Abstract
Background
The current evidence suggests that rotational stability in not restored in patients with anterior cruciate ligament (ACL) ruptures, despite reconstructive surgery. The graded pivot-shift is a useful clinical test to delineate extent of ligamentous laxity within the knee. Given its lateralised position, we hypothesized that reconstruction of the anterolateral ligament (ALL) would provide restraint to excessive internal rotation, restoring rotational stability.
Methods
10 patients with MRI confirmed diagnosis of an isolated ACL rupture were included. Patients assigned a grade-3 pivot-shift underwent dual-ligament reconstruction for the ACL and ALL (Group 2), whilst patients with an absent pivot-shift, grade-1 or grade-2 underwent single ligament reconstruction for just the ACL (Group 1). Total range of rotation (TRR) was measured using a 3D-kinematic system at 30°,60°and 90° of knee flexion. Data was collected on the pathology-free contralateral normal knee (CNK), ACL-deficient knee (ADK) and the ACL-reconstructed knee (ARK).
Results
A statistically significant pre-operative difference in TRR between the CNK and ADK was noted between Group 1 and 2 (4.04° vs. 1.53°; p < 0.05). Postoperatively, both groups achieved a TRR that was either equivalent, or surpassed values that were observed on the CNKs. The absolute and percentage reduction in TRR at 30° of knee flexion was significantly higher in Group-2 compared to Group-1 (−8.15° vs. −2.96°; p < 0.001) and (28.04% vs. 13.31%; p < 0.001) respectively.
Conclusion
Our findings are based primarily in anaesthetized patients, with kinematic values at time-zero postoperatively. Patients presenting with significant rotational instability following a primary ACL injury and assessed to have a grade-3 pivot-shift may benefit from dual-ligament reconstruction. Further research is required to assess long-term patient-centered clinical outcomes.
Keywords: Anterolateral ligament, Anterior cruciate ligament, Rotational stability
Highlights
-
•
To prevent excessive rotation in the knee, a structure needs to be present away from the centre axis; at the edge of a plane, resisting rotational motion.
-
•
The graded pivot-shift is a useful clinical test to help delineate extent of ligamentous laxity within the knee.
-
•
The higher the grade of the pivot-shift in the ACL deficient knee, the greater the TRR present.
-
•
The ALL plays a significant role in ACL deficient knees with a grade-3 pivot shift, restoring TRR at time-zero.
-
•
Further research is required assessing long-term patient-centered clinical outcomes.
1. Introduction
The discovery of the anterolateral ligament (ALL) within the confines of the human knee is undoubtedly enthralling. Its roots date back to 1879 when Dr. Paul Segond, a French surgeon, described a ‘pearly, resistant, fibrous band’ at the anterolateral aspect of the human knee that demonstrated ‘extreme amounts of tension’ during forced internal rotation of the knee. He further described an avulsion fracture pattern that occurred as a result of excessive forced internal rotation occurring ‘above and behind the tubercle of Gerdy’ - the eponymous ‘Segond fracture’ [1]. Further researchers have hypothesized and proved that avulsion fractures of the lateral tibial plateau can be regarded as a strong indication for the presence of an ACL injury [2], [3], [4].
Over time, this ‘pearly band’ has been neglected from anatomical descriptions and scarce information remains of its existence. It wasn't until the last decade that various authors have described synonymous structures in the same anatomical position. Its' descriptive name has varied from the ‘capsulo-osseous layers’ of the iliotibial band [5], the ‘mid-third lateral capsular ligament’ [6], the ‘anterior oblique ligament’ [7] or the ‘anterolateral ligament’ [8], [9]. Although some variability does indeed exist, all authors appear to be referring to the same anatomical structure, which we will refer to as the anterolateral ligament.
The purpose of an ACL reconstruction is to restore the function of the ligament, with a primary focus to restore the static anterior-posterior translation. However, despite a working theory that the native ACL constrains anterior-posterior (AP) translation, but also tibial internal-external rotation, kinematic studies of the reconstructed knees have demonstrated abnormal rotational motion when compared to the contralateral knee or healthy control knees [10], [11].
Anatomical studies by Claes et al. [12] and Dodds et al. [13] showed that the ALL was a clearly defined structure in 40 out of 41 and 33 out of 40 cadaveric specimens respectively. Its proximal attachment was situated at the prominence of the lateral femoral epicondyle, anterior to the origin of the lateral collateral ligament (LCL). Further, anatomical dissection carried out by Dodds et al. noted that the proximal attachment of the ALL was posterior to both the LCL attachment and the lateral epicondyle, rather than on the lateral epicondyle. The insertion point was located approximately half way between Gerdy's tubercle and the tip of the fibular head. They also noted that the ALL had a ‘firm attachment’ to the periphery of the middle third of the body of the lateral meniscus.
Given its anatomical orientation, the ALL was hypothesized to provide functional stabilisation during internal rotation of the knee. Therefore, the aim of this study was to investigate 2 surgical techniques utilising single or dual ligament reconstruction to restore rotational stability. Additionally, the anatomical position of the ALL coincides with the bony avulsion that occurs during a Segond fracture and this could help delineate its role in providing rotational stability to ACL-deficient knees.
1.1. Rotational instability
Symptomatic instability is common following an ACL rupture. Patients with rotational knee instability often report repeated episodes of the knee ‘giving way’ or buckling during the stance phase of the gait, pivoting or twisting movements. Unpredictable giving way of the knee without provocation has also been reported [14]. Occasionally, patients may present with joint line tenderness with associated swelling injured structures that provided rotational stability to the knee. With chronic cases, patients often complain of difficulty running on uneven surfaces. Patients with a confirmed diagnosis of a partial or complete ACL rupture should ideally undergo a tailored exercise rehabilitation programme that's aims to strengthen the muscles surrounding the knee complex. This is aimed at compensatory stability for the ruptured ACL. In the event of a failed rehabilitation programme, and a clinically symptomatic patient, surgical treatment is usually offered. In another subset of patients e.g. athletes involved in agility sports where loading, pivoting and running are integrated into their daily lives, surgical reconstruction is usually advised to safely return to sport [15]. Non-surgical treatment is an acceptable and appropriate treatment modality for patients who are clinically asymptomatic, less active or do not participate in activities that require running, jumping or a pivoting motion.
Several clinical tests have been proposed to assess rotational instability with variable sensitivities and specificities. Symptomatic excessive rotation (internal or external) in comparison to the contralateral ‘normal’ knee would therefore correlate with a diagnosis of rotational instability. These include tests such as passive rotation of the tibia at 30°, 60° and 90° of knee flexion, the external rotation recurvatum test or the dial test. The reverse pivot shift test is sometimes used to evaluate posterolateral rotational instability, with a significant positive result suggesting PCL, LCL and arcuate complex involvement.
