effect (RR 0.62, 95% CI 0.36 to 1.08; I² statistic = 30%; 3 trials, 326 participants, Analysis 1.3).
1.3. Analysis.
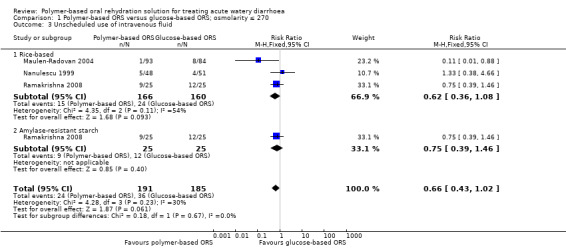
Comparison 1 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≤ 270, Outcome 3 Unscheduled use of intravenous fluid.
Adverse events
One small trial reported the number of participants with vomiting in each group (Iyngkaran 1998), but was too small to detect or exclude important differences (RR 0.56, 95% CI 0.24 to 1.34; 1 trial, 63 participants, Analysis 1.4). Three trials reported on the incidence of hyponatraemia (Bhattacharya 1998; Dutta 2000; Ramakrishna 2008), and again they were too small to reliably prove or exclude important differences (RR 0.88, 95% CI 0.43 to 1.82; 3 trials, 145 participants, Analysis 1.5). No trials reported hypokalaemia or the development of persistent diarrhoea.
1.4. Analysis.
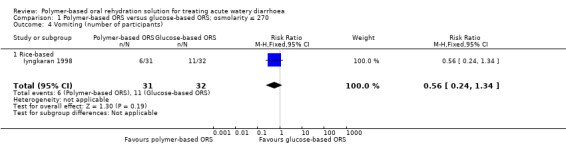
Comparison 1 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≤ 270, Outcome 4 Vomiting (number of participants).
1.5. Analysis.
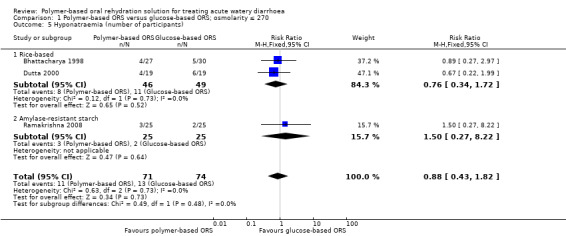
Comparison 1 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≤ 270, Outcome 5 Hyponatraemia (number of participants).
Comparison 2: Polymer‐based ORS versus glucose‐based ORS (≥ 310 mOsm/L)
Twenty‐seven trials (3532 participants) compared polymer‐based ORS with glucose‐based ORS ≥ 310 mOsm/L (see Table 6). Eighteen trials evaluated varieties of rice (precooked, uncooked, and pop rice), three evaluated maltodextrins (Akbar 1991; Santos Ocampo 1993; el‐Mougi 1996), one used amylase‐resistant starch (Ramakrishna 2000), and one trial each had a rice based in one arm and at least another polymer group: wheat (Alam 1987); mung beans (Bhan 1987); sorghum (Mustafa 1995); plantain flour (Bernal 2005); and wheat, millet, maize, sorghum, and potatoes (Molla 1989b). Overall, 23 trials used rice as a polymer source.
4. Polymer ORS ≥ 310 mOsm/L summary of trial characteristics.
| Trial | Type of polymer ORS | Age of participants | Cause of diarrhoea | Level of dehydration | Malnutrition | Country | Year of study |
| Akbar 1991 | Maltodextrin | 4 to 36 months | Rotavirus and ETEC | Mild and moderate | Excluded severe | Bangladesh | 1987 to 1988 |
| Alam 1987 | Wheat and rice | 1 to 8 years | Not stated | Moderate and severe | Excluded severe malnutrition (< 60% weight for age of 50th centile National Center for Health Statistics (NCHS) | Bangladesh | 1984 |
| Alam 1992 | Rice | 15 to 60 years | Cholera (positive for Vibrio cholerae) | Not stated | Not stated | Bangladesh | 1988 |
| Bernal 2005 | Plantain flour | 1 to 48 months | Mixed pathogens | "Presence", but without shock | Not stated | Colombia | Not stated |
| Bhan 1987 | Pop Rice and mung bean | 3 months to 5 years | Mixed pathogens | "Presence", level not stated | Included those with weight for height (wt/ht) > 70% of 50th centile of reference standard | India | Not stated |
| Dutta 1988 | Rice and pop rice | 4 months to 4 years | Not stated | Severe | Not stated | India | Not stated |
| Dutta 1998 | Rice | 3 to 12 years; 18 to 55 years |
Cholera (positive for V. cholerae) | Severe | Not stated | India | 1995 to 1996 |
| el‐Mougi 1988 | Rice | 4 months to 4 years | Not stated | Moderate and severe | Not stated. Excluded marasmic‐kwashiorkor | Egypt | Not stated |
| el‐Mougi 1996 | Maltodextrin | 3 to 24 months | Not stated | Moderate | Not stated. Excluded severe malnutrition | Egypt | Not stated |
| Faruque 1997 | Rice | 3 to 35 months | Mixed pathogens | Mild and Moderate | Excluded severe malnutrition | Bangladesh | 1990 to 1991 |
| Fayad 1993 | Rice | 3 to 18 months | Not stated | "Presence", level not stated | Excluded severe malnutrition | Egypt | 1990 to 1992 |
| Guiraldes 1995a | Rice | 3 to 18 months | Mixed pathogens | Moderate | Excluded moderate to severe malnutrition | Chile | Not stated |
| Guiraldes 1995b | Rice | 3 to 24 months | Mixed pathogens | Moderate | Excluded moderate to severe malnutrition | Chile | Not stated |
| Hossain 2003 | Rice | 18 to 60 years | V. cholerae | Severe | Not stated | Bangladesh | 1995 |
| Islam 1994 | Rice | < 6 months | Not stated | Mild and moderate | Included those with wt/age > 75% of 50th centile | Pakistan | 1990 |
| Maulen‐Radovan 1994 | Precooked rice | 1 to 6 months | Mixed pathogens | Mild and moderate | Excluded severe malnutrition | Mexico | Not stated |
| Mohan 1988 | Rice | 3 to 36 months | Not stated | "Presence", level not stated | Not stated | India | Not stated |
| Molla 1985, adults | Rice | "adults" | Not stated | Moderate and severe | Not stated | Bangladesh | 1983 |
| Molla 1985, children | Rice | < 10 years | Not stated | Moderate and severe | Not stated | Bangladesh | 1983 |
| Molla 1989a | Rice | < 5 years | V. cholerae | Moderate and severe | Not stated | Bangladesh | Not stated |
| Molla 1989b | Rice, maize, sorghum, millet, wheat, potatoes | 1 to 5 years | Not stated | Moderate and severe | Not stated | Bangladesh | Not stated |
| Mustafa 1995 | Rice, sorghum | 6 to 40 months | Not stated | Moderate and severe | Included normal and underweight children | Sudan | 1990 |
| Patra 1982 | Rice | 3 months to 5 years | Not stated | Moderate and severe | Not stated | India | Not stated |
| Ramakrishna 2000 | Rice flour, amylase resistant starch | 14 to 58 years | V. cholerae | Not stated | Not stated | India | 1994 to 1996 |
| Razafindrakoto 1993 | Rice | 6 to 36 months | Not stated | Mild and moderate | Excluded severe malnutrition, < 70% of reference standard | Madagascar | 1990 |
| Santos Ocampo 1993 | Maltodextrin | 3 to 36 months | Mixed pathogens | Mild and moderate | Excluded severe malnutrition | Philippines | Not stated |
| Sharma 1998 | Rice | 7 to 36 months | Non‐cholerae | Some (mild and moderate) | Included children > 80% as per Indian Academy of Pediatrics (IAP) classification | India | Not stated |
| Zaman 2001 | Rice | 5 to 15 years | Not stated | Moderate to severe | Not stated. Exclusion criteria: malnutrition < 65% weight for age | Bangladesh | 1997 |
Abbreviations: ORS: oral rehydration solution.NCHS: National Center for Health Statistics; IAP: Indian Academy of Pediatrics; wt/ht: weight for height.
Stool output
On average, the stool volume during the first 24 hours was around 65 mL/kg lower in the polymer‐based ORS group (MD −65.47, 95% CI −83.92 to −47.03; 16 trials, 1483 participants, Analysis 2.1). There was substantial statistical heterogeneity between trials (Chi² test P < 0.00001, I² statistic = 100%), which was not well explained by subgroup analyses based on age (Analysis 2.2), or pathogen (Analysis 2.3). The heterogeneity is mainly in the size of the effect which ranged from 181 mL/kg lower to 27 mL/kg higher.
2.1. Analysis.
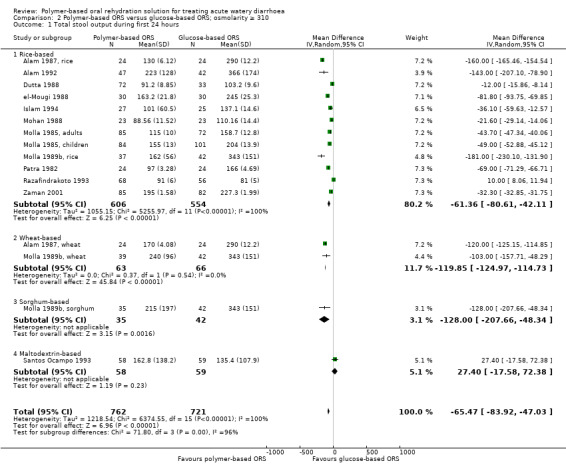
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 1 Total stool output during first 24 hours.
2.2. Analysis.
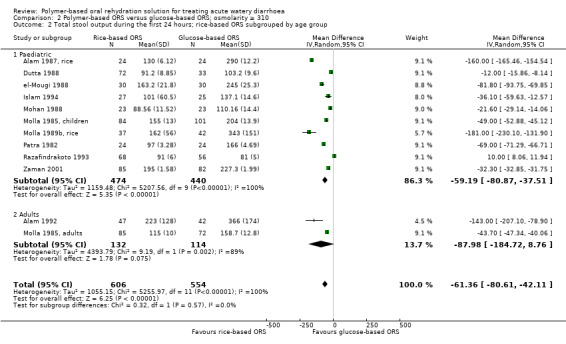
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 2 Total stool output during the first 24 hours; rice‐based ORS subgrouped by age group.
2.3. Analysis.
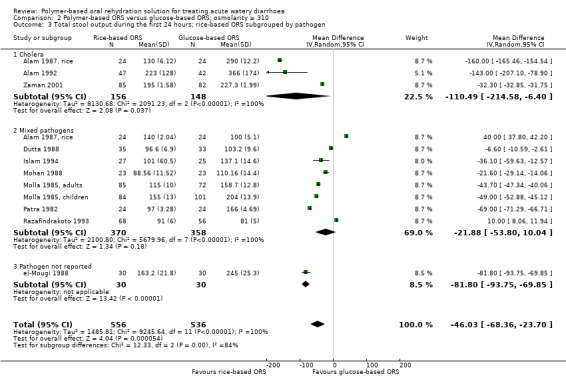
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 3 Total stool output during the first 24 hours; rice‐based ORS subgrouped by pathogen.
Duration of diarrhoea
On average, the duration of diarrhoea was around eight hours shorter in the polymer‐based ORS group compared to glucose‐based ORS (MD −8.47 hrs, 95% CI −12.86 to −4.08; 16 trials, 1187 participants, Analysis 2.4; Chi² test P < 0.00001, I² statistic = 100%). Substantial statistical heterogeneity between trials was not explained by subgroup analyses based on age (Analysis 2.5), and type of pathogen (Analysis 2.6). The heterogeneity is mainly in the size of the effect which ranged from 0.5 hours shorter to 27 hours shorter.
2.4. Analysis.
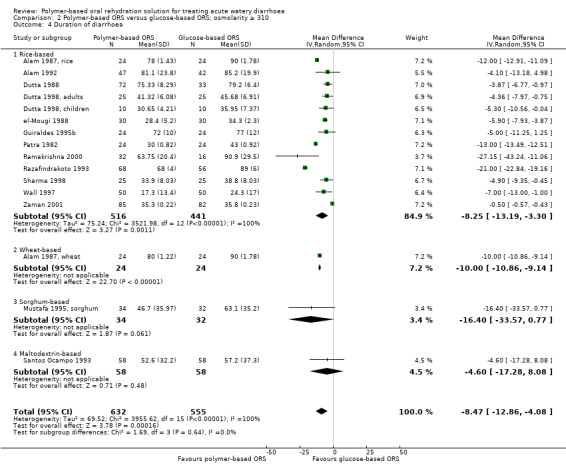
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 4 Duration of diarrhoea.
