Abstract
OBJECTIVES
To evaluate the relationship among the measures in a power wheelchair outcomes toolkit.
DESIGN
We performed path analysis of cross-sectional data from self-report questionnaires and one objective measure.
SETTING
Data were collected in six Canadian sites.
PARTICIPANTS
A convenience sample of 128 power wheelchair users. The majority, 69 (53.9%), were female. Multiple sclerosis and spinal cord injury/disease were the most common diagnoses.
INTERVENTIONS
Not applicable.
MAIN OUTCOME MEASURES
The power wheelchair version of the Wheelchair Skills Test (4.1) was used to carry out an objective evaluation of capacity to perform 32 wheelchair skills. The Late Life Disability Index measured frequency of participation in 16 life activities. The Life-space Assessment measured independence, extent and frequency of mobility. The Assistive Technology Outcomes Profile for Mobility was used to assess perceived difficulty performing activity and participation using assistive technology. The Wheelchair Use Confidence Scale for powered wheelchair users captured users’ self-efficacy with wheelchair use.
RESULTS
Wheelchair confidence was independently associated with less difficulty with activity (β =0.08, 0.01<p>0.05) and participation (β=0.39, p<0.01), increased life space (β=0.09, p<0.03) and greater wheelchair skills (β=0.37, p<0.01) Less perceived difficulty with activity was independently associated with increased frequency of participation (β=0.30, p<0.01). Life space mobility was independently associated with increased frequency of participation ((β=0.31, p<0.01). Less difficulty with participation was independently associated with greater life-space mobility (β=0.32, p<0.01) and greater frequency of participation (β=0.13, p<0.01).
CONCLUSION
This study provides empirical support for the measures included as part of the power wheelchair outcomes toolkit. They appear to provide complementary information on a variety of constructs related to power wheelchair use.
Keywords: power mobility, social participation, wheelchair confidence, mobility, life-space
INTRODUCTION
Mobility disability is one of the most common types of functional impairments, and it increases exponentially with age (1–3). For example, in Canada, mobility disability affects 24% of those aged 65–75 and over 60% of those over the age of 85 (1). For some individuals with a mobility disability, power wheelchairs are essential devices. Individuals who are unable to ambulate may have problems propelling a manual wheelchair due to limited upper extremity function, strength, or endurance (4). Although powered mobility has a number of advantages, there are some issues with its use (5). On one hand, most studies have found that power mobility prescription is associated with a variety of beneficial effects including increased mobility, increased social participation, and increased quality of life (6). On the other hand, some studies have indicated that abandonment is a concern (7, 8) and that users may experience increased problems with accessibility and transportation (9, 10).
Few studies have systematically evaluated the outcomes of power wheelchair provision. For example, a recent pre-post study found that power mobility provision significantly increased the frequency of mobility related activities and decreased difficulty in a variety of areas of participation (11). The study, however, did not document if there were changes in the extent of their mobility or how these outcomes might have been affected by changes in their wheelchair skills or confidence (11). The incomplete portrayal of relevant power mobility outcomes may be attributed to the atheoretical nature of research in this area and to the paucity of reliable and valid power wheelchair specific measures that operationalize relevant power wheelchair-related outcomes (12). Given the high cost of these devices, which may exceed $30,000 (USD), better evaluation is necessary to demonstrate the broad range of outcomes that can be attributed to power wheelchair provision.
Several models have been proposed to help understand the outcomes associated with assistive technology provision. The Human Activity-Assistive Technology Model indicates an assistive technology system is comprised of a human using an assistive technology to complete an activity within the context of his or her environment (13). The International Classification of Function, Disability and Health (ICF) has also been used as an assistive technology model. According to the ICF, functioning (which includes body structure and function, activity and participation) results from a complex interaction between an individual (with a health condition) and that individual’s contextual factors (environmental and personal). With the ICF, assistive technology is considered part of environment, but some functioning codes explicitly acknowledge the use of assistive technology (e.g., moving around with equipment (d465)) (14). Routhier et al. developed a performance assessment framework for wheelchairs, which indicates there are five main factors that influence wheeled mobility, which include user characteristics, environment, daily activities and social roles, assessment and training and the wheelchair itself. According to this model, wheeled mobility enables social participation. Activity and social participation are important elements in all of these models, but only Routhier et al.’s model suggests there is a hierarchical relationship between assistive technology use, mobility and social participation (15).
