Abstract
Rationale: Lung volume reduction surgery (LVRS) is associated with weight gain in some patients, but the group that gains weight after LVRS and the mechanisms underlying this phenomenon have not been well characterized.
Objectives: To describe the weight change profiles of LVRS patients enrolled in the National Emphysema Treatment Trial (NETT) and to correlate alterations in lung physiological parameters with changes in weight.
Methods: We divided 1,077 non–high-risk patients in the NETT into groups according to baseline body mass index (BMI): underweight (<21 kg/m2), normal weight (21–25 kg/m2), overweight (25–30 kg/m2), and obese (>30 kg/m2). We compared BMI groups and LVRS and medical groups within each BMI stratum with respect to baseline characteristics and percent change in BMI (%ΔBMI) from baseline. We examined patients with (ΔBMI ≥ 5%) and without (ΔBMI < 5%) significant weight gain at 6 months and assessed changes in lung function and ventilatory efficiency (V̇e/V̇co2).
Measurements and Main Results: The percent change in BMI was greater in the LVRS arm than in the medical arm in the underweight and normal weight groups at all follow-up time points, and at 12 and 24 months in the overweight group. In the LVRS group, patients with ΔBMI ≥ 5% at 6 months had greater improvements in FEV1 (11.53 ± 9.31 vs. 6.58 ± 8.68%; P < 0.0001), FVC (17.51 ± 15.20 vs. 7.55 ± 14.88%; P < 0.0001), residual volume (–66.20 ± 40.26 vs. –47.06 ± 39.87%; P < 0.0001), 6-minute walk distance (38.70 ± 69.57 vs. 7.57 ± 73.37 m; P < 0.0001), maximal expiratory pressures (12.73 ± 49.08 vs. 3.54 ± 32.22; P = 0.0205), and V̇e/V̇co2 (–1.58 ± 6.20 vs. 0.22 ± 8.20; P = 0.0306) at 6 months than patients with ΔBMI < 5% at 6 months.
Conclusions: LVRS leads to weight gain in nonobese patients, which is associated with improvement in lung function, exercise capacity, respiratory muscle strength, and ventilatory efficiency. These physiological changes may be partially responsible for weight gain in patients who undergo LVRS.
Keywords: pulmonary disease, chronic obstructive; lung volume reduction surgery; ventilatory efficiency; cachexia
At a Glance Commentary
Scientific Knowledge on the Subject
Lung volume reduction surgery results in greater exercise capacity, improved lung function, and a reduction in mortality in selected patients with advanced emphysema compared with medical therapy. The impact of lung volume reduction surgery on body mass index has not been well described.
What This Study Adds to the Field
This study shows that underweight patients who underwent lung volume reduction surgery experienced significant improvements in body mass index, and that weight gain after lung volume reduction surgery was related to improved lung function and ventilatory efficiency. These physiological changes may be partially responsible for weight gain in patients who undergo lung volume reduction surgery.
Chronic obstructive pulmonary disease (COPD) is an inflammatory lung disease with many associated comorbid disorders, including coronary heart disease, osteoporosis, metabolic syndrome, and low body mass index (BMI) (1, 2). The abnormal local inflammatory response to cigarette smoke leads to airflow obstruction and also results in systemic inflammation, characterized by increased levels of IL-6, IL-8, tumor necrosis factor (TNF)-α, and C-reactive protein (3); this systemic inflammation is believed to be responsible for accelerated bone loss, premature development of atherosclerotic heart disease, and skeletal muscle apoptosis (1, 2). A low BMI is also a result of several other factors, including breathlessness while eating, difficulty preparing meals because of breathlessness, derangement of glycolipemic hormone metabolism, higher resting energy expenditure from increased work of breathing, physical deconditioning, and respiratory cachexia (4–6).
Low BMI has been shown to be a risk factor for mortality in COPD, both independently as well as a part of a multidimensional index (7–9). Lung volume reduction surgery (LVRS) has been shown to decrease mortality in select patients with advanced emphysema (10) and may improve systemic inflammation and nutritional status (6, 11). In whom LVRS will cause weight gain and the mechanisms responsible are currently not well characterized.
We sought to describe the weight change profiles of LVRS patients enrolled in the National Emphysema Treatment Trial (NETT). We also correlated alterations in lung physiological parameters with changes in weight. We hypothesized that patients who were more underweight would gain more weight after LVRS, and that weight gain would be associated with improvements in lung function and ventilatory efficiency. Some of these data were reported in an abstract at the 2009 American Thoracic Society International Conference (12).
Methods
Patient Selection
Enrollment criteria for NETT have been previously described (10). All patients provided written informed consent, and the study was approved by the institutional review board at each center. Inclusion criteria included a physical examination consistent with emphysema, radiographic evidence of bilateral emphysema on high-resolution computed tomography (HRCT) scan, FEV1 not exceeding 45% predicted, but at least 15% of predicted if age 70 years or older, total lung capacity (TLC) equal to or greater than 100% predicted, RV equal to or greater than 150% predicted, Pco2 not greater than 60 mm Hg, Po2 equal to or greater than 45 mm Hg on room air, and a postrehabilitation 6-minute walk distance greater than 140 m. Patients also needed to be stable on not more than 20 mg of prednisone per day, nonsmoking for 4 months, and have a BMI not greater than 31.1 kg/m2 in men and not greater than 32.3 kg/m2 in women. All patients underwent 6–10 weeks of pulmonary rehabilitation, and then were randomized to either LVRS or continued medical therapy per American Thoracic Society guidelines. Baseline measurements of pulmonary function, 6-minute walk distance, and health-related quality of life obtained from the St. George’s Respiratory Questionnaire (SGRQ) were obtained after completing pulmonary rehabilitation but before randomization, and again at 6, 12, 24, and 36 months.
Patients considered at high risk for LVRS (13) were excluded, and one additional patient without BMI data at baseline was excluded. We divided the remaining 1,077 non–high-risk patients into four groups based on baseline BMI (after pulmonary rehabilitation and before randomization to either LVRS or medical therapy): underweight (<21 kg/m2), normal weight (21–25 kg/m2), overweight (25–30 kg/m2), and obese (>30 kg/m2). We compared the BMI groups with respect to baseline characteristics. We also stratified on BMI group and compared the LVRS and medical groups with respect to baseline characteristics and percent change in BMI (%ΔBMI) from baseline to follow-up at 6, 12, 24, and 36 months.
Stratifying by treatment arm, those with significant weight gain from baseline to 6 months (an increase in BMI ≥ 5%, ΔBMI ≥ 5%) were compared with those without significant weight gain (no change, a decrease, or an increase in BMI < 5%, ΔBMI < 5%) with respect to changes from baseline to 6 months in lung function, SGRQ score, ventilatory efficiency, and 6-minute walk distance. ΔBMI equal to or greater than 5% was chosen as significant because of existing data suggesting that a change in BMI of 5% is clinically significant (14, 15). Ventilatory efficiency was defined as the ratio of minute ventilation (V̇e) to carbon dioxide production (V̇co2) (16) during unloaded pedaling (chosen as an iso-study time point) during incremental cardiopulmonary exercise testing. Change in diffusing capacity of carbon monoxide (DlCO) was assessed at 12 months because this lung function parameter was not assessed at 6 months.
Statistical Analysis
Statistics were performed with JMP 8.0 (SAS, Cary, NC) or SAS 9.2 (SAS). Descriptive statistics are reported as means ± SD, except where otherwise noted. A P value less than 0.05 was considered statistically significant. An unpaired t test was used to compare baseline demographic and pulmonary function data between BMI groups and between LVRS and medical patients. In each BMI group, LVRS and medical patients were compared on %ΔBMI from baseline to each follow-up time point, using unpaired t tests. Within each treatment group, changes in lung function, ventilatory efficiency, 6-minute walk distance, and SGRQ scores were compared between those with ΔBMI equal to or greater than 5% and those with ΔBMI less than 5%, using unpaired t tests. Multivariate logistic regression was performed to assess the independent effects of treatment arm (LVRS vs. medical therapy), sex, and baseline exercise category (low vs. high exercise), BMI group, lung function, and V̇e/V̇co2 on ΔBMI equal to or greater than 5% at 6 months.
