SUMMARY
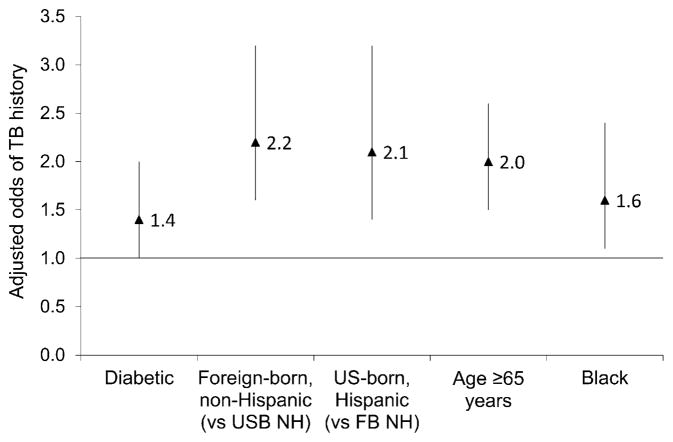
Blacks and Hispanics are disproportionately affected by diabetes, which may confound ethnic association with tuberculosis (TB). We analyzed 2000–2005 National Health Interview Survey data. We present adjusted odds ratios (aORs) and 99% confidence intervals (CIs) for the association of diabetes with history of TB disease, controlling for race/ethnicity and age. Diabetics had an aOR of 1.4 (99%CI 1.0–2.0) for history of TB, controlling for being foreign-born non-Hispanic (aOR 2.2, 99%CI 1.6–3.2), US-born Hispanic (aOR 2.1, 99%CI 1.4–3.2), age ≥65 years (aOR 2.0, 99%CI 1.5–2.6), and being Black (aOR 1.6, 99%CI 1.1–2.4). After controlling for race/ethnicity, self-identified diabetics had an increased aOR for history of TB.
Keywords: tuberculosis, diabetes
The centers for disease control and Prevention (CDC) estimates that over 18 million persons, or 6.3% of the US population, had diabetes in 2002.1 All but 0.3% of the diabetics were aged ≥20 years and 47% were aged ≥60 years.1 The estimated prevalence of diabetes had increased to 24 million persons (7.8%) by 2007, of whom 24% were undiagnosed.2
Diabetes is associated with tuberculosis (TB) disease incidence. While evidence is not conclusive that diabetes precedes and increases TB risk after latent TB infection (LTBI), three international prospective cohort studies found a three-fold greater risk of diabetics developing TB compared with non-diabetics.3 One study found that diabetes preceded TB in 78% of subjects.4 From case-control studies, the odds of persons with TB having diabetes (vs. not having diabetes) ranged from 1.2 to 7.8.3,5 A review presents potential mechanisms of interaction between TB and diabetes.6
While diabetes is associated with TB, Black and Hispanic race/ethnicities are also associated with TB. However, Blacks and Hispanics are disproportionately affected by diabetes, which may confound the association with TB.
The study objectives were to describe the prevalence of self-reported history of TB and diabetes from the US National Health Interview Survey (NHIS), and to analyze the association of history of TB with diabetes, controlling for race/ethnicity and age.
METHODS
The author aggregated six years (2000–2005) of NHIS data, an annual face-to-face multistage stratified cluster probability survey of civilian, non-institutionalized household residents aged ≥18 years representative of the US population. Since 1997, NHIS has included seven questions about TB disease knowledge and attitudes. Among all aggregated respondents, 87% had heard about TB and were asked: ‘What are your chances of getting TB? Would you say high, medium, low, or none?’ ‘Already have TB’ was a response category to the above question. It seemed most plausible that this meant respondents had a history of TB disease rather than current TB disease at the time of survey, and it was therefore designated as ‘history of TB’. We described the self-reported prevalence of diabetes by region of birth, by years in the United States, and associated socio-economic factors.
No human subjects approval was necessary for this anonymous data based study.
