Abstract
Japan has experienced pronounced population aging, and now has the highest proportion of elderly adults in the world. Yet few projections of Japan’s future demography go beyond estimating population by age and sex to forecast the complex evolution of the health and functioning of the future elderly. This study estimates a new state-transition microsimulation model – the Japanese Future Elderly Model (FEM) – for Japan. We use the model to forecast disability and health for Japan’s future elderly. Our simulation suggests that by 2040, over 27 percent of Japan’s elderly will exhibit 3 or more limitations in IADLs and social functioning; almost one in 4 will experience difficulties with 3 or more ADLs; and approximately one in 5 will suffer limitations in cognitive or intellectual functioning. Since the majority of the increase in disability arises from the aging of the Japanese population, prevention efforts that reduce age-specific morbidity can help reduce the burden of disability but may have only a limited impact on reducing the overall prevalence of disability among Japanese elderly. While both age and morbidity contribute to a predicted increase in disability burden among elderly Japanese in the future, our simulation results suggest that the impact of population aging exceeds the effect of age-specific morbidity on increasing disability in Japan’s future.
Keywords: Future Elderly Model, Microsimulation, Aging, Comorbidities, Long-term Care, Japan
1. Introduction
Population aging is a worldwide phenomenon, yet across the globe there are wide differences both in the rate of aging and the current age structure of societies (Kapteyn 2010). For some countries, the impact of a rapidly aging society can no longer be considered a hypothetical scenario far off in the future (Schoeni and Ofstedal 2010), Japan, in particular, has experienced pronounced population aging, with over 26.3% of the population aged 65 and over1, and now has the highest proportion of elderly adults in the world2. Yet few projections of Japan’s future health needs go beyond estimating population by age and sex to forecast the complex evolution of the health and functioning of the future elderly. In the last two decades, methodological advances in population studies and simulations have made it possible to estimate the needs of the future elderly, with implications for potential policy response. The goal of this study is to develop a model that projects the health conditions, disability and functional status of Japan’s elderly population. Such a model can support evidence-based assessments of future demand for health care, long-term care, public pensions, welfare and other government-supported programs, as well as labor force participation.
Japan’s super-aging demographic trends present a series of policy challenges for which a detailed model of competing risks for the future elderly would be useful (Ogawa, Mason et al. 2007). Long-term care insurance program spending (Miyazawa, Moudoukoutas et al. 2000) and medical care spending (Dow, Philipson et al. 1999, Lee and Skinner 1999, Gerdtham, Lundin et al. 2005, Bech, Christiansen et al. 2011) will be most directly impacted. Our study may hold particular interest for Japan’s policymakers with respect to planning for long-term care insurance. Since 2000, Japan has had a socialized long-term care insurance program that is both public and universal. All elderly Japanese over 65, regardless of means or the availability of a caregiver, are eligible for coverage based strictly on physical and mental disability (Campbell and Ikegami 2000). Japan’s generous long-term care insurance covers a substantial portion of need for disability care (Tamiya et al., 2011). Benefits cover a range of long-term care services, from institutional care for those with the most severe disabilities to at-home care services, community-based services, and “preventive services3” including outpatient rehabilitation care services for those who can otherwise live independently (Shimizutani 2014). In 2005, Japan spent approximately US$ 1,751 per person on long-term care, and 2008 figures reveal that 13.5% of all Japanese persons 65 years of age and older receive long-term care benefits, although 20% of those eligible chose not to receive any benefits (Campbell, Ikegami et al. 2010). Rising disability, such as that predicted by our simulation model, has tremendous implications for the sustainability of Japan’s socialized long-term care insurance program (Tamiya et al., 2011).
Our work elucidates the challenges that Japan faces by projecting the health needs of its future elderly. Most population projections for Japan have not modeled health status and disability, but simply projected population by age and sex. A few recent studies have attempted to go further (Fukawa 2007, Ogawa, Retherford et al. 2010, Shimizutani, Fujii et al. 2014). For example, Shimizutani et al. (2014) recently used the Japan Study of Aging and Retirement (JSTAR) data to estimate factors, including health, that affect the retirement decisions of the middle-aged and elderly in Japan. They develop a simulation model for enrollment into Japan’s disability program. While these studies represent an encouraging trend, there is much to gain from a more flexible and powerful simulation model of population aging in a country of Japan’s global economic importance that takes advantage of high quality longitudinal datasets like JSTAR. (See, for instance, Hauser and Weir, 2010; Yashin, Akushevich et al., 2013; and Zheng, 2014).
This paper extends the literature by developing a demographic and economic state-transition micro-simulation model for Japan that enables analysis of the impact of demographic change, aging, and population health on disability and care receiving. We estimate the model using the recently released multiple waves of the JSTAR survey, the Japanese version of the family of internationally comparable surveys that include the U.S. Health and Retirement Study (HRS), the English Longitudinal Survey on Ageing (ELSA), and the Survey on Health, Aging and Retirement in Europe (SHARE).
Our model is similar in structure to the American Future Elderly Model (Goldman et al., 2005), but with Japan-specific disease prevalence and transition probabilities and additional methodological innovations to compute Japan-specific conditional mortality rates. Our adaptation of the American FEM to Japan using Japanese data and innovate methodology to compensate for data limitations represents two of the most significant contributions of our work, given that country-specific disease prevalence and transition probabilities require customized data for each national FEM projection. Our strategy requires first estimating disease transition probabilities for diseases prevalent among Japanese middle-aged and elderly populations. We then estimate Japan-specific age-sex-specific mortality rates from Japanese death certificate data. Next, we use these health and mortality transition functions to construct a micro-simulation forecast of the health and age structure of Japan’s population over the next decades. Finally, we estimate how disabled this future population is likely to be given their health status. Our measure of disability, derived from the JSTAR survey, includes functional status measures like Activities of Daily Living (ADLs), Instrumental Activities of Daily Living (IADLs), as well as additional measures of cognition and social functioning.
More parsimonious macro-focused models are available to forecast the future health needs of the Japanese population, based on age structure alone. However, the great advantage of the FEM framework is that it permits counterfactual analyses of health policy interventions or future trends. For instance, we are able to simulate the impact of primary or secondary prevention efforts on Japan’s future disability burden in a way that is not possible using macro models.
We find that by 2040, over 27 percent of Japan’s elderly will exhibit 3 or more limitations in IADLs and social functioning; almost one in 4 will experience difficulties with 3 or more ADLs; and approximately one in 5 will suffer limitations in cognitive or intellectual functioning. The majority of the increase in disability arises from the aging of the Japanese population. Therefore, the economic impact of prevention efforts that reduce the underlying comorbid conditions associated with disability may be limited.
The remainder of this paper is organized as follows. Section 2 describes Japan’s demographic and institutional background. Section 3 describes the data and the methodology for adapting the FEM to Japan. Section 4 presents the empirical results regarding disability of Japan’s future elderly. The final section discusses policy implications. A technical appendix describes in greater detail the operationalization of the future elderly model in the Japanese context.
2. Background
The Japanese populace is well educated, with 34.7% of the population ultimately attaining a college education.4 The size of Japan’s working population in 2010 was 59.4% of the total population—roughly 65 million workers, which is similar to the labor force participation rate in the United States (Index Mundi 2011). However, as a result of longevity increase and fertility decline, Japan is experiencing dramatic population aging. Like most high-income countries, Japan has nearly zero population growth, with a total fertility rate well below replacement.
Since 1960, Japan has achieved the highest gains in life expectancy at age 65 among all OECD countries, with an increase of almost ten years for women and over seven years for men (OECD 2013). Life expectancies at age 65 (11.4 for women, 8.4 for men) and at age 80 are the highest in the world except for France (OECD 2013). Nearly 40% of the population will be aged over 65 years by 2050, and the proportion of the population aged over 80 is expected to nearly triple between 2010 and 2050 (rising from 6% to 16% (OECD 2013)).
Alongside mortality declines, Japan has experienced changes in morbidity, suggesting the need for models such as the FEM to forecast the future health of the elderly. The rate of obesity in Japan (4%) is lower than nearly all other high-income countries—with obesity in the US almost ten-fold the low rates of Japan. While hypertension prevalence remains high in Japan, rates have been declining since the 1980s. Japan has among the lowest death rates from ischemic heart disease (IHD) in the OECD (OECD 2013). By contrast, cancer incidence and mortality have increased, likely due to Japan’s aging population.5 Cancer is the leading cause of death in Japan (similar to Canada, Denmark, France, and the Netherlands). While rates of stomach cancer are higher than in the West and the incidence of once rare colorectal cancer is increasing, lung cancer has emerged as the main cause of death among patients with cancer (OECD 2013). Given the smoking rates among men, cancer mortality rates among men are not surprisingly more than twice those for women.