Results
There were 182, 391, 391, and 113 patients in the underweight, normal weight, overweight, and obese BMI groups, respectively (total n = 1,077). Baseline data are listed in Table 1. Racial distribution was not different between BMI groups. The underweight group was composed of fewer males compared with the normal weight and overweight groups (45 vs. 62, 65%, respectively; both P < 0.05). The underweight group had lower percent predicted FEV1 compared with the other three BMI groups (27 ± 7 vs. 28 ± 6, 28 ± 7, and 30 ± 7% predicted in the normal weight, overweight, and obese groups, respectively; all P < 0.05) as well as a lower percent predicted FVC (67 ± 16 vs. 70 ± 15, 69 ± 15, 70 ± 14% predicted, respectively; all P < 0.05), a higher percent predicted TLC (131 ± 15 vs. 127 ± 14, 127 ± 15, 125 ± 14% predicted, respectively; all P < 0.05), a higher percent predicted RV (226 ± 46 vs. 215 ± 43, 215 ± 47, 207 ± 41% predicted, respectively; all P < 0.05), and a lower percent predicted DlCO (26 ± 8 vs. 28 ± 9, 31 ± 9, 33 ± 10% predicted, respectively; all P < 0.05). The underweight group also had higher SGRQ scores compared with the other BMI groups (55 ± 12 vs. 51 ± 13, 52 ± 13, 54 ± 13, respectively; all P < 0.05), higher V̇e/V̇co2 during unloaded pedaling (46.0 ± 12.8 vs. 43.5 ± 10.9, 41.4 ± 8.5, 38.8 ± 8.1, respectively; all P < 0.05), and a greater percentage of patients categorized as low exercise capacity (≤40 W for men and ≤25 W for women on incremental cardiopulmonary exercise testing; 61.0 vs. 39.9, 34.8, 31.9%; all P < 0.05). All groups had comparable percentages of patients with upper lobe–predominant emphysema on CT scan. Overall, the underweight group had a higher percentage of the upper lobe–predominant emphysema/low-exercise capacity subgroup, as defined by NETT (10) (39.6 vs. 26.6, 22.8, 22.1%, respectively; all P < 0.05).
TABLE 1.
BASELINE CHARACTERISTICS OF PATIENTS IN EACH BODY MASS INDEX STRATUM
| Underweight (BMI < 21) |
Normal Weight (BMI 21–25) |
Overweight (BMI 25–30) |
Obese (BMI > 30) |
|||||||||
| All (n = 182) | LVRS (n = 97) | MED (n = 85) | All (n = 391) | LVRS (n = 207) | MED (n = 184) | All (n = 391) | LVRS (n = 176) | MED (n = 215) | All (n = 113) | LVRS (n = 158) | MED (n = 55) | |
| Age, yr | 68 ± 6* | 68 ± 6 | 68 ± 5 | 68 ± 6*† | 67 ± 7 | 67 ± 6 | 67 ± 6 | 67 ± 7 | 67 ± 7 | 66 ± 6 | 66 ± 6 | 66 ± 6 |
| Sex, % male | 45†‡ | 38 | 52 | 62 | 60 | 64 | 65 | 64 | 66 | 57 | 50 | 64 |
| Race, % white | 93 | 93 | 94 | 94 | 96 | 92 | 96 | 96 | 96 | 96 | 97 | 96 |
| FVC, %pred | 67 ± 16*†‡ | 66 ± 16 | 68 ± 16 | 70 ± 15 | 70 ± 14 | 70 ± 15 | 69 ± 15 | 69 ± 16 | 69 ± 14 | 70 ± 14 | 70 ± 14 | 71 ± 14 |
| FEV1, %pred | 27 ± 7* | 27 ± 7 | 27 ± 6 | 28 ± 6* | 28 ± 6 | 28 ± 7 | 28 ± 7* | 28 ± 7 | 28 ± 6 | 30 ± 7 | 30 ± 7 | 30 ± 7 |
| TLC, %pred | 131 ± 15*†‡ | 131 ± 16 | 131 ± 14 | 127 ± 14 | 128 ± 15 | 127 ± 13 | 127 ± 15 | 126 ± 14 | 128 ± 15 | 125 ± 14 | 125 ± 15 | 124 ± 13 |
| RV, %pred | 226 ± 46*†‡ | 226 ± 43 | 227 ± 48 | 215 ± 43 | 214 ± 45 | 216 ± 40 | 215 ± 47 | 212 ± 47 | 217 ± 47 | 207 ± 41 | 207 ± 45 | 206 ± 37 |
| PaO2, mm Hg | 64 ± 11‡ | 64 ± 11 | 64 ± 10 | 66 ± 11 | 67 ± 11 | 66 ± 10 | 64 ± 10‡ | 64 ± 10 | 64 ± 10 | 62 ± 9‡ | 61 ± 8 | 64 ± 10 |
| PaCO2, mm Hg | 43 ± 6‡ | 43 ± 6 | 43 ± 6 | 42 ± 5 | 42 ± 5 | 42 ± 5 | 43 ± 6‡ | 43 ± 6 | 43 ± 6 | 44 ± 5‡ | 44 ± 5 | 44 ± 5 |
| DlCO, %pred | 26 ± 8*†‡ | 26 ± 9 | 25 ± 8 | 28 ± 9*† | 29 ± 9 | 28 ± 8 | 31 ± 9* | 30 ± 9 | 31 ± 10 | 33 ± 10 | 32 ± 10 | 35 ± 10 |
| 6MWD, m | 366 ± 87†‡ | 374 ± 88 | 357 ± 85 | 385 ± 96*†§ | 383 ± 97 | 387 ± 95 | 379 ± 93 | 376 ± 92 | 382 ± 94 | 353 ± 96 | 347 ± 88 | 358 ± 104 |
| V̇e/V̇co2 | 46.0 ± 12.8*†‡ | 47.5 ± 13.3 | 44.2 ± 12.0 | 43.5 ± 10.9*† | 43.1 ± 12.0 | 44.0 ± 9.6 | 41.4 ± 8.5* | 40.9 ± 8.1 | 41.9 ± 8.7 | 38.8 ± 8.1 | 37.1 ± 8.3‖ | 40.5 ± 7.7 |
| SGRQ | 55 ± 12†‡ | 55 ± 12 | 56 ± 12 | 51 ± 13 | 50 ± 13 | 53 ± 13 | 52 ± 13 | 53 ± 13 | 52 ± 12 | 54 ± 13 | 52 ± 11 | 55 ± 14 |
| UL, % | 61.5 | 60.8 | 62.4 | 65.0 | 65.7 | 64.1 | 67.8 | 63.6 | 71.2 | 69.0 | 65.5 | 72.7 |
| Low Ex, % | 61.0*†‡ | 66.0 | 55.3 | 39.9 | 41.6 | 38.0 | 34.8 | 30.7 | 38.1 | 31.9 | 32.8 | 30.9 |
| ULLE, % | 39.6*†‡ | 43.3 | 35.3 | 26.6 | 26.1 | 27.2 | 22.8 | 17.6 | 27.0‖ | 22.1 | 20.7 | 23.6 |
| BMI, kg/m2 | 19.4 ± 1.2*†‡ | 19.4 ± 1.3 | 19.3 ± 1.2 | 23.2 ± 1.1*† | 23.2 ± 1.2 | 23.2 ± 1.1 | 27.2 ± 1.4* | 27.2 ± 1.4 | 27.0 ± 1.4 | 30.9 ± 0.7 | 31.1 ± 0.8 | 30.8 ± 0.6 |
Definition of abbreviations: %pred = percentage of predicted value; 6MWD = 6-minute walk distance; BMI = body mass index; DlCO = diffusing capacity of carbon monoxide; Low Ex = low-exercise group (≤40 W on cardiopulmonary exercise test for males, ≤25 W for females); LVRS = lung volume reduction surgery; MED = medical treatment arm; RV = residual volume; SGRQ = St. George’s Respiratory Questionnaire; TLC = total lung capacity; UL = upper lobe–predominant emphysema; ULLE = upper lobe–predominant emphysema and low-exercise subgroup; V̇e/V̇co2 = ventilatory efficiency.
P < 0.05 compared with obese.
P < 0.05 compared with overweight.
P < 0.05 compared with normal weight.
P < 0.05 compared with underweight.
P < 0.05 LVRS versus MED within BMI stratum.