2.5. Analysis.
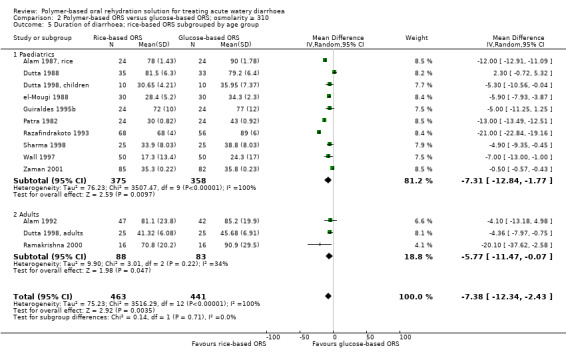
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 5 Duration of diarrhoea; rice‐based ORS subgrouped by age group.
2.6. Analysis.
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 6 Duration of diarrhoea; rice‐based ORS subgrouped by type of pathogen.
Unscheduled use of intravenous fluid
The proportion of participants that required intravenous hydration was low in most trials and without statistically significant differences between groups (RR 0.75, 95% CI 0.57 to 0.98; I² statistic = 0%; 19 trials, 1877 participants, Analysis 2.7). A subgroup analysis by type of pathogen found a statistically significant decrease on unscheduled intravenous fluid those infected with mixed pathogens (RR 0.63, 95% CI 0.41 to 0.96; I² statistic = 0%; 11 trials, 928 participants, Analysis 2.8), but not in participants positive for V. cholerae (RR 0.94, 95% CI 0.66 to 1.34; I² statistic = 0%; 7 trials, 535 participants, Analysis 2.8).
2.7. Analysis.
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 7 Unscheduled use of intravenous fluid.
2.8. Analysis.
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 8 Unscheduled use of intravenous fluid, subgrouped by type of pathogen.
Adverse effects
There was no statistically significant difference between the polymer‐based and glucose‐based ORS groups in the number of participants who developed vomiting (10 trials, 584 participants, Analysis 2.9), hyponatraemia (4 trials, 385 participants, Analysis 2.10), hypokalaemia (2 trials, 260 participants, Analysis 2.11), or persistent diarrhoea (2 trials, 885 participants, Analysis 2.12).
2.9. Analysis.
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 9 Vomiting (number of participants).
2.10. Analysis.
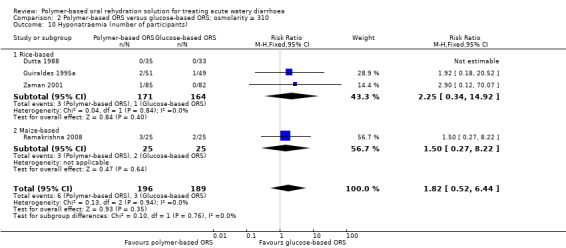
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 10 Hyponatraemia (number of participants).
2.11. Analysis.
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 11 Hypokalaemia (number of participants).
2.12. Analysis.
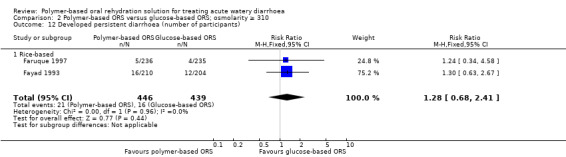
Comparison 2 Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310, Outcome 12 Developed persistent diarrhoea (number of participants).
Publication bias
We observed substantial, significant heterogeneity in the primary outcomes and therefore we decided to use a funnel plot for the secondary outcome, where the data were homogenous. We constructed a funnel plot of 19 trials that compared polymer‐based and ORS ≥ 310 and measured the outcome of unscheduled use of intravenous fluid (Figure 3). The funnel plot is asymmetric due to the absence of smaller trials at the base and to the right of the pooled estimate. Asymmetry in the funnel plot could result from possible selection bias where smaller studies reporting greater treatment benefit for the experimental group were published (publication bias). The gap in the bottom corner of the graph suggests that smaller studies without statistically significant effects remain unpublished. Differences in inclusion criteria (for example, cholera positive versus mixed pathogens) and method of assessment of unscheduled use of intravenous fluid may also account for the asymmetry.
3.
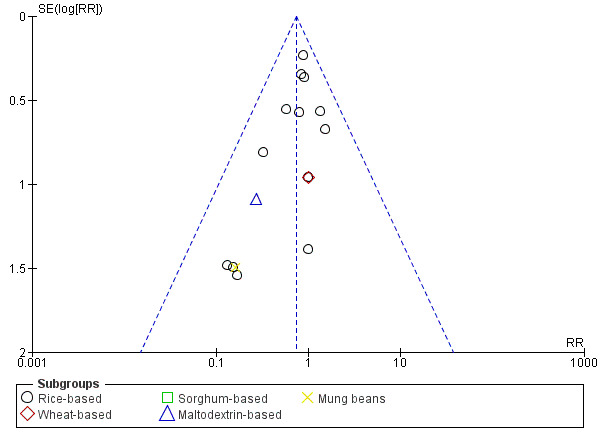
Funnel plot of comparison: 2 Polymer‐based ORS versus glucose‐based ORS, osmolarity ≥ 310, outcome: 2.7 Unscheduled use of intravenous fluid.
Discussion
Summary of main results
Polymer‐based ORS versus glucose‐based ORS (osmolarity ≤ 270)
Eight trials (752 participants) evaluated this comparison, and seven trials used rice as a polymer source. Polymer‐based oral rehydration solution (ORS) reduces mean stool output in the first 24 hours by 24 mLl/kg (mean difference (low quality evidence). The average duration of diarrhoea may be reduced by eight hours (low quality evidence) with polymer ORS but results are heterogeneous. Limited trials showed no observed difference in the risk of unscheduled use of intravenous fluid (very low quality evidence), vomiting (very low quality evidence), and hyponatraemia (very low quality evidence).
Polymer‐based ORS versus glucose‐based ORS (osmolarity ≥ 310)
Twenty‐seven trials (3532 participants) evaluated this comparison using a variety of polymers. On average, polymer ORS may reduce the total stool output in the first 24 hours by around 65 mLl/kg (low quality evidence) and may reduce the duration of diarrhoea by around eight hours (low quality evidence) with substantial heterogeneity. The proportion of participants that required intravenous hydration was low (low quality evidence) and without statistically significant difference between groups. Subgroup analysis by type of pathogen found a statistically significant decrease on unscheduled intravenous fluid in those infected with mixed pathogens (low quality evidence) but not in participants positive for Vibrio cholerae (low quality evidence). No difference was observed in the proportion of patients who developed vomiting (very low quality evidence), hyponatraemia (very low quality evidence), hypokalaemia (low quality evidence), or persistent diarrhoea (very low quality evidence).
Overall completeness and applicability of evidence
We retrieved all relevant trials regardless of language or publication status (published, unpublished, in press, and ongoing) and we included those that met the inclusion criteria. Most clinical trials included infants and children with acute diarrhoea and were conducted in developing countries, which are the age group and the setting with a high incidence of diarrhoea. However, most of the clinical trials (77%) used ORS ≥ 310. Since 2004, the World Health Organization (WHO) has recommended the use of reduced osmolarity ORS ≤ 270. There were only eight clinical trials that used ORS ≤ 270, thus, data from this review could not adequately compare the two formulations.
Quality of the evidence
Polymer‐based versus ORS ≤ 270
We assessed the quality of the evidence as low to very low. There was serious risk of bias. Of the eight trials, only five had adequate allocation sequence and only one had adequate allocation concealment (Maulen‐Radovan 2004). No study was blinded and there was one with inadequate follow‐up (Nanulescu 1999). There is serious risk of indirectness as most (88%) trials were conducted in a hospital setting. There is also risk of imprecision due to the limited sample size and wide confidence interval (CI) of the results.
Polymer‐based versus ORS ≥ 310
The quality of the evidence was from low to very low. Of the 27 trials, most trials (18 trials, 67%) had adequate allocation sequence but only 11 trials (41%) had adequate allocation concealment; the rest were unclear. Only three trials had complete blinding, the rest had partial, unclear, or no blinding. There is risk of indirectness as all but one trial was conducted in a hospital setting. There was no serious imprecision as the sample size was sufficient to detect any difference in the outcomes.
Overall, there is substantial heterogeneity in the clinical trials, despite statistically significant results in the primary outcomes. Different authors assessed the outcomes differently and this may explain the heterogeneity in the treatment effect (methodological diversity). Ideally, measurement of stool output should be made by taking the difference in the weight of the diaper before and after use. In some studies that included both males and females (especially in the paediatric group), the urine output may have been inadvertently mixed with the stool, giving an erroneously higher stool output. In adults, three trials used a cholera cot to measure stool output (Bhattacharya 1998; Dutta 2000; Ramakrishna 2000), while one trial did not state the measurement method used (Alam 1992). The cholera cot has a bucket underneath to measure the stool output more accurately. It was also unclear in most trials whether the duration of diarrhoea was measured from the initial onset of the disease, before admission to the study, or only from admission up to the time of discharge. Different trials may also have used different criteria to define patients who warrant an unscheduled use of intravenous fluid.
Polymer‐based ORS may have several advantages that are independent of glucose. The protein and amino acid component found in certain polymer‐based ORS, such as in rice‐based ORS, may stimulate sodium absorption and the slow breakdown of starch into glucose molecules may promote reabsorption of intestinal secretions and reduce the volume and duration of diarrhoea. The new reduced osmolarity ORS formulation (ORS ≤ 270) with reduced osmotic load is the currently recommended ORS (WHO 2004). This Cochrane Review failed to show with certainty that polymer‐based ORS is as effective as, or is more effective than, the reduced osmolarity ORS.
Potential biases in the review process
We searched different databases for clinical trials on ORS and acute diarrhoea. Also we checked the web sites of organizations and pharmaceutical companies who may be funding a similar study for unpublished or ongoing clinical trials. However, we still observed publication bias as evidenced by an asymmetric funnel plot due to the absence of smaller trials at the base and to the right of the pooled estimate. This suggests that clinical trials with small numbers of participants or with negative results remain unpublished. Most trials were done in the hospital setting under ideal conditions with highly selected participants that had evidence of moderate to severe dehydration. This limits the review's ability to be generalized as most acute diarrhoea cases start at home and the severity of dehydration may be minimized by immediately initiating ORS.
Agreements and disagreements with other studies or reviews
The efficacy of rice‐based ORS has previously been reported to decrease the stool output in the first 24 hours among V. cholerae‐positive patients, in both adults and children (Fontaine 1998). We observed that polymer‐based ORS as compared with glucose ORS ≥ 310 decreased the total stool output and duration of diarrhoea, regardless of whether the diarrhoea was secondary to V. cholerae infection or due to either bacterial or viral cause (mixed pathogens). This review considered all clinical trials that used rice and non‐rice sources of polymers, such as wheat, maize, or sorghum, that are used as staple foods in other parts of the world.
On the other hand, polymer‐based ORS ≥ 310 decreased the need for intravenous fluid only among those infected with mixed pathogens but not in V. cholerae‐positive patients. The difference in effect may be attributed to the difference in the diarrhoeal mechanism between these pathogens. Cholera is an enterotoxin‐mediated diarrhoea and intestinal secretory processes are activated by the bacteria, which leads to massive fluid and electrolyte losses, without any macro‐ or micro‐damage to the intestinal mucosa. Thus, there is a need for rapid fluid replacement which may not be possible with oral rehydration alone. On the other hand, commonly‐encountered enteric pathogens in childhood diarrhoea, such as rotavirus, Salmonella spp, and Shigella spp, cause injury to the intestinal mucosae which leads to a decrease in intestinal absorption of fluid, electrolytes, and nutrients.
In a large multicentre trial, the use of a reduced osmolarity ORS (ORS ≤ 270) compared to a glucose‐based ORS (ORS ≥ 310) decreased the need for unscheduled use of intravenous fluid by 33% (CHOICE 2001). In this review, most of the included clinical trials used ORS ≥ 310 and only a few trials used the newer ORS ≤ 270, which has a lower osmolarity. We were unable to make any definite conclusion on the efficacy of polymer‐based ORS compared with ORS ≤ 270.
Authors' conclusions
Implications for practice.
Polymer‐based ORS shows advantages compared to glucose‐based ORS (at ≥ 310 mOsm/L). Comparisons favoured polymer‐based ORS over ORS ≤ 270 but the analysis was underpowered.
Implications for research.
The rationale for the use of polymer‐based ORS is the slow release of glucose from starch, which provides the carrier molecules for sodium without the osmotic penalty that results if the quantity of glucose is increased by the use of ORS ≥ 310. Since the ORS presently recommended already has a reduced osmolarity (ORS ≤ 270), more clinical trials are needed to compare the polymer‐based ORS with ORS ≤ 270.