The confluence of low fertility, longevity, and reduced morbidity and mortality from many diseases (except for cancer) has resulted in a dramatic aging in Japan’s population. In addition, projections predict that the population will shrink to 87 million by 2060, with nearly 40 percent over the age of 65. In light of these demographic trends, Japan represents a “super-aging society” even among aging OECD countries.6 In the US, the Old Age Dependency Ratio (OADR, ratio of population age 65 and above to age 20 to 64) is projected to rise from 22% in 2010 to 39% in 2050 (Lee 2014). In Japan, the OADR was already 39% in 2012 and is projected to reach more than 70% by 2050 (OECD 2007).
While the sharp rise in the old age dependency ratio has been offset somewhat by the high labor force participation among the Japanese elderly compared to many other OECD countries, it remains questionable whether Japan can escape from the huge burden of social security and health expenditures (Ichimura, Shimizutani et al. 2009). For example, the poverty rate—defined as the proportion of individuals with equalized disposable income less than 50% of the median income—is higher in Japan (21.1%), and disproportionately among the elderly7, compared to most European countries (Ichimura, Shimizutani et al. 2009).
The rapid aging of the Japanese population poses a significant challenge to the government to maintain the financial viability of its health and long-term care system. Among all OECD countries, Japan allocates the greatest share of hospital expenditures to people aged 65 and over (64%), associated with the fact that it also has the highest share of people in that age group (23%; (OECD 2013)). Only in Israel and Japan (among OECD countries) has health spending growth as a percent of GDP accelerated rather than declined since the financial crisis of 2009 (OECD 2013), and both a stagnant GDP and population aging are important reasons.
The changing mortality and morbidity pattern in Japan increasingly strains Japan’s health and long-term care systems in ways that contrast with many other OECD countries. For example, Japan and Korea have the longest hospital stays, at more than double the OECD average of 8.0 days in 2011. A salient reason is that many acute care hospitals provide a significant share of long-term care services (“social admissions”) and serve the functions of skilled nursing facilities in a country like the United States. For example, Japan has the highest expenditure per discharge for cancer among OECD countries, probably because of its much longer lengths of stay (OECD 2013). Japan also has, by far, the highest number of MRI and CT scanners per capita. Largely because of a 2010 change in OECD accounting rules that now includes long-term care expenditures in total health expenditures, Japan’s ratio of health spending to GDP now exceeds the OECD average, revealing the true extent of Japan’s total financial burden from its aging population.
3. Data
Our data derives from the Japanese Study of Aging and Retirement (JSTAR), one of Japan’s first longitudinal datasets on middle-aged and elderly Japanese specifically designed for cross-national scientific investigation of aging and retirement. Two waves of interviews in 2007 and 2009 surveyed 3,862 respondents between 47 and 77 in five Japanese cities (Adachi, Kanazawa, Shirakawa, Sendai and Takikawa) on a variety of economic, social, and health conditions. The survey includes over 1,400 questions designed to mirror and ensure comparability with other surveys conducted internationally, such as the Health and Retirement Survey (HRS) in the United States, the Survey of Health, Aging and Retirement in Europe (SHARE), and the English Longitudinal Study of Aging (ELSA) in the United Kingdom. JSTAR is modeled after the US Health and Retirement Survey, and is thus comparable to that high quality panel data set on the elderly (Ichimura, Shimizutani et al. 2009). Only a subset of these data (90%) is released for research use. The response rate in the second wave among the respondents from the first wave is about 80% (i.e., an attrition rate of about 20%), with some variation across municipalities (Shimizutani, Fujii et al. 2014).
While only focused on a few municipalities and thus not nationally representative, JSTAR researchers argue that the focus on variations in a large number of individuals in selected municipalities controls for cultural, historical, and policy environment and thus constitutes “a unique approach to examining a variety of topics on aging and retirement and contributes to rethinking a way of sampling survey data” (Ichimura, Shimizutani et al. 2009). The JSTAR team is currently developing sample weights for the JSTAR survey, and in future extensions of our model, we hope to incorporate these weights so that our study results better reflect the Japanese population as a whole. For the current manuscript, we have weighted our sample by age and sex in order to reflect the 50- to 79-year-old population in Japan in 2007 (See Appendix Table 1 for the sample weights). Please see Appendix 2 for a more complete discussion of the strengths and weaknesses of the JSTAR data.
In addition to the prevalence of health conditions, JSTAR also includes detailed self-reported information on physical or mental limitations in performing Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). Furthermore, JSTAR also asks respondents detailed questions on measures of social and intellectual engagement, as well as caregiving and care receiving, both formally at skilled nursing facilities or informally through friends and family members.
Because JSTAR includes respondents only up to the age of 77, we construct a simulated population of 80- to 100-year-olds (“oldest old”) for 2010 by aging our current population into the future. That is, current 60- to 77-year-old Japanese in JSTAR are aged 20 years using our state-transition microsimulation model, and added to our 50- to 77-year-olds in 2010 to have a cohort of Japanese individuals from 50 to 100 in the first year of our cohort. To ascertain that our simulated “oldest-old” population is realistic, we compare our simulated oldest old cohort from JSTAR with actual 80–100-year old Japanese individuals in the Nihon University Japanese Longitudinal Study of Aging (NUJLSOA), with 1,921 respondents over age 80. NUJLSOA also includes detailed information on ADLs and IADLs, but has only 14 of the 19 health conditions available in JSTAR.
The NUJLSOA is a nationally representative longitudinal survey of individuals aged 65 and over in Japan. We use two waves of the data, the first wave of which was collected in November 1999, the second, in November 2001. NUJLSOA had a more limited focus than JSTAR, and was designed primarily to study changes in the health status of the Japanese elderly over time. In addition, NUJLSOA also investigated the association between long-term care insurance and healthcare utilization as well as the relationship between co-residence and the use of long-term care. While the emphasis of the data is on health and healthcare utilization, several other topics related to aging, such as intergenerational transfer, living arrangements, caregiving, and labor force participation, are included in the survey data.
We chose the following sample selection criteria for our primary data set, JSTAR. Individuals must be at least 45 years old. This yielded 3,862 respondents with a total of 7,724 interview years. We then dropped observations of individuals with a missing value for any of our health measures of interest. Following this selection criterion, we arrived at the final estimation sample consisting of 2,526 individuals for 2007, 2,659 for 2009, and 1,854 individuals and 3,708 interview years for the pooled JSTAR data. For the 80+ cohort in the NUJLSOA data, the same exclusion criteria led to a total of 1,921 survey respondents and 3,842 respondent-years. Most missing data occurred for self-reported health states. The summary statistics for the JSTAR study sample in 2007 are presented in Appendix Table 1.
4. Methods
The Future Elderly Model (FEM) is a demographic and economic simulation model designed to predict the future health status of the elderly and explore what current trends or future shifts imply for policy (Goldman et al., 2005). The FEM is a state-transition microsimulation model that permits direct modeling of competing mortality risks. It also permits counterfactual analyses of hypothetical scenarios, such as the implications of a smoke-free or obesity-free population on health and mortality, by replacing the model parameters with alternative values and rerunning the simulation. We present an abridged discussion of the FEM below, and include only our main policy-relevant simulation results from the state-transition model in the main text. A detailed description of the evaluation and construction of the FEM is provided in the Technical Appendix.
4.1 Health Transition Model
This section describes the steps we took to estimate individual health transition models for the Japan FEM. The JSTAR and NUJLSOA data provide self-reported health status measures. With JSTR, we use logit regressions to estimate the probability of transitioning to each of 19 health conditions in 2009 based on the presence of those same health conditions in 2007 and controlling for demographic and comorbid conditions in 2007.
Because these health states are measured by responses to questions that are prefaced by “Have you ever been told by a doctor ….”, we treat all health status states as absorbing. In sensitivity analyses, we estimated the likelihood of transitioning out of the disease states but found little evidence of recovery for the listed medical conditions in our sample (that is, very few people who reported a health condition in 2007 reported not having that same condition in 2009). As a result, we only model transitions into these states (without allowing for cure) in the following logit functional form: , where pi,j,t+2 is the probability of having the j-th condition for individual i at time t+2 (2009) conditional on not having the j-th condition at time t; and Xijt are demographic characteristics (age, and where appropriate, an indicator for BMI ≥ 23.5, and an indicator for heavy smoking, defined as ≥ 20 cigarettes per day) and co-morbidities for individual i in time t (2007) that affect the onset of condition j.