To specifically delineate the extent of internal rotational laxity, (where we hypothesized that the ALL would play a significant role), we opted to perform the pivot shift test. This was first described by Galway, Beaupre and Macintosh [16] in 1972 and is now routine utilised in clinical practice to assess the extent of ligamentous laxity within the knee. A positive test has been shown to be a good indicator for concomitant ACL rupture. The sensitivity of the test varies from clinician to clinician depending on the examination technique, force applied and whether the patient is apprehensive or relaxed [17]. The Jakob classification [17] is a simple and reproducible method of grading the pivot shift. Based on this classification, patients with a grade 3-pivot shift were deemed to have the greatest degree of rotation laxity with involvement of both the posteromedial and posterolateral corners. Subsequent surgical considerations (single or dual ligaments) were therefore based upon outcome of this clinical test. Patients with a greater degree of rotational laxity underwent dual ligament (ACL + ALL) reconstruction whilst those with a lesser degree of rotational laxity underwent single ligament (ACL) reconstruction.
2. Materials and methods
Ethical approval - This study was performed as service evaluation of current clinical practice at the Royal Derby Hospital and was therefore registered with the Research and Development Department, without the need for formal ethical approval. All patients received an information sheet entailing the aims and objectives of the study, with a clear explanation that the study would not alter the surgical procedural decision. Following this, written consent was obtained to take part in the study.
Sample size - In the absence of any available literature that assessed knee kinematics following dual ligament reconstruction, the novelty of the study made it difficult to select an appropriate study to estimate a sample size. We therefore opted for a research study done by Tsai et al. [18] evaluating rotational knee laxity on normal knees. We assumed an 80% power with a 45% effect size on a two-sample study. Using a tibial rotation value of 25.8° and a standard deviation of 5.9° (at 30°of knee flexion), a minimum of 4 patients were required for each group.
Patient identification - Potential patients were identified during their initial presentation at the acute knee clinic at the Royal Derby Hospital and subsequently followed through the duration of the study.
Inclusion criteria - All patients included in the study had an isolated, unilateral ACL rupture that was confirmed by clinical evaluation by the operating orthopaedic surgeon, as well as radiologically, via MR imaging. Arthroscopic confirmation was also performed at the time of ACL reconstruction. Concomitant meniscal injuries were also noted in 2 patients intra-operatively; and were repaired intra-operatively.
Exclusion criteria - Patients without an MRI confirmed diagnosis of an ACL rupture were excluded from the study. In addition to the primary injury, patients identified with significant meniscal damage requiring menisectomy, posterior cruciate ligament (PCL) injury, collateral ligament (CL) injury or a posterolateral corner (PLC) injury were all excluded. This was because these additional injuries were deemed as confounding factors for rotational laxity despite the primary injury.
Measurement regime - 6 pre-operative measurements of the total range of rotation were taken with the knee in 30, 60 or 90° of flexion, with 3 measurements on the contralateral normal knee (CNK) and 3 measurements on the ACL-deficient knee (ADK). After anaesthetic induction, the ADN was examined via the pivot-shift test to estimate the extent of rotational laxity. The test was performed solely by the operating surgeon on all 10 patients, ensuring uniformity of the subsequent outcomes. Patients with an absent pivot-shift (0), grade 1 or grade 2 pivot-shift underwent a single ligament (ACL) reconstruction (Group 1) and those with a pivot-shift grade 3 underwent dual ligament (ACL + ALL) reconstruction (Group2). Following single or dual ligament reconstruction, and whilst the patients were still anaesthetized, the final set of reading were obtained i.e. 3 measurements from the ACL-reconstructed knee (ARK) (at 30°, 60° and 90° of knee flexion).
Surgical technique - To preserve uniformity, a single-bundle ACL reconstruction technique using the semi-tendinosus was used for all 10 patients. For the ALL, either the gracillis tendon was utilised (9 patients) or a graft was harvested from the iliotibial band (1 patient). The midpoint between the fibular head and Gerdy's Tubercle was used as the distal ALL insertion point while the LE was utilised for the proximal attachment. The surgical technique has been described in further detail below.
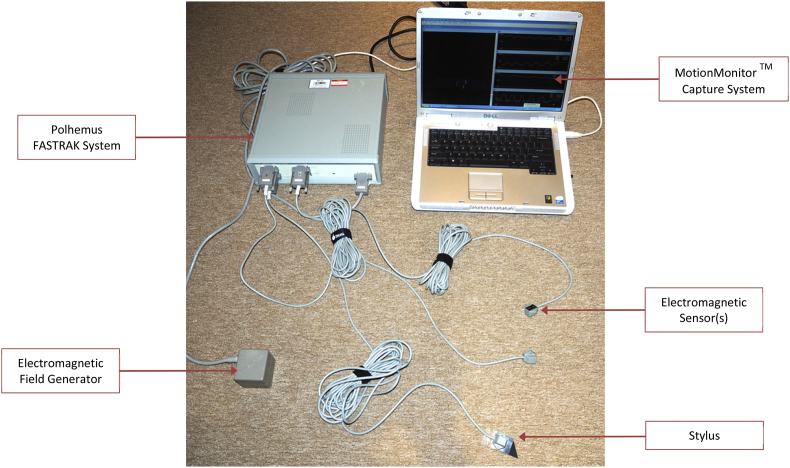
Equipment Used to Measure Rotational Laxity - Knee kinematics were recorded on all participants using the MotionMonitor™ motion capture system (Innovative Sports Training Incorporated, Chicago). The software communicates with a three-dimensional (3D) tracking device, the Polhemus FASTRAK sensor system (Polhemus incorporated, Colchester, Vermont) (Fig. 1). This is a 6 degrees-of-freedom measuring device that emits a low frequency electromagnetic field via a transmitter. Tracking sensors are detected within this magnetic field, and their position, orientation and spatial relationship is recorded simultaneously. Sensor position is delineated using the Cartesian coordinate system that specifies each point uniquely in a plane (X, Y, Z), whilst its orientation is captured using a combination of three angular quantities: azimuth, pitch and roll. Data is gathered from the tracking sensors through space, relative to the source transmitter. This can be represented as a real-time graph or numerically, as a range of movement [19]. Data is then analysed digitally using the MotionMonitor™ system. This data collection model using the MotionMonitor™ and the Polhemus FASTRAK has been previously validated [18], [20] and the accuracy of this model has been reported to be within 0.1–0.3° [21], [22]. Hagemeister et al. [23] described a repeatable, functional and postural method to define a bone-embedded anatomical frame (BAF) on the femur and tibia, and were subsequently able to create a knee joint coordinate system and thus interpret movement within the knee joint using a Cardan angle sequence based on Grood and Suntay [24]. The Grood-Suntay joint angles were analysed during knee flexion at 90°, 60°° and 30° based on the above joint coordinate system.
Fig. 1.
The MotionMonitor and Polhemus Fastrak system.
To perform each assessment, micropore surgical tape was used to secure two tracking sensors to the patient's skin. The ‘thigh’ sensor was positioned 2 cm above the base of the patella - on the quadriceps tendon, while the ‘shank’ sensor was positioned 2 cm below the anterior tibial tuberosity. Fixing the sensor in these positions helped define a bone-technical frame (BTF) that could be used to track each segment. A third sensor was configured as a stylus that was used to digitise 10 anatomical landmarks.