Based on these models, and our clinical and research experience, we developed a power wheelchair outcomes toolkit that we felt assessed important, complementary outcomes related to power wheelchair provision. The purpose of this toolkit is to capture important outcomes of wheelchair provision that can be used to justify wheelchair-related equipment and intervention services and help to inform prescribers’ clinical reasoning. For example, initially device provision and training might lead to improved power wheelchair confidence. As device use becomes more habitual, it may lead to changes in mobility and social participation. As illustrated in Table I, the toolkit included five measures: the Wheelchair Skills Test for powered wheelchair users (WST-P) (16), the Late Life Disability Index (LLDI) (17), Life-space Assessment (LSA) (18), the Assistive Technology Outcomes Profile for Mobility, which includes two independent sub-scales for activity and participation (ATOP/M-A and ATOP/M-P) and the Wheelchair Use Confidence Scale for powered mobility users (WheelCon-P) (18, 19).
Table I.
Description of Measures Included in the Power Wheelchair Toolkit
| Areas of Measurement (domain) | Measurement Tool | Rationale for Inclusion | Items | Scoring |
|---|---|---|---|---|
| Wheelchair skill capacity | Wheelchair Skills Test for powered wheelchair users (WST-P) version 4.1. | Wheelchair skills should have an effect on confidence, mobility, and social participation. (23, 24) | Measures capacity to perform 32 skills including basic mobility (e.g., making turns, moving forwards and backwards), negotiating obstacles (e.g., thresholds and ramps), performing transfers, and other basic power wheelchair operations (e.g., turning the chair on and off). | Items are scored dichotomously (pass/fail) by a trained rater. An overall score is calculated to represent the percentage of applicable items that are accomplished successfully. |
| Frequency of participation | The Late Life Disability Index (LLDI) | Power wheelchair use should affect participation. (25,26) | Measures frequency of participation in 16 life activities (e.g., visiting friends and families in their homes, taking part in active recreation, taking care of others, taking care of your own health). | Frequency is measured on a five-point scale (1 = never to 5 = very often) and a total, cumulative score can be calculated which ranges from 16–80. |
| Mobility performance | Life-space Assessment (LSA) | Life-space mobility should be increased by power wheelchair use (27) and should be related to social participation. | Measures independence and frequency of mobility in five, increasingly larger, life-spaces: home, around home, neighbourhood, or town, and outside of their city or town in the last four weeks. | Frequency is measured on a 4-point scale, which ranges from less than once per week to daily. Assistance required from a person and/or assistive technology is measured on a three-point scale. A composite life-space mobility score, which ranges from 0–120 is calculated by multiplying the independence scores by the frequency scores for each life by the life-space multiplier (1–5) and summing the total. |
| Perceived difficulty with activity and participation | Assistive Technology Outcomes Profile for Mobility (ATOP/M) | By comparing perceived difficulty with participation with and without assistive technology, this measure provides subjective data on how a power wheelchair affects users’ sense of well-being, which has been found to be influenced by the use of power wheelchair. (28) | Measures perceived difficulty with activity, (e.g., physical performance and instrumental skills of daily living (IADLs), and participation (e.g., social and discretionary role performance) with and without assistive technology. | The scale was developed using item response theory, and the measure was administered using computer adaptive testing. A T-score was calculated for each domain (0–100).social roles) with assistive technology. |