The probabilities of the onset of the various conditions are assumed to be linear in the covariates. Age and male gender enter into all transition models, but the other covariates enter into the regression only if the two medical doctors on our author list agreed that they are likely causative factors in the onset of the specific disease model in question. Given the low prevalence of obesity in Japan, we choose a BMI value of 23.5 as our measure of excess body weight. For smoking, because of the high number of smokers among Japanese males, we set the indicator variable for smoker if the respondent answers smoking 20 or more cigarettes per day in 2007. Sensitivity analyses suggest that our results would be qualitatively similar if we had chosen different cut-offs.
The unit of observation is the interview-pair. All independent variables are measured with a two-year lag, and represent the respondent’s characteristics as of 2007. Transition probabilities are estimated only using individuals who did not suffer from a specific condition at baseline. As a result, the sample sizes for various health status transition regressions vary. For example, consider a respondent who was interviewed in 2007 without cancer but with a heart condition. In 2009, he is diagnosed with cancer. This person’s baseline condition included “heart disease,” so given our assumption that health conditions are absorbing, he does not contribute to the heart disease transition model in any way. On the other hand, he contributes one observation to the cancer transition model. Because JSTAR had only two time points during construction of the health state-transition matrix, we ignore clustering standard errors at the individual level because any given person will contribute at most one observation to a specific disease model.
We generate sample weights by sex and age in five-year increments (50–54, 55–59, …, 75–79) by dividing the number of the Japanese population in each age group-sex category by the number of the JSTAR population in the same category, and normalizing the weights such that they sum to one across the JSTAR age group-sex categories. We use these weights as probability weights in our logit regressions so that the age-sex mix of our results reflects that Japanese population.
4.2 Disability Models
We use our model to simulate how the probability of functional limitations and cognitive disability will change given population aging. JSTAR data assesses survey participants for the presence of activities of daily living limitations (ADLs) and instrumental activities of daily living (IADLs). The former measures an individual’s ability to perform basic tasks like bathing oneself or feeding oneself; the latter measures an individual’s social roles and engaging in higher-level activities, such as managing finances and shopping for groceries.
Measures of ADLs in the JSTAR survey data follow closely the standard definition used in the HRS family of surveys. JSTAR includes questions on whether respondents are able to dress themselves, walk around in their room, bathe, eat, get in and out of bed, and use Western-style toilets. We use the number of ADLs performed with difficulty as the outcome variable of interest, defined as 0, 1, 2, and 3 or more. Measures of IADLs are captured by seven questions that ask whether respondents are able to take public transportation alone, shop for daily necessities, prepare daily meals, pay bills, handle their own banking, make telephone calls and take medications. Again, we use 0, 1, 2, and 3 or more IADLs performed with difficulty as the outcome variable.
Four additional questions each pertain to the survey respondents’ social interactions (visiting friends, being called on for advice, visiting sick friends, and initiating conversations with younger individuals) and intellectual activities (filling out pension forms, reading the newspaper, reading books or magazines, and taking interest in the news). For these two measures of social function as well, we use four categories for the outcome variable, i.e., having difficulty with 0, 1, 2, or 3+ functions. Finally, we code as dichotomous variables whether respondents received any type of help, any help for physical care, and any help for household chores from friends or family members.
We project future disability status (number of ADLs, IADLs, social/intellectual tasks performed with difficulty, and the receipt of assistance from friends/family) using ordered logit regressions for all specifications with 0, 1, 2, and 3+ as the outcome variable, and logit regression for all specifications with dichotomous outcome variables. The explanatory variables are the full set of covariates as described in the health transition model, including age, gender, weight, smoking status, and a vector of the 19 defined health conditions. Because we pool 2007 and 2009 data, each respondent potentially contributes up to two observations, and we cluster our standard errors at the individual level. These outcome models were used to predict the distribution of Japan’s future population with ADLs, IADLs, and receiving assistance through 2040, based on the FEM model projections of health conditions by age and sex among survivors.
4.3 Disease-Specific Mortality Rates
To complete the FEM simulation model, we also need to estimate disease-specific mortality rates by age and sex for the Japanese population. The Japanese vital statistics data provide detailed information on the leading cause of mortality by age and sex. However, there is limited information the health conditions that the individual had at the time of death: only the leading cause of death is reported. The difficulty is that the proximate cause of death listed on the death certificate often represents the end stage of a complex disease process. For instance, a patient with diabetes is more likely to suffer from a heart attack, leading to congestive heart failure which predisposes a patient to fluid build up in the lungs and pneumonia. If that patient dies with pneumonia, doctors will typically list that as the cause of death, even though the patient’s diabetes and heart disease played key roles.
Using JSTAR and these mortality data, we developed an algorithm to compute condition-specific mortality rates for each of the 19 conditions, as described in more detail in the Technical Appendix. In brief, we used the iterative proportional fitting (IPF) algorithm to calculate the conditional mortality rates from JSTAR and the Japanese vital statistics data (Statistics Bureau). Intuitively, the algorithm reduces the conditional probability of death from a disease condition if it is very often seen in the death certificate data, but less often seen in the JSTAR disease prevalence. To calculate the conditional mortality rates, we assume conditional independence of the disease-specific mortalities. In other words, the probability that any given disease is the cause of death does not depend on the other comorbidities that an individual has. Appendix Table 3 illustrates the setup for the IPF algorithm. The algorithm generates a ranking of conditional mortality rates that corresponds to the ranking independently derived by our physician coauthors before our statistical calculations.
5. Results
5.1 Model Calibration Results
Since our primary goal is to project Japan’s future elderly health, disability, and need for care, we report all of our state-transition probability matrices (Appendix Table 4) and estimated condition-specific mortality rates (Appendix Figure 2) in the Technical Appendix. Overall, our specifications produced plausible results, particularly for ages up to 77 (the oldest respondents in the JSTAR dataset in 2007). For example, our transition matrix predicts that greater age, male gender, BMI greater than 23.5, as well as having heart disease, hyperlipidemia, cerebrovascular disease, and liver disease in 2007 are all positively associated with the probability of developing hypertension by 2009. Likewise, having a joint disorder, a broken hip, mental health issues, or dementia are associated with the greatest probabilities of having difficulties in both ADLs and IADLs. We supplement our censored JSTAR data (truncated at 77) using a simulated cohort in order to include “respondents” aged 80 to 100. The disability transition matrices are presented in Appendix Table 5.
Our conditional mortality estimates show that cancer is linked to the highest annual mortality rates for both men and women, followed by cerebrovascular disease/stroke and heart disease. “Other” diseases, osteoporosis, and eye disease had the lowest annual mortality rates. In addition, the predicted disease-specific mortality rates closely followed the rates observed in the vital statistics.
We also include in the Technical Appendix predictions of Japan’s future disease prevalence from our health transition models.