After establishing a BAF, the subject was asked to lay supine; and the CKN was flexed to 90°. The MotionMonitor has an inbuilt goniometer that allows real-time analysis, so that the observer can estimate the correct knee flexion angle. The femur was then fixed and in the absence of a force-moment sensor to estimate torque, continuous manual internal-external rotation was performed to an end-point feel. Readings were carried over 20 s bursts, and a total of 600 readings were obtained and extrapolated in graphical form. The entire process was repeated with the knee flexed at 60° and 30°. A third set of 3 measurements was taken on the ACL-deficient knee, however, in this case, the configuration used for the BAF was saved as ‘preference file’ on the MotionMonitor re-utilised for the final set of measurements following surgical reconstruction of the ADN.
Statistical analysis - Statistical evaluation was carried out using SPSS. Descriptive statistics were used to characterise the group samples. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to assess normality of the distribution and homogeneity of variance of other base-line variables. Based on these results, an unpaired t-test was used to assess the difference in means between the contralateral normal knee and ACL-deficient knee whilst a paired t-test was used to assess means between the ACL-deficient knee pre and post operatively. For the primary objective (investigating the change in rotation laxity between the two groups), unpaired t-tests were once again performed. Statistical significance was set as p < 0.05.
3. Surgical technique
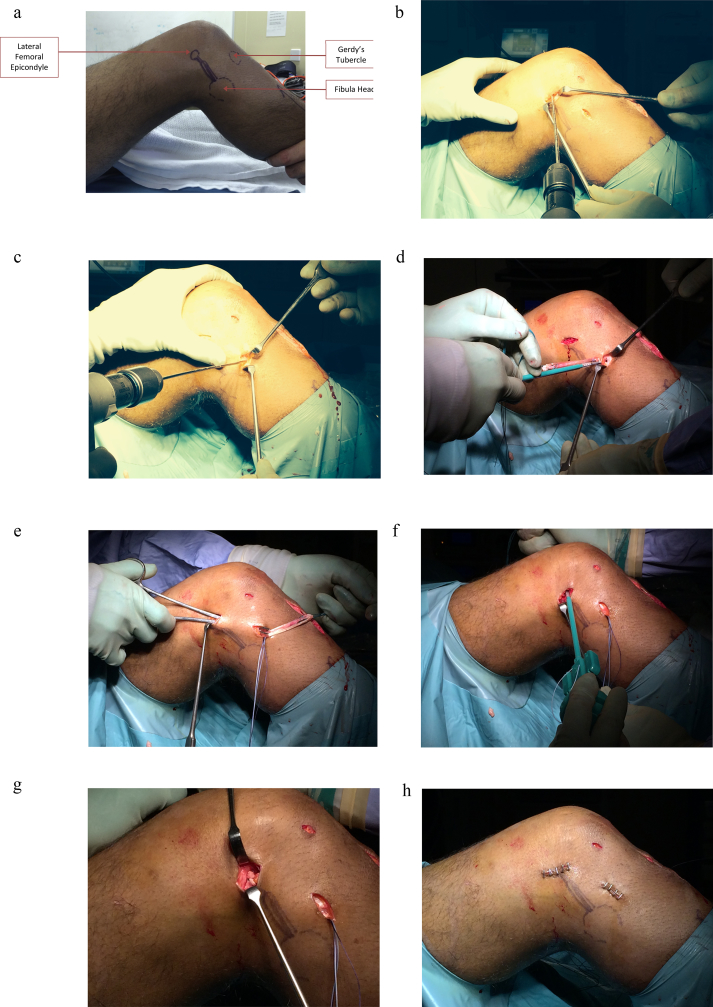
Although the surgical technique used for ACL reconstruction is indeed important, it exceeds the scope of this project. However, to preserve uniformity, a single-bundle reconstruction technique using the hamstrings was used for all 10 patients. The origin of the ALL comes from the prominence of the lateral epicondyle, just superior and anterior to the origin of the lateral collateral ligament (LCL) and proximal and posterior to the insertion point of the popliteus tendon (PT) [12]. The insertion point of the ALL was deemed to be midway between Gerdy's Tubercle and insertion of the LCL on the fibular head [12], [13]. An oblique incision was made over the pes anserinus to identify the hamstring tendons. If dual ligament reconstruction was opted for, both the semitendinosus and gracilis tendons were harvested in the standard fashion. On one occasion, the graft was harvested from the iliotibial band (ITB). For the preparation of the ALL graft, the gracilis tendon was whipstiched in the distal centimetres and cleared of tissue at the other end. Anatomical landmarks are first identified and marked - the lateral femoral epicondyle, the fibular head and Gerdy's Tubercle (GT) (Fig. 2a).
Fig. 2.
a: Anatomical landmarks. b: Preparation of femoral socket. c: Preparation of tibial socket. d: Fixation of the tibia end of the ALL graft, using the SwivelLock™. e: Tunnelling of the ALL graft under the ITB. f: Fixation of the femoral end of the ALL graft using the SwivelLock™. g: ALL graft in situ. h: skin closure with staples depicting origin and insertion landmarks.
Following this, the midpoint between the fibular head and GT is also marked to establish the ALL insertion point. The incision was made roughly ten mm below the joint line. A horizontal incision is then made over the femoral epicondyle and a 2.4 mm guide wire is inserted at the origin point of the ALL, above and superior to the LCL, and is then directed anteriorly and proximally (Fig. 2b). A 4.5 mm SwivelLock™ drill is then used, and the socket depth is made in excess of 25 mm a longitudinal incision is made over the insertion point of the ALL over the tibia and sharp dissection is carried out to bone. Once again, a 2.4 mm guide wire is used, but directed inferiorly (Fig. 2c). This is followed by the SwivelLock™ drill, which is again used to a depth of over 25 mm. The SwivelLock™ size is modified according to the size of the graft. The FibreWire® suture present in the device is first removed and then reloaded following passage of the passing wire into the SwivelLock™. The loop of the passing wire is cut and a loop of FibreWire® can then be visualised. This acts as a snaring tool for the proximal fixation of the ALL.
Following preparation of the sockets, the SwivelLock™ is inserted onto the tibial socket and deployed in the standard way to fix the tibial end (Fig. 2d).
The graft is then tunnelled through by creating a plane under the ITB. The femoral end of the ALL graft is then pulled deep to the ITB via the femoral incision. This was done using a passing suture; up through to the femoral socket where it is delivered and tensioned on the SwivelLock™. The modified SwivelLock™ is used on the femoral end, which act as a snare by pulling on the suture exiting from the SwivelLock™. This loop is then tightened and moved to a suitable distance to allow an adequate amount of graft to enter the socket (Fig. 2e).
The socket is then tapped into place. Once the sockets are cleared of soft tissue, the knee is externally rotated and the SwivelLock™ is advanced (Fig. 2f). The tension is the ALL checked one last time before committing, and fixing it with the SwivelLock™.
Fig. 2g shows the reconstructed ALL graft in situ, and the incisions are then closed with sutures or skin staples (Fig. 2h).