| Power wheelchair confidence | Wheelchair Use Confidence Scale for powered wheelchair users (WheelCon-P) | Self-efficacy is an important predictor of performance above and beyond capacity (i.e., wheelchair skills). (21) | Includes 63 items that captures users’ self-efficacy with negotiating the physical environment, wheelchair-related activities, knowledge and problem solving, advocacy, managing social situations, and managing emotions. | Item responses are recorded using a 101 point scale (0=not confident at all; 100=completely confident) and the average total score ranges from 0–100. |
Theoretical Model
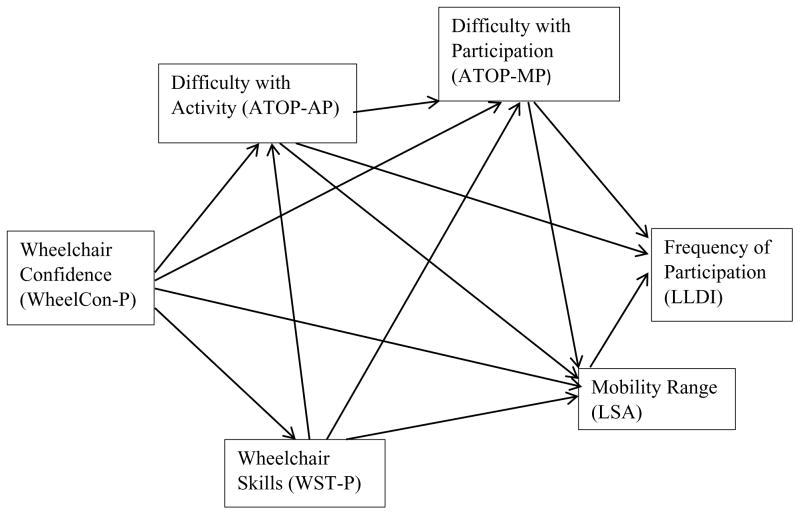
We hypothesized a model of how we anticipated these measures would relate to one another (see Figure I). The model was informed by empirical evidence described in Table 1 and by our conceptual understanding of the relationship among the variables. For example, in keeping with social cognitive theory, self-efficacy (i.e., wheelchair confidence) is anticipated to play a key role in predicting behaviour (i.e., mobility and participation) (26). Therefore, in our model, confidence with a powered wheelchair (WheelCon-P) is anticipated to have a direct influence on powered wheelchair skills (WST-P), life-space mobility (LSA), as well as perceived difficulty with physical performance and instrumental skills of daily living (IADLs) (i.e., ATOP/M-A), and social and discretionary role performance (i.e., ATOP/M-P) with power wheelchair use. There is some empirical support for these relationships among manual wheelchair users as wheelchair skill training has been found to improve confidence with a manual wheelchair (19) and wheelchair confidence is associated with increased frequency of participation (27). As a capacity measure, wheelchair skills are anticipated to have a direct effect on life-space mobility (LSA) and perceived difficulty with activity and participation (ATOP/M). According to social learning theory (26), confidence (i.e., self-efficacy) is expected to moderate the relationship between capacity (WST) and performance (LSA). Perceived difficulty with activity (ATOP/M-A) is expected to have a direct effect on perceived difficulty with participation (ATOP/M-P), which, in turn, has a direct effect on the frequency of participation (LLDI) and life-space mobility (LSA). Likewise, perceived difficulty with activity (ATOP/M-A) is hypothesized to have a direct effect on the frequency of participation (LLDI) and life-space mobility (LSA). Life-space mobility (LSA) is expected to have a direct effect on the frequency of participation (LLDI).
Figure I.
Anticipated Relationship among Measures Included in the Power Wheelchair Toolkit
ATOP/M = Assistive Technology Outcome Profile, Range: 0–100
LLDI = Late Life Disability Index, Range: 16–80
LSA = Life-space Assessment, Range: 0–120
WheelCon-P = Wheelchair Confidence Scale for Power Wheelchair Users, Range: 0–100
WST-P = Wheelchair Skills Test for Power Wheelchair Users, Range: 0–100
Our model is similar to those described above in that it stresses the importance of activity and participation. However, our model also emphasizes the subjective and objective dimensions of outcomes related to power mobility prescription and, like the model proposed by Routhier et al., indicates there is a hierarchical relationship between mobility and participation. Further, it indicates there is a hierarchical relationship between wheelchair confidence, wheelchair skills, and mobility (15). The model can serve as a clinical reasoning tool to help clinicians identify areas for potential interventions to improve the mobility and participation of power wheelchair users.
