Abstract
The significantly higher implant failure rates in maxillofacial patients, undergoing radiotherapy, might be caused by the long-term effects of reduced vascularization compromising the implantation site. An extensive preclinical animal literature and a multitude of clinical reports suggest the use of hyperbaric oxygen (HBO) therapy as it can improve the tissue vascularity. Hence, it may increase the implant survival rate by enhancing osseointegration process in such patients. The objective of this systematic review was to investigate the effectiveness of HBO therapy on dental implant survival rate in irradiated maxillofacial patients who require prosthodontic rehabilitation. An electronic search without time restrictions was undertaken in April 2016 using databases: PubMed, Google Scholar, and the Cochrane Oral Health Group Trials Register. We also tried to contact the manufacturers and researchers in the field for necessary details. Clinical human studies, on irradiated maxillofacial dental implant patients, including randomized controlled trials (RCTs), prospective controlled trials, retrospective studies, and preliminary reports were included in the study. Data collection was carried out by two of the authors’ independently. The titles and abstracts of all reports were screened for the study design and type of reported intervention; all the duplicates were removed. The data search yielded 62 titles, out of which 14 articles were selected for the study by the article filtration criteria: Title/abstract/full text. Data which were extracted by two authors with any disagreement were resolved by the third author, and a meta-analysis was done using binary random-effect model. The results show decreased implant failure rate in HBO group (9.21%) compared to non-HBO group (22.44%). The potential limitations of this study are amount of radiation doses used, period lasting from radiotherapy to the placement of the implants, and follow-up period which varies for every subject of the included study, which can affect the treatment outcome. Although there are many sensitive articles published about HBO, including a number of review papers, RCTs are still lacking. According to the statistical analysis, it can be concluded that preventive HBO therapy can reduce the risk of implant failures in irradiated patients by 1.21 (relative risk) with 95% confidence interval (P < 0.001). Hence, HBO can be the effective treatment protocol for the implant treatment in irradiated maxillofacial patients.
Keywords: Dental implants, dental implant failures, hyperbaric oxygen, implants, irradiation, osseointegrated, radiotherapy, randomized controlled trials
INTRODUCTION
Description of the condition
Thorough knowledge and wide field of understanding of the etiologic and risk factors of the implant failure are necessary to decrease the implant failure rates. From the last few years, implants are more commonly used in maxillofacial oral cancer patients, so whether these irradiated patient in the head and neck region are more at risk of losing dental implants or not is still unclear. Reduced tissue healing capacity leads to osteoradionecrosis, necrotic bone exposure, and pathological fracture in response to tissue trauma; thus, with reduced healing ability and osteoradionecrosis in response to injury, the implant survival rate may be reduced for the maxillofacial oral cancer patients who have undergone radiotherapy treatment.[1,2,3,4,5,6]
Description of the intervention
Hyperbaric oxygen (HBO) therapy and its effectiveness is still a controversial topic.[7] There are numerous studies reported for the usefulness of HBO for the treatment of osteoradionecrosis of different bone tissues. In addition to its usefulness in treating osteoradionecrosis, it may also prevent this condition. A randomized/prospective clinical trial using HBO and penicillin was carried out by Marx et al.[8] This trial demonstrated that HBO reduced the development of osteoradionecrosis after tooth removal and this reduction was statistically significant.[9]
HBO therapy can be performed in multiplace or monoplace chambers. Patient is kept in a pure 100% oxygen chamber under pressure of 1.5–3 atmosphere absolute.[10]
How the intervention might work?
HBO therapy increases the oxygen pressure, collagen production, and fibroblastic activity and creates a matrix for neovascularizations.[11] According to Johnsson, it also counteracts the negative effect of irradiation, stimulates the osseointegration, and improves the implant survival rate.[12]
Need to do this systematic review
This systematic review helps maxillofacial surgeon and prosthodontist to understand the evidence, to integrate the valid information, and to provide rational decision-making on the use of the HBO therapy for their patients. It will also help them in improving the dental implant survival rate and quality of life of such patients by providing long-term successful rehabilitation.
OBJECTIVE
The objective of the present review was to compare the implant failure rates for patients being irradiated or previously irradiated in the head and neck region and receiving HBO therapy versus irradiated patients and not receiving such therapy having follow up period of 1-2 years to 26 years.
MATERIALS AND METHODS
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs), prospective clinical trials, and retrospective studies.
Types of participants
Maxillofacial patients who have had radiotherapy and treated with dental implants for oral rehabilitation.
Types of intervention
HBO therapy compared with no HBO therapy.