Although the surgical technique described above utilises a minimally invasive method, it can also be modified to an open approach using the same principles, anatomical landmarks and origin and insertion points.
4. Results
Given that our research is based from a single surgeon case-series, the results have been reported in line with SCARE criteria [25]. The characteristics of each subject are presented in Table 1. A total of 10 patients were recruited during the study time frame. The age range varied from 19 to 51 years, with a mean of 31.8 years. There were 6 females and 4 males included in the study. 40% of the patients were obese, with the mean BMI being 30.29 kg/m2. Despite a small sample size, there were no statistically significant differences between the baseline characteristics of age and BMI between the two groups. These factors would therefore not be responsible for the variability in subsequent outcomes. There was however an uneven sex distribution noted between the two groups.
Table 1.
Patient profile.
| Patient No. | Gender | Age | BMI | Operation | Op Side | Pivot Shift Grade |
|---|---|---|---|---|---|---|
| 1 | F | 19 | 21.6 | ACL | Left | 0 |
| 2 | M | 34 | 25.0 | ACL | Right | 1 |
| 3 | M | 24 | 29.7 | ACL | Right | 1 |
| 4 | F | 35 | 36.9 | ACL | Right | 2 |
| 5 | M | 26 | 24.9 | ACL | Right | 2 |
| 6 | F | 37 | 36.1 | ACL + ALL | Left | 3 |
| 7 | F | 25 | 37.0 | ACL + ALL | Right | 3 |
| 8 | F | 34 | 28.7 | ACL + ALL | Left | 3 |
| 9 | F | 51 | 37.7 | ACL + ALL | Left | 3 |
| 10 | M | 33 | 25.3 | Revision ACL + ALL | Right | 3 |
4.1. Pre-operative results
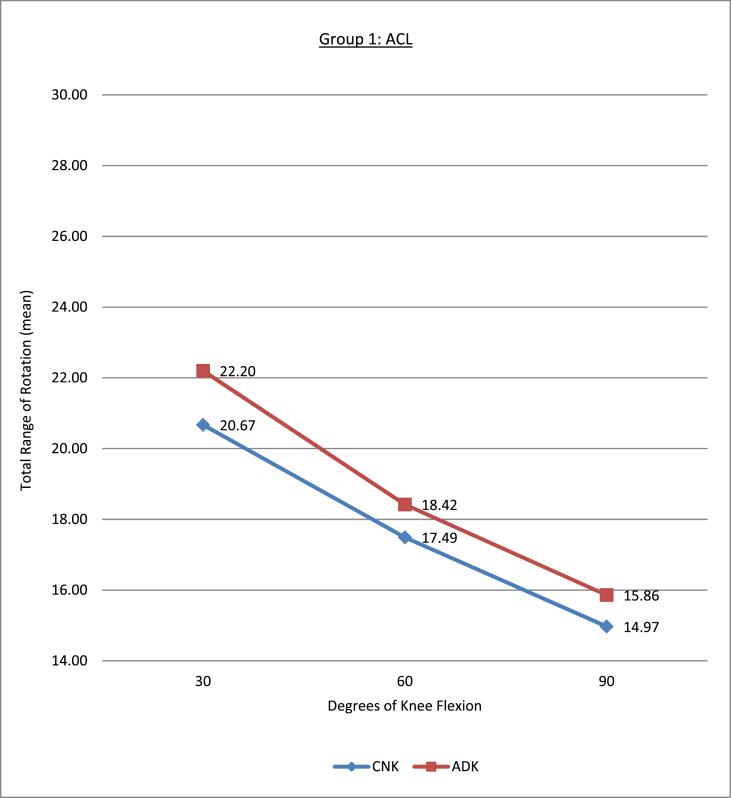
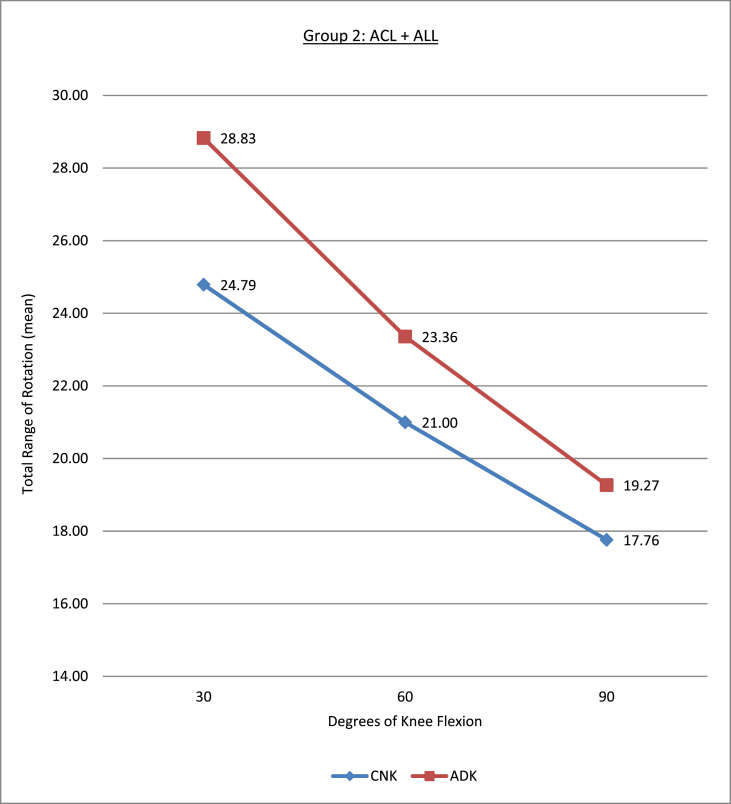
Table 2, Table 3 illustrate the variation in the total range of rotation (TRR) between the contralateral normal knee (CNK) and the ACL-deficient knee (ADK) and their respective means at 30, 60 and 90° of knee flexion in the pre-operative state. At 30°, a difference of 1.53 ± 0.95° was noted in Group 1 while a 4.04 ± 1.79° difference was noted in Group 2. Similarly, at 60° a difference of 0.93 ± 0.50° was noted in Group 1 and a 2.36 ± 0.94° difference in Group 2. This was deemed to be a clinically significant in both cases (p < 0.05). Although a subtle difference in TRR was also noted at 90° of knee flexion between the CNK and the ADN, the subsequent p-value did not achieve statistical significance (p = 0.5).
Table 2.