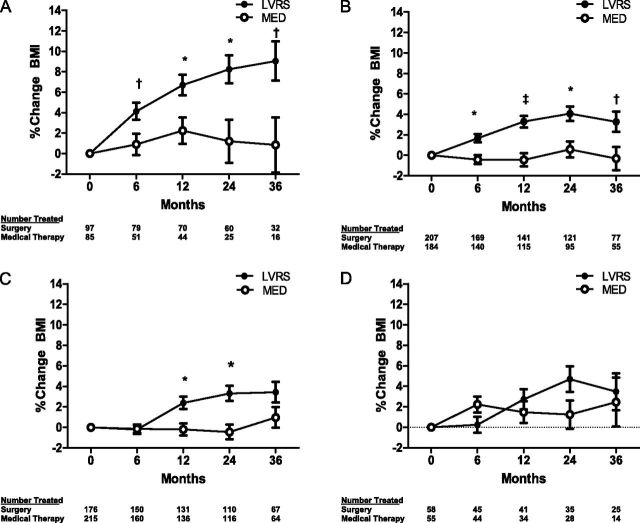
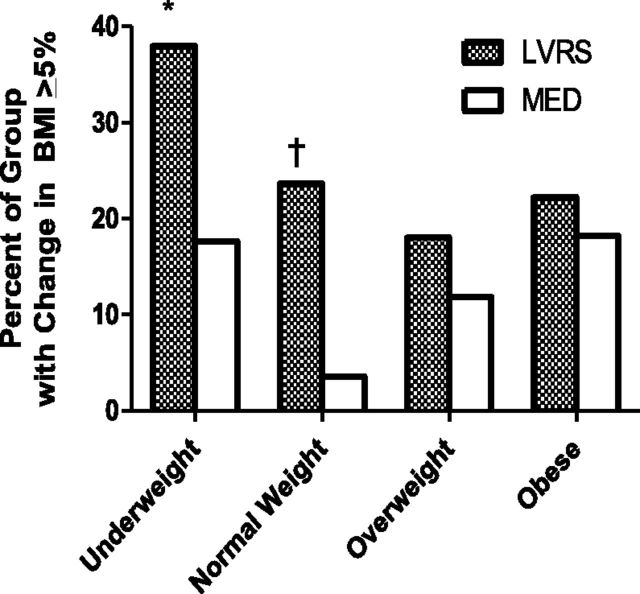
Changes in BMI in each BMI group are listed in Table 2 and displayed in Figure 1. BMI remained relatively stable in all weight groups in medically treated patients. %ΔBMI was significantly higher in the LVRS arm compared with the medical arm in the underweight and normal weight groups at all follow-up time points. In the overweight group, %ΔBMI was significantly higher in the LVRS arm at 12 and 24 months compared with the medical arm. There were no significant differences between LVRS and medical arms in the obese group. The differences in %ΔBMI between LVRS and medical arms were greatest in the underweight group compared with other BMI groups, and the mean BMI change from baseline progressively increased in the underweight group at 12, 24, and 36 months. The underweight and normal weight groups had a significantly higher percentage of patients in the LVRS arm who had a significant increase in BMI (ΔBMI ≥ 5%) at 6 months compared with the medical arm (see Figure 2).
TABLE 2.
PERCENT CHANGE IN BODY MASS INDEX (BMI) OVER TIME WITHIN BASELINE BMI GROUP
| Underweight (BMI < 21) |
Normal Weight (BMI 21–25) |
Overweight (BMI 25–30) |
Obese (BMI > 30) |
|||||||||
| LVRS (n = 97) | MED (n = 85) | P Value | LVRS (n = 207) | MED (n = 184) | P Value | LVRS (n = 176) | MED (n = 215) | P Value | LVRS (n = 58) | MED (n = 55) | P Value | |
| 6 mo | 4.13 ± 8.65 | 0.89 ± 4.82 | 0.0164 | 1.67 ± 6.02 | −0.42 ± 3.79 | 0.0004 | −0.20 ± 6.34 | −0.14 ± 4.38 | 0.9276 | 0.25 ± 6.30 | 2.23 ± 3.62 | 0.0735 |
| (n = 79) | (n = 51) | (n = 169) | (n = 140) | (n = 150) | (n = 160) | (n = 45) | (n = 44) | |||||
| 12 mo | 6.70 ± 9.76 | 2.25 ± 6.02 | 0.0077 | 3.30 ± 7.69 | −0.45 ± 5.61 | <0.0001 | 2.37 ± 8.07 | −0.19 ± 5.77 | 0.0029 | 2.72 ± 6.87 | 1.47 ± 5.49 | 0.3915 |
| (n = 70) | (n = 44) | (n = 141) | (n = 115) | (n = 131) | (n = 136) | (n = 41) | (n = 34) | |||||
| 24 mo | 8.25 ± 11.62 | 1.21 ± 7.60 | 0.0066 | 4.07 ± 7.84 | 0.58 ± 7.59 | 0.0012 | 3.32 ± 8.52 | −0.45 ± 6.89 | 0.0003 | 4.69 ± 8.08 | 1.25 ± 6.33 | 0.0695 |
| (n = 60) | (n = 25) | (n = 121) | (n = 95) | (n = 110) | (n = 116) | (n = 35) | (n = 28) | |||||
| 36 mo | 9.05 ± 12.14 | 0.85 ± 7.64 | 0.0117 | 3.28 ± 8.67 | -0.32 ± 8.44 | 0.0188 | 3.43 ± 9.10 | 0.97 ± 6.95 | 0.0859 | 3.48 ± 9.65 | 2.46 ± 7.44 | 0.7352 |
| (n = 32) | (n = 16) | (n = 77) | (n = 55) | (n = 67) | (n = 64) | (n = 25) | (n = 14) | |||||
| % of each group with ΔBMI ≥ 5% at 6 mo | 37.97 | 17.65 | 0.0182 | 23.67 | 3.57 | <0.0001 | 18.00 | 11.88 | 0.1510 | 22.22 | 18.18 | 0.7928 |
Definition of abbreviations: BMI = body mass index; LVRS = lung volume reduction surgery; MED = medical treatment arm.
All data are expressed as means ± SD, except percentage of each group with ΔBMI equal to or greater than 5% at 6 months. P values are for differences between LVRS and MED within the BMI group.
Bold indicates P values less than 0.05, the level of statistical significance.
Figure 1.
Percent change in body mass index by treatment group and body mass index (BMI) group: (A) underweight, (B) normal weight, (C) overweight, and (D) obese. Solid circles represent patients in the lung volume reduction surgery (LVRS) group, and open circles represent patients in the medical therapy (MED) group. Data present means ± SE. *P < 0.01, †P < 0.05, ‡P < 0.0001 for LVRS versus MED.
Figure 2.
Percentage of each body mass index (BMI) group with an increase in BMI of at least 5% at 6 months after randomization to lung volume reduction surgery (LVRS) or medical therapy (MED). *P < 0.05, †P < 0.0001 for LVRS versus MED.
Table 3 and Figure 3 summarize the changes in physiological parameters, gas exchange, walk distance, health-related quality of life, and ventilator efficiency in patients who had a significant increase in BMI (ΔBMI ≥ 5%) and those who did not (ΔBMI < 5%) at 6 months, stratified by treatment. Overall, 24.7% of the LVRS group had a ΔBMI of at least 5%, whereas only 10.3% of the MED group had a ΔBMI of at least 5%. Compared with the LVRS ΔBMI < 5% group, the LVRS ΔBMI ≥ 5% group had greater improvements in percent predicted FEV1 (11.53 ± 9.31 vs. 6.58 ± 8.68%; P < 0.0001), FVC (17.51 ± 15.20 vs. 7.55 ± 14.88%; P < 0.0001), and RV (–66.20 ± 40.26 vs. –47.06 ± 39.87%; P < 0.0001). Similarly, the LVRS ΔBMI ≥ 5% group compared with the LVRS ΔBMI < 5% group had greater improvements in 6-minute walk distance (38.70 ± 69.57 vs. 7.57 ± 73.37 m; P < 0.0001), PaCO2 (–2.80 ± 5.02 vs. –1.70 ± 4.66 mm Hg; P = 0.0300), PaO2 (7.48 ± 9.18 vs. 3.73 ± 9.41 mm Hg; P < 0.0002), and SGRQ scores (–15.30 ± 14.08 vs. –9.15 ± 14.44; P < 0.0001). Changes in maximal expiratory pressures (12.73 ± 49.08 vs. 3.54 ± 32.22; P = 0.0205) were greater in the LVRS ΔBMI ≥ 5% group compared with the LVRS ΔBMI < 5% group. V̇e/V̇co2 decreased at 6 months in the LVRS ΔBMI ≥ 5% group, whereas in the LVRS ΔBMI < 5% group the V̇e/V̇co2 increased (–1.58 ± 6.20 vs. 0.22 ± 8.20; P = 0.0306). There were no significant differences in changes from baseline in the aforementioned parameters in the MED ΔBMI ≥ 5% group compared with the MED ΔBMI < 5% group, with the exception of 6-minute walk distance, which decreased more in the MED ΔBMI ≥ 5% group and in the MED ΔBMI < 5% group (–46.98 ± 8.18 vs. –21.34 ± 2.78; P = 0.0032).
TABLE 3.