We used SUDAAN® (RTI International, Research Triangle Park, NC, USA) multivariate logistic regression to model history of TB and its association (adjusted odds ratios [aORs]) with diabetes, controlling for sex, race/ethnicity, foreign birth, age, high school drop-out, history of homelessness or incarceration, ever cancer diagnosis, current cigarette smoking, past year alcohol abuse, no health insurance and ever human immunodeficiency virus (HIV) testing. Race/ethnicity was defined as white, black, Hispanic, or other, which were consistently reported over time (other race/ethnicity likely includes mostly Asian and American Indian/Alaskan Natives, which comprise 5% and 1%, respectively, of the US population).7 The responses were weighted for the sampling design, ratio, non-response and post-stratification adjustments to census totals for sex, age and race/ethnicity. Only bivariate ORs and aORs significant at the 99% confidence interval (CI) are presented. Cited percentages are of the weighted sample.
RESULTS
The number of unweighted respondents from 2000 to 2005 was 190 350: 48% were males and 52% females. Whites comprised 73% of the sample, Blacks 11%, Hispanics 12% and other race/ethnicity 4%; 14% were foreign born, of whom 1.7% had resided in the United States for <1 year, 14.4% for 1–4 years, 15.7% for 5–9 years, 14.9% for 10–14 years and 53.2% for ≥15 years; 13% were aged 18–24, 39% aged 25–44, 32% aged 45–64 and 15% aged ≥ 65 years.
Approximately 0.31% (unweighted n = 668) reported a history of TB (i.e., a past prevalence rate = 310 per 100 000 population). Foreign-born respondents reported twice the rate (550/100 000) of US-born respondents (260/100 000).
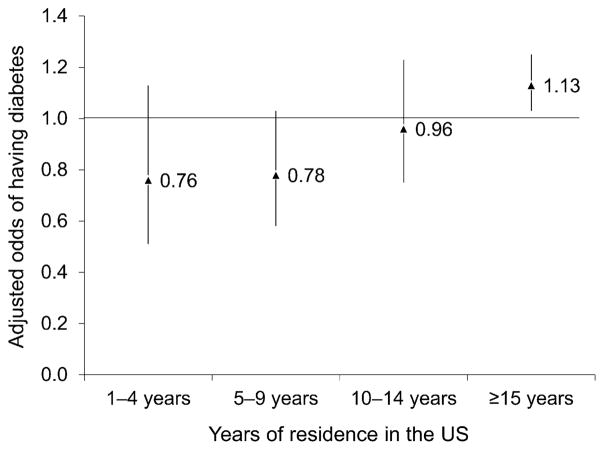
Almost 7% (6.65%, unweighted n = 13 798) reported having diabetes. In bivariate analyses, those aged ≥65 years had 3.8 times greater odds of diabetes than younger respondents. Diabetes prevalence was also high among those who had cancer (OR 2.4), low education (OR 2), were aged 45–64 years (OR 1.9), were Black (OR 1.5) and were male (OR 1.1). Diabetes prevalence was highest (>7%) in those born on the Indian subcontinent, followed by (nearly 7%) those born in the United States, Mexico, Central America, the Caribbean Islands and Africa. In a model of diabetes by residence cohort controlling for age, foreign-born respondents in the United States for ≥15 years had a significant 13% increased aOR compared with those in the United States for <1 year; the aORs increased in each of the remaining cohorts, but were not statistically significant (Figure 1).
Figure 1.
Odds of having diabetes mellitus in relation to years of residence in the United States adjusted for age. 99% confidence levels are shown. Adjusted odds ratios are from multivariate analysis including the above years in the United States and age groups 25–44, 45–64 and ≥65 years.
The unadjusted odds of diabetics having a TB history was 1.8 (99%CI 1.3–2.4). Figure 2 shows the aORs of TB history associated with diabetes, controlling for foreign birth, race/ethnicity and age. Diabetics had a 40% increased odds (aOR 1.4, 99%CI 1.0–2.0) of TB history, controlling for being foreign-born non-Hispanic (aOR 2.2, 99%CI 1.6–3.2; vs. US-born non-Hispanic), US-born Hispanic (aOR 2.1, 99%CI 1.4–3.2; vs. foreign-born non-Hispanic), age ≥65 years (aOR 2.0, 99%CI 1.5–2.6; vs. younger), and being Black (aOR 1.6, 99%CI 1.1–2.4; vs. non-Black).