Variation in the total range of rotation (TRR) between the contralateral normal knee (CNK) and the ACL-deficient knee (ADK) pre-operatively.
| Patient No. | Operation | CNK30 | CKN60 | CKN90 | ADK30 | ADK60 | ADK90 | |
|---|---|---|---|---|---|---|---|---|
| 1 | ACL | 18.78 | 15.68 | 13.48 | 20.54 | 16.22 | 13.25 | |
| 2 | ACL | 20.44 | 16.78 | 12.83 | 20.76 | 17.18 | 12.83 | |
| 3 | ACL | 22.49 | 17.67 | 14.54 | 24.11 | 19.33 | 15.52 | |
| 4 | ACL | 21.17 | 19.17 | 18.64 | 22.24 | 20.29 | 19.31 | |
| 5 | ACL | 20.47 | 18.15 | 15.38 | 23.37 | 19.09 | 18.37 | |
| 6 | ACL + ALL | 25.94 | 21.69 | 17.01 | 29.26 | 23.98 | 17.93 | |
| 7 | ACL + ALL | 22.73 | 18.74 | 14.76 | 25.29 | 20.43 | 16.56 | |
| 8 | ACL + ALL | 27.52 | 22.11 | 20.03 | 31.34 | 24.07 | 21.48 | |
| 9 | ACL + ALL | 25.48 | 22.09 | 19.07 | 32.61 | 26.09 | 22.89 | |
| 10 | Revision ACL + ALL | 22.29 | 20.38 | 17.91 | 25.65 | 22.23 | 17.52 | |
Table 3.
Comparison of difference in TRR between CNK and ADK between the two groups.
| Mean | CNK30 vs. ADK30 | CNK60 vs. ADK60 | CNK90 vs. ADK90 |
|---|---|---|---|
| ACL Group (1) | 1.53 ± 0.95 | 0.93 ± 0.50 | 0.88 ± 1.27 |
| ACL + ALL Group (2) |
4.04 ± 1.79 |
2.36 ± 0.94 |
1.52 ± 1.53 |
| P Value | P = 0.024 | P = 0.017 | P = 0.50 |
| Significance | S | S | NS |
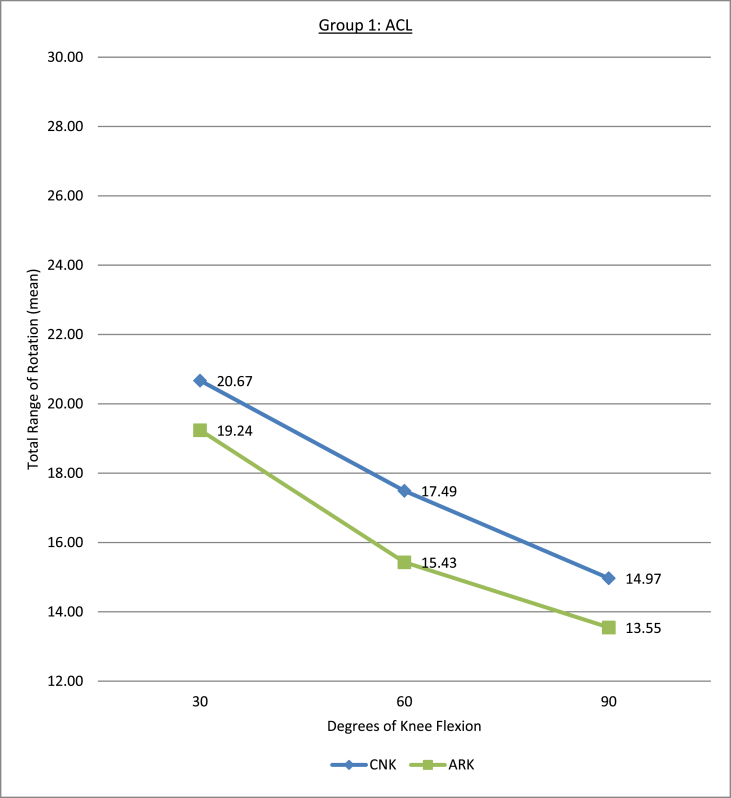
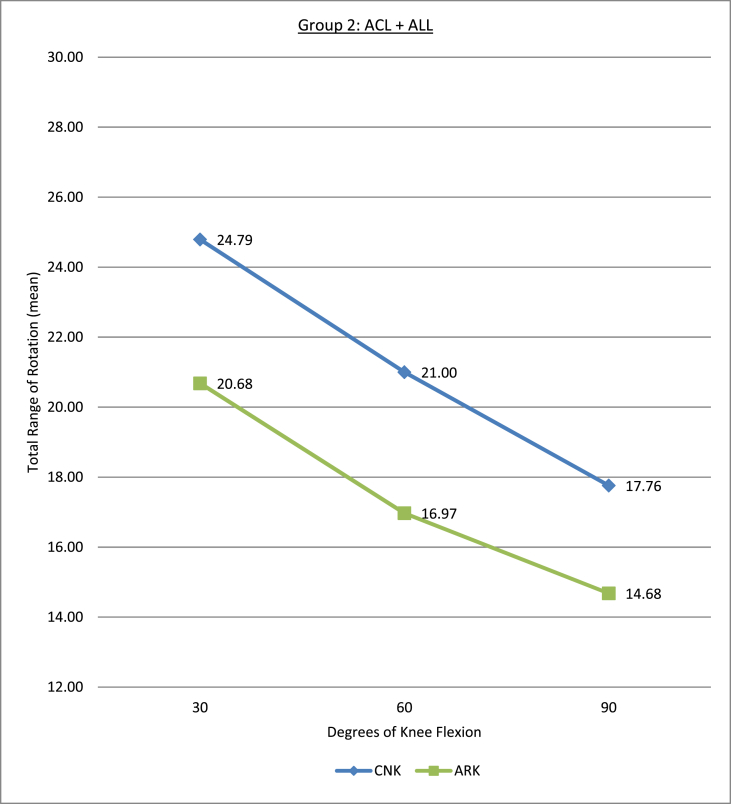
Fig. 3, Fig. 4 are a graphical representation of the variation in TRR between group 1 and 2 during the various stages of knee flexion.
Fig. 3.
Variation in TRR in Group 1 pre-operatively.
Fig. 4.
Variation in TRR in Group 2 pre-operatively.
4.2. Post-operative results
The post-operative results are summarised in Table 4. An independent t-test comparing the mean TRR between groups 1 and 2 in the ARKs revealed no statistical difference at 30 (p = 0.198), 60 (p = 0.297) or 90° (p = 0.379) of knee flexion (p < 0.05) which meant that all reconstructed knees had a similar post-operative rotation range.
Table 4.