CHANGES IN LUNG FUNCTION, RESPIRATORY MUSCLE STRENGTH, 6-MINUTE WALK DISTANCE, RESTING GAS EXCHANGE, HEALTH-RELATED QUALITY OF LIFE, AND VENTILATORY EFFICIENCY STRATIFIED BY TREATMENT GROUP AND CHANGE IN BODY MASS INDEX AT 6 MONTHS IN 900 PATIENTS SURVIVING AT 6 MONTHS
| LVRS |
MED |
|||||
| Variable | ΔBMI ≥ 5% (n = 117) | ΔBMI < 5% (n = 357) | P Value | ΔBMI ≥ 5% (n = 44) | ΔBMI < 5% (n = 382) | P Value |
| FEV1, %pred | 11.53 ± 9.31 | 6.58 ± 8.68 | <0.0001 | −0.59 ± 4.63 | −0.38 ± 4.27 | 0.7622 |
| FVC, %pred | 17.51 ± 15.20 | 7.55 ± 14.88 | <0.0001 | −2.05 ± 9.21 | −1.44 ± 10.09 | 0.6091 |
| RV, %pred | −66.20 ± 40.26 | −47.06 ± 39.87 | <0.0001 | −4.82 ± 36.93 | 1.78 ± 29.63 | 0.1740 |
| TLC, %pred | −16.30 ± 11.84 | −14.46 ± 13.17 | 0.1797 | −2.11 ± 10.31 | −0.29 ± 10.23 | 0.2640 |
| DlCO, %pred | 4.10 ± 9.10 | 1.44 ± 8.34 | 0.0100 | −1.23 ± 5.80 | −2.01 ± 6.68 | 0.5108 |
| MIP, %pred | 25.20 ± 38.34 | 18.43 ± 33.93 | 0.0706 | 6.62 ± 23.48 | 0.80 ± 31.26 | 0.2326 |
| MEP, %pred | 12.73 ± 49.08 | 3.54 ± 32.22 | 0.0205 | 9.56 ± 37.41 | 0.87 ± 30.32 | 0.0834 |
| 6MWD, m | 38.70 ± 69.57 | 7.57 ± 73.37 | <0.0001 | −46.98 ± 8.18 | −21.34 ± 2.78 | 0.0032 |
| PaCO2, mm Hg | −2.80 ± 5.02 | −1.70 ± 4.66 | 0.0300 | 1.11 ± 3.21 | 0.65 ± 3.69 | 0.4245 |
| PaO2, mm Hg | 7.48 ± 9.18 | 3.73 ± 9.41 | 0.0002 | −1.68 ± 8.83 | 1.22 ± 6.98 | 0.6864 |
| SGRQ | −15.30 ± 14.08 | −9.15 ± 14.44 | <0.0001 | 2.83 ± 8.13 | 1.92 ± 10.49 | 0.5806 |
| V̇e/V̇co2 | −1.58 ± 6.20 | 0.22 ± 8.20 | 0.0306 | −1.73 ± 5.05 | 0.03 ± 8.02 | 0.1610 |
Definition of abbreviations: 6MWD = 6-minute walk distance; BMI = body mass index; DlCO = diffusing capacity of carbon monoxide; LVRS = lung volume reduction surgery; MED = medical treatment arm; MEP = maximal expiratory pressure; MIP = maximal inspiratory pressure; RV = residual volume; SGRQ = St. George’s Respiratory Questionnaire; TLC = total lung capacity; V̇e/V̇co2 = ventilatory efficiency.
All values are expressed as means ± SD. All data were reported at 6 months of follow-up, except for DlCO, which was determined at 12 months.
Bold indicates P values less than 0.05, the level of statistical significance.
Figure 3.
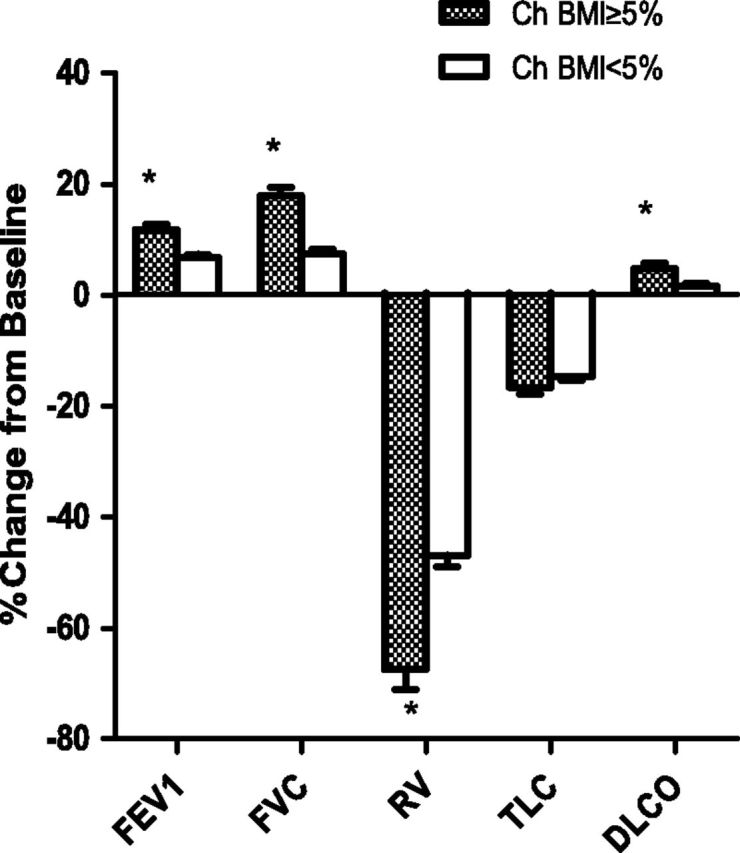
Change in body mass index (BMI) at 6 months and percent changes in lung function measures from baseline to 6 months (except the diffusing capacity of carbon monoxide [DlCO], which was assessed at 12 mo). Shaded columns represent patients who had an increase in BMI of at least 5% at 6 months, and open columns represent patients with a change in BMI less than 5%. Data represent the lung volume reduction surgery (LVRS) treatment group and are expressed as means ± SE. *P < 0.0001 for ΔBMI ≥ 5% versus ΔBMI < 5%.
In multivariate analysis using a binary logistic regression model of ΔBMI equal to or greater than 5% on treatment arm (LVRS vs. medical), sex, exercise category (low- vs. high-exercise capacity), upper lobe predominance (vs. other), baseline lung function, baseline V̇e/V̇co2, and BMI group, the LVRS arm (vs. MED) and the underweight group (vs. normal) were significantly associated with a ΔBMI equal to or greater than 5% (odds ratio [OR], 2.70; 95% confidence interval [CI], 1.81–4.04; and OR, 2.36; 95% CI, 1.39–4.01, respectively). Baseline FVC was inversely associated with ΔBMI equal to or greater than 5% (OR, 0.97; 95% CI, 0.95–0.99). Sex and baseline exercise category, FEV1, TLC, RV, and V̇e/V̇co2 were not significantly associated with ΔBMI equal to or greater than 5% (see Table 4).
TABLE 4.
ADJUSTED ODDS RATIOS IN MULTIVARIATE ANALYSIS FOR CHANGE IN BODY MASS INDEX OF AT LEAST 5% AT 6 MONTHS IN 837 NON–HIGH-RISK PATIENTS SURVIVING TO 6 MONTHS
| Variable | OR | 95% CI | P Value | P Value for Combination of Factors |
| LVRS vs. MED | 2.70 | 1.81, 4.04 | <0.0001 | |
| Female vs. male | 0.79 | 0.50, 1.25 | 0.2998 | |
| Low exercise vs. high exercise | 0.93 | 0.61, 1.41 | 0.7194 | |
| UL predominant vs. other | 1.48 | 0.98, 2.25 | 0.0651 | |
| Underweight vs. normal | 2.36 | 1.39, 4.01 | 0.0015 | 0.0057 |
| Overweight vs. normal | 1.02 | 0.64, 1.62 | 0.9301 | |
| Obese vs. normal | 1.52 | 0.80, 2.90 | 0.2015 | |
| Baseline FVC, % predicted | 0.97 | 0.95, 0.99 | 0.0019 | |
| Baseline FEV1, % predicted | 1.03 | 0.99, 1.07 | 0.2174 | |
| Baseline TLC, % predicted | 1.02 | 0.99, 1.05 | 0.1522 | |
| Baseline RV, % predicted | 1.00 | 0.99, 1.01 | 0.7202 | |
| Baseline V̇e/V̇co2 | 1.00 | 0.98, 1.01 | 0.6479 |
Definition of abbreviations: CI = confidence interval; LVRS = lung volume reduction surgery; MED = medical treatment arm; OR = odds ratio; RV = residual volume; TLC = total lung capacity; UL = upper lobe; V̇e/V̇co2 = ventilatory efficiency.
Bold indicates P values less than 0.05, the level of statistical significance.
Discussion
We showed in a large group of well-characterized patients with advanced emphysema that LVRS was more likely to be associated with significant weight gain, whereas medical therapy alone had little effect on weight. Using preoperative BMI, we were also able to identify patient groups more likely to gain weight, as well as their associated changes in lung function and ventilatory efficiency. Significant weight gain was accomplished in those who were not obese at baseline, and these effects were independent of preoperative exercise subgroup and distribution of emphysema on CT scan, which were primary predictors of outcome in the NETT. The changes in BMI were most profound in the underweight group, followed by the normal weight and overweight groups. In addition, the underweight group continued to gain weight through 36 months of follow-up, whereas the normal weight and overweight groups achieved a plateau of weight gain at 24 months. In the LVRS arm, those who experienced significant weight gain had greater improvements in spirometry, respiratory muscle strength, lung volumes, ventilatory efficiency, health-related quality of life, and 6-minute walk distance compared with those without a significant weight gain. Therefore, we posit that these changes in lung physiology exert a positive effect on BMI by improving exercise capacity, with a resultant increase in muscle mass and a reduction of resting energy expenditure (REE).