Figure 2.
History of TB in relation to demographic and clinical characteristics. The odds are adjusted for all variables shown in this graph. All odds ratios are significant at the 99% confidence level. TB = tuberculosis; USB = US-born; NH = non-Hispanic; FB = foreign-born.
DISCUSSION
Our study found that diabetics (vs. non-diabetics) were more likely to be aged ≥45 years, to have had cancer, to have low education, to be Black or to be male, factors also associated with US TB incidence. Among foreign-born persons, we found that reported diabetes prevalence rose with each consecutive 5-year cohort of US residence, adjusted for age. If diabetes prevalence rates in India, where they are the highest, foretell diabetes expectations among US foreign-born populations, then the association between diabetes and TB will be very important to US efforts to eliminate TB. By concurrently analyzing factors associated with both TB and diabetes, we found that diabetics had a 40% increased odds of TB, controlling for the confounding effects of race/ethnicity and age.
The study’s limitations include the cross-sectional nature of NHIS data that does not permit time of diabetes or TB incidence assessment. Self-reported diabetes or TB data might be underestimated or overestimated. The study’s TB history prevalence of 0.31% is approximately 7% of estimated LTBI prevalence (4.2%),8 which is consistent with knowledge that <10% of those with LTBI progress to TB.9,10 As the NHIS questions were about TB disease and none about LTBI, we assumed the responses reflected TB disease.
CONCLUSIONS
There are approximately 24 million diabetics in the United States, some of whom (due to TB exposure and LTBI) are at high risk for TB progression. Self-reported diabetics, obviously previously diagnosed, are likely to be receiving diabetes care and theoretically have access to LTBI treatment for TB prevention. Diabetes providers should be aware of the increased TB risk of their clients.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the author and do not necessarily represent the views of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet. Atlanta, GA, USA: CDC; 2010. [Accessed April 2011]. http://www.cdc.gov/diabetes/pubs/estimates.htm. [Google Scholar]
- 2.Centers for Disease Control and Prevention. National diabetes fact sheet, 2007. Atlanta, GA, USA: CDC; 2007. [Accessed April 2011]. http://apps.nccd.cdc.gov/DDTSTRS/FactSheet.aspx. [Google Scholar]
- 3.Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PloS Med. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. http://www.plosmedicine.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dyck RF, Klomp H, Marciniuk DD, et al. The relationship between diabetes and tuberculosis in Saskatchewan: comparison of registered Indians and other Saskatchewan people. Can J Public Health. 2007;98:55–59. doi: 10.1007/BF03405386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevenson CR, Critchley JA, Forouhi NG, et al. Diabetes and the risk of tuberculosis: a neglected threat to public health. Chronic Illness. 2007;3:228–245. doi: 10.1177/1742395307081502. [DOI] [PubMed] [Google Scholar]
- 6.Dooley KE, Chaisson R. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis. 2009;9:737–746. doi: 10.1016/S1473-3099(09)70282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Census Bureau. Annual estimates of the population by sex, race, and Hispanic or Latino origin for the United States: April 1, 2000 to July 1, 2009. Washington DC, USA: US Census Bureau; 2009. [Accessed April 2011]. http://www.census.gov/popest/national/asrh/NC-EST2009-srh.html. [Google Scholar]
- 8.Bennett DE, Courval JM, Onorato I, et al. Prevalence of tuberculosis infection in the United States population: the national health and nutrition examination survey, 1999–2000. Am J Respir Crit Care Med. 2008;177:348–355. doi: 10.1164/rccm.200701-057OC. [DOI] [PubMed] [Google Scholar]
- 9.Aronson NE, Santosham M, Comstock GW, et al. Long-term efficacy of BCG vaccine in American Indians and Alaska natives: a 60-year follow-up study. JAMA. 2004;291:2086–2091. doi: 10.1001/jama.291.17.2086. [DOI] [PubMed] [Google Scholar]
- 10.Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis: a general review. Adv Tuberc Res. 1969;17:49–57. [PubMed] [Google Scholar]