Feedback
Polymer‐based ORS versus low osmolarity glucose ORS
Summary
The authors have rightly mentioned that since 2004, the WHO has recommended that low osmolarity (< 270 mOsm/L) oral rehydrating solution be used as the treatment for dehydration. This being the case, the rationale for undertaking a systematic review to compare standard osmolarity oral rehydration solutions (glucose‐ or polymer‐based) is not clear. It would have been more appropriate to conduct the review on currently recommended oral rehydration solutions (low osmolarity). In continuation to the above, it is therefore inappropriate to pool together (in meta‐analysis) trials with low osmolarity ORS as well as trials with standard osmolarity ORS. Incidentally, polymer‐based ORS has been shown to be superior only when these trials (apples and oranges) were pooled together. Similarly, it is inappropriate to pool data from adults and children together, because they behave differently in response to diarrhoea and consequent dehydration. Therefore, a re‐analysis of data on low osmolarity ORS in children (the critical age group which is the focus of the WHO and Millennium Development Goals) reveals that there are only four trials that can be pooled together (these are present in the subgroup analysis). I have undertaken a fresh search on 25th April and have not come across any trials beyond the search date mentioned in the review; hence these four trials can be taken as the current evidence. There is significant heterogeneity among the four trials with respect to age of participants, type of diarrhoea, severity of dehydration, and outcomes chosen. However, the salient findings are as follows.
Polymer based ORS is comparable to glucose‐based ORS in terms of treatment failure (requirement of intravenous fluid).
Polymer‐based ORS is comparable to glucose‐based ORS for two adverse events viz vomiting and hyponatraemia. Hyponatremia was surprisingly frequent in the single trial reporting it (Dutta 2000); this trial was conducted in children with cholera diarrhoea having severe dehydration. This could be a matter of concern for using low osmolarity ORS (either type) if substantiated by other reports.
The duration and amount of diarrhoea were significantly reduced with non‐glucose ORS. However, these statistically significant differences may not have as much clinical significance considering that the duration was shortened by only about 4.5 hours and the amount by less than 25 g/kg, that is, 2.5% body weight, although the latter represents approximately 25% decrease compared to glucose ORS. It may be recalled that 5% loss results in mild dehydration in infants and young children (3% in older).
Therefore, at best polymer‐based ORS can be regarded as comparable to glucose‐based ORS, but not superior. Of course, considering the limited data, further research may yield a more definitive answer.
Reply
We have singled out the results of the low osmolarity glucose solutions (ORS < 270) and have re‐analysed the data considering separately the glucose ORS low and high osmolarity solutions. Based on a re‐analysis, there were six trials that used ORS < 270 (low) and 29 trials with ORS > 300 (high). Using the stratification of ORS < 270 and ORS > 300 in all analyses, we made the following conclusions.
No statistically significant difference between the polymer‐based and glucose‐based ORS groups in the number of participants with vomiting, hyponatraemia, hypokalaemia, and development of persistent diarrhoea.
Total stool output in the first 24 hours is shorter in those who were given rice‐based ORS as compared to those who were given glucose‐based ORS < 270 (based on one trial).
Unscheduled use of Intravenous fluid was fewer in those given rice‐based ORS as compared to those given ORS > 300 (13 trials). There was only one trial on ORS < 270 that reported unscheduled use of Intravenous fluids.
Significantly shorter duration of diarrhoea in adults in those given rice‐based ORS as compared with ORS > 310 (two trials) or ORS < 270 (two trials).
With stratification of the data on whether they were given ORS < 270 or ORS > 300, no definite conclusions could be made as significant data (bullet points 2 and 4 above) is based only on two trials with the use of ORS < 270. The authors believe that we should wait for further trials on ORS < 270 before doing a reanalysis of the review.
Contributors
Germana V. Gregorio
Nanulescu trial
Summary
The number of participants in the Nanulescu 1999 trial have been shown as rice‐based ORS (N = 48) and glucose‐based ORS (N = 51) in the analysis but the other way round in the 'Characteristics of included studies' table. Perhaps this is a typographical error; if not it has some serious implications.
Reply
There was a typographical error in the Nanulescu 1999 trial in the 'Characteristics of included studies' table and this has been corrected.
Contributors
Germana V. Gregorio
What's new
| Date | Event | Description |
|---|---|---|
| 6 December 2016 | New search has been performed | The review authors assessed the results of the literature search and included one new trial (Intarakhao 2010). They used the GRADE approach to assess the quality of the evidence and constructed 'Summary of findings' tables. |
| 6 December 2016 | New citation required but conclusions have not changed | The updated review includes 35 trials. The review authors subgrouped trials according to the osmolarity of glucose ORS (ORS ≥ 310 or ORS ≤ 270) and type of polymer (rice, wheat, maltodextrins, and sorghum). |
Acknowledgements
The editorial base of the Cochrane Infectious Diseases Group is funded by UK aid from the UK Government for the benefit of developing countries (Grant: 5242). The views expressed in this review do not necessarily reflect UK government policy.
Appendices
Appendix 1. Search methods: detailed search strategies
| Search set | MEDLINE1,2 | EMBASE1,2 | Other1,2 |
| 1 | REHYDRATION SOLUTIONS | FLUID THERAPY | oral rehydration |
| 2 | FLUID THERAPY | ORAL REHYDRATION THERAPY | fluid therapy |
| 3 | oral rehydration solution | oral rehydration solution | ORS |
| 4 | ORS | ORS | 1 or 2 or 3 |
| 5 | 1 or 2 or 3 or 4 | 1 or 2 or 3 or 4 | glucose |
| 6 | STARCH | GLUCOSE‐POLYMER | rice |
| 7 | glucose | STARCH | amylase |
| 8 | rice | glucose | amylopectin |
| 9 | amylase | rice | corn |
| 10 | amylopectins | amylase | sorghum |
| 11 | corn | amylopectins | maize |
| 12 | sorghum | corn | 6‐11/or |
| 13 | maize | sorghum | 4 and 12 |
| 14 | 6‐13/or | maize | — |
| 15 | 5 and 14 | 6‐14 | — |
| 16 | Limit 15 to human | 5 and 15 | — |
| 17 | — | Limit 16 to human | — |
1Search terms used in combination with the search strategy for retrieving trials developed by Cochrane (Lefebvre 2011); upper case: MeSH or EMTREE heading; lower case: free text term. 2Search terms used for the Cochrane Infectious Diseases Group Specialized Register, CENTRAL, and LILACS.
Appendix 2. 'Risk of bias' assessment
| Trial | Allocation sequence | Allocation concealment | Blinding | Inclusion of randomized participants in analysis |
| Akbar 1991 | Adequate | Adequate | Participants, providers, outcome assessors | Inadequate |
| Alam 1987 | Adequate | Unclear | None | Adequate |
| Alam 1992 | Adequate | Unclear | None | Adequate |
| Bernal 2005 | Adequate | Adequate | Unclear | Adequate |
| Bhan 1987 | Unclear | Unclear | None | Adequate |
| Bhattacharya 1998 | Adequate | Unclear | None | Adequate |
| Dutta 1988 | Adequate | Unclear | Unclear | Adequate |
| Dutta 1998 | Adequate | Unclear | None | Adequate |
| Dutta 2000 | Adequate | Unclear | None | Adequate |
| el‐Mougi 1988 | Adequate | Unclear | None | Adequate |
| el‐Mougi 1996 | Adequate | Adequate | Participants, providers, outcome assessors | Adequate |
| Faruque 1997 | Unclear | Unclear | None | Adequate |
| Fayad 1993 | Adequate | Adequate | Unclear | Adequate |
| Guiraldes 1995a | Adequate | Adequate | None | Adequate |
| Guiraldes 1995b | Adequate | Adequate | None | Adequate |
| Hossain 2003 | Adequate | Adequate | None | Adequate |
| Intarakhao 2010 | Unclear | Unclear | Unclear | Adequate |
| Islam 1994 | Adequate | Unclear | None | Adequate |
| Iyngkaran 1998 | Unclear | Unclear | None | Adequate |
| Maulen‐Radovan 1994 | Adequate | Adequate | None | Adequate |
| Maulen‐Radovan 2004 | Adequate | Adequate | None | Adequate |
| Mohan 1988 | Unclear | Unclear | None | Adequate |
| Molla 1985 | Adequate | Unclear | None | Adequate |
| Molla 1989a | Unclear | Unclear | Unclear | Adequate |
| Molla 1989b | Adequate | Unclear | Participants and providers not blinded; outcome assessors unclear | Adequate |
| Mustafa 1995 | Unclear | Unclear | Unclear | Adequate |
| Nanulescu 1999 | Unclear | Unclear | None | Inadequate |
| Patra 1982 | Unclear | Adequate | None | Adequate |
| Ramakrishna 2000 | Adequate | Unclear | Participants and providers partially blinded; outcome assessors unclear | Adequate |
| Ramakrishna 2008 | Adequate | Adequate | Assessors but not the participants or providers were blinded because of the nature of the study | Adequate |
| Razafindrakoto 1993 | Unclear | Unclear | None | Adequate |
| Santos Ocampo 1993 | Adequate | Adequate | Participants, providers, outcome assessors | Adequate |
| Sharma 1998 | Unclear | Unclear | None | Adequate |
| Wall 1997 | Adequate | Unclear | Participants and providers not blinded; outcome assessors unclear | Adequate |
| Zaman 2001 | Adequate | Unclear | None | Adequate |
Data and analyses
Comparison 1. Polymer‐based ORS versus glucose‐based ORS; osmolarity ≤ 270.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total stool output during first 24 hours | 1 | 99 | Mean Difference (IV, Random, 95% CI) | ‐24.60 [‐40.69, ‐8.51] |
| 1.1 Rice‐based | 1 | 99 | Mean Difference (IV, Random, 95% CI) | ‐24.60 [‐40.69, ‐8.51] |
| 2 Duration of diarrhoea | 5 | 364 | Mean Difference (IV, Random, 95% CI) | ‐8.24 [‐13.17, ‐3.30] |
| 2.1 Rice‐based | 5 | 364 | Mean Difference (IV, Random, 95% CI) | ‐8.24 [‐13.17, ‐3.30] |
| 3 Unscheduled use of intravenous fluid | 3 | 376 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.43, 1.02] |
| 3.1 Rice‐based | 3 | 326 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.36, 1.08] |
| 3.2 Amylase‐resistant starch | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.39, 1.46] |
| 4 Vomiting (number of participants) | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.24, 1.34] |
| 4.1 Rice‐based | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.24, 1.34] |
| 5 Hyponatraemia (number of participants) | 3 | 145 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.43, 1.82] |
| 5.1 Rice‐based | 2 | 95 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.34, 1.72] |
| 5.2 Amylase‐resistant starch | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.27, 8.22] |
Comparison 2. Polymer‐based ORS versus glucose‐based ORS; osmolarity ≥ 310.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total stool output during first 24 hours | 16 | 1483 | Mean Difference (IV, Random, 95% CI) | ‐65.47 [‐83.92, ‐47.03] |
| 1.1 Rice‐based | 12 | 1160 | Mean Difference (IV, Random, 95% CI) | ‐61.36 [‐80.61, ‐42.11] |
| 1.2 Wheat‐based | 2 | 129 | Mean Difference (IV, Random, 95% CI) | ‐119.85 [‐124.97, ‐114.73] |
| 1.3 Sorghum‐based | 1 | 77 | Mean Difference (IV, Random, 95% CI) | ‐128.0 [‐207.66, ‐48.34] |
| 1.4 Maltodextrin‐based | 1 | 117 | Mean Difference (IV, Random, 95% CI) | 27.40 [‐17.58, 72.38] |
| 2 Total stool output during the first 24 hours; rice‐based ORS subgrouped by age group | 12 | 1160 | Mean Difference (IV, Random, 95% CI) | ‐61.36 [‐80.61, ‐42.11] |
| 2.1 Paediatric | 10 | 914 | Mean Difference (IV, Random, 95% CI) | ‐59.19 [‐80.87, ‐37.51] |
| 2.2 Adults | 2 | 246 | Mean Difference (IV, Random, 95% CI) | ‐87.98 [‐184.72, 8.76] |
| 3 Total stool output during the first 24 hours; rice‐based ORS subgrouped by pathogen | 11 | 1092 | Mean Difference (IV, Random, 95% CI) | ‐46.03 [‐68.36, ‐23.70] |
| 3.1 Cholera | 3 | 304 | Mean Difference (IV, Random, 95% CI) | ‐110.49 [‐214.58, ‐6.40] |
| 3.2 Mixed pathogens | 8 | 728 | Mean Difference (IV, Random, 95% CI) | ‐21.88 [‐53.80, 10.04] |
| 3.3 Pathogen not reported | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐81.80 [‐93.75, ‐69.85] |
| 4 Duration of diarrhoea | 16 | 1187 | Mean Difference (IV, Random, 95% CI) | ‐8.47 [‐12.86, ‐4.08] |
| 4.1 Rice‐based | 13 | 957 | Mean Difference (IV, Random, 95% CI) | ‐8.25 [‐13.19, ‐3.30] |
| 4.2 Wheat‐based | 1 | 48 | Mean Difference (IV, Random, 95% CI) | ‐10.0 [‐10.86, ‐9.14] |
| 4.3 Sorghum‐based | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐16.4 [‐33.57, 0.77] |
| 4.4 Maltodextrin‐based | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐4.60 [‐17.28, 8.08] |
| 5 Duration of diarrhoea; rice‐based ORS subgrouped by age group | 13 | 904 | Mean Difference (IV, Random, 95% CI) | ‐7.38 [‐12.34, ‐2.43] |
| 5.1 Paediatrics | 10 | 733 | Mean Difference (IV, Random, 95% CI) | ‐7.31 [‐12.84, ‐1.77] |
| 5.2 Adults | 3 | 171 | Mean Difference (IV, Random, 95% CI) | ‐5.77 [‐11.47, ‐0.07] |
| 6 Duration of diarrhoea; rice‐based ORS subgrouped by type of pathogen | 13 | 888 | Mean Difference (IV, Random, 95% CI) | ‐7.31 [‐12.47, ‐2.15] |
| 6.1 Cholera | 7 | 453 | Mean Difference (IV, Random, 95% CI) | ‐4.79 [‐7.99, ‐1.59] |
| 6.2 Mixed pathogens | 6 | 435 | Mean Difference (IV, Random, 95% CI) | ‐8.88 [‐14.97, ‐2.78] |
| 7 Unscheduled use of intravenous fluid | 19 | 1877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.57, 0.98] |
| 7.1 Rice‐based | 16 | 1698 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.60, 1.03] |
| 7.2 Wheat‐based | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.53] |
| 7.3 Sorghum‐based | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.4 Maltodextrin‐based | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.03, 2.32] |
| 7.5 Mung beans | 1 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 3.01] |
| 8 Unscheduled use of intravenous fluid, subgrouped by type of pathogen | 19 | 1877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.57, 0.98] |
| 8.1 Cholera | 7 | 535 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.66, 1.34] |
| 8.2 Mixed pathogens | 11 | 928 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.41, 0.96] |
| 8.3 Pathogen not reported | 1 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.07, 1.59] |
| 9 Vomiting (number of participants) | 10 | 584 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.72, 1.14] |
| 9.1 Rice‐based | 9 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.68, 1.12] |
| 9.2 Sorghum‐based | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.59, 2.22] |
| 10 Hyponatraemia (number of participants) | 4 | 385 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [0.52, 6.44] |
| 10.1 Rice‐based | 3 | 335 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.25 [0.34, 14.92] |
| 10.2 Maize‐based | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.27, 8.22] |
| 11 Hypokalaemia (number of participants) | 2 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.74, 2.25] |
| 11.1 Rice‐based | 2 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.74, 2.25] |
| 12 Developed persistent diarrhoea (number of participants) | 2 | 885 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.68, 2.41] |
| 12.1 Rice‐based | 2 | 885 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.68, 2.41] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Akbar 1991.