What defines a significant weight change is a matter of debate. In the elderly population, involuntary weight loss of 5% in 6 months is associated with increased mortality (14), and intentional weight loss of 5% in the obese population significantly reduces cardiovascular risk (15). However, in the underweight population, it is unclear how much weight gain is necessary to have a significant impact on outcome. A prospective study of an aggressive nutritional support program in 203 patients with COPD has shown that a weight gain of 2 kg over 8 weeks in nutritionally depleted patients was associated with improvement in long-term outcomes (7). In addition, a small study of 30 LVRS patients revealed that a 5% increase in BMI was associated with improved health-related quality of life, dyspnea scores, and lung function (17). On the basis of these data, we chose a threshold of a 5% increase in BMI in 6 months to be considered clinically significant for our analysis.
Cachexia is a common systemic manifestation of COPD, affecting 20–35% of patients (18, 19). The underlying mechanisms are unclear, but multiple factors have been implicated, including increased REE (4, 20), elevated systemic inflammation (5), derangement of anabolic hormone metabolism (21, 22), and muscle disuse atrophy. Sergi and colleagues found that REE was 10% higher in patients with COPD than in normal subjects similar in age, height, and weight (20). Similarly, Schols and colleagues found that REE, when adjusted for fat-free mass, was higher in patients with COPD who lost weight compared with those whose weight remained stable (23). Serum levels of TNF-α are higher in cachectic patients with COPD compared with noncachectic patients with COPD and healthy control subjects (24, 25), and elevations in IL-1 and IL-6 may also play a role in the development of cachexia (26, 27). Reductions in circulating levels of testosterone, growth hormone, insulin-like growth factor, and leptin have also been found in cachectic patients with COPD (21, 22, 25).
LVRS has numerous beneficial effects on metabolism and systemic inflammation, and can potentially reduce the processes leading to cachexia in COPD. In a study of 30 LVRS and 22 pulmonary rehabilitation patients, the LVRS group had an 8% decrease in REE adjusted for fat-free mass, compared with the rehabilitation group, which had in increase of 4.2% (17). There was also a profound decrease in respiratory muscle oxygen consumption by 44.1%, which correlated well with decreases in RV after surgery. Another study of 28 LVRS patients found significant reductions in serum levels of TNF-α, IL-6, and IL-8 after surgery, which again correlated with reductions in RV (11). Similarly, in 33 LVRS patients, the reduction in RV correlated with increases in serum ghrelin (an appetite-stimulating hormone), decreases in serum leptin (a fat-burning hormone and appetite suppressant), and increases in fat-free mass (6). In addition, all these studies demonstrated weight gain after LVRS. One study found that the reduction in RV after LVRS not only correlated with increases in BMI but was also related to improved pulmonary and cardiovascular outcomes (28). Therefore, it seems that the reduction in hyperinflation from lung volume reduction is a major mechanism responsible for the reduction in energy expenditure, systemic inflammation, and anabolic hormone metabolism, and weight gain seen after LVRS.
However, these studies involved small numbers of patients with primarily low baseline BMI (mean BMI approximately 22 to 23 kg/m2 across studies). As in prior studies, our study shows that reduction in residual volume was greater in those with significant weight gain, supporting the notion that the reduction in air trapping leads to decreased systemic inflammation and reduced REE. Unlike other studies, our study involved the analysis of 1,077 patients with a wide range of BMI, and is the first to stratify changes in weight according to baseline BMI. We also found weight gain in those who were normal weight and overweight, but not in those who were obese. The greatest increases in BMI occurred in the underweight group, suggesting that REE and systemic inflammation are highest in this group, which was more profoundly affected by LVRS.
An important contribution of our study is the demonstration of improvements in ventilatory efficiency and respiratory muscle strength in those who had significant weight gain. Ventilatory efficiency, defined as the ratio of minute ventilation to carbon dioxide production (16), has been shown to have prognostic value in heart failure and several pulmonary diseases (29, 30). At rest or during mild exercise, V̇e/V̇co2 can vary widely depending on PaCO2, anxiety, breathing pattern, ventilation–perfusion matching, underlying metabolic demand, and ratio of dead space to tidal volume (Vd/Vt) (31). The observed reductions of V̇e/V̇co2 after LVRS may be due to decreases in Vd/Vt, alterations in breathing pattern, and a fall in resting PaCO2 (32). These improvements in ventilatory efficiency may explain the decreases in REE, thereby leading to a gain in weight for a given caloric input.
Although this is the largest analysis of changes in BMI after LVRS, some limitations should be acknowledged. This study involved a select group of patients with advanced emphysema, with a post-hoc breakdown of patients into groups based on their BMI at baseline. In addition, incomplete follow-up is a weakness of our data set. Two hundred and forty (22%) of the 1,077 patients in our study population did not have data at 6 months, either due to death in the first 6 months of follow-up (53 patients) or because they did not return for the 6-month visit (187 patients), possibly due to declining health or for some reason unrelated to health. An analysis assuming that all those who missed the 6-month visit (due to death or other reason) were in the ΔBMI < 5% group gave results consistent with our primary results. An analysis assuming those who died before 6 months were in the ΔBMI < 5% group and that those who missed the visit for other reasons were in the ΔBMI ≥ 5% group gave results that were partially consistent with the primary results; in this analysis, LVRS and medical patients had similar odds of weight gain. Although our assumptions were extreme given the unequal proportions in the LVRS and medical groups of patients with ΔBMI equal to or greater than 5%, it is possible that loss to follow-up affected our findings.
Another limitation is that because only BMI was measured, it is not clear that the observed weight gain is due to cachexia reversal in these patients. Indeed, weight gain was seen in those who were normal weight or overweight, two groups that are less likely to have muscle cachexia. However, the significant improvements in maximal inspiratory and expiratory pressures are consistent with the concept that the observed weight gain is due to an increase in muscle mass. The small size of the obese group and the exclusion of patients with BMI greater than 31.1 kg/m2 (males) or 32.3 kg/m2 (females) also limit our ability to make firmer conclusions about obese patients with respect to their changes in BMI over time. The NETT protocol did not include measures of inflammatory cytokines or hormones, or nutritional evaluation such as anthropometric and metabolic parameters, to validate the results from prior studies. Last, events after randomization such as exacerbations, hospitalizations, and complications that could have had an effect on weight change were not accounted for in our analysis.
Nevertheless, our study imparts a significant contribution to our current understanding of the beneficial effects of LVRS. Our findings of weight gain after LVRS validate the findings in previous smaller studies in a large cohort of well-characterized patients in a randomized controlled trial and provide greater understanding of the patient profiles that gain weight after LVRS. We showed that weight gain is associated with changes in spirometry, respiratory muscle strength, lung volumes and ventilatory efficiency after LVRS. These physiological changes may be at least partially responsible for the weight gain in patients who undergo LVRS. In addition, a thorough and rigorous nutritional, hormonal, and metabolic assessment before LVRS may allow better prediction of changes in body composition and weight after surgery.
Acknowledgments
The authors thank Arthur Gelb, M.D., Lakewood Regional Medical Center (Lakewood, CA).
Members of the NETT Research Group: Office of the Chair of the Steering Committee, University of Pennsylvania, Philadelphia, PA: Alfred P. Fishman, M.D. (Chair); Betsy Ann Bozzarello; Ameena Al-Amin.
Clinical Centers
Baylor College of Medicine, Houston, TX: Marcia Katz, M.D. (Principal Investigator); Carolyn Wheeler, R.N., B.S.N. (Principal Clinic Coordinator); Elaine Baker, R.R.T., R.P.F.T.; Peter Barnard, Ph.D., R.P.F.T.; Phil Cagle, M.D.; James Carter, M.D.; Sophia Chatziioannou, M.D.; Karla Conejo-Gonzales; Kimberly Dubose, R.R.T.; John Haddad, M.D.; David Hicks, R.R.T., R.P.F.T.; Neal Kleiman, M.D.; Mary Milburn-Barnes, C.R.T.T.; Chinh Nguyen, R.P.F.T.; Michael Reardon, M.D.; Joseph Reeves-Viets, M.D.; Steven Sax, M.D.; Amir Sharafkhaneh, M.D.; Owen Wilson, Ph.D.; Christine Young P.T.; Rafael Espada, M.D. (Principal Investigator, 1996–2002); Rose Butanda (1999–2001); Minnie Ellisor (2002); Pamela Fox, M.D. (1999–2001); Katherine Hale, M.D. (1998–2000); Everett Hood, R.P.F.T. (1998–2000); Amy Jahn (1998–2000); Satish Jhingran, M.D. (1998–2001); Karen King, R.P.F.T. (1998–1999); Charles Miller III, Ph.D. (1996–1999); Imran Nizami, M.D. (Co-Principal Investigator, 2000–2001); Todd Officer (1998–2000); Jeannie Ricketts (1998–2000); Joe Rodarte, M.D. (Co-Principal Investigator, 1996–2000); Robert Teague, M.D. (Co-Principal Investigator, 1999–2000); Kedren Williams (1998–1999).