Type of comparison
HBO group versus non-HBO group.
Types of outcome measures
Implant failure rates.
SEARCH STRATEGIES
An electronic search without time restrictions was undertaken in April 2016 for clinical studies comparing the implant failure rates (O), in irradiated maxillofacial patients (P), undergoing dental implant treatment either with additional HBO therapy (I) or without HBO therapy (C), using following databases: PubMed, Google Scholar, and the Cochrane Oral Health Group Trials Register. The search strategy used a combination of controlled vocabulary and free text terms.
Following keywords were used in the search box of all three databases either alone or in combination with two or more keywords (i.e., #1, #2, #3, or #1, #2, #3, #5) in an attempt not to miss any related trial, eligible to get included in the study.
Dental implants or oral implants or endosseous implants or osseointegrated implants
Radiation therapy or radiotherapy or irradiation or irradiated tissues
Hyperbaric oxygen or hyperbaric oxygen therapy or HBO therapy or hyperbaric oxygenation
Dental implant failures and/or randomized controlled trials
HBO therapy and experimental trials
Irradiation, dental implants, HBO therapy, randomized controlled trials, experimental trials (Word variations had been used, i.e., radiotherapy for irradiation).
A manual search of dental implant-related journals, reference list of the identified studies, and relevant reviews on the subject was also scanned for possible additional studies. Moreover, online databases providing information about clinical trials in progress were also checked (clinicaltrials.gov; www.centerwatch.com/clinicaltrials; www.clinicalconnection.com; www.cochranelibrary.com).
Data collection and analysis
Selection of studies
The review process consisted of two phases. In the first phase, titles and abstracts of the search were initially screened by two authors for relevance and the full text of relevant abstract was obtained and accessed. Any disagreement was solved by discussion and with the third author's suggestion. The hand search of selected journals as well as search of reference of the selected studies was also done. The articles were obtained after first step of the review process using the following inclusion and exclusion criteria and were screened in the second phase, and relevant and suitable articles were isolated for further processing and data extraction. Duplicates and articles with insufficient necessary data were excluded.
Inclusion criteria's
Clinical human studies, on irradiated maxillofacial dental implant patients, including:
RCTs
Prospective study
Retrospective study
Preliminary reports.
Exclusion criteria's
Case reports
Technical reports
Animal studies
In vitro studies
Review articles
<5 patients treated.
In general, RCTs constitute the highest level of evidence. Although developing recommendations based on the highest level of evidence is desirable, adequate number of RCTs is not always available. Hence, we included some prospective and retrospective clinical studies with a preliminary report (Ali et al., 1997). The purpose of the report was to provide some preliminary data collected from a long-term, prospective investigation on the effects of HBO therapy on implant integration in the irradiated jaw. Data on the effects of various doses of irradiation to the perioral region were collected by regular clinical, radiologic, and histologic examinations.
Data extraction and management
Three review authors independently extracted data from the studies using standardized selection criteria, developed for this review. We tried to contact the authors of primary studies to request further information when data were missing or incomplete. Review authors resolved all differences by discussion. Data were excluded until further clarification became available if agreement could not be reached.
For each trial, the following data were recorded.
Year of publication and country of origin
Details of the participants including demographic characteristics and criteria for inclusion
Details of the type of intervention
Details of the outcomes reported including method of assessment and time intervals.
Assessment of “risk of bias” in the included study
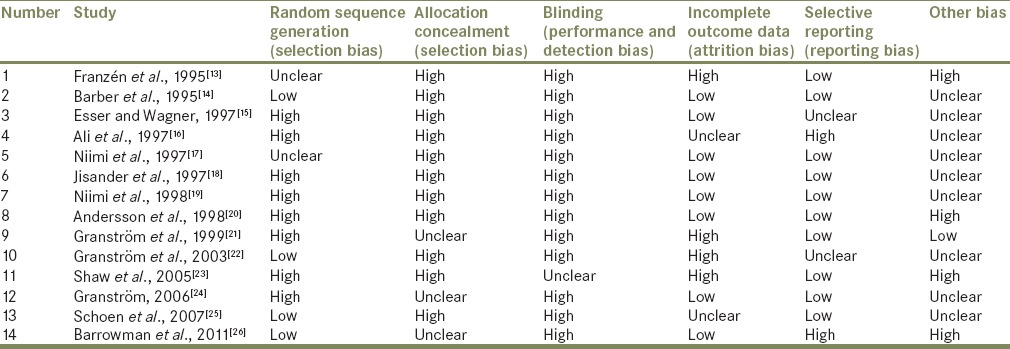
The assessment of the risk bias was conducted using the recommended approach by Cochrane reviews [Table 1 and Graph 1] and was completed independently and in duplicate by two review authors as a part of the data extraction process.