| Methods | Randomized controlled trial (RCT) Generation of allocation sequence: block randomization Allocation concealment: code broken at the end of the study Blinding: participants, providers, outcome assessors Inclusion of participants in analysis: 81% (maltodextrin group 33/43, 77%; glucose group 36/43, 84%) Duration: 20 months, from January 1987 to August 1988 |
|
| Participants | Number of participants: 86 enrolled Inclusion criteria: male; 4 to 36 months; diarrhoea < 3 days; mild to moderate dehydration Exclusion criteria: bloody diarrhoea; antibiotic treatment in the last 3 days; severe malnutrition; presence of systemic illness |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization |
| Allocation concealment (selection bias) | Low risk | Code broken at the end of the study |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, providers, and outcome assessors were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, providers, and outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Inadequate inclusion of randomized participants in analysis |
| Selective reporting (reporting bias) | High risk | 81% (maltodextrin group 33/43, 77%; glucose group 36/43, 84%) |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Alam 1987.
| Methods | RCT Generation of allocation sequence: permuted block design Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 13 months, from April 1983 to April 1984 |
|
| Participants | Number of participants: 72 enrolled Inclusion criteria: age 1 to 8 years; watery diarrhoea < 3 days; presence of moderate to severe dehydration Exclusion criteria: antibiotic treatment before admission; severe malnutrition; presence of systemic illness |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | Participants given rice ORS were less dehydrated compared to those given glucose ORS, but the difference was not statistically significant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | This was not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Alam 1987, rice.
| Methods | Rice arm of Alam 1987 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Alam 1987, wheat.
| Methods | Wheat arm of Alam 1987 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Alam 1992.
| Methods | RCT Generation of allocation sequence: random numbers Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 30 months, from July 1986 to December 1988 |
|
| Participants | Number of participants: 182 enrolled Inclusion criteria: age 15 to 60 years; acute watery diarrhoea; presence of dehydration; positive for Vibrio cholerae Exclusion criteria: history of antidiarrhoeal or antimicrobial intake before admission |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | Analysed separately with or without food intake | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT by random number |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial included over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Bernal 2005.
| Methods | RCT Generation of allocation sequence: permuted blocks of variable length Allocation concealment: sealed, opaque envelopes Blinding: unclear Inclusion of participants in analysis: > 90% Duration: 17 months, from March 2001 to July 2002 |
|
| Participants | Number of participants: 101 enrolled Inclusion criteria: age 1 to 48 months; acute watery diarrhoea < 7 days; presence of dehydration but without hypovolaemic shock Exclusion criteria: malnourished, kwashiorkor type; presence of paralytic ileus |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Medellin, Colombia |
|
| Notes | Data on total stool output in first 24 hours are skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted blocks of variable length |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Bhan 1987.
| Methods | RCT Generation of allocation sequence: randomly assigned using sealed envelopes Allocation concealment: sealed envelopes Blinding: none Inclusion of participants in analysis: > 90% Duration: not specified; only stated that trial was done for 10 consecutive months |
|
| Participants | Number of participants: 93 enrolled Inclusion criteria: males; age 3 months to 5 years; watery diarrhoea < 5 days; presence of dehydration; weight for height > 70% of 50th centile of reference standard Exclusion criteria: female; persistent vomiting; bloody diarrhoea; temperature > 39°C; other associated medical illness; intake of antibiotics during illness |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: New Delhi, India |
|
| Notes | Participants who were given glucose ORS were more malnourished as compared to the treatment groups, but the difference was not statistically significant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned using sealed envelopes |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Bhan 1987, mung bean.
| Methods | Mung bean ORS arm of Bhan 1987 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned using sealed envelopes |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Bhan 1987, rice.
| Methods | Pop rice ORS arm of Bhan 1987 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: the trial used sealed envelopes to randomly assign participants. |
| Allocation concealment (selection bias) | Unclear risk | The trial used sealed envelopes to randomly assign participants. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial authors included all randomized participants in the analysis. |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% participants in the final analysis. |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Bhattacharya 1998.
| Methods | RCT Generation of allocation sequence: permuted block of random numbers Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 32 months, from August 1993 to March 1996 |
|
| Participants | Number of participants: 123 enrolled Inclusion criteria: adult males; acute watery diarrhoea; presence of severe dehydration; no antibiotic or intravenous fluid intake; no systemic illness Exclusion criteria: presence of systemic illness; use of intravenous fluid before admission |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L and ≤ 270 mOsm/L | |
| Setting | Hospital‐based trial Location: Calcutta, India |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Dutta 1988.
| Methods | RCT Generation of allocation sequence: random‐numbers table Allocation concealment: not reported Blinding: unclear Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 105 enrolled Inclusion criteria: age 4 months to 4 years; males; acute watery diarrhoea; presence of severe dehydration Exclusion criteria: presence of systemic illness; antibiotic intake before admission |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Calcutta, India |
|
| Notes | Results of rice ORS and pop rice ORS were combined both for the continuous and dichotomous outcomes, and compared with glucose ORS. These were all reported as rice‐based ORS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: random‐numbers table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Dutta 1998.
| Methods | RCT Generation of allocation sequence: permuted block of random numbers Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 14 months, from May 1995 to June 1996 |
|
| Participants | Number of participants: 50 adults and 20 children enrolled Inclusion criteria: age 3 to 12 years for children, and 18 to 55 years for adults; acute watery diarrhoea; severe dehydration Exclusion criteria: presence of systemic illness; with intake of drug or intravenous fluid before admission |
|
| Interventions | Adults
Children
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Calcutta, India |
|
| Notes | Children and adults were randomized separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Dutta 1998, adults.
| Methods | Adult arm of Dutta 1998 | |
| Participants |
|
|
| Interventions | — | |
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Dutta 1998, children.
| Methods | Children arm of Dutta 1998 | |
| Participants |
|
|
| Interventions | — | |
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Dutta 2000.
| Methods | RCT Generation of allocation sequence: permuted blocks of random numbers Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 34 months, from August 1995 to May 1998 |
|
| Participants | Number of participants: 58 enrolled Inclusion criteria: age 2 to 10 years; acute watery diarrhoea; presence of severe dehydration; positive for V. cholerae Exclusion criteria: presence of systemic illness; with intake of drug or intravenous fluid before admission |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L and ≤ 270 mOsm/L | |
| Setting | Hospital‐based trial Location: Calcutta, India |
|
| Notes | Only the data on glucose ORS ≤ 270 were used as this is the one with same electrolyte composition as the rice ORS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted blocks of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
el‐Mougi 1988.
| Methods | RCT Generation of allocation sequence: random permuted blocks Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% of randomized participants included in the final analysis Duration: not stated |
|
| Participants | Number of participants: 60 enrolled Inclusion criteria: age 4 months to 4 years; males; acute watery diarrhoea; presence of moderate to severe dehydration; on milk formula intake Exclusion criteria: presence of bloody diarrhoea; severe dehydration; febrile (temperature > 38.5°C); marasmic‐kwashiorkor malnutrition |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Cairo, Egypt |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: random permuted blocks |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
el‐Mougi 1996.
| Methods | RCT Generation of allocation sequence: random blocks of fixed length Allocation concealment: serially numbered identical ORS packets Blinding: participants, providers, outcome assessors Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 89 enrolled Inclusion criteria: age 3 to 24 months; acute watery diarrhoea; presence of mild to moderate dehydration; non‐cholera diarrhoea Exclusion criteria: presence of bloody diarrhoea; severe malnutrition; with no or severe dehydration |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Cairo, Egypt |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: random blocks of fixed length |
| Allocation concealment (selection bias) | Low risk | Serially numbered identical ORS packets |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, providers, and outcome assessors were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, providers, and outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Faruque 1997.
| Methods | RCT Generation of allocation sequence: randomized Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 17 months, from August 1990 to December 1991 |
|
| Participants | Number of participants: 471 enrolled Inclusion criteria: age 3 to 35 months; acute watery diarrhoea; presence of mild and moderate dehydration Exclusion criteria: presence of severe dehydration; severe malnutrition; intercurrent illness or chronic disease |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization unclear |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Fayad 1993.
| Methods | RCT Generation of allocation sequence: random permuted blocks of variable length Allocation concealment: sealed, serially numbered envelopes Blinding: unclear Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 441 enrolled Inclusion criteria: age 3 to 18 months, acute watery diarrhoea < 7 days; presence of dehydration Exclusion criteria: bloody diarrhoea; severe malnutrition; presence of systemic illness; exclusively or mostly breastfed |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Cairo, Egypt |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: random permuted blocks of variable length |
| Allocation concealment (selection bias) | Low risk | Sealed, serially numbered envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Guiraldes 1995a.
| Methods | RCT Generation of allocation sequence: permuted block randomization Allocation concealment: code was kept Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 100 enrolled Inclusion criteria: age 3 to 18 months; acute watery diarrhoea; presence of moderate dehydration; non‐breastfed Exclusion criteria: presence of systemic illness; presence of moderate to severe malnutrition |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Santiago, Chile |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block randomization |
| Allocation concealment (selection bias) | Low risk | Code was kept |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Guiraldes 1995b.
| Methods | RCT Generation of allocation sequence: block randomization Allocation concealment: code was kept until end of trial Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 48 enrolled Inclusion criteria: age 3 to 24 months; acute watery diarrhoea; presence of moderate dehydration; non‐breastfed Exclusion criteria: presence of systemic illness; moderate to severe malnutrition |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Santiago, Chile |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block randomization |
| Allocation concealment (selection bias) | Low risk | Code was kept |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Hossain 2003.