The objective of this study was to evaluate the relationship among the measures in our outcomes toolkit to see if they were consistent with the model we developed. [Insert Figure I]
METHODS
The study used cross-sectional, baseline data from a larger, multi-site, longitudinal study of power wheelchair use. The study was approved by ethics boards in the six Canadian sites where the research took place: Vancouver, British Columbia; London, Ontario; Toronto, Ontario; Montréal, Québec; Québec City, Québec; and Halifax, Nova Scotia.
Participants
To be included in the study, participants needed to be ≥50 years of age, independent power wheelchair users, and French or English speaking. Participants with cognitive impairments that precluded them from providing consent or completing questionnaires were excluded from the study.
Recruitment
A convenience sample of participants were recruited from a variety of settings, including rehabilitation facilities, wheelchair seating programs, and wheelchair equipment vendors. Potential participants were informed about the study via posters and direct invitation from third party recruiters. Participants were also recruited via social media, advertisements in newsletters and newspapers, and word-of-mouth. Research coordinators at each site confirmed eligibility, reviewed the study protocol, and scheduled an appointment to obtain informed consent and commence data collection with interested individuals.
Power Wheelchair Outcomes Toolkit Measures
As noted in Table 1, the toolkit included five measures. Preliminary evaluation of the measurement properties of measures included in the toolkit indicated that they all had good reliability (intraclass reliability coefficients >.78) and demonstrated construct validity (28, 29). Previous research has found the Life Space Assessment has excellent measurement properties for power mobility users (30). All of the measures were available in French and English, except the Wheelchair Use Confidence Scale.
Demographic Information
For descriptive purposes, demographic information was collected on each participant, including age, sex, marital status, income, education, primary diagnosis, living situation, and months of power wheelchair experience.
Data Collection
Data were collected by raters, who were formally trained to administer all study assessments. Raters entered participant responses in OpenClinica (Isovera Inc., Waltham, MA).
Analysis
Data were checked for out of range values and data entry errors. To describe the sample, descriptive statistics were calculated. To explore the relationship among the variables, a Pearson’s correlation matrix was constructed. Path analysis was used to test our proposed model, which is intended to explain the relationship among the measures included in the toolkit. To ensure reliable results, it is recommended that the sample size should be approximately 10 times greater than the number of paths estimated (31). As the hypothesized model had 12 paths, this would indicate a minimum sample size of 120. As path analysis requires a complete set of data, missing values diagnostics were performed using IBM SPSS Statistics 19 (IBM Corp., Armonk, NY). All variables had <4% missing values, except for the WheelCon-P. For this measure, a French translation of the tool was unavailable at baseline, and so data for this variable was unavailable for 29% of participants. Given the systematic reason for this missing data, it was considered missing at random (32) (i.e., that the missingness was not related to the value of the variable), as we did not anticipate wheelchair confidence would vary geographically. Therefore, missing values were imputed using Bayesian multiple imputation in AMOS (SPSS Inc., Chicago, IL), which produced 10 complete data sets, which were used for the path analysis. Maximum likelihood was used to calculate parameter estimates. To evaluate the model, four goodness-of-fit statistics were calculated: Chi-square, minimum sample discrepancy function (CMIN/DF), root mean square error of approximation (RMSEA), and the Normed Fit Index (NFI). Good fitting models should have a non-significant Chi-square and a CMIN/DF below 2, an RMSEA ≤ 0.05, and a NFI ≥ 0.92(33, 34). Modification indices were reviewed to determine if any paths should be omitted or added.