Brigham and Women’s Hospital, Boston, MA: John Reilly, M.D. (Principal Investigator); David Sugarbaker, M.D. (Co-Principal Investigator); Carol Fanning, R.R.T. (Principal Clinic Coordinator); Simon Body, M.D.; Sabine Duffy, M.D.; Vladmir Formanek, M.D.; Anne Fuhlbrigge, M.D.; Philip Hartigan, M.D.; Sarah Hooper, E.P.; Andetta Hunsaker, M.D.; Francine Jacobson, M.D.; Marilyn Moy, M.D.; Susan Peterson, R.R.T.; Roger Russell, M.D.; Diane Saunders; Scott Swanson, M.D. (Co-Principal Investigator, 1996–2001).
Cedars-Sinai Medical Center, Los Angeles, CA: Rob McKenna, M.D. (Principal Investigator); Zab Mohsenifar, M.D. (Co-Principal Investigator); Carol Geaga, R.N. (Principal Clinic Coordinator); Manmohan Biring, M.D.; Susan Clark, R.N., M.N.; Jennifer Cutler, M.D.; Robert Frantz, M.D.; Peter Julien, M.D.; Michael Lewis, M.D.; Jennifer Minkoff-Rau, MSW; Valentina Yegyan, B.S., C.P.F.T.; Milton Joyner, B.A. (1996–2002).
Cleveland Clinic Foundation, Cleveland, OH: Malcolm DeCamp, M.D. (Principal Investigator); James Stoller, M.D. (Co-Principal Investigator); Yvonne Meli, R.N.C. (Principal Clinic Coordinator); John Apostolakis, M.D.; Darryl Atwell, M.D.; Jeffrey Chapman, M.D.; Pierre DeVilliers, M.D.; Raed Dweik, M.D.; Erik Kraenzler, M.D.; Rosemary Lann, L.I.S.W.; Nancy Kurokawa, R.R.T., C.P.F.T.; Scott Marlow, R.R.T.; Kevin McCarthy, R.C.P.T.; Priscilla McCreight, R.R.T., C.P.F.T.; Atul Mehta, M.D.; Moulay Meziane, M.D.; Omar Minai, M.D.; Mindi Steiger, R.R.T.; Kenneth White, R.P.F.T.; Janet Maurer, M.D. (Principal Investigator, 1996–2001); Terri Durr, R.N. (2000–2001); Charles Hearn, D.O. (1998–2001); Susan Lubell, P.A.-C. (1999–2000); Peter O’Donovan, M.D. (1998–2003); Robert Schilz, D.O. (1998–2002).
Columbia University, New York, NY in consortium with Long Island Jewish Medical Center, New Hyde Park, NY: Mark Ginsburg, M.D. (Principal Investigator); Byron Thomashow, M.D. (Co-Principal Investigator); Patricia Jellen, M.S.N., R.N. (Principal Clinic Coordinator); John Austin, M.D.; Matthew Bartels, M.D.; Yahya Berkmen, M.D.; Patricia Berkoski, M.S., R.R.T. (Site Coordinator, LIJ); Frances Brogan, M.S.N., R.N.; Amy Chong, B.S., C.R.T.; Glenda DeMercado, B.S.N.; Angela DiMango, M.D.; Sandy Do, M.S., P.T.; Bessie Kachulis, M.D.; Arfa Khan, M.D.; Berend Mets, M.D.; Mitchell O’Shea, B.S., R.T., C.P.F.T.; Gregory Pearson, M.D.; Leonard Rossoff, M.D.; Steven Scharf, M.D., Ph.D. (Co-Principal Investigator, 1998–2002); Maria Shiau, M.D.; Paul Simonelli, M.D.; Kim Stavrolakes, M.S., P.T.; Donna Tsang, B.S.; Denise Vilotijevic, M.S., P.T.; Chun Yip, M.D.; Mike Mantinaos, M.D. (1998–2001); Kerri McKeon, B.S., R.R.T., R.N. (1998–1999); Jacqueline Pfeffer, M.P.H., P.T. (1997–2002).
Duke University Medical Center, Durham, NC: Neil MacIntyre, M.D. (Principal Investigator); R. Duane Davis, M.D. (Co-Principal Investigator); John Howe, R.N. (Principal Clinic Coordinator); R. Edward Coleman, M.D.; Rebecca Crouch, R.P.T.; Dora Greene; Katherine Grichnik, M.D.; David Harpole, Jr., M.D.; Abby Krichman, R.R.T.; Brian Lawlor, R.R.T.; Holman McAdams, M.D.; John Plankeel, M.D.; Susan Rinaldo-Gallo, M.E.D.; Sheila Shearer, R.R.T.; Jeanne Smith, A.C.S.W.; Mark Stafford-Smith, M.D.; Victor Tapson, M.D.; Mark Steele, M.D. (1998–1999); Jennifer Norten, M.D. (1998–1999).
Mayo Foundation, Rochester, MN: James Utz, M.D. (Principal Investigator); Claude Deschamps, M.D. (Co-Principal Investigator); Kathy Mieras, C.C.R.P. (Principal Clinic Coordinator); Martin Abel, M.D.; Mark Allen, M.D.; Deb Andrist, R.N.; Gregory Aughenbaugh, M.D.; Sharon Bendel, R.N.; Eric Edell, M.D.; Marlene Edgar; Bonnie Edwards; Beth Elliot, M.D.; James Garrett, R.R.T.; Delmar Gillespie, M.D.; Judd Gurney, M.D.; Boleyn Hammel; Karen Hanson, R.R.T.; Lori Hanson, R.R.T.; Gordon Harms, M.D.; June Hart; Thomas Hartman, M.D.; Robert Hyatt, M.D.; Eric Jensen, M.D.; Nicole Jenson, R.R.T.; Sanjay Kalra, M.D.; Philip Karsell, M.D.; Jennifer Lamb; David Midthun, M.D.; Carl Mottram, R.R.T.; Stephen Swensen, M.D.; Anne-Marie Sykes, M.D.; Karen Taylor; Norman Torres, M.D.; Rolf Hubmayr, M.D. (1998–2000); Daniel Miller, M.D. (1999–2002); Sara Bartling, R.N. (1998–2000); Kris Bradt (1998–2002).
National Jewish Medical and Research Center, Denver, CO: Barry Make, M.D. (Principal Investigator); Marvin Pomerantz, M.D. (Co-Principal Investigator); Mary Gilmartin, R.N., R.R.T. (Principal Clinic Coordinator); Joyce Canterbury; Martin Carlos; Phyllis Dibbern, P.T.; Enrique Fernandez, M.D.; Lisa Geyman, M.S.P.T.; Connie Hudson; David Lynch, M.D.; John Newell, M.D.; Robert Quaife, M.D.; Jennifer Propst, R.N.; Cynthia Raymond, M.S.; Jane Whalen-Price, P.T.; Kathy Winner, O.T.R.; Martin Zamora, M.D.; Reuben Cherniack, M.D. (Principal Investigator, 1997–2000).
Ohio State University, Columbus, OH: Philip Diaz, M.D. (Principal Investigator); Patrick Ross, M.D. (Co-Principal Investigator); Tina Bees (Principal Clinic Coordinator); Jan Drake; Charles Emery, Ph.D.; Mark Gerhardt, M.D., Ph.D.; Mark King, M.D.; David Rittinger; Mahasti Rittinger.
Saint Louis University, Saint Louis, MO: Keith Naunheim, M.D. (Principal Investigator); Robert Gerber, M.D. (Co-Principal Investigator); Joan Osterloh, R.N., M.S.N. (Principal Clinic Coordinator); Susan Borosh; Willard Chamberlain, D.O.; Sally Frese; Alan Hibbit; Mary Ellen Kleinhenz, M.D.; Gregg Ruppel; Cary Stolar, M.D.; Janice Willey; Francisco Alvarez, M.D. (Co-Principal Investigator, 1999–2002); Cesar Keller, M.D. (Co-Principal Investigator, 1996–2000).