| Methods | RCT Generation of allocation sequence: computer‐generated randomization Allocation concealment: sealed envelopes Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 113 enrolled Inclusion criteria: adult males 18 to 60 years old; acute watery diarrhoea; presence of severe dehydration; positive for V. cholerae Exclusion criteria: presence of concomitant illness; received antibiotic and ORS before admission |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | Data for primary outcomes reported as median (range) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: computer generated randomization |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Intarakhao 2010.
| Methods | RCT Generation of allocation sequence: unclear Allocation concealment: unclear Blinding: unclear Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 70 enrolled Inclusion criteria: 9 months to 5 years old; acute watery diarrhoea Exclusion criteria: presence of invasive diarrhoea (white blood cell count > 5 cell/high power field (hpf) or red blood cells > 5 cell/hpf from stool examination), profound shock, alteration of consciousness or convulsion, severe electrolyte imbalance, severe malnutrition or malabsorption syndrome, renal failure, severe systemic infection, rice allergy, acute abdominal conditions |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≤ 270 mOsm/L | |
| Setting | Hospital‐based trial Location: Patumthanee, Thailand |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT but generation of allocation sequence is unclear |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Islam 1994.
| Methods | RCT Generation of allocation sequence: permuted block randomization Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 14 months, from March 1989 to April 1990 |
|
| Participants | Number of participants: 52 enrolled Inclusion criteria: age < 6 months; acute watery diarrhoea; presence of mild to moderate dehydration; weight for height > 75% of 50th centile Exclusion criteria: presence of bloody diarrhoea; systemic illness; unable to take ORS; intake of antibiotic |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial (diarrhoea training unit) Location: Karachi, Pakistan |
|
| Notes | Participants who were given rice ORS were younger compared to those given glucose ORS, but the difference is not statistically significant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: Permuted block randomization |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Iyngkaran 1998.
| Methods | RCT Generation of allocation sequence: randomized Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 63 enrolled Inclusion criteria: age < 6 months; loose stools < 7 days' duration Exclusion criteria: presence of systemic illness; intake of antibiotic/anti‐diarrhoeal before admission; severe dehydration |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≤ 270 mOsm/L | |
| Setting | Hospital‐based trial Location: Kuala Lumpur, Malaysia |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Maulen‐Radovan 1994.
| Methods | RCT Generation of allocation sequence: randomly assigned permuted blocks Allocation concealment: serially numbered sealed envelopes Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 97 enrolled Inclusion criteria: age 1 to 6 months; acute watery diarrhoea < 5 days; presence of mild to moderate dehydration Exclusion criteria: presence of bloody diarrhoea; systemic illness; severe malnutrition; history of diarrhoea in the last 2 weeks |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial (emergency department) Location: Mexico City, Mexico |
|
| Notes | Results for primary outcome skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: randomly assigned permuted blocks |
| Allocation concealment (selection bias) | Low risk | Serially numbered sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Maulen‐Radovan 2004.
| Methods | RCT Generation of allocation sequence: block randomization Allocation concealment: serially numbered sealed envelopes Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 189 enrolled Inclusion criteria: age 3 to 24 months; males; acute watery diarrhoea; presence dehydration Exclusion criteria: presence of bloody diarrhoea; systemic illness; severe malnutrition |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≤ 270 mOsm/L | |
| Setting | Hospital‐based trial Location: Mexico City, Mexico |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: block randomization |
| Allocation concealment (selection bias) | Low risk | Serially numbered sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants, providers. and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants, providers. and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Mohan 1988.
| Methods | RCT Generation of allocation sequence: randomized Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 50 enrolled Inclusion criteria: age 3 to 36 months, acute watery diarrhoea, presence of dehydration Exclusion criteria: none reported |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: New Delhi, India |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomized |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers. and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers. and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1985.
| Methods | RCT Generation of allocation sequence: predetermined random numbers Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 4 months, from December 1982 to March 1983 |
|
| Participants | Number of participants: 342 enrolled Inclusion criteria: children aged < 10 years and adults; acute watery diarrhoea; presence of moderate and severe dehydration Exclusion criteria: presence of systemic illness; intake of antibiotics and ORS before admission |
|
| Interventions | Adults
Children
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | Separate analysis for children and adults | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: predetermined random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1985, adults.
| Methods | Adult trial arm of Molla 1985 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: predetermined random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1985, children.
| Methods | Children trial arm of Molla 1985 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: predetermined random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1989a.
| Methods | RCT Generation of allocation sequence: randomly assigned Allocation concealment: not reported Blinding: unclear Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 93 enrolled Inclusion criteria: children aged < 5 years; acute watery diarrhoea; presence of moderate and severe dehydration; positive for V. cholerae Exclusion criteria: breastfed; those with previous treatment |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | Data on total stool output in first 24 hours are skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants, providers, and outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants, providers, and outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1989b.
| Methods | RCT Generation of allocation sequence: permuted block design Allocation concealment: not reported Blinding: participants and providers not blinded; outcome assessors unclear Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 276 enrolled Inclusion criteria: age 1 to 5 years; acute watery diarrhoea < 48 hours; presence of moderate to severe dehydration; no complications Exclusion criteria: none reported |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Dhaka, Bangladesh |
|
| Notes | Study with 6 treatment groups versus 1 control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1989b, rice.
| Methods | Rice arm of Molla 1989b | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1989b, sorghum.
| Methods | Sorghum arm of Molla 1989b | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Molla 1989b, wheat.
| Methods | Wheat arm of Molla 1989b | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Mustafa 1995.
| Methods | RCT Generation of allocation sequence: randomly assigned Allocation concealment: not reported Blinding: unclear Inclusion of participants in analysis: > 90% Duration: 9 months, from April to December 1990 |
|
| Participants | Number of participants: 96 enrolled Inclusion criteria: males aged < 5 years; acute watery diarrhoea; presence of moderate and severe dehydration Exclusion criteria: presence of bloody diarrhoea; no systemic illness |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Khartoum, Sudan |
|
| Notes | Study with 3 treatment arms: 2 polymer‐based ORS versus 1 control group. Data on duration of diarrhoea are skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Mustafa 1995, rice.
| Methods | Rice arm of Mustafa 1995 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Mustafa 1995, sorghum.
| Methods | Sorghum arm of Mustafa 1995 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Nanulescu 1999.
| Methods | RCT Generation of allocation sequence: randomly assigned Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: 88% (rice group, 48/56, 86%; glucose group, 51/57, 89%) Duration: 12 months, from 1 May 1995 to 1 May 1996 |
|
| Participants | Number of participants: 113 enrolled Inclusion criteria: age 1 to 12 months; acute watery diarrhoea; presence of mild or moderate dehydration; weight for age > 80% of 50th centile Exclusion criteria: newborn; presence of bloody diarrhoea; systemic illness; intake of antibiotics; severe dehydration; moderate to severe malnutrition |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≤ 270 mOsm/L | |
| Setting | Paediatric clinic Location: Ciuj‐Napoca, Romania |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers. and outcome assessors not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers. and outcome assessors not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The trial included only 88% of the randomized participants in the analysis |
| Selective reporting (reporting bias) | High risk | The trial reported only 88% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Patra 1982.
| Methods | RCT Generation of allocation sequence: randomly assigned Allocation concealment: sealed envelopes Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 52 participants Inclusion criteria: age 3 months to 5 years; acute watery diarrhoea; presence of moderate to severe dehydration Exclusion criteria: none reported |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Calcutta, India |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | RCT: randomly assigned |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Ramakrishna 2000.
| Methods | RCT Generation of allocation sequence: block randomization Allocation concealment: not reported Blinding: participants and providers partially blinded; outcome assessors unclear Inclusion of participants in analysis: > 90% Duration: 27 months, from May 1994 to July 1996 |
|
| Participants | Number of participants: 48 enrolled Inclusion criteria: age 14 to 58 years old; acute watery diarrhoea < 72 hours; positive for V. cholerae Exclusion criteria: presence of systemic illness; intake of antibiotics |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Vellore, India |
|
| Notes | Study with 3 treatment arms: 2 polymer‐based ORS versus glucose ORS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: block randomization |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers partially blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Ramakrishna 2000, amylase.
| Methods | Amylase arm of Ramakrishna 2000 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: block randomization |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers partially blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Ramakrishna 2000, rice.
| Methods | Rice arm of Ramakrishna 2000 | |
| Participants | — | |
| Interventions |
|
|
| Outcomes | — | |
| Glucose‐based ORS osmolarity | — | |
| Setting | — | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: block randomization |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers partially blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Ramakrishna 2008.
| Methods | RCT Generation of allocation sequence: table of random numbers Allocation concealment: serially numbered ORS packages Blinding: assessors but not the participants or providers were blinded because of the nature of the study Inclusion of participants in analysis: 100% Duration: not stated |
|
| Participants | Number of participants: 50 enrolled Inclusion criteria: males; 18 to 65 years old; acute watery diarrhoea Exclusion criteria: presence of bloody diarrhoea; presence of systemic illness |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≤ 270 mOsm/L | |
| Setting | Hospital‐based trial Location: Vellore, India |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: Table of random numbers |
| Allocation concealment (selection bias) | Low risk | Serially numbered ORS packages |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers were not blinded because of the nature of the study |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Razafindrakoto 1993.
| Methods | RCT Generation of allocation sequence: randomized Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: 27 months, from January 1988 to March 1990 |
|
| Participants | Number of participants: 150 enrolled Inclusion criteria: age 6 to 36 months; males; acute watery diarrhoea; mild to moderate dehydration; severe malnutrition < 70% of reference standard Exclusion criteria: presence of bloody diarrhoea; presence of systemic illness; patients in shock |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Antanarivo, Madagascar |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, and outcome assessors not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, and outcome assessors not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Santos Ocampo 1993.
| Methods | RCT Generation of allocation sequence: table of random numbers Allocation concealment: code was kept until the end of trial Blinding: participants, providers, outcome assessors Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 120 enrolled Inclusion criteria: age 3 to 36 months; males; acute diarrhoea < 5 days; mild to moderate dehydration Exclusion criteria: presence of bloody diarrhoea; systemic illness; intake of antibiotics; severe dehydration; severe malnutrition; history of diarrhoea in the last 2 weeks |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsml/L | |
| Setting | Hospital‐based trial Location: Manila, Philippines |
|
| Notes | Results of total stool output in first 24 hours, total stool output from randomization to discharge, and duration of diarrhoea are skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: table of random numbers |
| Allocation concealment (selection bias) | Low risk | Code was kept until the end of trial |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, providers, outcome assessors were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, providers, outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Sharma 1998.
| Methods | RCT Generation of allocation sequence: randomized Allocation concealment: not reported Blinding: none Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 100 enrolled Inclusion criteria: age 7 to 36 months; acute diarrhoea; some dehydration; non‐cholerae; weight > 80% of reference standard Exclusion criteria: presence of bloody diarrhoea; presence of systemic illness; severe dehydration; malnutrition; abdominal distension |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Rohtak, India |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Wall 1997.
| Methods | RCT Generation of allocation sequence: table of random numbers Allocation concealment: not reported Blinding: participants and providers not blinded; outcome assessors unclear Inclusion of participants in analysis: > 90% Duration: not stated |
|
| Participants | Number of participants: 100 enrolled Inclusion criteria: age 4 weeks to 5 years old; acute diarrhoea; mild to moderate dehydration Exclusion criteria: presence of systemic illness; intake of antibiotics/antidiarrhoeals; severe dehydration; previous surgery |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Hospital‐based trial Location: Brisbane, Australia |
|
| Notes | Data on duration of diarrhoea are skewed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Zaman 2001.