RESULTS
As described in Table II, the sample included 128 participants. The majority were female; their median income was between $15,000–$30,000 (CAD); and most had some college or university education. Almost half lived alone, one-quarter were new wheelchair users, and multiple sclerosis was their most common primary diagnosis. The mean duration of power wheelchair use was almost 10 years. Most participants had their wheelchairs funded via provincial or federal health-care assistance programs, and a majority of them had power wheelchairs that could tilt-in-space. The participants’ mean wheelchair skills and wheelchair confidence were approximately 80, their mean LSA scores was 40. Participants’ means on the LLDI, ATOP/M-A and ATOP/M-P were near the middle of the range of possible scores.
Table II.
Background and Outcome Variables for Assistance Users
| Variable | mean ±SD1, %(N) |
|---|---|
|
| |
| Demographic Variables | |
|
| |
| Age (years) | 61.1±7.6 |
|
| |
| Female | 53.9% (69) |
|
| |
| Primary Diagnosis | |
| Spinal Cord Injury/Disease | 21.9% (28) |
| Multiple Sclerosis | 21.9% (28) |
| Stroke | 13.2% (17) |
| Arthritis | 7.8% (11) |
| Muscular Dystrophy | 4.7% (6) |
| Amputation | 3.9.3% (5) |
| COPD2 | 2.3% (3) |
| Heart Disease | 1.6% (2) |
| Diabetes | 1.6% (2) |
| Parkinson’s Disease | 0.8% (1) |
| Other (e.g., trauma, post polio) | 19.5% (25) |
|
| |
| Education | |
| High School | 29.7% (38) |
| Some College/University | 60.0% (77) |
|
| |
| Living Alone | 48.4% (62) |
|
| |
| Marital Status | |
| Single | 29.7% (38) |
| Married | 32.8% (42) |
| Common-Law | 5.5% (7) |
|
| |
| Median Income (CAD) | |
| < $15,000 | 32.8% (42) |
| $15,000 – 30,000 | 19.5% (25) |
| $30,000 – 45,000 | 10.9% (14) |
| $45,000 – 60,000 | 8.6% (11) |
| $60,000 – 75,000 | 2.3% (3) |
| > $75,000 | 7.0% (9) |
| Prefer not to answer | 18.8% (18) |
|
| |
| Wheelchair Related Variables | |
|
| |
| Power Wheelchair Use (months) | 119.7±123.7 |
|
| |
| Provided with Power | 29.7% (38) |
|
| |
| Education | |
| High School | 29.7% (38) |
| Some College/University | 60.0% (77) |
|
| |
| Living Alone | 48.4% (62) |
|
| |
| Marital Status | |
| Single | 29.7% (38) |
| Married | 32.8% (42) |
| Common-Law | 5.5% (7) |
|
| |
| Wheelchair Training | |
|
| |
| Wheelchair Features | |
| Tilt | 57.0% (73) |
| Recline | 9.4% (12) |
| Seat Elevation | 12.5% (16) |
| Elevated Footrest | 11.7% (15) |
|
| |
| Funding | |
| Provided with Provincial or Federal Assistance | 66.4% (85) |
| Public Insurance | 6.3% (8) |
|
| |
| Wheelchair Toolkit Variables | |
|
| |
| Education | |
| High School | 29.7% (38) |
| Some College/University | 60.0% (77) |
|
| |
| Living Alone | 48.4% (62) |
|
| |
| Marital Status | |
| Single | 29.7% (38) |
| Married | 32.8% (42) |
| Common-Law | 5.5% (7) |
|
| |
| WST-P3 (0–100) (N=124) | 82.2±11.0 |
|
| |
| LSA4 (1–120) (N=128) | 40.9±15.6 |
|
| |
| LLDI5 (16–80) (N=123) | 49.8±8.7 |
|
| |
| WheelCon-P6 (0–100) (N=91) | 78.6±14.4 |
|
| |
| ATOP/M-P7 (0–100) (N=127) | 52.9±8.7 |
|
| |
| ATOP/M-A8 (0–100) (N=127) | 46.6±4.8 |
Standard Deviation
Chronic Obstructive Pulmonary Disease
Wheelchair Skills Test for powered wheelchair users
Life Space Assessment
Late Life Disability Index
Wheelchair Use Confidence Scale for powered wheelchair users
Assistive Technology Outcomes Measure Participation Score
Assistive Technology Outcomes Measure Activity Score
Table III presents the correlation matrix for measures included in the toolkit. The correlation coefficients ranged from 0.164 (for the correlation between the WST-P and ATOP/M-P) to 0.490 (for the correlation between the WST-P and ATOP/M-A). Twelve of the correlations were considered moderate (between 0.3 and 0.6) and three were considered small (less than 0.3). Only the correlation between WST-P and ATOP/M-P was not significant.