Post-operative results with comparison of the difference in TRR between the ADK and the ACL-reconstructed knee (ARK).
| Operation | ARK30 | ARK60 | ARK90 | Absolute Reduction (Degrees) |
Percentage Reduction |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | AR 30 | AR 60 | AR 90 | PR 30 | PR 60 | PR 90 | ||||
| 1 | ACL | 17.47 | 13.85 | 12.54 | −3.07 | −2.37 | −0.71 | 14.95 | 14.61 | 5.36 |
| 2 | ACL | 18.1 | 13.02 | 11.75 | −2.66 | −4.16 | −1.08 | 12.81 | 24.21 | 8.42 |
| 3 | ACL | 19.9 | 15.62 | 12.51 | −4.21 | −3.71 | −3.01 | 17.46 | 19.19 | 19.39 |
| 4 | ACL | 20.1 | 17.19 | 15.23 | −2.14 | −3.1 | −4.08 | 9.62 | 15.28 | 21.13 |
| 5 | ACL | 20.63 | 17.47 | 15.72 | −2.74 | −1.62 | −2.65 | 11.72 | 8.49 | 14.43 |
| 6 | ACL + ALL | 20.63 | 14.26 | 13.58 | −8.63 | −9.72 | −4.35 | 29.49 | 40.53 | 24.26 |
| 7 | ACL + ALL | 19.77 | 16.5 | 13.43 | −5.52 | −3.93 | −3.13 | 21.83 | 19.24 | 18.90 |
| 8 | ACL + ALL | 21.86 | 19.62 | 17.89 | −9.48 | −4.45 | −3.59 | 30.25 | 18.49 | 16.71 |
| 9 | ACL + ALL | 22.96 | 19.18 | 15.54 | −9.65 | −6.91 | −7.35 | 29.59 | 26.49 | 32.11 |
| 10 | Revision ACL + ALL | 18.2 | 15.27 | 12.97 | −7.45 | −6.96 | −4.55 | 29.04 | 31.31 | 25.97 |
Fig. 5, Fig. 6 are graphical representations of the variation in mean TRR between the CNK and ARK between group 1 and 2 in the post-operative state at 30°, 60° and 90°.
Fig. 5.
Variation in TRR in Group 1 post-operatively.
Fig. 6.
Variation in TRR in Group 2 post-operatively.
The difference in TRR between the ADK and the ACL-reconstructed knee (ARK) has been demonstrated in Table 5. Values have described as an absolute reduction (degrees) (AR) or as a percentage reduction (PR), using the ADK as a baseline. When considering the absolute reduction, both groups had an objective and subjective reduction in total range of rotation.
Table 5.
Comparison of the difference in TRR between the ADK and the ACL-reconstructed knee (ARK) between the two groups.
| Mean | Absolute Reduction (Degrees) |
Percentage Reduction |
||||
|---|---|---|---|---|---|---|
| AR 30 | AR 60 | AR 90 | PR 30 | PR 60 | PR 90 | |
| ACL Group [1] | −2.96 ± 0.77 | −2.99 ± 1.01 | −2.3 ± 1.40 | 13.31 ± 3.01 | 16.35 ± 5.83 | 13.75 ± 6.81 |
| ACL + ALL Group [2] |
−8.15 ± 1.02 |
−6.39 ± 2.32 |
−4.59 ± 1.64 |
28.04 ± 3.50 |
27.21 ± 9.14 |
23.59 ± 6.08 |
| P value | P = 0.0003 | P = 0.017 | P = 0.045 | P = 0.0001 | P = 0.056 | P = 0.042 |
| Significance | S | S | S | S | NS | S |
Group 2 had a greater reduction in TRR in comparison to Group 1 at all levels of flexion. These results were particularly significant at 30°of knee flexion (−8.15 vs. −2.96) with a p value of <0.001. Statistical significance was also achieved at 60 and 90° with a corresponding p value of <0.05. We recognise that a difference in TRR existed pre-operatively in the ADK corresponding to the grade of the pivot-shift. By utilising the PR alone and subsequently eliminating the pre-operative difference, statistical significance was still achieved at 30° between the two groups (13.31% vs. 28.04%; p = 0.0001). Statistically significant results were also obtained at 90° with a p value of 0.04. Statistical significance was not achieved at 60° of flexion (p = 0.056).
The aim of surgical ligament reconstruction is restore the ligament deficient knee to a normative state, or what would be deemed as ‘normal’ range of motion for the patient. The contralateral knee was therefore used as ‘control’ to see whether the range of rotation following surgical reconstruction returned to baseline values. Except for one patient (patient 5) whose post-operative measurements at 30 and 90° were marginally greater than the CNK measurements, all other patient post-operative values not only reached baseline values, but also exceeded those that were deemed as ‘normal’ for them. Longitudinal studies are indeed required to see whether this ‘over-correction’ may correlate to clinical symptoms in the future.
5. Discussion
As Dr. Steven Claes so aptly questioned, ‘How can a centrally located cord-like structure (like the ACL) prevent rotation?’ [26]. To prevent excessive rotation, a structure needs to be present away from the centre axis; at the edge of a plane that would then resist this rotational motion. This thought process led to the belief of the existence of additional structure on the lateral aspect of the knee that would prevent rotation - the ALL. Surgical reconstruction of the ALL is still a novel procedure lacking any literature evidence of outcome measures. We believe that the outcome of our study specifically addresses the role of the ligament in providing rotational stability. Work by Claes et al. [26] using sequential cutting techniques on cadaveric knees have demonstrated that damage to the ALL was indeed a pre-requisite for obtaining a grade 3 pivot shift. They also showed that sectioning (isolated cutting) of the ALL increases the grade of the pivot shift by a minimum of 1, irrespective of the structural integrity of the ACL. This finding further strengthens the view that the ALL plays a crucial role in controlling internal rotation of the knee and subsequently, rotational stability. Conversely, work by Kittl et al. [27] showed that the iliotibial tract showed larger contributions in restraining anterior subluxation and tibial internal rotation, with the ALL playing a minor role. Therefore, there is much debate regarding the role of the ALL, and as such, more research is indeed required.
If we consider the elastic nature of the ACL, rotational stability cannot be determined on the basis of the rotation angle alone. We must therefore consider the moment of force that results in rotation, and the ability of the ACL (and its surrounding ligaments) to resist this rotation [28]. Current practice based in ACL reconstruction focuses on restoring the pathological anterior translation of the tibia with good outcomes. However, despite evidence to suggest improved rotational stability with double-bundle reconstruction, meta-analysis of these randomised control trials have concluded that the TRR and consequently rotational stability, is still not restored to normative values (10, 11). This instability (in both groups) is particularly evident during loading and extreme rotation conditions (pivoting). Rotational instability can be assessed using the graded pivot shift test. It is still one of the most specific tests for detecting an ACL injury with a specificity ranging from 97% to 100% [29], [30]. However, the test is still highly subjective and observer dependent with the outcome being easily skewed by muscle guarding. We attempted to eliminate this bias by having the test performed by the same operating surgeon as well as being performed after the patient was anaesthetized.
The reconstruction technique of the ACL no doubt plays a crucial role in restoring stability to the knee and similar outcomes have been noted when comparing single-bundle vs. double-bundle reconstruction techniques. We attempted to overcome the discrepancy in the reconstruction technique used for the ACL by using a uniform, single-bundle reconstruction technique across all patients, which might reduce, but not necessarily eliminate surgical bias in a small patient group.