| Methods | RCT Generation of allocation sequence: table of random numbers Allocation concealment: not specified whether envelope is opaque and sealed Blinding: none Inclusion of participants in analysis: > 90% of randomized participants included in the final analysis Duration: September 1996 to May 1997 |
|
| Participants | Number of participants: 167 enrolled Inclusion criteria: age 5 to 15 years; acute diarrhoea; moderate to severe dehydration; purging rate > 2 mL/kg/hour Exclusion criteria: presence of bloody diarrhoea; systemic illness; intake of antibiotics; malnutrition < 65% weight for age |
|
| Interventions |
|
|
| Outcomes |
|
|
| Glucose‐based ORS osmolarity | ≥ 310 mOsm/L | |
| Setting | Rural treatment centre Location: Matlab, Bangladesh |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | RCT: table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not specified whether envelope is opaque and sealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants, providers, outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants, providers, outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial included all randomized participants in the analysis |
| Selective reporting (reporting bias) | Low risk | The trial reported over 90% of the included participants in the final analysis |
| Other bias | Unclear risk | We did not detect any other sources of bias |
Abbreviations: RCT: randomized controlled trial; ORS: oral rehydration solution; hpf: high power field.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agustina 2007 | This was not a clinical trial on oral rehydration solution (ORS). |
| Alam 2008 | Guar gum, a soluble fibre and not a polymer, was added to the ORS. |
| Alam 2009 | The ORS contained other electrolytes such as zinc, copper, and magnesium, which are not present in the World Health Organization (WHO)‐recommended ORS. |
| Ansaldi 1990 | Different electrolyte composition of the 2 groups. |
| Barclay 1995 | Different electrolyte composition of the 2 groups. |
| Barragan‐Guzmán 1998 | The trial gave the control group oral saline solution, not ORS. |
| Bhandari 2008 | This was not a clinical trial on ORS. |
| Cohen 1995 | Different electrolyte composition of the 2 groups. |
| Gutiérrez 2007 | L‐glutamine, an amino acid and not a polymer, was added in the ORS. |
| Hoekstra 2004 | Investigated the use of non‐digestible carbohydrates, which are not polymers. |
| Jirapinyo 1996 | Different electrolyte composition of the 2 groups. |
| Kassaye 1994 | The composition of the home‐made ORS is not known. |
| Kenya 1989 | The 2 groups had different sources of bicarbonate: polymer‐based ORS used sodium bicarbonate and glucose ORS, trisodium citrate dihydrate. |
| Lebenthal 1995 | Polymer‐based ORS has an additional amino acid. |
| Molina 1995 | Glucose‐based ORS contained 50 mmol/L sodium. The inclusion criteria of this review specified 90 or 60 to 75 mmol/L of sodium. |
| Molla 1982 | This study used a sucrose and not a glucose‐based ORS as a control group. |
| Molla 2000 | This was not an efficacy study. The study compared the biochemical analysis of home‐made rice ORS versus glucose‐based ORS. |
| Mota‐Hernández 1991 | Different electrolyte composition of the 2 groups. |
| Murphy 1996 | Unknown electrolyte composition of the wheat‐based ORS. |
| Patra 1984 | Treatment group used an amino acid‐based ORS, not a polymer‐based ORS. |
| Pelleboer 1990 | This was not a RCT, as the study performed alternate allocation of participants in the 2 interventions. |
| Pizarro 1991 | Different electrolyte composition of the 2 groups. |
| Prasad 1993 | The primary outcome of interest relevant to the study was not evaluated. |
| Rabbani 2005 | The study had no control group that used glucose‐based ORS. The control group contained L‐histidine, an amino acid. |
| Raghupathy 2006 | Polymer was not used in place of glucose. Instead, the amylase‐resistant starch was added to the glucose‐based ORS. |
| Roslund 2008 | This was not a clinical trial on ORS. |
| Sabchareon 1992 | Different electrolyte content of rice ORS and glucose‐based ORS. |
| Sarker 2001 | Participants with persistent diarrhoea (more than 14 days). |
| Sirivichayakul 2000 | Different electrolyte composition of the 2 groups. |
| Teferedegn 1993 | This was not an efficacy but an effectiveness study. |
| Yang 2007 | This was a clinical trial on the use of reduced osmolarity ORS in acute diarrhoea. Not a clinical trial on the use of polymer‐based ORS. |
| Yartev 1995 | Different electrolyte composition of the 2 groups. |
| Yurdakök 1995 | The study only observed participants during the rehydration phase. The primary outcome of interest relevant to the study was not evaluated. |
| Zaman 2007 | This was not a clinical trial on ORS. |
| Zavaleta 2007 | Different electrolyte composition of the 2 groups. |
Abbreviations: ORS: oral rehydration solution; RCT: randomized controlled trial.
Differences between protocol and review
Change in title: we changed the review title to highlight the fact that this is a review of polymer‐based ORS (not glucose‐based ORS).
New author: EG Martinez joined the review author team after the protocol was published.
Data extraction: we originally planned to extract count data by determination of the total number of episodes in each group (if the episode is rare) or the number of person years in each group for each treatment arm (if the episode is common). However, during the assessment of the trials, the trials reported the number of participants with unscheduled use of intravenous fluid, and thus we considered it to be a dichotomous rather than a count outcome. Similarly, in the data extraction for number of episodes of vomiting, there were only four trials that reported this outcome, while nine clinical trials reported the number of participants with vomiting. We decided that we would report the latter. Other adverse effects that were reported in the trials included number of participants with hypokalaemia (low potassium levels) and those with development of persistent diarrhoea (diarrhoea of more than 10 days' duration from onset), which we also included in the review.
Data analysis: in multiple treatment arms with two or more polymer‐based ORS as treatment groups, we combined the outcomes as appropriate and compared them collectively with the control group. Most trials included both cholera and non‐cholera cases, and we collectively termed this group as having mixed pathogens rather than non‐cholera diarrhoea.
Subgroup analyses: these were limited to the osmolarity of the glucose ORS, the type of polymer, and the effects of participant's age and pathogen. The review authors did not evaluate the source of the polymer and the effect of feeding as most of the polymers were locally prepared and only one trial withheld feeding after hydration.
Publication bias: we confirmed the presence of publication bias with a statistical software programme (StatsDirect 2008).
Contributions of authors
GV Gregorio was the principal investigator, wrote the protocol (Gregorio 2007), assessed the methodological quality of the included studies using the GRADE approach, performed data extraction and analysis, and wrote the final manuscript. MLM Gonzales helped to write the protocol, carried out the 'Risk of bias' (methodological quality) assessment and data extraction, and commented on the final manuscript. LF Dans assessed the methodological quality of the included studies using the GRADE approach and commented on the final manuscript. EG Martinez performed data extraction.
Sources of support
Internal sources
Liverpool School of Tropical Medicine, UK.
External sources
-
Department for International Development (DFID), UK.
Grant: 5242
Declarations of interest
Germana V. Gregorio has no known conflicts of interest. Maria Liza M. Gonzales has no known conflicts of interest. Leonila F. Dans has no known conflicts of interest. Elizabeth G. Martinez was employed as Director of Unilab Medical Education and Development of United Laboratories, Inc. from August 2009 to February 2015.
Unchanged
References
References to studies included in this review
Akbar 1991 {published data only}
- Akbar MS, Baker KM, Aziz MA, Khan WA, Salim AF. A randomised, double‐blind clinical trial of a maltodextrin containing oral rehydration solution in acute infantile diarrhoea. Journal of Diarrhoeal Diseases Research 1991;9(1):33‐7. [PubMed] [Google Scholar]
Alam 1987 {published data only}
- Alam AN, Sarker SA, Molla AM, Rahaman MM, Greenhough WB 3rd. Hydrolyzed wheat based oral rehydration solution for acute diarrhoea. Archives of Disease in Childhood 1987;62(5):440‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alam 1987, rice {published data only}
- Alam AN, Sarker SA, Molla AM, Rahaman MM, Greenhough WB 3rd. Hydrolyzed wheat based oral rehydration solution for acute diarrhoea. Archives of Disease in Childhood 1987;62(5):440‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alam 1987, wheat {published data only}
- Alam AN, Sarker SA, Molla AM, Rahaman MM, Greenhough WB 3rd. Hydrolyzed wheat based oral rehydration solution for acute diarrhoea. Archives of Disease in Childhood 1987;62(5):440‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alam 1992 {published data only}
- Alam NH, Ahmed T, Kharun M, Molla AM. Effects of food with two oral rehydration therapies: a randomised controlled clinical trial. Gut 1992;33(4):560‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bernal 2005 {published data only}
- Bernal C, Alcaraz GM, Bolero JE. Oral rehydration with a plantain flour‐based solution precooked with standardized electrolytes [Hidratación oral con una solución a based de harina de plátano precocida con electrolitos estandrarizados]. Biomédica 2005;25(1):11‐21. [PubMed] [Google Scholar]
Bhan 1987 {published data only}
- Bhan MK, Ghai OP, Khoshoo V, Vasudev A, Bhatnagar S, Arora NK, et al. Efficacy of mung bean (lentil) and pop rice based rehydration solutions in comparison with standard glucose electrolyte solution. Journal of Pediatric Gastroenterology and Nutrition 1987;6(3):392‐9. [DOI] [PubMed] [Google Scholar]
Bhan 1987, mung bean {published data only}
- Bhan MK, Ghai OP, Khoshoo V, Vasudev A, Bhatnagar S, Arora NK, et al. Efficacy of mung bean (lentil) and pop rice based rehydration solutions in comparison with standard glucose electrolyte solution. Journal of Pediatric Gastroenterology and Nutrition 1987;6(3):392‐9. [DOI] [PubMed] [Google Scholar]
Bhan 1987, rice {published data only}
- Bhan MK, Ghai OP, Khoshoo V, Vasudev A, Bhatnagar S, Arora NK, et al. Efficacy of mung bean (lentil) and pop rice based rehydration solutions in comparison with standard glucose electrolyte solution. Journal of Pediatric Gastroenterology and Nutrition 1987;6(3):392‐9. [DOI] [PubMed] [Google Scholar]
Bhattacharya 1998 {published data only}
- Bhattacharya MK, Bhattacharya SK, Dutta D, Deb AK, Deb M, Dutta A, et al. Efficacy of oral hyposmolar glucose‐based and rice‐based oral rehydration salt solutions in the treatment of cholera in adults. Scandinavian Journal of Gastroenterology 1998;33(2):159‐63. [DOI] [PubMed] [Google Scholar]
Dutta 1988 {published data only}
- Dutta P, Dutta S, Bhattacharya MK, Bhattacharya SK, Sinha AK, Mondal BC, et al. Comparative efficacy of three different oral rehydration solutions for treatment of dehydrating diarrhoea in children. Indian Journal of Medical Research 1988;87:229‐33. [PubMed] [Google Scholar]
Dutta 1998 {published data only}
- Dutta D, Bhattacharya MK, Deb A, Chowdhury AS, Nair GB, Ramakrishna BS, et al. Uncooked rice powder in oral rehydration solution: an alternative to glucose or cooked rice powder. Indian Journal of Medical Research 1998;107:257‐62. [PubMed] [Google Scholar]
Dutta 1998, adults {published data only}
- Dutta D, Bhattacharya MK, Deb A, Chowdhury AS, Nair GB, Ramakrishna BS, et al. Uncooked rice powder in oral rehydration solution: an alternative to glucose or cooked rice powder. Indian Journal of Medical Research 1998;107:257‐62. [PubMed] [Google Scholar]
Dutta 1998, children {published data only}
- Dutta D, Bhattacharya MK, Deb A, Chowdhury AS, Nair GB, Ramakrishna BS, et al. Uncooked rice powder in oral rehydration solution: an alternative to glucose or cooked rice powder. Indian Journal of Medical Research 1998;107:257‐62. [PubMed] [Google Scholar]
Dutta 2000 {published data only}