Table 1.
Assessment of “risk of bias” in the trials included in the meta-analysis
Graph 1.
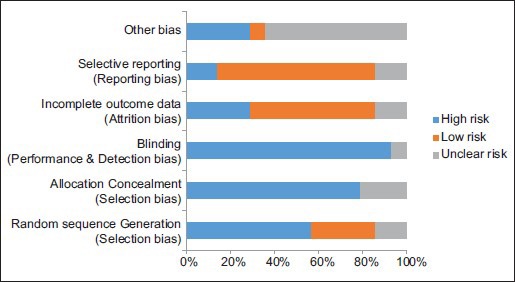
The assessment of the risk of bias of the included studies
Results of the search for data collection
The database search yielded 62 titles, out of which 22 titles were discarded by title evaluation. Abstracts evaluation was done for the remaining 40 articles, and 6 articles were discarded on the basis of inclusion and exclusion criteria. Full-text data were obtained for the remaining 34 articles, among which 8 articles were discarded due to insufficient data and 12 articles did not match the criteria of the study. Hence, finally, 14 articles were selected for the study [Flowchart 1].
Flowchart 1.
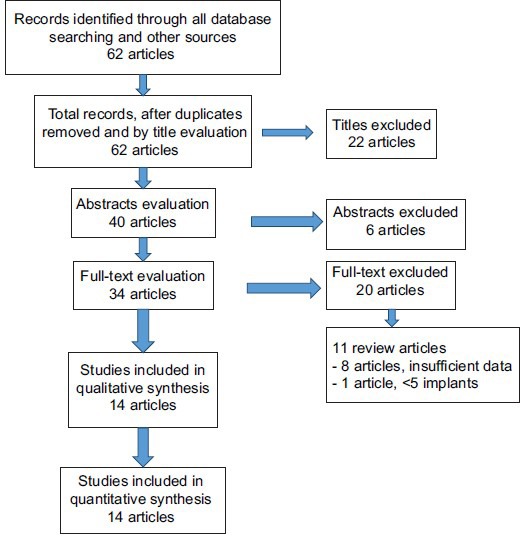
Results of the search through various sources
Description of the included studies
The data obtained after the search strategy were tabulated and statistically analyzed. The results were as follows:
Table 2 shows the required details, regarding the 14 selected studies, included in this systematic review
Table 3 shows the evidence level of the selected articles according to the study design
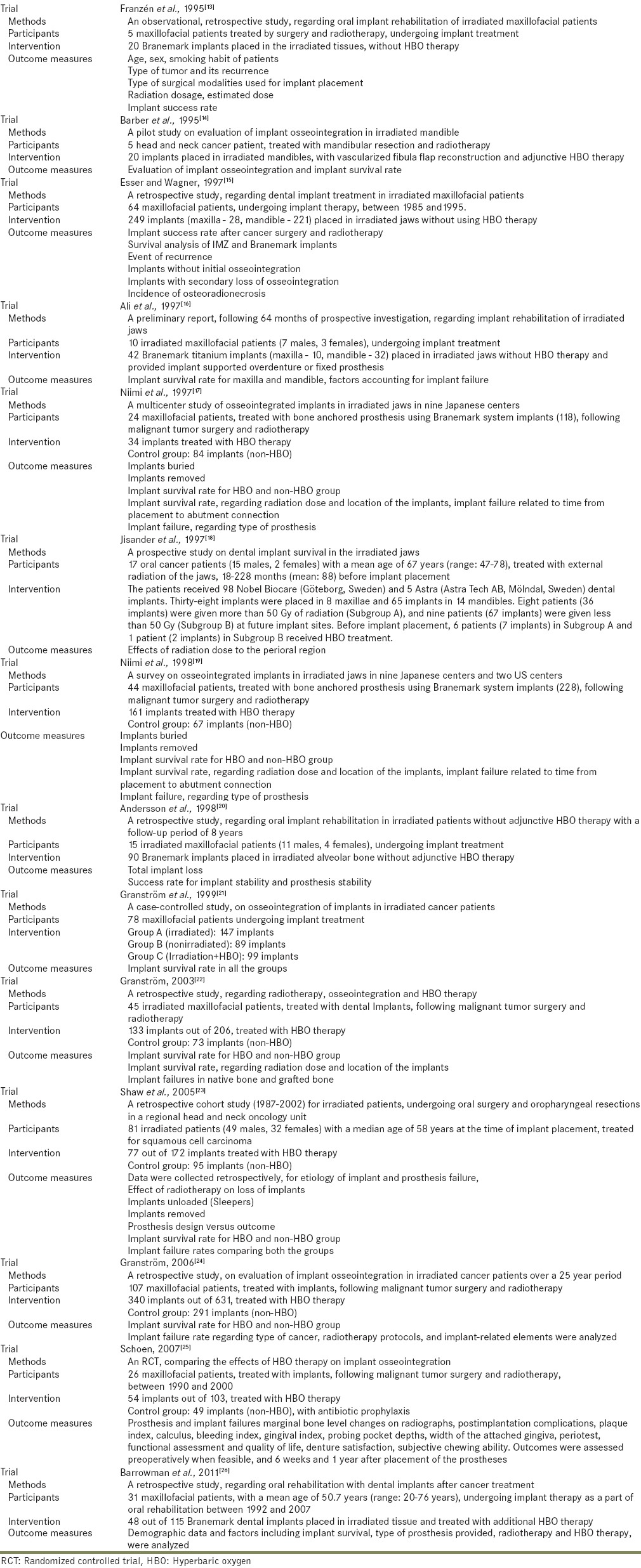
Table 4 shows the characteristics of the each included study.
Table 2.
Summarized data
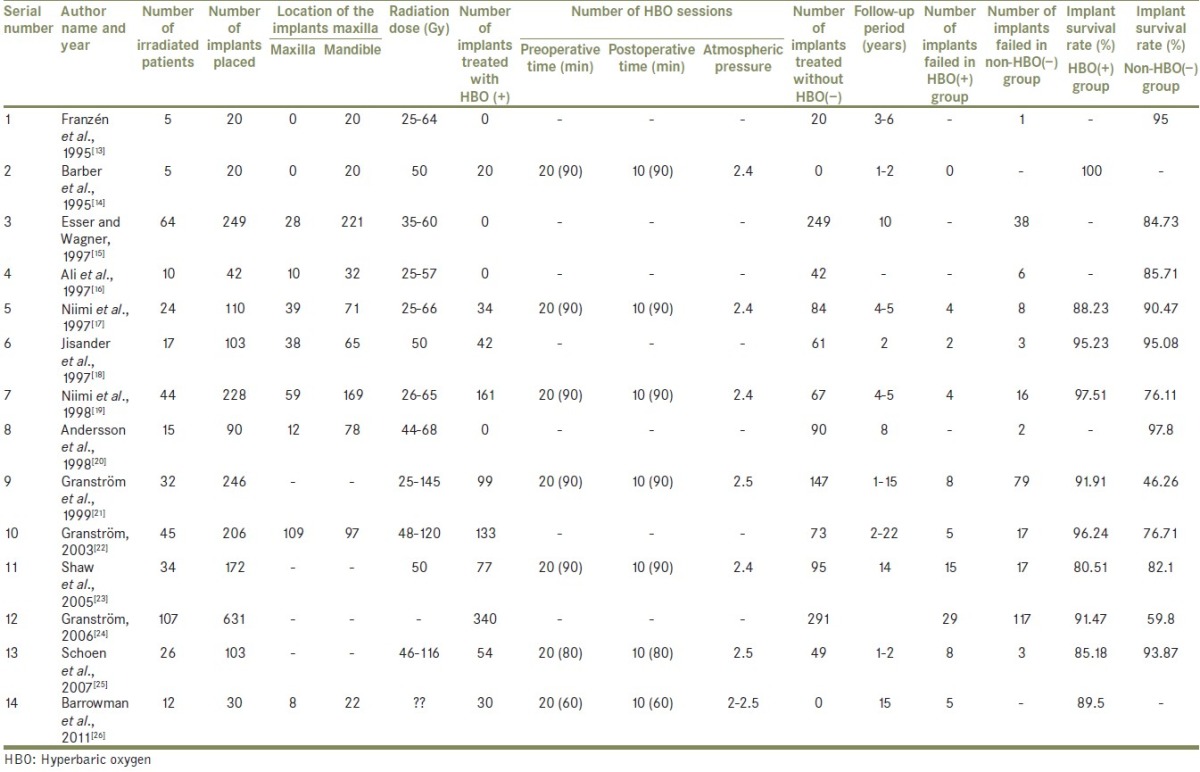
Table 3.