Temple University, Philadelphia, PA: Gerard Criner, M.D. (Principal Investigator); Satoshi Furukawa, M.D. (Co-Principal Investigator); Anne Marie Kuzma, R.N., M.S.N. (Principal Clinic Coordinator); Roger Barnette, M.D.; Neil Brister, M.D.; Kevin Carney, R.N., C.C.T.C.; Wissam Chatila, M.D.; Francis Cordova, M.D.; Gilbert D’Alonzo, D.O.; Michael Keresztury, M.D.; Karen Kirsch; Chul Kwak, M.D.; Kathy Lautensack, R.N., B.S.N.; Madelina Lorenzon, C.P.F.T.; Ubaldo Martin, M.D.; Peter Rising, M.S.; Scott Schartel, M.D.; John Travaline, M.D.; Gwendolyn Vance, R.N., C.C.T.C.; Phillip Boiselle, M.D. (1997–2000); Gerald O’Brien, M.D. (1997–2000).
University of California, San Diego, San Diego, CA: Andrew Ries, M.D., M.P.H. (Principal Investigator); Robert Kaplan, Ph.D. (Co-Principal Investigator); Catherine Ramirez, B.S., R.C.P. (Principal Clinic Coordinator); David Frankville, M.D.; Paul Friedman, M.D.; James Harrell, M.D.; Jeffery Johnson; David Kapelanski, M.D.; David Kupferberg, M.D., M.P.H.; Catherine Larsen, M.P.H.; Trina Limberg, R.R.T.; Michael Magliocca, R.N., C.N.P.; Frank J. Papatheofanis, M.D., Ph.D.; Dawn Sassi-Dambron, R.N.; Melissa Weeks.
University of Maryland at Baltimore, Baltimore, MD in consortium with Johns Hopkins Hospital, Baltimore, MD: Mark Krasna, M.D. (Principal Investigator); Henry Fessler, M.D. (Co-Principal Investigator); Iris Moskowitz (Principal Clinic Coordinator); Timothy Gilbert, M.D.; Jonathan Orens, M.D.; Steven Scharf, M.D., Ph.D.; David Shade; Stanley Siegelman, M.D.; Kenneth Silver, M.D.; Clarence Weir; Charles White, M.D.
University of Michigan, Ann Arbor, MI: Fernando Martinez, M.D. (Principal Investigator); Mark Iannettoni, M.D. (Co-Principal Investigator); Catherine Meldrum, B.S.N., R.N., C.C.R.N. (Principal Clinic Coordinator); William Bria, M.D.; Kelly Campbell; Paul Christensen, M.D.; Kevin Flaherty, M.D.; Steven Gay, M.D.; Paramjit Gill, R.N.; Paul Kazanjian, M.D.; Ella Kazerooni, M.D.; Vivian Knieper; Tammy Ojo, M.D.; Lewis Poole; Leslie Quint, M.D.; Paul Rysso; Thomas Sisson, M.D.; Mercedes True; Brian Woodcock, M.D.; Lori Zaremba, R.N.
University of Pennsylvania, Philadelphia, PA: Larry Kaiser, M.D. (Principal Investigator); John Hansen-Flaschen, M.D. (Co-Principal Investigator); Mary Louise Dempsey, B.S.N., R.N. (Principal Clinic Coordinator); Abass Alavi, M.D.; Theresa Alcorn, Selim Arcasoy, M.D.; Judith Aronchick, M.D.; Stanley Aukberg, M.D.; Bryan Benedict, R.R.T.; Susan Craemer, B.S., R.R.T., C.P.F.T.; Ron Daniele, M.D.; Jeffrey Edelman, M.D.; Warren Gefter, M.D.; Laura Kotler-Klein, M.S.S.; Robert Kotloff, M.D.; David Lipson, M.D.; Wallace Miller, Jr., M.D.; Richard O’Connell, R.P.F.T.; Staci Opelman, M.S.W.; Harold Palevsky, M.D.; William Russell, R.P.F.T.; Heather Sheaffer, M.S.W.; Rodney Simcox, B.S.R.T., R.R.T.; Susanne Snedeker, R.R.T., C.P.F.T.; Jennifer Stone-Wynne, M.S.W.; Gregory Tino, M.D.; Peter Wahl; James Walter, R.P.F.T.; Patricia Ward; David Zisman, M.D.; James Mendez, M.S.N., C.R.N.P. (1997–2001); Angela Wurster, M.S.N., C.R.N.P. (1997–1999).
University of Pittsburgh, Pittsburgh, PA: Frank Sciurba, M.D. (Principal Investigator); James Luketich, M.D. (Co-Principal Investigator); Colleen Witt, M.S. (Principal Clinic Coordinator); Gerald Ayres; Michael Donahoe, M.D.; Carl Fuhrman, M.D.; Robert Hoffman, M.D.; Joan Lacomis, M.D.; Joan Sexton; William Slivka; Diane Strollo, M.D.; Erin Sullivan, M.D.; Tomeka Simon; Catherine Wrona, R.N., B.S.N.; Gerene Bauldoff, R.N., M.S.N. (1997–2000); Manuel Brown, M.D. (1997–2002); Elisabeth George, R.N., M.S.N. (Principal Clinic Coordinator, 1997–2001); Robert Keenan, M.D. (Co-Principal Investigator, 1997–2000); Theodore Kopp, M.S. (1997–1999); Laurie Silfies (1997–2001).
University of Washington, Seattle, WA: Joshua Benditt, M.D. (Principal Investigator), Douglas Wood, M.D. (Co-Principal Investigator); Margaret Snyder, M.N. (Principal Clinic Coordinator); Kymberley Anable; Nancy Battaglia; Louie Boitano; Andrew Bowdle, M.D.; Leighton Chan, M.D.; Cindy Chwalik; Bruce Culver, M.D.; Thurman Gillespy, M.D.; David Godwin, M.D.; Jeanne Hoffman; Andra Ibrahim, M.D.; Diane Lockhart; Stephen Marglin, M.D.; Kenneth Martay, M.D.; Patricia McDowell; Donald Oxorn, M.D.; Liz Roessler; Michelle Toshima; Susan Golden (1998–2000).
Other Participants
Agency for Healthcare Research and Quality, Rockville, MD: Lynn Bosco, M.D., M.P.H.; Yen-Pin Chiang, Ph.D.; Carolyn Clancy, M.D.; Harry Handelsman, D.O.
Centers for Medicare and Medicaid Services, Baltimore, MD: Steven M. Berkowitz, Ph.D.; Tanisha Carino, Ph.D.; Joe Chin, M.D.; JoAnna Baldwin; Karen McVearry; Anthony Norris; Sarah Shirey; Claudette Sikora; Steven Sheingold, Ph.D. (1997–2004).
Coordinating Center, Johns Hopkins University, Baltimore, MD: Steven Piantadosi, M.D., Ph.D. (Principal Investigator); James Tonascia, Ph.D. (Co-Principal Investigator); Patricia Belt; Amanda Blackford, Sc.M.; Karen Collins; Betty Collison; Ryan Colvin, M.P.H.; John Dodge; Michele Donithan, M.H.S.; Vera Edmonds; Gregory L. Foster, M.A.; Julie Fuller; Judith Harle; Rosetta Jackson; Shing Lee, Sc.M.; Charlene Levine; Hope Livingston; Jill Meinert; Jennifer Meyers; Deborah Nowakowski; Kapreena Owens; Shangqian Qi, M.D.; Michael Smith; Brett Simon, M.D.; Paul Smith; Alice Sternberg, Sc.M.; Mark Van Natta, M.H.S.; Laura Wilson, Sc.M.; Robert Wise, M.D.
Cost Effectiveness Subcommittee: Robert M. Kaplan, Ph.D. (Chair); J. Sanford Schwartz, M.D. (Co-Chair); Yen-Pin Chiang, Ph.D.; Marianne C. Fahs, Ph.D.; A. Mark Fendrick, M.D.; Alan J. Moskowitz, M.D.; Dev Pathak, Ph.D.; Scott Ramsey, M.D., Ph.D.; Steven Sheingold, Ph.D.; A. Laurie Shroyer, Ph.D.; Judith Wagner, Ph.D.; Roger Yusen, M.D.
Cost Effectiveness Data Center, Fred Hutchinson Cancer Research Center, Seattle, WA: Scott Ramsey, M.D., Ph.D. (Principal Investigator); Ruth Etzioni, Ph.D.; Sean Sullivan, Ph.D.; Douglas Wood, M.D.; Thomas Schroeder, M.A.; Karma Kreizenbeck; Kristin Berry, M.S.; Nadia Howlader, M.S.
CT Scan Image Storage and Analysis Center, University of Iowa, Iowa City, IA: Eric Hoffman, Ph.D. (Principal Investigator); Janice Cook-Granroth, B.S.; Angela Delsing, R.T.; Junfeng Guo, Ph.D.; Geoffrey McLennan, M.D.; Brian Mullan, M.D.; Chris Piker, B.S.; Joseph Reinhardt, Ph.D.; Blake Wood; Jered Sieren, R.T.R.; William Stanford, M.D.