- Dutta D, Bhattacharya MK, Deb AK, Sarkar D, Chatterjee A, Biswas AB, et al. Evaluation of oral hypo‐osmolar glucose‐based and rice‐based oral rehydration solutions in the treatment of cholera in children. Acta Paediatrica 2000;89(7):787‐90. [PubMed] [Google Scholar]
el‐Mougi 1988 {published data only}
- el‐Mougi M, Hegazi E, Galal O, Akkad N, el‐Abhar A, Nour N, et al. Controlled clinical trial on the efficacy of rice powder‐based oral rehydration solution on the outcome of acute diarrhea in infants. Journal of Pediatric Gastroenterology and Nutrition 1988;7(4):572‐6. [DOI] [PubMed] [Google Scholar]
el‐Mougi 1996 {published data only}
- el‐Mougi M, Hendawi A, Koura H, Hegazi E, Fontaine O, Pierce N. Efficacy of standard glucose‐based and reduced osmolarity maltodextrin‐based oral rehydration solutions: effect of sugar malabsorption. Bulletin of the World Health Organization 1996;74(5):471‐7. [PMC free article] [PubMed] [Google Scholar]
Faruque 1997 {published data only}
- Faruque ASG, Hoque SS, Fuchs GJ, Mahalanabis D. Randomized, controlled, clinical trial of rice versus glucose oral rehydration solutions in infants and young children with acute watery diarrhoea. Acta Paediatrica 1997;86(12):1308‐11. [DOI] [PubMed] [Google Scholar]
Fayad 1993 {published data only}
- Fayad IM, Hasham M, Duggan C, Refat M, Bakir M, Fontaine O, et al. Comparative efficacy of rice‐based and glucose‐based oral rehydration salts plus early reintroduction of food. The Lancet 1993;342(8874):772‐5. [DOI] [PubMed] [Google Scholar]
Guiraldes 1995a {published data only}
- Guiraldes E, Triviño X, Figueroa G, Parker M, Gutiérrez C, Vásquez A, et al. Comparison of an oral rice‐based electrolyte solution and a glucose‐based electrolyte solution in hospitalized infants with diarrheal dehydration. Journal of Pediatric Gastroenterology and Nutrition 1995;20(4):417‐24. [DOI] [PubMed] [Google Scholar]
Guiraldes 1995b {published data only}
- Guiraldes E, Triviño X, Hodgson M, Quintana J, Quintana C. Treatment of acute infantile diarrhoea with a commercial rice‐based oral rehydration solution. Journal of Diarrhoeal Disease Research 1995;13(4):207‐11. [PubMed] [Google Scholar]
Hossain 2003 {published data only}
- Hossain M, Salam M, Rabbani GH, Kahir I, Biswas R, Mahalanabis D. Rice‐ORS versus glucose‐ORS in management of severe cholera due to Vibrio cholerae 0139 Bengal: a randomized, controlled clinical trial. Journal of Health, Population, and Nutrition 2003;21(4):325‐31. [PubMed] [Google Scholar]
Intarakhao 2010 {published data only}
- Intarakhao S, Sritipsukho P, Aue‐u‐lan K. Effectiveness of packed rice‐oral rehydration solution among children with acute watery diarrhea. Journal of the Medical Association of Thailand 2010;93(Suppl 7):S21‐5. [PubMed] [Google Scholar]
Islam 1994 {published data only}
- Islam A, Molla AM, Ahmed MA, Yameen A, Thara R, Molla A, et al. Is rice based oral rehydration therapy effective in young infants?. Archives of Disease in Childhood 1994;71(1):19‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iyngkaran 1998 {published data only}
- Iyngkaran N, Yadev M. Rice‐starch oral rehydration therapy in neonates and young infants. Journal of Tropical Pediatrics 1998;44(4):199‐203. [DOI] [PubMed] [Google Scholar]
Maulen‐Radovan 1994 {published data only}
- Maulen‐Radovan I, Fernandez‐Varela H, Acosta‐Bastidas M, Frenk S. Safety and efficacy of a rice‐based oral rehydration salt solution in the treatment of diarrhea in infants less than 6 months of age. Journal of Pediatric Gastroenterology and Nutrition 1994;19(1):78‐82. [DOI] [PubMed] [Google Scholar]
Maulen‐Radovan 2004 {published data only}
- Maulen‐Radovan I, Gutierrez‐Castrellón P, Hashem M, Neylan M, Braggs G, Zaldo R, et al. Safety and efficacy of a premixed rice‐based oral rehydration solution. Journal of Pediatric Gastroenterology and Nutrition 2004;38(2):159‐63. [DOI] [PubMed] [Google Scholar]
Mohan 1988 {published data only}
- Mohan M, Antony TJ, Malik S, Mathur M. Rice powder oral rehydration solution as an alternative to glucose electrolyte solution. Indian Journal of Medical Research 1988;87:234‐9. [PubMed] [Google Scholar]
Molla 1985 {published data only}
- Molla AM, Ahmed SM, Greenough WB 3rd. Rice‐based oral rehydration solution decreases the stool volume in acute diarrhoea. Bulletin of the World Health Organization 1985;63(4):751‐6. [PMC free article] [PubMed] [Google Scholar]
Molla 1985, adults {published data only}
- Molla AM, Ahmed SM, Greenough WB 3rd. Rice‐based oral rehydration solution decreases the stool volume in acute diarrhoea. Bulletin of the World Health Organization 1985;63(4):751‐6. [PMC free article] [PubMed] [Google Scholar]
Molla 1985, children {published data only}
- Molla AM, Ahmed SM, Greenough WB 3rd. Rice‐based oral rehydration solution decreases the stool volume in acute diarrhoea. Bulletin of the World Health Organization 1985;63(4):751‐6. [PMC free article] [PubMed] [Google Scholar]
Molla 1989a {published data only}
- Molla AM, Molla A, Rohde J, Greenough WB 3rd. Turning off the diarrhea: the role of food and ORS. Journal of Pediatric Gastroenterology and Nutrition 1989;8(1):81‐4. [DOI] [PubMed] [Google Scholar]
Molla 1989b {published data only}
- Molla AM, Molla A, Nath SK, Khatun M. Food‐based oral rehydration salt solution for acute childhood diarrhoea. The Lancet 1989;2(8660):429‐31. [DOI] [PubMed] [Google Scholar]
Molla 1989b, rice {published data only}
- Molla AM, Molla A, Nath SK, Khatun M. Food‐based oral rehydration salt solution for acute childhood diarrhoea. The Lancet 1989;2(8660):429‐31. [DOI] [PubMed] [Google Scholar]
Molla 1989b, sorghum {published data only}
- Molla AM, Molla A, Nath SK, Khatun M. Food‐based oral rehydration salt solution for acute childhood diarrhoea. The Lancet 1989;2(8660):429‐31. [DOI] [PubMed] [Google Scholar]
Molla 1989b, wheat {published data only}
- Molla AM, Molla A, Nath SK, Khatun M. Food‐based oral rehydration salt solution for acute childhood diarrhoea. The Lancet 1989;2(8660):429‐31. [DOI] [PubMed] [Google Scholar]
Mustafa 1995 {published data only}
- Mustafa SA, Karrar ZE, Suliman JI. Cereal‐based oral rehydration solutions in Sudanese children with diarrhoea: a comparative clinical trial of rice‐based and sorghum‐based oral rehydration solutions. Annals of Tropical Paediatrics 1995;15(4):313‐9. [DOI] [PubMed] [Google Scholar]
Mustafa 1995, rice {published data only}
- Mustafa SA, Karrar ZE, Suliman JI. Cereal‐based oral rehydration solutions in Sudanese children with diarrhoea: a comparative clinical trial of rice‐based and sorghum‐based oral rehydration solutions. Annals of Tropical Paediatrics 1995;15(4):313‐9. [DOI] [PubMed] [Google Scholar]
Mustafa 1995, sorghum {published data only}
- Mustafa SA, Karrar ZE, Suliman JI. Cereal‐based oral rehydration solutions in Sudanese children with diarrhoea: a comparative clinical trial of rice‐based and sorghum‐based oral rehydration solutions. Annals of Tropical Paediatrics 1995;15(4):313‐9. [DOI] [PubMed] [Google Scholar]
Nanulescu 1999 {published data only}
- Nanulescu M, Popa M, Panta P, Butanariu A, Muresan M, Gocan S, et al. The efficacy of an oral‐rice based electrolyte solution in infants with acute diarrhea as compared to a glucose‐based electrolyte solution. Romanian Journal of Gastroenterology 1999;8(3):177‐82. [Google Scholar]
Patra 1982 {published data only}
- Patra FC, Mahalanabis D, Jalan KN, Sen A, Banerjee P. Is oral rice electrolyte solution superior to glucose electrolyte solution in infantile diarrhoea?. Archives of Disease in Childhood 1982;57(12):910‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramakrishna 2000 {published data only}
- Ramakrishna B, Venkataraman S, Srinivasan P, Dash P, Young G, Binder H. Amylase‐resistant starch plus oral rehydration solution for cholera. The New England Journal of Medicine 2000;342(5):308‐13. [DOI] [PubMed] [Google Scholar]
Ramakrishna 2000, amylase {published data only}
- Ramakrishna B, Venkataraman S, Srinivasan P, Dash P, Young G, Binder H. Amylase‐resistant starch plus oral rehydration solution for cholera. The New England Journal of Medicine 2000;342(5):308‐13. [DOI] [PubMed] [Google Scholar]
Ramakrishna 2000, rice {published data only}
- Ramakrishna B, Venkataraman S, Srinivasan P, Dash P, Young G, Binder H. Amylase‐resistant starch plus oral rehydration solution for cholera. The New England Journal of Medicine 2000;342(5):308‐13. [DOI] [PubMed] [Google Scholar]
Ramakrishna 2008 {published data only}
- Ramakrishna B, Subramanian V, Mohan V, Sebastian BK, Young GP, Farthing MJ, et al. A randomized controlled trial of glucose versus amylase resistant starch hypo‐osmolar oral rehydration solution for adult acute dehydrating diarrhea. PLoS One 2008;3(2):e1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
Razafindrakoto 1993 {published data only}
- Razafindrakoto O, Ravelomanana N, Randriamiharisoa F, Rasoarivao V, Ramialimanana V, Rakotoarimanana D, et al. Rice‐based rehydration solution: an alternative to glucose‐based solutions in acute diarrhea in malnourished children [La solution de réhydration orale (SRO) à base de riz, une alternative de la SRO de l'OMS dans la diarrhée aiguë chez les patients souffrant de malnutrition]. Archives Françaises de Pédiatrie 1993;50(2):101‐5. [PubMed] [Google Scholar]
Santos Ocampo 1993 {published data only}
- Santos Ocampo PD, Bravo LC, Rogacion JM, Battad GR. A randomized double‐blind clinical trial of a maltodextrin‐containing oral rehydration solution in acute infantile diarrhea. Journal of Pediatric Gastroenterology and Nutrition 1993;16(1):23‐8. [DOI] [PubMed] [Google Scholar]
Sharma 1998 {published data only}
- Sharma A, Pradhan RK. Comparative study of rice‐based oral rehydration salt solution versus glucose‐based oral rehydration salt solution (WHO) in children with acute dehydrating diarrhoea. Journal of Indian Medical Association 1998;96(12):367‐8. [PubMed] [Google Scholar]
Wall 1997 {published data only}
- Wall CR, Swanson CE, Cleghorn GJ. A controlled trial comparing the efficacy of rice‐based and hypotonic glucose oral rehydration solutions in infants and young children with gastroenteritis. Journal of Gastroenterology and Hepatology 1997;12(1):24‐8. [DOI] [PubMed] [Google Scholar]
Zaman 2001 {published data only}
- Zaman K, Yunus M, Rahman A, Chowdhury HR, Sack DA. Efficacy of a packaged rice oral rehydration solution among children with cholera and cholera‐like illness. Acta Paediatrica 2001;90(5):505‐10. [PubMed] [Google Scholar]
References to studies excluded from this review
Agustina 2007 {published data only}
- Agustina R, Lukito W, Firmansyah A, Suhardjo HN, Murniati D, Bindels J. The effect of nutritional supplementation with a mixture of probiotic, prebiotic, fiber and micronutrients in infants with acute diarrhoea in Indonesia. Asia Pacific Journal of Clinical Nutrition 2007;16(3):435‐42. [PubMed] [Google Scholar]
Alam 2008 {published data only}
- Alam N, Ashraf H, Sarker SA, Olesen M, Troup J, Salam MA, et al. Efficacy of partially hydrolyzed guar gum added oral rehydration solution in the treatment of severe cholera in adults. Digestion 2008;78(1):24‐9. [DOI] [PubMed] [Google Scholar]
Alam 2009 {published data only}
- Alam NH, Islam S, Sattar S, Monira S, Desjeux JF. Safety of rapid intravenous rehydration and comparative efficacy of 3 oral rehydration solutions in the treatment of severely malnourished children with dehydrating cholera. Journal of Pediatric Gastroenterology and Nutrition 2009;48(3):318‐27. [DOI] [PubMed] [Google Scholar]
Ansaldi 1990 {published data only}
- Ansaldi N, Dell'Olio D, Poli E, Grandi G. Importance of oral rehydration in acute infantile diarrhea. Comparison of 2 rehydration solutions [Importanza della reidratzaione orale nelle diarree acute infantili]. Minerva Pediatrica 1990;42(1‐2):9‐14. [PubMed] [Google Scholar]
Barclay 1995 {published data only}
- Barclay D, Gil‐Ramos J, Mora JO, Dirren H. A packaged rice‐based oral rehydration solution for acute diarrhea. Journal of Pediatric Gastroenterology and Nutrition 1995;20(4):408‐16. [DOI] [PubMed] [Google Scholar]
Barragan‐Guzmán 1998 {published data only}
- Barragan‐Guzmán B, Orozco‐Alatorre L, Mariscal‐Zuno S. Corn meal solution compared to oral saline solution in the treatment of children with acute diarrhea and high fecal output [Atole de maiz comparado con Vida Suero Oral en el tratamiento de niños con diarrea aguda de gasto fecal alto]. Boletín Médico del Hospital Infantil de México 1998;55(2):65‐8. [Google Scholar]