Evidence level of selected articles
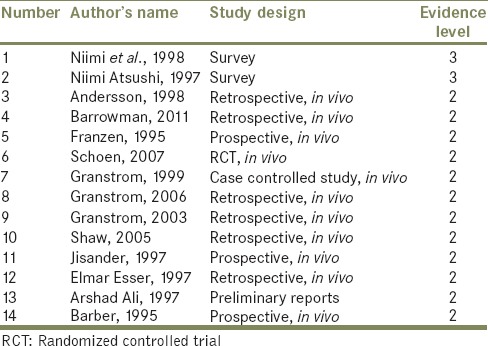
Table 4.
Characteristics of included studies
Description of the excluded studies (with the reason for being excluded)
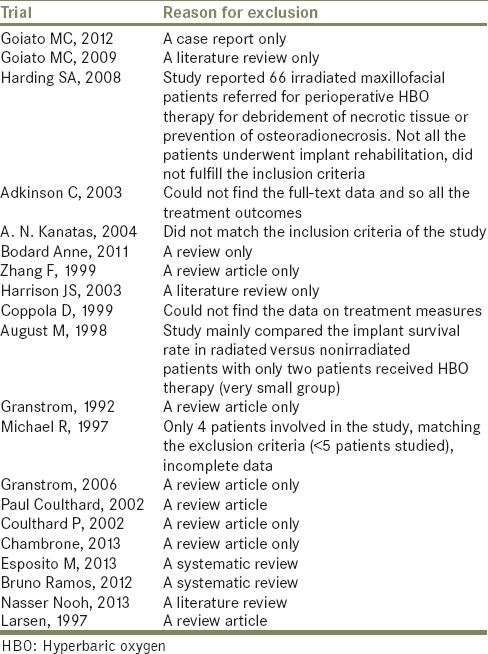
Table 5 shows the characteristics of the excluded studies.
Table 5.
Characteristics of excluded studies
Risk of bias assessment
Table 1 shows the assessment of the risk of bias of the included studies.
Graph 1 shows the assessment of the risk of bias of the included studies.
Effects of intervention and statistical analysis
Effect of intervention was studied for all 14 selected studies, and the implant survival rate for each group was statistically calculated [Tables 2 and 4].
Results of the study
Experimental studies
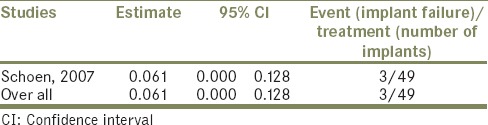
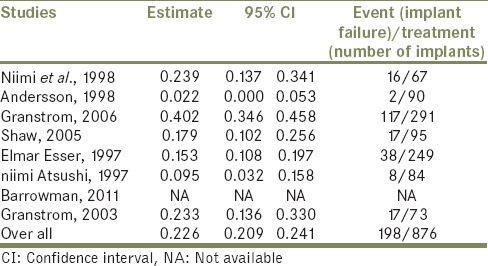
Table 6 shows estimated values for implant failures in HBO(+) group for an experimental study when the P value is set at P < 0.05, with the confidence interval (CI) of 95%.
Table 6.
Estimated values for implant failures in hyperbaric oxygen(+) group for an experimental study when the P value is set at P<0.05, with the confidence interval of 95%
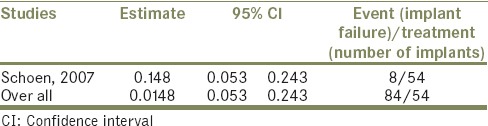
Table 7 shows estimated values for implant failures in non-HBO(+) group for an experimental study when the P value is set at P < 0.05, with the CI of 95%.
Table 7.
Estimated values for implant failures in nonhyperbaric oxygen(+) group for an experimental study when the P value is set at P<0.05, with the confidence interval of 95%
Forest Plot 1 shows implant failures in HBO and non-HBO group for experimental studies.
Forest Plot 1.
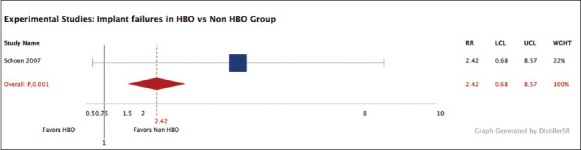
Experimental studies: Implant failures in hyperbaric oxygen versus nonhyperbaric oxygen group
Prospective studies
Table 8 shows estimated values for implant failures in HBO(−) group for three prospective studies when the same P value is set at P < 0.05, with the same CI of 95%.
Table 8.