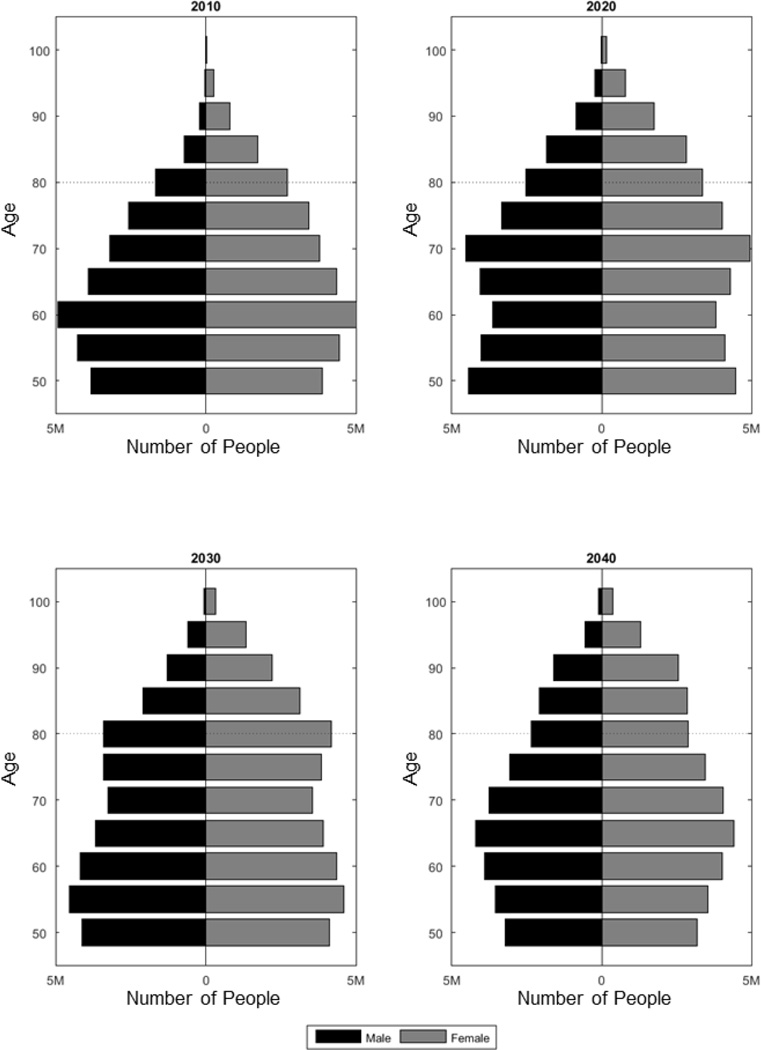
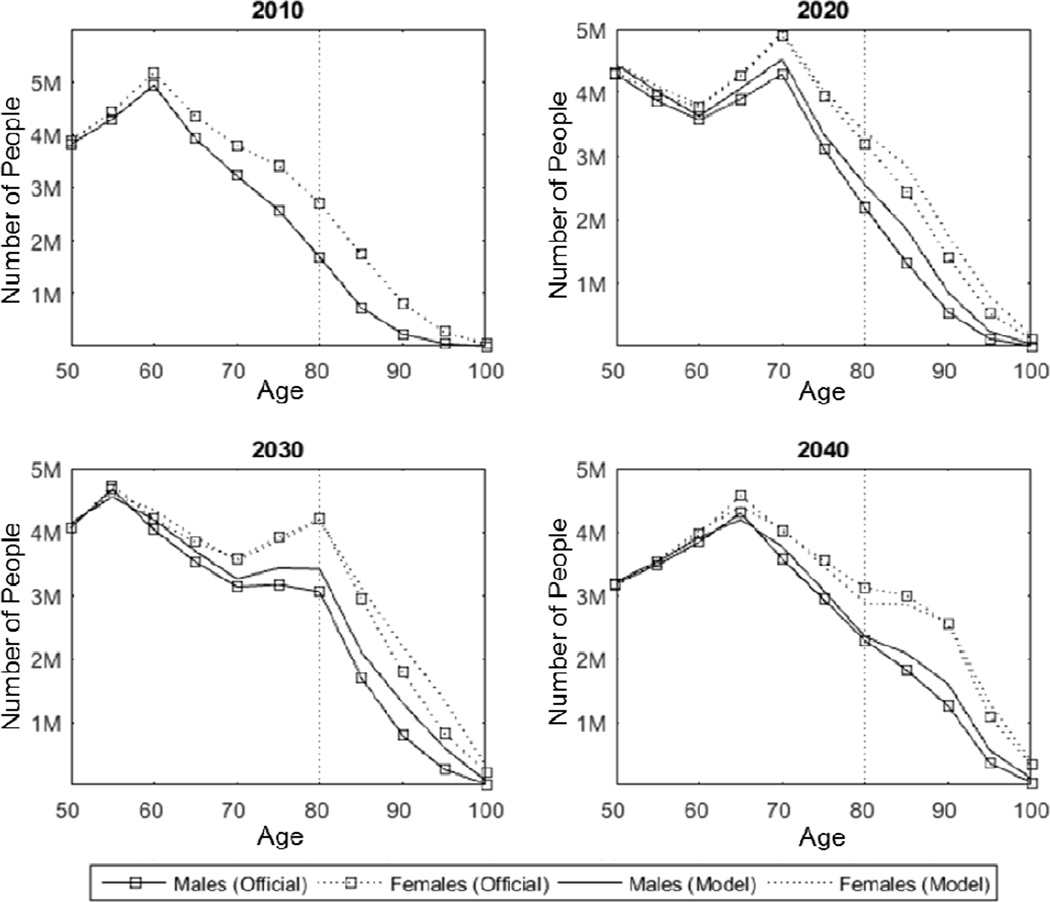
5.2 Population Simulation Model Results
Putting all the pieces together, the Japan FEM can estimate the health status and functioning of Japan’s 50+ population into the future. Figure 1 shows the simulated population pyramids for Japanese age 50 and older from 2014 through 2040. We see significant population aging within the over-50 population, combined with overall population decline: a pyramid with a large “base” of 50- and 60-year olds in 2014, and clearly showing the large post-war baby boom, evolves into a more rectangular shape by 2040, with a smaller base, an echo of the baby boom, and larger proportion of oldest-old, especially among women. Figure 2 compares the FEM estimated population to official Japanese governmental projections from the National Institute of Population and Social Security Research (IPSS 2012). Overall, the model matches the official projections quite well.
Figure 1.
Projected population pyramid for Japanese 50+ population, 2014–2040
Figure 2.
Comparing the FEM Estimated Population to Official Projections, 2010–2040
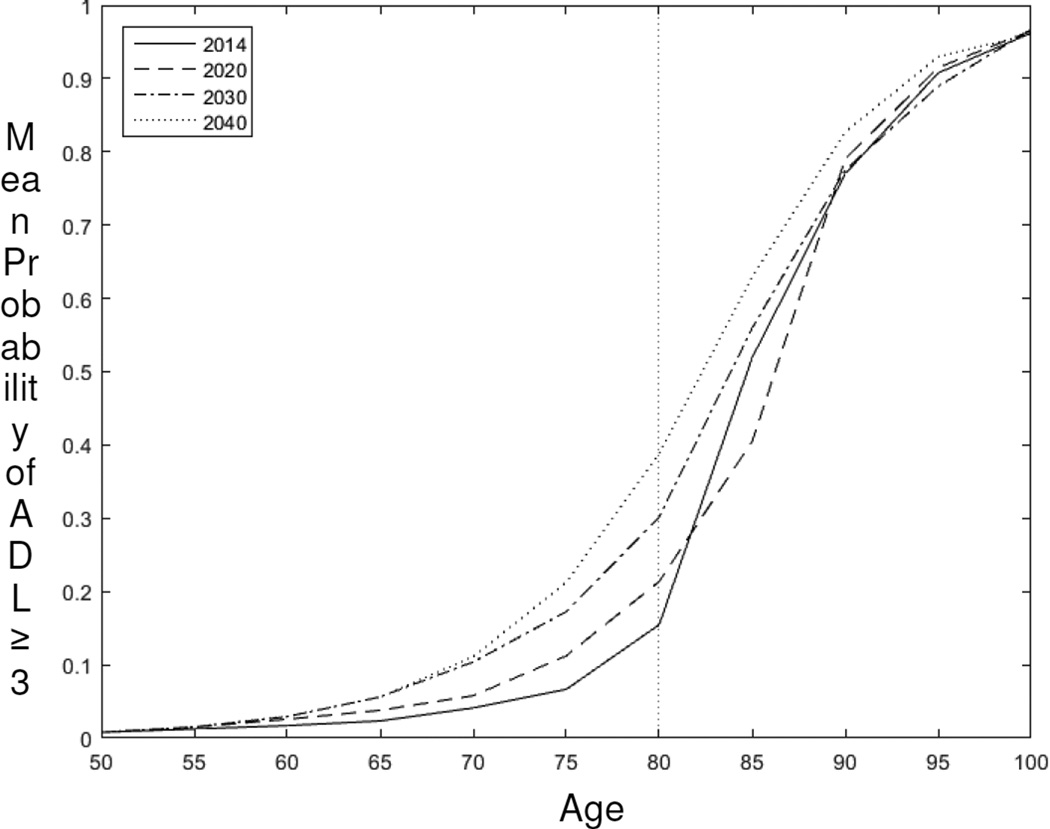
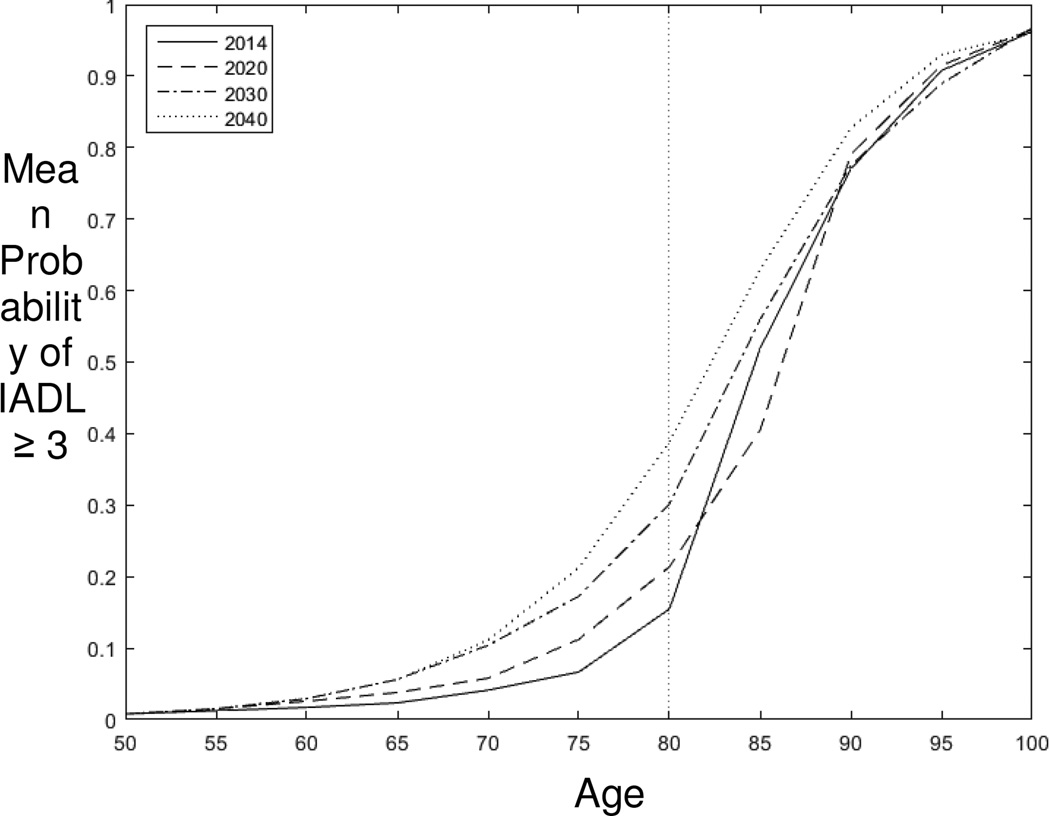
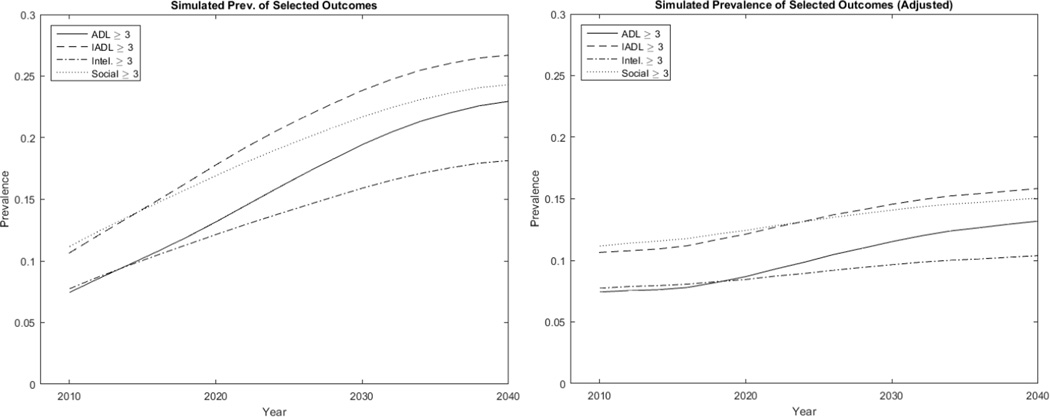
Our projections portend rising disability among the elderly in Japan. Using our 4 measures of disability, we project how the population with 3 or more disabilities will evolve over the 2014–2040 period. As shown in Figure 3, the prevalence of difficulty with 3 or more ADLs increases sharply with age, with only moderate changes in the age pattern of disability by simulation year. Similar patterns arise for IADLs (Figure 4) as well as for cognitive/intellectual disabilities and social functioning disabilities (not shown). Therefore, the prevalence of disabilities among the future elderly (Figure 