Bhandari 2008 {published data only}
- Bhandari N, Mazumder S, Taneja S, Dube B, Agarwal RC, Mahalanabis D, et al. Effectiveness of zinc supplementation plus oral rehydration salts compared with oral rehydration salts alone as a treatment for acute diarrhoea in a primary care setting: a cluster randomised trial. Pediatrics 2008;121(5):e1279‐85. [DOI] [PubMed] [Google Scholar]
Cohen 1995 {published data only}
- Cohen MB, Mezoff AG, Laney DW Jr, Bezerra JA, Beane BM, Drazner D, et al. Use of a single solution for oral rehydration and maintenance therapy of infants with diarrhea and mild to moderate dehydration. Pediatrics 1995;95(5):639‐45. [PubMed] [Google Scholar]
Gutiérrez 2007 {published data only}
- Gutiérrez C, Villa S, Mota FR, Calva JJ. Does an L‐glutamine containing glucose free oral rehydration solution reduce stool output and time to rehydrate in children with acute diarrhea? A double blind randomized clinical trial. Journal of Health Population and Nutrition 2007;25(3):278‐84. [PMC free article] [PubMed] [Google Scholar]
Hoekstra 2004 {published data only}
- Hoekstra J, Szajewska H, Zikri MA, Micetic‐Turk D, Weizman Z, Papadopoulou A, et al. Oral rehydration solution containing a mixture of non‐digestible carbohydrates in the treatment of acute diarrhea: a multicenter randomized placebo controlled study on behalf of the ESPGHAN working group on intestinal infections. Journal of Pediatric Gastroenterology and Nutrition 2004;39(3):239‐45. [DOI] [PubMed] [Google Scholar]
Jirapinyo 1996 {published data only}
- Jirapinyo P, Moran JR. Comparison of oral rehydration solutions made with rice syrup solids or glucose in the treatment of acute diarrhea in infants. Journal of the Medical Association of Thailand 1996;79(3):154‐60. [PubMed] [Google Scholar]
Kassaye 1994 {published data only}
- Kassaye M, Larson C, Carlson D. A randomized community trial of prepackaged and homemade oral rehydration therapies. Archives of Pediatrics and Adolescent Medicine 1994;148(12):1288‐92. [DOI] [PubMed] [Google Scholar]
Kenya 1989 {published data only}
- Kenya PR, Odongo HW, Oundo G, Waswa K, Muttunga J, Molla A, et al. Cereal based oral rehydration solutions. Archives of Disease in Childhood 1989;64(7):1032‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lebenthal 1995 {published data only}
- Lebenthal E, Khin‐Maung‐U, Khin‐Myat‐Tun, Tin‐Nu‐Swe, Thein‐Thein‐Myint, Jirapinyo P, et al. High‐calorie, rice‐derived, short‐chain, glucose polymer‐based oral rehydration solution in acute watery diarrhea. Acta Paediatrica 1995;84(2):165‐72. [DOI] [PubMed] [Google Scholar]
Molina 1995 {published data only}
- Molina S, Vettorazzi C, Peerson J, Solomons N, Brown K. Clinical trial of glucose‐oral rehydration solution, rice dextrin‐ORS, and rice flour‐ORS for the management of children with acute diarrhea and mild or moderate dehydration. Pediatrics 1995;95(2):191‐7. [PubMed] [Google Scholar]
Molla 1982 {published data only}
- Molla AM, Sarker SA, Hossain M, Molla A, Greenough WB 3rd. Rice‐powder electrolyte solution as oral‐therapy in diarrhoea due to Vibrio cholerae and Escherichia coli. The Lancet 1982;1(8285):1317‐9. [DOI] [PubMed] [Google Scholar]
Molla 2000 {published data only}
- Molla A, Bari A, Greenough WB 3rd, Molla AM, Budhiraja P, Sharma PN. Bangladeshi rural mothers prepare safer rice oral rehydration solutions. Acta Paediatrica 2000;89(7):791‐4. [PubMed] [Google Scholar]
Mota‐Hernández 1991 {published data only}
- Mota‐Hernández F, Bross‐Soriano D, Pérez‐Ricardez M, Velásquez‐Jones L. Rice solution and World Health Organization solution by gastric infusion for high stool output diarrhea. American Journal of Diseases of Childhood 1991;145(8):937‐40. [DOI] [PubMed] [Google Scholar]
Murphy 1996 {published data only}
- Murphy H, Bari A, Molla AM, Zaidi A, Hirschhorn N. A field trial of wheat‐based oral rehydration solution among Afghan refugee children. Acta Paediatrica 1996;85(2):151‐7. [DOI] [PubMed] [Google Scholar]
Patra 1984 {published data only}
- Patra F, Mahalanabis D, Jalan KN, Sen A, Banerjee P. In search of a super solution: controlled trial of glycine‐glucose oral rehydration solution in infantile diarrhoea. Acta Paediatrica Scandinavica 1984;73(1):18‐21. [DOI] [PubMed] [Google Scholar]
Pelleboer 1990 {published data only}
- Pelleboer RA, Felius A, Goje BS, Gelderen HH. Sorghum‐based oral rehydration solution in the treatment of acute diarrhoea. Tropical and Geographical Medicine 1990;42(1):63‐8. [PubMed] [Google Scholar]
Pizarro 1991 {published data only}
- Pizarro D, Posada G, Sandi L, Moran JR. Rice‐based oral electrolyte solutions for the management of infantile diarrhea. The New England Journal of Medicine 1991;324(8):517‐21. [DOI] [PubMed] [Google Scholar]
Prasad 1993 {published data only}
- Prasad B. Rice‐based oral rehydration solution: a controlled clinical trial in Nepal. Journal of Tropical Pediatrics 1993;39(6):368‐9. [DOI] [PubMed] [Google Scholar]
Rabbani 2005 {published data only}
- Rabbani GH, Sack DA, Ahmed S, Peterson JW, Saha SK, Marni F, et al. Antidiarrheal effects of L‐histidine supplemented rice‐based oral rehydration solution in the treatment of male adults with severe cholera in Bangladesh: a double‐blind randomized trial. The Journal of Infectious Diseases 2005;191(9):1507‐14. [DOI] [PubMed] [Google Scholar]
Raghupathy 2006 {published data only}
- Raghupathy P, Ramakrishna BS, Oommen SP, Ahmed MS, Priyas G, Dziura J, et al. Amylase‐resistant starch as adjunct to oral rehydration therapy in children with diarrhea. Journal of Pediatric Gastroenterology and Nutrition 2006;42(4):362‐8. [DOI] [PubMed] [Google Scholar]
Roslund 2008 {published data only}
- Roslund G, Hepps TS, McQuillen KK. The role of ondansetron in children with vomiting as a result of acute gastritis/gastroenteritis who have failed oral rehydration therapy: a randomized controlled trial. Annals of Emergency Medicine 2008;52(1):22‐9.e.6. [DOI] [PubMed] [Google Scholar]
Sabchareon 1992 {published data only}
- Sabchareon A, Chongsuphajaisiddhi T, Kittikoon P, Chanthavanich P. Rice‐powder salt solution in the treatment of acute diarrhea in young children. Southeast Asian Journal of Tropical Medicine and Public Health 1992;23(3):427‐32. [PubMed] [Google Scholar]
Sarker 2001 {published data only}
- Sarker S, Mahalanabis D, Alam NH, Sharmin S, Khan AM, Fuchs GJ. Reduced osmolarity oral rehydration solution for persistent diarrhea in infants: a randomized controlled clinical trial. The Journal of Pediatrics 2001;138(4):532‐8. [DOI] [PubMed] [Google Scholar]
Sirivichayakul 2000 {published data only}
- Sirivichayakul C, Chokejindachai W, Vithayasai N, Chanthavanich P, Pengsaa K, Wisetsing P, et al. Effects of rice powder salt solution and milk‐rice mixture on acute watery diarrhoea in young children. Southeast Asian Journal of Tropical Medicine and Public Health 2000;31(2):354‐9. [PubMed] [Google Scholar]
Teferedegn 1993 {published data only}
- Teferedegn B, Larson CP, Carlson D. A community‐based randomized trial of home‐made oral rehydration therapies. International Journal of Epidemiology 1993;22(5):917‐22. [DOI] [PubMed] [Google Scholar]
Yang 2007 {published data only}
- Yang DF, Guo W, Tian DY, Luo XP, He YW, Dai YA, et al. Efficacy and safety of reduced osmolality oral rehydration salts in treatment of dehydration in children with acute diarrhea ‐ a multicenter, randomized, double blind clinical trial. Zhonghua Er Ke Za Zhi [Chinese Journal of Pediatrics] 2007;45(4):252‐5. [PubMed] [Google Scholar]
Yartev 1995 {published data only}
- Yartev J, Nkrumah F, Hori H, Harrison K, Armar D. Clinical trial of fermented maize‐based oral rehydration solution in the management of acute diarrhoea in children. Annals of Tropical Paediatrics 1995;15(1):61‐8. [DOI] [PubMed] [Google Scholar]
Yurdakök 1995 {published data only}
- Yurdakök K, Yalçin S. Comparative efficacy of rice‐ORS and glucose‐ORS in moderately dehydrated Turkish children with diarrhea. The Turkish Journal of Pediatrics 1995;37(4):315‐21. [PubMed] [Google Scholar]
Zaman 2007 {published data only}
- Zaman S, Mannan J, Lange S, Lönnroth I, Hanson LA. B 221, a medical food containing antisecretory factor reduces child diarrhoea: a placebo controlled trial. Acta Paediatrica 2007;96(11):1655‐9. [DOI] [PubMed] [Google Scholar]
Zavaleta 2007 {published data only}
- Zavaleta N, Figueroa D, Rivera J, Sánchez J, Alfaro S, Lönnerdal B. Efficacy of rice‐based oral rehydration solution containing recombinant human lactoferrin and lysozyme in Peruvian children with acute diarrhea. Journal of Pediatric Gastroenterology and Nutrition 2007;44(2):258‐64. [DOI] [PubMed] [Google Scholar]
Additional references
Carpenter 1988
- Carpenter CC, Greenough WB, Pierce NF. Oral‐rehydration therapy‐‐the role of polymeric substrates. The New England Journal of Medicine 1988;319(20):1346‐8. [DOI] [PubMed] [Google Scholar]
Casburn‐Jones 2004
- Casburn‐Jones AC, Farthing MJ. Management of infectious diarrhoea. Gut 2004;53(2):296‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
CHOICE 2001
- CHOICE Study Group. Multicenter, randomized double blind clinical trial to evaluate the efficacy and safety of a reduced osmolality oral rehydration salts solution in children with acute watery diarrhea. Pediatrics 2001;107(4):613‐8. [DOI] [PubMed] [Google Scholar]
Claeson 1990
- Claeson M, Merson MH. Global progress in the control of diarrheal diseases. The Pediatric Infectious Disease Journal 1990;9(5):345‐55. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clinical Trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Fontaine 1998
- Fontaine O, Gore SM, Pierce NF. Rice‐based oral rehydration solution for treating diarrhoea. Cochrane Database of Systematic Reviews 1998, Issue 4. [DOI: 10.1002/14651858.CD001264.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2014 [Computer program]
- GRADE Working Group, McMaster University. GRADEpro GDT. Version accessed 10 August 2015. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Hahn 2002
- Hahn S, Kim Y, Garner P. Reduced osmolarity oral rehydration solution for treating dehydration caused by acute diarrhoea in children. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD002847] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunt 1992
- Hunt JB, Elliott EJ, Fairclough PD, Clark ML, Farthing MJ. Water and solute absorption from hypotonic glucose‐electrolyte solutions in human jejunum. Gut 1992;33(4):479‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kosek 2003
- Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease as estimated from studies published between 1992 and 2000. Bulletin of the World Health Organization 2003;81(3):197‐204. [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Santosham 1991
- Santosham M, Greenough WB 3rd. Oral rehydration therapy: a global perspective. The Journal of Pediatrics 1991;118(4 Pt 2):S44‐51; discussion S52. [DOI] [PubMed] [Google Scholar]
StatsDirect 2008 [Computer program]
- StatsDirect Ltd. StatsDirect. Version 2.6. Altrincham: StatsDirect Ltd, 1 June 2008.
Victora 2000
- Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bulletin of the World Health Organization 2000;78(10):1246‐55. [PMC free article] [PubMed] [Google Scholar]
WHO 2004
- World Health Organization Department of Child and Adolescent Health and Development. Clinical management of acute diarrhoea: WHO/UNICEF joint statement [WHO/FCH/CAH/04.7]. Geneva: World Health Organization, 2004. [Google Scholar]
WHO/icddr,b 1995
- World Health Organization, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr, b). 25 years of ORS: Joint WHO/ICDDR,B Consultative Meeting on ORS Formulation, Dhaka, Bangladesh, 10‐12 December 1994 [CDR/CDD/95.2]. Geneva: World Health Organization, 1995. [Google Scholar]
References to other published versions of this review
Gregorio 2007
- Gregorio GV, Gonzales LML, Dans LF, Martinez EG. Glucose polymer‐based oral rehydration solution for treating acute watery diarrhoea. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD006519] [DOI] [PubMed] [Google Scholar]
Gregorio 2009
- Gregorio GV, Gonzales MLM, Dans LF, Martinez EG. Polymer‐based oral rehydration solution for treating acute watery diarrhoea. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006519.pub2] [DOI] [PubMed] [Google Scholar]