Estimated values for implant failures in hyperbaric oxygen(−) group for prospective studies when the same P value is set at P<0.05, with the same confidence interval of 95%
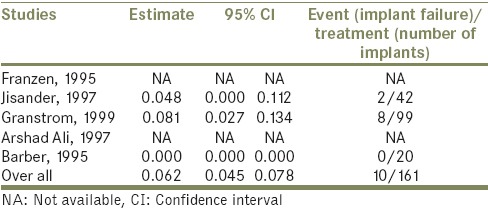
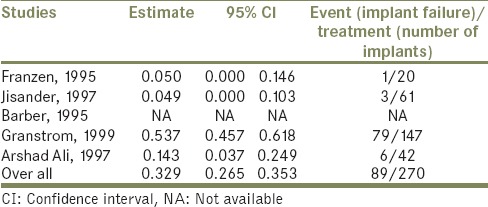
Table 9 shows estimated values for implant failures in non-HBO(−) group for 3 prospective studies when the P value is set at P < 0.05, with the same CI of 95%.
Table 9.
Estimated values for implant failures in nonhyperbaric oxygen(−) group for 3 prospective studies when the P value is set at P<0.05, with the same confidence interval of 95%
Forest Plot 2 shows implant failures in HBO and non-HBO group for prospective studies.
Forest Plot 2.

Prospective studies: Implant failures in hyperbaric oxygen versus nonhyperbaric oxygen group
Retrospective studies
Table 10 shows estimated values for implant failures in HBO(−) group for four retrospective studies when the same P value is set at P < 0.05, with the same CI of 95%.
Table 10.
Estimated values for implant failures in hyperbaric oxygen(−) group for 4 retrospective studies when the same P value is set at P<0.05, with the same confidence interval of 95%
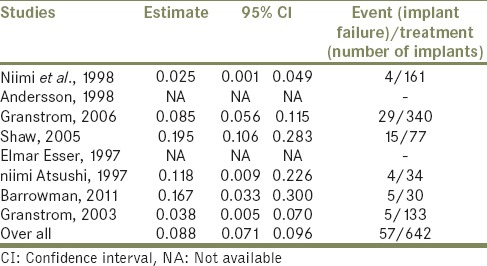
Table 11 shows estimated values for implant failures in non-HBO(−) group for seven retrospective studies when the same P value is set at P < 0.05, with the same CI of 95%.
Table 11.
Estimated values for implant failures in nonhyperbaric oxygen(−) group for 7 retrospective studies when the same P value is set at P<0.05, with the same confidence interval of 95%
Forest Plot 3 shows implant failures in HBO and non-HBO group for retrospective studies.
Forest Plot 3.
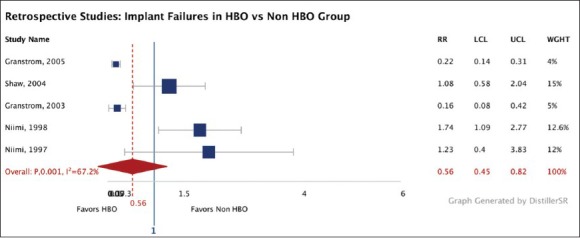
Retrospective studies: Implant failures in hyperbaric oxygen versus nonhyperbaric oxygen group
Table 12 represents “Pearson's Chi-square test” which shows the total number of implants placed, failed, and survived in both the groups, with P < 0.001, which shows that significant difference exists between both the group regarding the number of implants failed and survived.
Table 12.
Represents “Pearson's Chi-square test” which shows the total number of implants placed, failed, and survived in both the groups, with P<0.001, which shows that significant difference exists between both the groups regarding the number of implants failed and survived
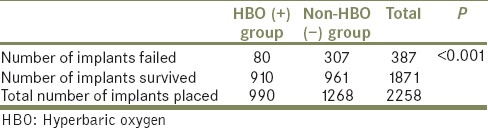
Graph 2 shows the significant difference regarding the implant failure rate in both the groups:
Graph 2.
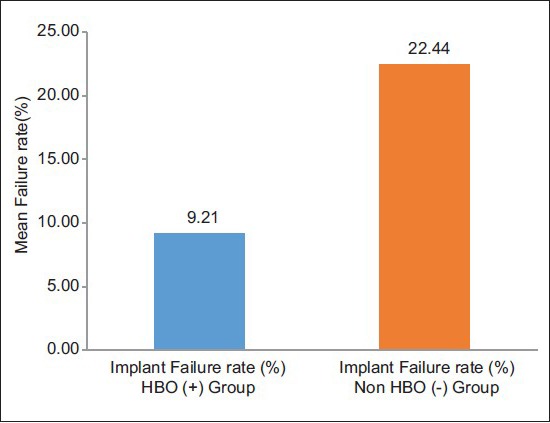
The significant difference regarding the implant failure rate in both the groups
Implant failure rate (%) in HBO(+) group: 9.21%
Implant failure rate (%) in non-HBO(−) group: 22.44%
SUMMARY
The present systematic review was undertaken to compare the implant failure rates for patients being irradiated in the head and neck region and receiving HBO therapy versus non-HBO therapy. There are many scientific papers[27] written about this subject including a number of review articles, but only one RCT (Schoen et al. 2007) including a limited number of participants was found for this review.