5a) is largely driven by the evolution of the age structure among the 50+ population towards a greater proportion of oldest-old with a larger share of disability, although holding the age distribution constant at the 2010 age distribution reveals that a modest future increase in disability at given age (Figure 5b).
Figure 3.
Predicted Prevalence of 3 or more Difficulties with ADLs by Age, 2014–2040
Figure 4.
Predicted Prevalence of 3 or more Difficulties with IADLs by Age, 2014–2040
Figure 5.
Estimated Average Population Prevalence of Three or More Disabilities: ADLs, IADLs, Intellectual/Cognitive, or Social Disabilities, 2010–2040, (a) Unadjusted and (b) Holding Age Constant at 2010 Levels
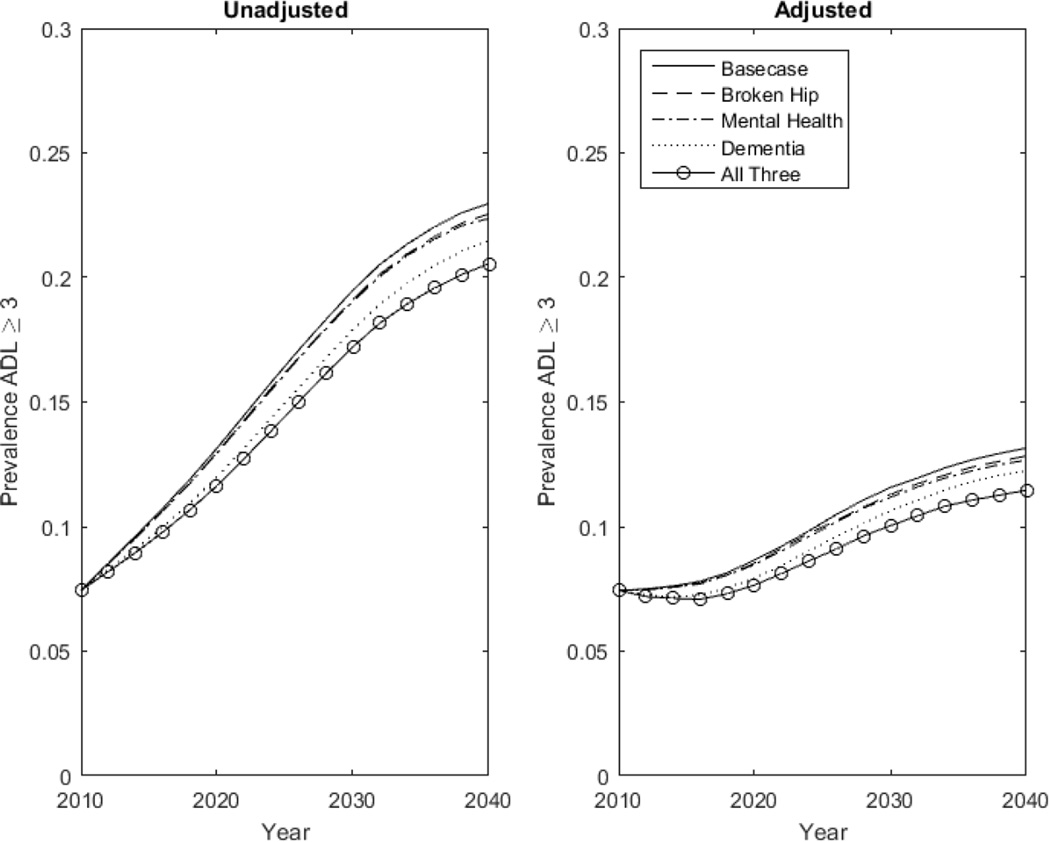
Additional counterfactual simulations further highlight the effect of aging on Japan’s future disability burden, and the limited role that primary prevention plays in reducing this burden. By primary prevention, we mean efforts to reduce the probability of transitioning into a disease state from one period to the next. This goal may be achieved, for example, by new medical technology or pharmacological therapeutics that lower the onset of dementia, or by measures to prevent falls and accidents. In Figures 6a and 6b, we show the impact of primary prevention efforts on the prevalence of having difficulty in three or more ADLs, respectively unadjusted and adjusted for age and sex. In Figure 6a, the baseline case represents future disability burden if the probabilities of transitioning into our 19 mutually exclusive comorbid conditions remain unchanged. The lines other than the base case scenario represent what would happen to Japan’s future disability burden if we halved the probability of disease transition respectively for broken hip, mental health disorder, dementia, or all three of the medical conditions.