Statistically significant differences in the TRR were noted in the CNKs between Group 1 and Group 2. Therefore, when considering the type of surgery that the patient should undergo, we need to take into account the fact that ‘normal knees’ in Group 2 actually had a greater range of rotation. This may be accounted for by the larger female to male ratio in Group 2 compared to Group 1. It is widely accepted that female knees demonstrate greater joint laxity compared to males [31], [32], [33]. Whether this larger degrees of rotation corresponds to symptomatic laxity is entire subjective. Of note, all 10 patients reported no issues with their normal knees and therefore a larger TRR may not necessarily correlate to rotational instability. When you then consider the ADKs, a larger TRR was noted in Group 2 compared to Group 1. More importantly, a larger difference in the TRR had been observed between the CNK and the ADK (mean TRR at 30° of knee flexion: 1.53 ± 0.95 vs. 4.04 ± 1.79; p < 0.05). Therefore, despite a notable difference in the CNKs between the groups, the extent of rotational deficit as a consequence of an ACL injury was significantly higher in Group 2 – which was why they had dual ligament reconstruction. These differences can be replicated clinically using the graded pivot-shift test and therefore, we can still objectively identify patients who demonstrate excessive rotational laxity.
The integrity of the reconstructed ACL graft was assessed intra-operatively and post-operatively using the Lachman's test. Our results showed that whilst both groups attained a normative range of rotation following single or dual ligament reconstruction, the absolute reduction (in degrees) was much higher in Group 2 compared to Group 1 (−8.15% vs. −2.96%; p < 0.001) at 30° of knee flexion (See Table 5). A similar result was also obtained at 60° and 90° of knee flexion. Conversely, we recognise that a difference in TRR existed pre-operatively in the ADK, which corresponded to the grade of the pivot shift. Therefore, even if we consider the percentage reduction that occurred post-operatively (thereby eliminating the pre-operative difference), statistical significance was still achieved at 30° between the two groups (13.31% vs. 28.04%; p = 0.0001) confirming the validity of our results.
What would be considered as a normal range of rotational motion is often subjective to the patient. Patients who are generally lax may not necessarily report symptoms of instability. It is therefore important to consider whether dual ligament reconstruction is appropriate in this subset of patients, and this decision can once again be based upon the outcome of the pivot shift test. Fortunately for our study, all 10 patients had no known pathology in their contralateral knees and we could therefore designate the contralateral knee as a reference point for a stable joint.
Our findings are based primarily in anaesthetized patients, with true kinematic values at time-zero post-operatively. This itself has its advantages and disadvantages. Kinematic studies in the anaesthetized patients give ‘true’ ranges of motion, but we appreciate that this may not necessarily correlate to clinical ranges of motion. This again highlights the need for long-term clinical and patient-centered outcome measures.
Our results demonstrate that all 10 patients achieved better than normative values following surgery. This result could be interpreted in two ways: both surgical procedures are effective modalities for which they were intended i.e. dependent on the extent of rotational instability during the pre-operative state as well as the grade of the pivot shift. However, we also need to consider whether this ‘over-correction’ may result in joint stiffness. We therefore need further longitudinal studies that will assess and correlate clinical symptoms to the type of procedure that the patient underwent. To add to this, our main strength of the study was the use of the validated, and highly accurate kinematic analysis device. Furthermore, the pivot shift test was performed solely by the operating surgeon, as were the surgical procedures carried out on all 10 patients. A uniform single-bundle ACL reconstruction technique was used for all patients in the case series minimising the surgical discrepancy in the study.
Despite achieving acceptable numbers derived from our power calculation, we recognise that the small sample size utilised is itself a potential source of bias. The differences in sex distribution between the groups highlights a potential confounder, accounting for the variation in the pre-operative TRR in the CNKs. We also recognised that subjective relief of symptoms is an important clinical indicator of a successful surgery, an outcome that was not measured in our study. Therefore, the use of a validated patient-centered outcome measure such as the Cincinnati knee rating system, the modified Lysholm scale [34] or more recently, Mohtadi quality-of-life questionnaire for the ACL-injured knee [35] would be a welcomed addition for integration into future studies.
Further studies assessing long-term clinical and patient-centered outcomes are undoubtedly necessary to reinforce the role the reconstructed ALL in restoring rotational stability to the knee.
6. Conclusion
The aim our study was to investigate the post-operative change in total range of tibial rotation following surgical reconstruction of either single (ACL) or dual ligaments (ACL + ALL) after a primary ACL injury in an anesthetised knee. We established that pre-operatively, the higher the grade of the pivot-shift on the ACL deficient knee, the greater the TRR present. Subsequently, all patients with a grade 3 pivot shift underwent dual ligament reconstruction, whilst those with an absent pivot shift or grade 1 or 2 underwent single ligament reconstruction. Both groups of patients achieved a TRR that was equivalent, or even better that observed on their contralateral ‘normal’ knee.
Our findings are based primarily in anaesthetized patients, with true kinematic values at time-zero post-operatively. We do not believe that every patient should undergo dual ligament reconstruction rather, our case series highlights that patients who present with a history suggestive of significant rotational instability following a primary ACL injury, and are objectively assessed to have a grade 3 pivot shift may benefit from reconstruction of the both the ACL and the ALL.
There is no doubt that further research is required assessing long-term clinical outcomes, but we believe that our study provides a foundation for the role of the ALL in maintaining rotational stability.
Ethical approval
This study was performed as service evaluation of current clinical practice at the Royal Derby Hospital and was therefore registered with the Research and Development Department, without the need for formal ethical approval.
Funding
No funding was obtained for this research.
Author contribution
R Shah was involved in study concept, design, data collection, analysis and write up of the manuscript.
R Singh was involved in data collection, analysis and operative assistant.
CD was involved in study concept, design, analysis and write up the manuscript.
GG was the senior surgeon performing all surgical procedures as well as being involved in the study concept and design.
Conflicts of interest
All authors have no conflicts of interest.
Guarantor
Rohi Shah (Lead Author).
Consent
All patients received an information sheet entailing the aims and objectives of the study, with a clear explanation that the study would not alter the surgical procedural decision. Following this, written consent was obtained to take part in the study.
Registration of research studies
Given that the study was based on service evaluation, the study did not need to be registered to a publicly accessible database.