Table III.
Pearson’s Correlation Matrix of Measures Included in the Toolkit
| Measure | Wheelchair Confidence-P | Life-space Mobility1 | ATOP Activity2 | ATOP Participation3 | LLDI4 | |
|---|---|---|---|---|---|---|
| WST-P | r | 0.408 | 0.344 | 0.490 | 0.164 | 0.313 |
| Sig. | <0.001 | <0.001 | <0.001 | 0.07 | 0.001 | |
| N | 91 | 124 | 123 | 123 | 120 | |
| Wheelchair Confidence-P | r | 0.341 | 0.300 | 0.415 | 0.251 | |
| Sig. | 0.001 | 0.004 | <0.001 | 0.018 | ||
| N | 91 | 90 | 90 | 89 | ||
| Life-space Mobility | r | 0.250 | 0.388 | 0.441 | ||
| Sig. | 0.005 | 0 | <0.001 | |||
| N | 127 | 127 | 123 | |||
| ATOP: Activity | r | 0.380 | 0.431 | |||
| Sig. | <0.001 | <0.001 | ||||
| N | 127 | 122 | ||||
| ATOP: Participation Score | r | 0.385 | ||||
| Sig. | <0.001 | |||||
| N |
Life-space Mobility Assessment
Assistive Technology Outcomes Project Activity Score
Assistive Technology Outcomes Project Participation Score
Late Life Disability Index
Path Analysis
Given that the correlation between WST-P and ATOP/M-P was not significant, this path was excluded from the model tested. The initial overall Chi square for the model was poor (Chi-square = 28.386, degrees of freedom = 4, p< 0.001) the CMIN/DF was 7.1, the RMSEA was 0.07 and the NFI was 0.98, which indicated problems with model fit. Modification indices (MI) suggested including a path of covariance between the error terms for ATOP/M-A and ATOP/M-P (MI= 18.972, expected parameter change= −9.312). When this change was made the model fit improved substantially (Chi-square = 4.137, degrees of freedom = 2, p = 0.126). For this final model the CMIN/DF was 2.069, the RMSEA was 0.029 and the NFI was 0.998, which indicated good model fit. Given the proportion of participants with missing WheelCon-P data we re-ran the analysis without imputed values. The results remained almost identical except for the path between perceived difficulty with participation (ATOP/M-P) and frequency of participation (LLDI), which became non-significant (p=0.178).
Table IV describes the standardized β weights, standard error, and critical ratios for each path in the model in descending order based on their β weights. Eight of the paths had p value of ≤0.001, one path had a p value of 0.02, and another had a p value of 0.03. The association was strongest between ATOP/M-Participation and LSA.
Table IV.
Beta Weights, Standard Error and Critical Ratios of Paths Included in the Model.