Figure 6.
a and b. Simulated Population Prevalence of Having Three or More Disabilities Given Primary Prevention Measures That Halve the Incidence of Hip Fracture, Mental Disorder, Dementia, or All Three Conditions, Unadjusted (6a) and Adjusted (6b) for Age and Sex
Unsurprisingly, halving the transition probabilities of all three disability-associated comorbid conditions has a greater effect on reducing Japan’s future prevalence of disability than reducing the incidence any single one of these three medical conditions. However, if we were to focus on primary prevention on a single medical condition, the figure shows that halving the onset of dementia would have a greater effect of reducing disability burden than reducing the probability of either hip fractures or other mental health disorders alone.
As Figure 6b demonstrates, however, the potential effect on disability of primary prevention pales in comparison with the effect of aging. In every scenario, simply holding Japan’s age and sex structure constant at 2010 levels predicts a much lower future disability burden. The prevalence of having difficulty with three or more ADLs would increase over 5% to approximately 13% by 2040 without any primary prevention (solid line, Figure 6b) if Japan’s 2040 age and sex structure remains the same as in 2010. By contrast, in the presence of population aging, the prevalence of difficulty with three or more ADLs would increase approximately 12% to approximately 20% by 2040 (solid line with circle, Figure 6a) even if medical technology or public health measures reduce the probability of having hip fracture, mental health disorder, and dementia by half.
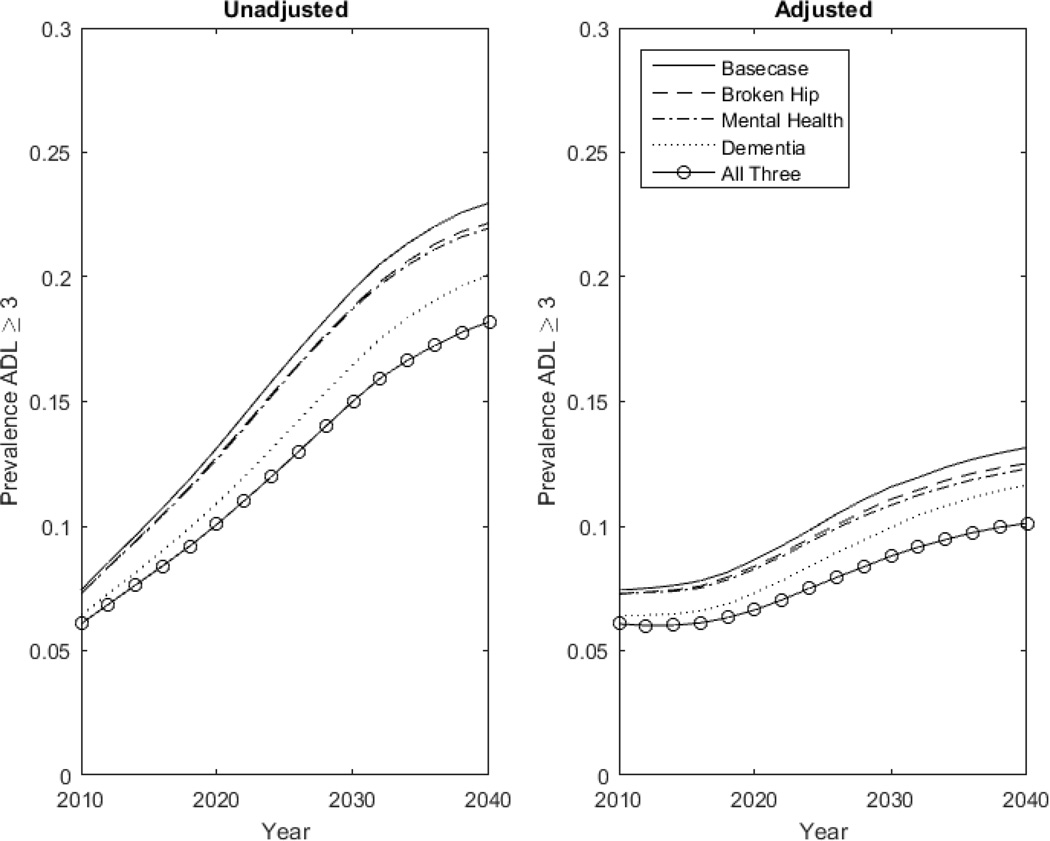
In Figures 7a and 7b, we present, respectively, the unadjusted and adjusted simulated future disability burden in Japan if secondary prevention measures reduce the probability of disability by 50% given the presence of disease. In other words, instead of preventing the onset of disease, we focus on policies or technologies such as robotic assistance for the elderly with a fractured hip that weaken the association between disease and disability. As the figures show, again the effect of aging overwhelms the potential disability reduction achievable through secondary prevention. In fact, both primary and secondary measures that respectively reduce by 50% the probability of disease onset and the probability of disability given a disease yield similar results. However, secondary prevention reduces the prevalence of disability burden slightly more than primary prevention. Secondary prevention measures also take immediate effect (shown by the immediate separation of the lines in Figures 7a and 7b), whereas primary prevention requires a time lag for a reduction in future disease onset (demonstrated by the gradual separation of the lines in Figures 6a and 6b).
Figure 7.
a and b. Simulated Population Prevalence of Having Three or More Disabilities Given Secondary Prevention Measures That Halve the Probability of Disability in the Presence of Hip Fracture, Mental Disorder, Dementia, or All Three Conditions, Unadjusted (7a) and Adjusted (7b) for Age and Sex
6. Discussion and Conclusion
Our FEM simulation suggests that by 2040, over 27 percent of Japan’s elderly will exhibit 3 or more limitations in IADLs and social functioning; almost one in 4 will experience difficulties with 3 or more ADLs; and approximately one in 5 will suffer limitations in cognitive or intellectual functioning. These projections suggest a disturbingly high future burden of disability in Japan. Since the majority of the increase in disability arises from a shift to a more elderly population, prevention efforts that reduce the underlying comorbidities may have only a limited impact on reducing the overall prevalence of disability among Japanese elderly.
Our simulations show a modest increase in disability burden in the future even when we hold Japan’s future population age and sex structure at 2010 levels. This result contrasts with findings from other FEM models, and particularly the U.S. model, which predict that disability rates will remain flat after adjusting for age and sex. Our results are likely driven by an increasing prevalence of disability-associated morbidities in Japan’s future population, a possible scenario given a trend toward greater survival with multiple comorbidities. (See Appendix Figure 9). In fact, our simulations show that disability associated morbidities (e.g., joint, broken hip, osteoporosis, mental health & dementia) are increasing, a projection which is in line with greater survival with increased morbidity (See Appendix Figure 11).
There are at least two potential factors that could moderate the projected increases in age-specific morbidities and disability that we project: first, given secular increases in educational attainment in Japan, future cohorts of Japanese age 50 and older will have higher average educational attainment than the current elderly population, suggesting they may be healthier at a given age than is captured in our projections. Second, if there are any secular trends leading the compression of morbidity among incoming cohorts of 50-year olds (such as fewer smokers or lower mortality risk for a given vector of co-morbidities because of healthier conditions in childhood), then the future age- and sex- specific prevalence of morbidities may be over-estimated.
Caution is warranted in comparing these Japanese projected disability rates to those for other countries, since measuring disability comparably across countries is difficult even for international surveys explicitly crafted for comparability like JSTAR, HRS, SHARE, and ELSA. Differential item response analyses suggest that summary indexes (counts of ADL and IADL limitations) likely underestimate mean percentage of population with disability in these international populations (Chan, Kasper et al. 2012). Nevertheless, comparisons can be useful for framing the policy debates and understanding the challenges Japan faces as a super-aging society, including the sustainability of Japan’s social programs supporting the elderly, from disability and pensions to health insurance and long-term care insurance.