References
- 1.Segond P.-F. Publications du Progrès médical; 1879. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. [Google Scholar]
- 2.Woods G.W., Stanley R.F., Tullos H.S. Lateral capsular sign: x-ray clue to a significant knee instability. Am. J. Sports Med. 1979;7(1):27–33. doi: 10.1177/036354657900700107. [DOI] [PubMed] [Google Scholar]
- 3.Goldman A.B., Pavlov H., Rubenstein D. The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am. J. Roentgenol. 1988;151(6):1163–1167. doi: 10.2214/ajr.151.6.1163. [DOI] [PubMed] [Google Scholar]
- 4.Hess T., Rupp S., Hopf T., Gleitz M., Liebler J. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin. Orthop. Relat. Res. 1994;303:193–197. [PubMed] [Google Scholar]
- 5.Terry G.C., Hughston J.C., Norwood L.A. The anatomy of the iliopatellar band and iliotibial tract. Am. J. Sports Med. 1986;14(1):39–45. doi: 10.1177/036354658601400108. [DOI] [PubMed] [Google Scholar]
- 6.LaPrade R.F., Gilbert T.J., Bollom T.S., Wentorf F., Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am. J. Sports Med. 2000;28(2):191–199. doi: 10.1177/03635465000280020901. [DOI] [PubMed] [Google Scholar]
- 7.Campos J.C., Chung C.B., Lektrakul N., Pedowitz R., Trudell D., Yu J. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219(2):381–386. doi: 10.1148/radiology.219.2.r01ma23381. [DOI] [PubMed] [Google Scholar]
- 8.Vieira E.L., Vieira E.A., da Silva R.T., Berlfein P.A., Abdalla R.J., Cohen M. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23:269–274. doi: 10.1016/j.arthro.2006.11.019. United States. [DOI] [PubMed] [Google Scholar]
- 9.Vincent J.P., Magnussen R.A., Gezmez F., Uguen A., Jacobi M., Weppe F. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg. Sports Traumatol. Arthrosc. 2012;20(1):147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 10.Kongtharvonskul J., Attia J., Thamakaison S., Kijkunasathian C., Woratanarat P., Thakkinstian A. Clinical outcomes of double- vs single-bundle anterior cruciate ligament reconstruction: a systematic review of randomized control trials. Scand. J. Med. Sci. Sports. 2013;23(1):1–14. doi: 10.1111/j.1600-0838.2011.01439.x. [DOI] [PubMed] [Google Scholar]
- 11.Xu M., Gao S., Zeng C., Han R., Sun J., Li H. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29:357–365. doi: 10.1016/j.arthro.2012.08.024. United States: 2013 Arthroscopy Association of North America. Published by Elsevier Inc. [DOI] [PubMed] [Google Scholar]
- 12.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J. Anat. 2013;223(4):321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dodds A.L., Halewood C., Gupte C.M., Williams A., Amis A.A. The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Jt. J. 2014;96-B:325–331. doi: 10.1302/0301-620X.96B3.33033. England. [DOI] [PubMed] [Google Scholar]
- 14.Physiopedia. Knee Rotatory Instability [Available from: http://www.physio-pedia.com/Knee_Rotary_Instability-cite_note-3.
- 15.Surgeons AAoO. Anterior Cruciate Ligament (ACL) Injuries [Available from: http://orthoinfo.aaos.org/topic.cfm?topic=a00549.
- 16.Noyes F.R., Bassett R.W., Grood E.S., Butler D.L. Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J. Bone Jt. Surg. Am. 1980;62(5):687–695. 757. [PubMed] [Google Scholar]
- 17.Jakob R.P., Staubli H.U., Deland J.T. Grading the pivot shift. Objective tests with implications for treatment. J. Bone Jt. Surg. Br. 1987;69(2):294–299. doi: 10.1302/0301-620X.69B2.3818763. [DOI] [PubMed] [Google Scholar]
- 18.Tsai A.G., Wijdicks C.A., Walsh M.P., Laprade R.F. Comparative kinematic evaluation of all-inside single-bundle and double-bundle anterior cruciate ligament reconstruction: a biomechanical study. Am. J. Sports Med. 2010;38:263–272. doi: 10.1177/0363546509348053. United States. [DOI] [PubMed] [Google Scholar]
- 19.Walley G., Datir S., Sayana M., Rahmatalla A., Dos Remedios I., Wynn-Jones C. Anteroposterior glide versus rotating platform low contact stress (LCS) knee arthroplasty: a randomised controlled trial. BMC Musculoskelet. Disord. 2007;8:87. doi: 10.1186/1471-2474-8-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Griffith C.J., LaPrade R.F., Johansen S., Armitage B., Wijdicks C., Engebretsen L. Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. Am. J. Sports Med. 2009;37:1762–1770. doi: 10.1177/0363546509333852. United States. [DOI] [PubMed] [Google Scholar]
- 21.McKellop H., Hoffmann R., Sarmiento A., Ebramzadeh E. Control of motion of tibial fractures with use of a functional brace or an external fixator. A study of cadavera with use of a magnetic motion sensor. J. Bone Jt. Surg. Am. 1993;75(7):1019–1025. doi: 10.2106/00004623-199307000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Sati M., de Guise J.A., Drouin G. Computer assisted knee surgery: diagnostics and planning of knee surgery. Comput. Aided Surg. 1997;2:108–123. doi: 10.1002/(SICI)1097-0150(1997)2:2<108::AID-IGS4>3.0.CO;2-3. United States. [DOI] [PubMed] [Google Scholar]
- 23.Hagemeister N., Parent G., Van de Putte M., St-Onge N., Duval N., de Guise J. A reproducible method for studying three-dimensional knee kinematics. J. Biomech. 2005;38:1926–1931. doi: 10.1016/j.jbiomech.2005.05.013. United States. [DOI] [PubMed] [Google Scholar]
- 24.Grood E.S., Suntay W.J. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J. Biomech. Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 25.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 26.Claes S. Anterolateral Ligament Reconstruction Using SwiveLock®. http://www.arthrex.com/resources/video/JOVv2r2KoE-v7gFCU0pqVw/anterolateral-ligament-reconstruction-using-swivelock Available from:
- 27.Kittl C., El-Daou H., Athwal K.K., Gupte C.M., Weiler A., Williams A. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am. J. Sports Med. 2016;44(2):345–354. doi: 10.1177/0363546515614312. [DOI] [PubMed] [Google Scholar]
- 28.Bohn M.B., Sorensen H., Petersen M.K., Soballe K., Lind M. Rotational laxity after anatomical ACL reconstruction measured by 3-D motion analysis: a prospective randomized clinical trial comparing anatomic and nonanatomic ACL reconstruction techniques. Knee Surg. Sports Traumatol. Arthrosc. 2015 Dec;23(12):3473–3481. doi: 10.1007/s00167-014-3156-5. Epub 2014 Jul 4. [DOI] [PubMed] [Google Scholar]
- 29.Jain D.K., Amaravati R., Sharma G. Evaluation of the clinical signs of anterior cruciate ligament and meniscal injuries. Indian J. Orthop. 2009;43(4):375–378. doi: 10.4103/0019-5413.55466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katz J.W., Fingeroth R.J. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am. J. Sports Med. 1986;14(1):88–91. doi: 10.1177/036354658601400115. [DOI] [PubMed] [Google Scholar]
- 31.Boguszewski D.V., Cheung E.C., Joshi N.B., Markolf K.L., McAllister D.R. Male-female differences in knee laxity and stiffness: a cadaveric study. Am. J. Sports Med. 2015;43(12):2982–2987. doi: 10.1177/0363546515608478. [DOI] [PubMed] [Google Scholar]
- 32.Rosene J.M., Fogarty T.D. Anterior tibial translation in collegiate athletes with normal anterior cruciate ligament integrity. J. Athl. Train. 1999;34(2):93–98. [PMC free article] [PubMed] [Google Scholar]
- 33.Rozzi S.L., Lephart S.M., Gear W.S., Fu F.H. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am. J. Sports Med. 1999;27(3):312–319. doi: 10.1177/03635465990270030801. [DOI] [PubMed] [Google Scholar]
- 34.Lysholm J., Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am. J. Sports Med. 1982;10(3):150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 35.Mohtadi N. Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am. J. Sports Med. 1998;26(3):350–359. doi: 10.1177/03635465980260030201. [DOI] [PubMed] [Google Scholar]