Data and Safety Monitoring Board: John A. Waldhausen, M.D. (Chair); Gordon Bernard, M.D.; David DeMets, Ph.D.; Mark Ferguson, M.D.; Eddie Hoover, M.D.; Robert Levine, M.D.; Donald Mahler, M.D.; A. John McSweeny, Ph.D.; Jeanine Wiener-Kronish, M.D.; O. Dale Williams, Ph.D.; Magdy Younes, M.D.
Marketing Center, Temple University, Philadelphia, PA: Gerard Criner, M.D. (Principal Investigator); Charles Soltoff, M.B.A.
Project Office, National Heart, Lung, and Blood Institute, Bethesda, MD: Gail Weinmann, M.D. (Project Officer); Joanne Deshler (Contracting Officer); Dean Follmann, Ph.D.; James Kiley, Ph.D.; Margaret Wu, Ph.D. (1996–2001).
Footnotes
The National Emphysema Treatment Trial (NETT) is supported by contracts with the National Heart, Lung, and Blood Institute (N01HR76101, N01HR76102, N01HR76103, N01HR76104, N01HR76105, N01HR76106, N01HR76107, N01HR76108, N01HR76109, N01HR76110, N01HR76111, N01HR76112, N01HR76113, N01HR76114, N01HR76115, N01HR76116, N01HR76118, and N01HR76119), the Centers for Medicare and Medicaid Services (CMS), and the Agency for Healthcare Research and Quality (AHRQ).
Author Contributions: All authors contributed to the conception, design, data analysis, and interpretation of this manuscript.
Originally Published in Press as DOI: 10.1164/rccm.201203-0538OC on August 9, 2012
References
- 1.Chatila WM, Thomashow BM, Minai OA, Criner GJ, Make BJ. Comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc 2008;5:549–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fabbri LM, Luppi F, Beghe B, Rabe KF. Complex chronic comorbidities of COPD. Eur Respir J 2008;31:204–212. [DOI] [PubMed] [Google Scholar]
- 3.Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 2004;59:574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schols AM, Fredrix EW, Soeters PB, Westerterp KR, Wouters EF. Resting energy expenditure in patients with chronic obstructive pulmonary disease. Am J Clin Nutr 1991;54:983–987. [DOI] [PubMed] [Google Scholar]
- 5.Wagner PD. Possible mechanisms underlying the development of cachexia in COPD. Eur Respir J 2008;31:492–501. [DOI] [PubMed] [Google Scholar]
- 6.Mineo D, Ambrogi V, Frasca L, Cufari ME, Pompeo E, Mineo TC. Effects of lung volume reduction surgery for emphysema on glycolipidic hormones. Chest 2008;134:30–37. [DOI] [PubMed] [Google Scholar]
- 7.Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1791–1797. [DOI] [PubMed] [Google Scholar]
- 8.Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sorensen TI, Lange P. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med 2006;173:79–83. [DOI] [PubMed] [Google Scholar]
- 9.Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, Pinto Plata V, Cabral HJ. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004;350:1005–1012. [DOI] [PubMed] [Google Scholar]
- 10.National Emphysema Treatment Trial Research Group. A randomized trial comparing lung volume–reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059–2073. [DOI] [PubMed] [Google Scholar]
- 11.Mineo D, Ambrogi V, Cufari ME, Gambardella S, Pignotti L, Pompeo E, Mineo TC. Variations of inflammatory mediators and α1-antitrypsin levels after lung volume reduction surgery for emphysema. Am J Respir Crit Care Med 2010;181:806–814. [DOI] [PubMed] [Google Scholar]
- 12.Kretschman DM, Kim V, Pechulis RM, Criner GJ; on behalf of the National Emphysema Treatement Trial Research Group. Effect of lung volume reduction surgery on body mass index [abstract]. Am J Respir Crit Care Med 2009;179:A2915. [Google Scholar]
- 13.National Emphysema Treatment Trial Research Group. Patients at high risk of death after lung-volume-reduction surgery. N Engl J Med 2001;345:1075–1083. [DOI] [PubMed] [Google Scholar]
- 14.Wallace JI, Schwartz RS, LaCroix AZ, Uhlmann RF, Pearlman RA. Involuntary weight loss in older outpatients: incidence and clinical significance. J Am Geriatr Soc 1995;43:329–337. [DOI] [PubMed] [Google Scholar]
- 15.Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, Hill JO, Brancati FL, Peters A, Wagenknecht L; Look AHEAD Research Group. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011;34:1481–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun XG, Hansen JE, Garatachea N, Storer TW, Wasserman K. Ventilatory efficiency during exercise in healthy subjects. Am J Respir Crit Care Med 2002;166:1443–1448. [DOI] [PubMed] [Google Scholar]
- 17.Mineo TC, Pompeo E, Mineo D, Ambrogi V, Ciarapica D, Polito A. Resting energy expenditure and metabolic changes after lung volume reduction surgery for emphysema. Ann Thorac Surg 2006;82:1205–1211. [DOI] [PubMed] [Google Scholar]
- 18.Schols AM, Soeters PB, Dingemans AM, Mostert R, Frantzen PJ, Wouters EF. Prevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitation. Am Rev Respir Dis 1993;147:1151–1156. [DOI] [PubMed] [Google Scholar]
- 19.Engelen MP, Schols AM, Baken WC, Wesseling GJ, Wouters EF. Nutritional depletion in relation to respiratory and peripheral skeletal muscle function in out-patients with COPD. Eur Respir J 1994;7:1793–1797. [DOI] [PubMed] [Google Scholar]
- 20.Sergi G, Coin A, Marin S, Vianello A, Manzan A, Peruzza S, Inelmen EM, Busetto L, Mulone S, Enzi G. Body composition and resting energy expenditure in elderly male patients with chronic obstructive pulmonary disease. Respir Med 2006;100:1918–1924. [DOI] [PubMed] [Google Scholar]
- 21.Creutzberg EC, Casaburi R. Endocrinological disturbances in chronic obstructive pulmonary disease. Eur Respir J Suppl 2003;46:76s–80s. [DOI] [PubMed] [Google Scholar]
- 22.Koehler F, Doehner W, Hoernig S, Witt C, Anker SD, John M. Anorexia in chronic obstructive pulmonary disease: association to cachexia and hormonal derangement. Int J Cardiol 2007;119:83–89. [DOI] [PubMed] [Google Scholar]
- 23.Schols AM, Soeters PB, Mostert R, Saris WH, Wouters EF. Energy balance in chronic obstructive pulmonary disease. Am Rev Respir Dis 1991;143:1248–1252. [DOI] [PubMed] [Google Scholar]
- 24.Di Francia M, Barbier D, Mege JL, Orehek J. Tumor necrosis factor-α levels and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1994;150:1453–1455. [DOI] [PubMed] [Google Scholar]
- 25.Takabatake N, Nakamura H, Abe S, Hino T, Saito H, Yuki H, Kato S, Tomoike H. Circulating leptin in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999;159:1215–1219. [DOI] [PubMed] [Google Scholar]
- 26.Broekhuizen R, Grimble RF, Howell WM, Shale DJ, Creutzberg EC, Wouters EF, Schols AM. Pulmonary cachexia, systemic inflammatory profile, and the interleukin 1β-511 single nucleotide polymorphism. Am J Clin Nutr 2005;82:1059–1064. [DOI] [PubMed] [Google Scholar]
- 27.Van Helvoort HA, Heijdra YF, Thijs HM, Vina J, Wanten GJ, Dekhuijzen PN. Exercise-induced systemic effects in muscle-wasted patients with COPD. Med Sci Sports Exerc 2006;38:1543–1552. [DOI] [PubMed] [Google Scholar]
- 28.Mineo D, Ambrogi V, Lauriola V, Pompeo E, Mineo TC. Recovery of body composition improves long-term outcomes after lung volume reduction surgery for emphysema. Eur Respir J 2010;36:408–416. [DOI] [PubMed] [Google Scholar]
- 29.Kleber FX, Vietzke G, Wernecke KD, Bauer U, Opitz C, Wensel R, Sperfeld A, Glaser S. Impairment of ventilatory efficiency in heart failure: prognostic impact. Circulation 2000;101:2803–2809. [DOI] [PubMed] [Google Scholar]
- 30.Hansen JE, Wasserman K. Pathophysiology of activity limitation in patients with interstitial lung disease. Chest 1996;109:1566–1576. [DOI] [PubMed] [Google Scholar]
- 31.Wasserman K, Hansen JE, Sue DY, Stringer WW, Whipp BJ. Principles of exercise testing and interpretation: including pathophysiology and clinical applications. Philadelphia, PA: Lippincott Williams &Wilkins; 2005.
- 32.Criner GJ, Belt P, Sternberg AL, Mosenifar Z, Make BJ, Utz JP, Sciurba F; National Emphysema Treatment Trial Research Group. Effects of lung volume reduction surgery on gas exchange and breathing pattern during maximum exercise. Chest 2009;135:1268–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]