In the first wave of JSTAR, about 1.3% of the sample (aged 47–77) answered that they were receiving a disability pension at the time of the interview; in the second wave, that number was 1.2% (aged 52–78 (Shimizutani, Fujii et al. 2014)). As shown by Coile, Milligan, and Wise (2014), the share of the population receiving disability benefits at older ages varies substantially across countries (likely due to different eligibility criteria), and is among the lowest in Japan. Their international collaborative research project also demonstrates that international comparisons of disability status are feasible, although Japan’s measures from the JSTAR should be interpreted with caution. Analysis of a health index developed by Poterba, Venti, and Wise (1996) – the first principal component of 25 indicators that are common to the HRS and to all of the SHARE countries, with overlap in the JSTAR – revealed that the weights across countries were strikingly consistent among all the countries, except for Japan. Nevertheless, in general, the correlations between Japan and the other countries are between 0.88 and 0.93 (Coile, Milligan et al. 2014), suggesting comparability if interpreted with appropriate caution.
According to the National Research Council report “Aging and the Macroeconomy: Long-Term Implications of an Older Population” (Institute of Medicine (US) Committee on the Long-Run Macroeconomic Effects of the Aging US Population 2012), compression of morbidity suggests that older individuals will be active longer. Indeed, self-reported health of 60-year-old men in the 1970s was about the same as for 69-year-olds in the 2000s (NRC 2012:90). The expert committee developed projections of labor supply through 2050, concluding that there would be “very little change in the proportion of the population age 20–74 that could hypothetically supply labor between 2010 and 2050. Individual decisions and public policies may lead to a flat age at retirement in coming decades, but this will not be dictated by health and biology” (Lee 2014). It is far less clear that such a sanguine forecast could be made for Japan, given the projections of health and disability. For example, (Hashimoto, Kawado et al. 2010) estimate that between 1995 and 2004, duration of life with a light or moderate disability increased for both men and women in Japan. Our simulation suggests a substantial further increase as the proportion of the oldest old continues to increase in Japan.
The development of a Future Elderly Model (FEM) for Japan contributes to the literature in a variety of ways. First, such a model has never been estimated for Japan, even though Japan’s population aging is far more significant than for the US and most other OECD countries. Second, arguably the need for such a model is especially great for Japan since its health system already features many components—such as universal coverage with strict payment regulation—that limit the ability to further reduce spending growth associated with population aging. The model provides a foundation for future simulations of policies to improve the fiscal sustainability of Japan’s health care programs in light of its super-aging population. The FEM can also generate projections of how a wide range of health policies, programs, technologies, and services will influence the morbidity, mortality, health spending, long term care use, retirement, labor supply, and earnings of older populations.
Supplementary Material
Acknowledgments
This study uses data from the Japanese Study on Aging and Retirement (JSTAR), which was conducted by the Research Institute of Economy, Trade, and Industry (RIETI) and Hitotsubashi University in 2007 and 2009. We thank the JSTAR team for providing access to the data. We also thank the Freeman Spogli Institute for International Studies Japan Fund, the Stanford Center on the Demography and Economics of Health and Aging, and the National Institute on Aging (AG017253) for financial support for this research. Dr. Bhattacharya is grateful for support from the National Institute on Aging for his work on this project (P30 AG017253, R37AG036791 and P01AG05842).
We would also like to thank Michelle Zhao for excellent research assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
http://www.soumu.go.jp/johotsusintokei/whitepaper/ja/h25/html/nc123110.html. Japan overtook Italy and Germany to have the highest proportion of elderly adults in 2008.
Types of preventive services include home-visit care, outpatient rehabilitation service, and short-term stay at a care facility. Types of care services include in-home services such as home help service and day care, and facility services such as intensive care home, long-term care health facilities, and sanatorium-type care facilities, and community-based services such as home-visit at night, day care for dementia patients, and small-sized multifunctional in-home care (http://www.ipss.go.jp/s-info/e/ssj2014/PDF/ssj2014.pdf, p. 34)
Crude mortality is increasing in Japan, while age-adjusted mortality has been relatively constant or decreasing since the late1990s, suggesting that population aging is the main driver of increased number of cancer deaths. http://ganjoho.jp/data/professional/statistics/backnumber/2013/fig14.pdf
The 2015 World Population Prospects reports that globally Japan has the highest median age (46.5 in 2015 [Table S.7, p.32]) and the lowest Potential Support Ratio (PSR) -- the number of people aged 20 to 64 divided by the number of people aged 65 and over (p.7, http://esa.un.org/unpd/wpp/publications/files/key_findings_wpp_2015.pdf). In addition, the 2015 World Population Prospects Key Findings and Advance Tables document compiled by the United Nations Department of Economic and Social Affairs, Table S.5. Countries Whose Population Is Projected to Decrease Between 2015 and 2020, shows that Japan is ranked 11th, behind only one other OECD country, Hungary, which is ranked 10th (http://www.oecd.org/about/membersandpartners/list-oecd-member-countries.htm). http://esa.un.org/unpd/wpp/publications/files/key_findings_wpp_2015.pdf.
References
- Aisa R, Pueyo F, Sanso M. Life expectancy and labor supply of the elderly. Journal of Population Economics. 2012;25(2):545–568. [Google Scholar]
- Bech M, Christiansen T, Khoman E, Lauridsen J, Weale M. Ageing and health care expenditure in EU-15. The European Journal of Health Economics. 2011;12(5):469–478. doi: 10.1007/s10198-010-0260-4. [DOI] [PubMed] [Google Scholar]
- Behrman JR, Parker SW. Is Health of the Aging Improved by Conditional Cash Transfer Programs? Evidence From Mexico. Demography. 2013;50(4):1363–1386. doi: 10.1007/s13524-013-0199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom DE, Canning D, Graham B. Longevity and Life-cycle Savings*. The Scandinavian Journal of Economics. 2003;105(3):319–338. [Google Scholar]
- Campbell JC, Ikegami N. Long-term care insurance comes to Japan. Health Affairs. 2000;19(3):26–39. doi: 10.1377/hlthaff.19.3.26. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Ikegami N, Gibson MJ. Lessons from public long-term care insurance in Germany and Japan. Health Affairs. 2010;29(1):87–95. doi: 10.1377/hlthaff.2009.0548. [DOI] [PubMed] [Google Scholar]
- Chan KS, Kasper JD, Brandt J, Pezzin LE. Measurement equivalence in ADL and IADL difficulty across international surveys of aging: findings from the HRS, SHARE, and ELSA. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2012;67(1):121–132. doi: 10.1093/geronb/gbr133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coile C, Milligan KS, Wise DA. Social Security Programs and Retirement Around the World: Disability Insurance Programs and Retirement-Introduction and Summary. National Bureau of Economic Research Working Paper 20120. 2014 [Google Scholar]
- Coleman D, Rowthorn R. Who's afraid of population decline? A critical examination of its consequences. PoPulation and develoPment review. 2011;37(s1):217–248. doi: 10.1111/j.1728-4457.2011.00385.x. [DOI] [PubMed] [Google Scholar]
- Cullinan J, Gannon B, O’Shea E. The welfare implications of disability for older people in Ireland. The European Journal of Health Economics. 2013;14(2):171–183. doi: 10.1007/s10198-011-0357-4. [DOI] [PubMed] [Google Scholar]
- Dow WH, Philipson TJ, Sala-i-Martin X. Longevity complementarities under competing risks. American Economic Review. 1999:1358–1371. [Google Scholar]
- Finkelstein A, Poterba J. Adverse selection in insurance markets: Policyholder evidence from the UK annuity market. Journal of Political Economy. 2004;112(1):183–208. [Google Scholar]
- Foundation for Promotion of Cancer Research. Trends in Age-adjusted in Mortality Rate (1958–2012) 2013;2015 [Google Scholar]
- Fukawa T. Health and long-term care expenditures of the elderly in Japan using a micro-simulation model. The Japanese Journal of Social Security Policy. 2007;6(2):199–206. [Google Scholar]