CONCLUSION
According to above statistical analysis, results show that preventive HBO therapy can reduce the risk of implant failures in irradiated patients, may be due to improved vascularity which leads to reduced risk of radiation-induced damages to tissue, and thus, HBO can be the effective treatment protocol, while planning for the implant treatment in irradiated maxillofacial patients. Still, some important factors, other than irradiation, that affect the implant survival rate in irradiated bone were type of implant, surgical procedures used, time interval between radiotherapy and implant placement, and radiation dose, which were not included in the meta-analysis, due to insufficient data.
Hence, further research work has to be done to specify above-mentioned various reasons of failures and various factors affecting the success and failure rates of dental implants in irradiated maxillofacial patients.
There is a definite need for more RCTs to ascertain the effectiveness of HBO in irradiated maxillofacial dental implant patients. These trials ought to be of a high quality and reported as recommended by the consort statement (www.consort-statement.org/). Each clinical center may have limited numbers of patients and it is likely that multicentered trials will be needed. Only with that clinicians will receive the evidence they need for their study and make the best treatment decisions possible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Urken ML, Weinberg H, Buchbinder D, Moscoso JF, Lawson W, Catalano PJ, et al. Microvascular free flaps in head and neck reconstruction. Report of 200 cases and review of complications. Arch Otolaryngol Head Neck Surg. 1994;120:633–40. doi: 10.1001/archotol.1994.01880300047007. [DOI] [PubMed] [Google Scholar]
- 2.Boyd JB, Rosen I, Rotstein L, Freeman J, Gullane P, Manktelow R, et al. The iliac crest and the radial forearm flap in vascularized oromandibular reconstruction. Am J Surg. 1990;159:301–8. doi: 10.1016/s0002-9610(05)81223-1. [DOI] [PubMed] [Google Scholar]
- 3.Chrcanovic BR, Albrektsson T, Wennerberg A. Dental implants in irradiated versus non-irradiated patients: A meta-analysis. Head Neck. 2016;38:448–81. doi: 10.1002/hed.23875. [DOI] [PubMed] [Google Scholar]
- 4.Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399–410. doi: 10.1016/s0022-3913(83)80101-2. [DOI] [PubMed] [Google Scholar]
- 5.Granström G. Osseointegration in irradiated cancer patients: An analysis with respect to implant failures. J Oral Maxillofac Surg. 2005;63:579–85. doi: 10.1016/j.joms.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Nooh N. Dental implant survival in irradiated oral cancer patients: A systematic review of the literature. Int J Oral Maxillofac Implants. 2013;28:1233–42. doi: 10.11607/jomi.3045. [DOI] [PubMed] [Google Scholar]
- 7.Johnson RP, Marx RE, Buckley SB. Hyperbaric oxygen in oral and maxillofacial surgery. In: Worthington P, Evans JR, editors. Controversies in Oral and Maxillofacial Surgery. London: WB Saunders Co., Harcourt Brace and Co; 1994. pp. 107–26. [Google Scholar]
- 8.Marx RE, Johnson RP, Kline SN. Prevention of osteoradionecrosis: A randomized prospective clinical trial of hyperbaric oxygen versus penicillin. J Am Dent Assoc. 1985;111:49–54. doi: 10.14219/jada.archive.1985.0074. [DOI] [PubMed] [Google Scholar]
- 9.Granström G, Jacobsson M, Tjellström A. Titanium implants in irradiated tissue: Benefits from hyperbaric oxygen. Int J Oral Maxillofac Implants. 1992;7:15–25. [PubMed] [Google Scholar]
- 10.Sahni T, Hukku S, Jain M, Prasad A, Prasad R, Singh K. Recent advances in hyperbaric oxygen therapy. Med Update. 2004;14:632–9. [Google Scholar]
- 11.Marx RE, Ames JR. The use of hyperbaric oxygen therapy in bony reconstruction of the irradiated and tissue-deficient patient. J Oral Maxillofac Surg. 1982;40:412–20. doi: 10.1016/0278-2391(82)90076-3. [DOI] [PubMed] [Google Scholar]
- 12.Johnsson ÅA. On implant integration in irradiated bone. An experimental study of the effects of hyperbaric oxygenation and delayed implant placement. Sweden: Thesis, University of Gothenburg; 1999. [Google Scholar]
- 13.Franzén L, Rosenquist JB, Rosenquist KI, Gustafsson I. Oral implant rehabilitation of patients with oral malignancies treated with radiotherapy and surgery without adjunctive hyperbaric oxygen. Int J Oral Maxillofac Implants. 1995;10:183–7. [PubMed] [Google Scholar]
- 14.Barber HD, Seckinger RJ, Hayden RE, Weinstein GS. Evaluation of osseointegration of endosseous implants in radiated, vascularized fibula flaps to the mandible: A pilot study. J Oral Maxillofac Surg. 1995;53:640–4. doi: 10.1016/0278-2391(95)90158-2. [DOI] [PubMed] [Google Scholar]
- 15.Esser E, Wagner W. Dental implants following radical oral cancer surgery and adjuvant radiotherapy. Int J Oral Maxillofac Implants. 1997;12:552–7. [PubMed] [Google Scholar]
- 16.Ali A, Patton DW, el-Sharkawi AM, Davies J. Implant rehabilitation of irradiated jaws: A preliminary report. Int J Oral Maxillofac Implants. 1997;12:523–6. [PubMed] [Google Scholar]
- 17.Niimi A, Fujimoto T, Nosaka Y, Ueda M. A Japanese multicenter study of osseointegrated implants placed in irradiated tissues: A preliminary report. Int J Oral Maxillofac Implants. 1997;12:259–64. [PubMed] [Google Scholar]
- 18.Jisander S, Grenthe B, Alberius P. Dental implant survival in the irradiated jaw: A preliminary report. Int J Oral Maxillofac Implants. 1997;12:643–8. [PubMed] [Google Scholar]
- 19.Niimi A, Ueda M, Keller EE, Worthington P. Experience with osseointegrated implants placed in irradiated tissues in Japan and the United States. Int J Oral Maxillofac Implants. 1998;13:407–11. [PubMed] [Google Scholar]
- 20.Andersson G, Andreasson L, Bjelkengren G. Oral implant rehabilitation in irradiated patients without adjunctive hyperbaric oxygen. Int J Oral Maxillofac Implants. 1998;13:647–54. [PubMed] [Google Scholar]
- 21.Granström G, Tjellström A, Brånemark PI. Osseointegrated implants in irradiated bone: A case-controlled study using adjunctive hyperbaric oxygen therapy. J Oral Maxillofac Surg. 1999;57:493–9. doi: 10.1016/s0278-2391(99)90059-9. [DOI] [PubMed] [Google Scholar]
- 22.Granström G. Radiotherapy, osseointegration and hyperbaric oxygen therapy. Periodontol. 2000;2003;33:145–62. doi: 10.1046/j.0906-6713.2002.03312.x. [DOI] [PubMed] [Google Scholar]
- 23.Shaw RJ, Sutton AF, Cawood JI, Howell RA, Lowe D, Brown JS, et al. Oral rehabilitation after treatment for head and neck malignancy. Head Neck. 2005;27:459–70. doi: 10.1002/hed.20176. [DOI] [PubMed] [Google Scholar]
- 24.Granström G. Placement of dental implants in irradiated bone: The case for using hyperbaric oxygen. J Oral Maxillofac Surg. 2006;64:812–8. doi: 10.1016/j.joms.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 25.Schoen PJ, Raghoebar GM, Bouma J, Reintsema H, Vissink A, Sterk W, et al. Rehabilitation of oral function in head and neck cancer patients after radiotherapy with implant-retained dentures: Effects of hyperbaric oxygen therapy. Oral Oncol. 2007;43:379–88. doi: 10.1016/j.oraloncology.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Barrowman RA, Wilson PR, Wiesenfeld D. Oral rehabilitation with dental implants after cancer treatment. Aust Dent J. 2011;56:160–5. doi: 10.1111/j.1834-7819.2011.01318.x. [DOI] [PubMed] [Google Scholar]
- 27.Coulthard P, Esposito M, Worthington HV, Jokstad A. Therapeutic use of hyperbaric oxygen for irradiated dental implant patients: A systematic review. J Dent Educ. 2003;67:64–8. [PubMed] [Google Scholar]