- Gannon B, Davin B. Use of formal and informal care services among older people in Ireland and France. The European Journal of Health Economics. 2010;11(5):499–511. doi: 10.1007/s10198-010-0247-1. [DOI] [PubMed] [Google Scholar]
- Gender Equality Bureau, Cabinet Office. A special summary of Comprehensive Survey of Living Conditions (Kokumin seikatsu kiso chosa tokubetsu shukei zantei kekka) 2008 [Google Scholar]
- Gerdtham U-G, Lundin D, Sáez-Martí M. The ageing of society, health services provision and taxes. Journal of population economics. 2005;18(3):519–537. [Google Scholar]
- Goldman DP, Shang B, Bhattacharya J, Garber AM, Hurd M, Joyce GF, Lakdawalla DN, Panis C, Shekelle PG. Consequences of health trends and medical innovation for the future elderly. Health Affairs. 2005;24:W5. doi: 10.1377/hlthaff.w5.r5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J, Hoorens S, Sivadasan S, van het Loo M, DaVanzo J. Low fertility and population ageing: causes consequences and policy options. 2004 [Google Scholar]
- Hashimoto S, Kawado M, Seko R, Murakami Y, Hayashi M, Kato M, Noda T, Ojima T, Nagai M, Tsuji I. Trends in disability-free life expectancy in Japan, 1995–2004. Journal of Epidemiology. 2010;20(4):308–312. doi: 10.2188/jea.JE20090190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser RM, Weir D. Recent developments in longitudinal studies of aging in the United States. Demography. 2010;47(1):S111–S130. doi: 10.1353/dem.2010.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshi T, Ito T. Defying gravity: can Japanese sovereign debt continue to increase without a crisis? Economic Policy. 2014;29(77):5–44. [Google Scholar]
- Ichimura H, Shimizutani S, Hashimoto H. JSTAR First Results 2009 Report, Research Institute of Economy, Trade and Industry (RIETI) 2009 [Google Scholar]
- Imrohoroğlu S, Kitao S. Social security reforms: benefit claiming, labor force participation, and long-run sustainability. American Economic Journal: Macroeconomics. 2012;4(3):96–127. [Google Scholar]
- Index Mundi. Japan Demographics Profile 2011. [Retrieved November 18, 2014];2011 from http://www.indexmundi.com/japan/demographics_profile.html. [Google Scholar]
- Institute of Medicine (US) Committee on the Long-Run Macroeconomic Effects of the Aging US Population. Aging and the Macroeconomy: Long-Term Implications of an Older Population. IPSS (2012). Population Projections for Japan: 2011–2060. National Institute of Population and Social Security Research. 2012 [Google Scholar]
- Jalal H, Eggleston K, Chen B, Hashimoto H, Schoemaker L, Suen S-C, Bhattacharya J. A Microsimulation of the Aging Japanese Population. 2015 [Google Scholar]
- Kapteyn A. What can we learn from (and about) global aging? Demography. 2010;47(1):S191–S209. doi: 10.1353/dem.2010.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keys A, Menotti A, Aravanis C, Blackburn H, Djordevič BS, Buzina R, Dontas A, Fidanza F, Karvonen MJ, Kimura N. The seven countries study: 2,289 deaths in 15 years. Preventive medicine. 1984;13(2):141–154. doi: 10.1016/0091-7435(84)90047-1. [DOI] [PubMed] [Google Scholar]
- Lee R, Skinner J. Will aging baby boomers bust the Federal budget? The Journal of Economic Perspectives. 1999:117–140. [Google Scholar]
- Lee RD. Macroeconomic Consequences of Population Aging in the United States: Overview of a National Academy Report. The American Economic Review. 2014;104(5):234–239. [Google Scholar]
- Manton KG, Stallard E, Corder L. Economic effects of reducing disability. American Economic Review. 1998:101–105. [Google Scholar]
- Martínez MJS, Marín RG. Aging and Demographic Weakness in the European Union: The Spanish Model. Population Review. 2014;53(2) [Google Scholar]
- Ministry of Internal Affairs and Communications. White Paper on the Infornation and Communications in Japan in 2013 (Joho Tsushin Hakusho) 2013 [Google Scholar]
- Miyazawa K, Moudoukoutas P, Yagi T. Is public long-term care insurance necessary? Journal of Risk and Insurance. 2000:249–264. [Google Scholar]
- National Institute of Popoulation and Social Security Research. Population Projections for Japan (January 2012): Medium-Variant Fertility and Mortality Projections. 2012 [Google Scholar]
- OECD. Society at a Glance 2006: OECD Social Indicators. OECD Publishing; 2007. Age-Dependency Ratios; pp. 42–43. [Google Scholar]
- OECD. Health at a Glance 2013: OECD Indicators, OECD Publishing. 2013 [Google Scholar]
- Ogawa N, Mason A, Maliki RM, Nemoto K. Population aging and health care spending in Japan: Public-and private-sector responses. In: Clark RL, Ogawa N, Tason A, editors. Population Aging, Intergenerational Transfers and the Macroeconomy. Northampton, MA, USA: Edward Elgar Publishing Inc.; 2007. pp. 192–223. [Google Scholar]
- Ogawa N, Retherford RD, Saito Y. Ageing in Advanced Industrial States. Springer; 2010. Care of the elderly and women’s labour force participation in Japan; pp. 223–261. [Google Scholar]
- Oshio T, Shimizutani S, Oishi AS. Social Security Programs and Retirement around the World: The Relationship to Youth Employment. University of Chicago Press; 2010. Does social security induce withdrawal of the old from the labor force and create jobs for the young? The case of Japan; pp. 217–241. [Google Scholar]
- Philipson TJ, Becker GS. Old-age longevity and mortality-contingent claims. Journal of Political Economy. 1998;106(3):551–573. [Google Scholar]
- Poterba JM. Retirement Security in an Aging Population. The American Economic Review. 2014;104(5):1–30. [Google Scholar]
- Poterba JM, Venti SF, Wise DA. How retirement saving programs increase saving. The Journal of Economic Perspectives. 1996:91–112. [Google Scholar]
- Prettner K, Canning D. Increasing life expectancy and optimal retirement: does population aging necessarily undermine economic prosperity? No.9112. Program on the Global Demography of Aging. 2012 [Google Scholar]
- Schieber SJ. Demography and the Economy. University of Chicago Press; 2010. Aging Populations, Pension Operations, Potential Economic Disappointment and Its Allocation; pp. 293–325. [Google Scholar]
- Schoeni RF, Ofstedal MB. Key themes in research on the demography of aging. Demography. 2010;47(1):S5–S15. doi: 10.1353/dem.2010.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizutani S. The future of long-term care in Japan. Asia-Pacific Review. 2014;21(1):88–119. [Google Scholar]
- Shimizutani S, Fujii M, Oshio T. Social Security Programs and Retirement Around the World: Disability Insurance Programs and Retirement. University of Chicago Press; 2014. Option Value of Work, Health Status, and Retirement Decisions in Japan: Evidence from the Japanese Study on Aging and Retirement (JSTAR) [Google Scholar]
- Singh Y. Applied Demography and Public Health. Springer; 2013. Population Aging and Health Expenditure in Kerala: An Empirical Analysis; pp. 61–75. [Google Scholar]
- Statistics Bureau, Ministry of Internal Affairs and Communications. Result of the Population Estimates, Monthly Report in August 1, 2014 (Final estimates), January 1, 2015 (Provisional estimates) 2015 [Google Scholar]
- Statistics Bureau, Ministry of Internal Affairs and Communications, Death Rates by Causes of Death. [accessed October 12, 2015]; available at http://www.stat.go.jp/english/data/nenkan/1431-21.htm. [Google Scholar]
- Statistics Bureau, Ministry of Internal Affairs and Communications. 2010 Population Census of Japan. Ministry of Internal Affairs and Communications. [accessed October 12, 2015];2010 available at http://www.stat.go.jp/english/data/kokusei/ [Google Scholar]
- Statistics Bureau, Ministry of Internal Affairs and Communications. Population and Households of Japan (Final Report of the 2010 Population Census) 2010 [Google Scholar]
- Suzman R. Prologue: Research on the demography and economics of aging. Demography. 2010;47:S1–S4. doi: 10.1353/dem.2010.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamiya N, Noguchi H, Nishi A, Reich MR, Ikegami N, Hashimoto H, Shibuya K, Kawachi I, Campbell JC. Population ageing and wellbeing: lessons from Japan's long-term care insurance policy. The Lancet. 2011;378(9797):1183–1192. doi: 10.1016/S0140-6736(11)61176-8. [DOI] [PubMed] [Google Scholar]
- Venti SF. Demography and the Economy. University of Chicago Press; 2010. Comment on" Aging Populations, Pension Operations, Potential Economic Disappointment and Its Allocation; pp. 326–331. [Google Scholar]
- Yashin A, Akushevich I, Arbeev K, Kulminski A, Ukraintseva S. Applied Demography and Public Health. Springer; 2013. Methodological Aspects of Studying Human Aging, Health, and Mortality; pp. 337–355. [Google Scholar]
- Zheng H. Aging in the context of cohort evolution and mortality selection. Demography. 2014;51(4):1295–1317. doi: 10.1007/s13524-014-0306-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.