| β | S.E.1 | C.R.2 | p | |||
|---|---|---|---|---|---|---|
| ATOP/M-Participation3 | ---> | LSA | .587 | .052 | 11.317 | >.001 |
| ATOP/M-Activity4 | ---> | LLDI5 | .554 | .046 | 12.020 | >.001 |
| WST-P6 | ---> | LSA | .387 | .043 | 8.973 | >.001 |
| WheelCon-P7 | ---> | WST-P | .302 | .020 | 15.266 | >.001 |
| WheelCon-P | ---> | ATOP/M-Participation | .225 | .018 | 12.392 | >.001 |
| WST-P | ---> | ATOP/M-Activity | .198 | .011 | 17.198 | >.001 |
| LSA8 | ---> | LLDI | .167 | .014 | 12.038 | >.001 |
| ATOP/M-Participation | ---> | LLDI | .130 | .027 | 4.883 | >.001 |
| WheelCon-P | ---> | LSA | .095 | .032 | 3.016 | .003 |
| WheelCon-P | ---> | ATOP/M-Activity | .028 | .009 | 3.149 | .002 |
| ATOP/M-Activity | ---> | ATOP/M-Participation | .081 | .110 | .734 | .463 |
| ATOP/M-Activity | ---> | LSA | −.082 | .100 | −.821 | .412 |
Standard Error
Critical Ratios
Assistive Technology Outcomes Measure Participation Score
Assistive Technology Outcomes Measure Activity Score
Late Life Disability Index
Wheelchair Skills Test for power wheelchair users
Wheelchair Use Confidence Scale for power wheelchair users
Life Space Assessment
Figure II presents the results of the path analysis for the model. All, except two paths were as anticipated. Neither the path between ATOP/M-A and LSA nor the path between ATOP/M-A and ATOP/M-P were significant (p= 0.412 and p=0.463, respectively); but the covariance between the error terms for the latter measures was significant (p<0.001), which suggests these variables reflect an underlying latent construct. This model explained almost one-third of the variation in participation frequency scores.
Figure II.
Empirical Relationship among Variables Included in the Power wheelchair Toolkit
ATOP/M = Assistive Technology Outcome Profile, Range: 0–100
LLDI = Late Life Disability Index, Range: 16–80
LSA = Life-space Assessment, Range: 0–120
WheelCon-P = Wheelchair Confidence Scale for Power Wheelchair Users, Range: 0–100
WST-P = Wheelchair Skills Test for Power Wheelchair Users, Range: 0–100
*** = p<0.001
** = p≥0.001, p<0.01
* = p≥0.01, p <0.05
Numbers in the upper right hand corner of each represent the proportion of variance explained
Number along each line indicate the standardized Beta weight.
DISCUSSION
We accomplished our goal of evaluating the relationships among the outcome measures in our power wheelchair outcomes toolkit. The absence of collinearity suggests that the measures are complementary in nature, and provide unique information related to power wheelchair use, not just in terms of more objective measures of frequency and capacity, but also more subjective measures of perceived difficulty.
The results of the path analysis provide empirical support for our hypothesized model. Scores from the ATOP had the strongest associations with life-space mobility and participation frequency. This is in keeping with previous research, which found perceived limitations and participation frequency were moderately correlated among non-fallers and one time only fallers (35). On one hand, ATOP/M-A scores were strongly associated with frequency of participation but were not significantly associated with life space mobility. On the other hand, ATOP/M-P scores were strongly associated with life space mobility and, to a lesser extent, with frequency of participation. It may be that perceived difficulty with physical performance and instrumental activities of daily living reflects a hierarchical relationship between activity and participation. It may also reflect the content of the measures, as the instrumental activities of daily living (IADLs) included in ATOP/M-A match many of the items found in the LLDI. The later explanation seems more compelling, given that the third strongest association was between WST-P and LSA scores. The WST- tends to be moderately to strongly correlated with functional status measures like the Functional Independence Measure (36, 37). In this regard, it seems that wheelchair skills, which likely reflect functional ability, are associated with life space mobility. However, it should be emphasized that perceived difficulty in physical performance and IADLs when using one’s mobility device (measured via the ATOP/M-A) is a different construct than functional ability itself. Scores on the ATOP/M-P might be more strongly related to LSA, as those who perceive fewer limitations in work and social related roles may be more active and mobile in their communities.
A variety of significant associations were identified between the WheelCon-P and other measures in the toolkit. As anticipated, wheelchair confidence was associated with wheelchair skills (WST) and had the fourth strongest association. Similar moderate correlations between wheelchair confidence and objective wheelchair skills have been observed among manual wheelchair users. (38, 39). Wheelchair confidence was also associated with perceived difficulty in participation (ATOP/M-P) and had he fifth strongest association. This association is not surprising as many of the WheelCon-P items are about negotiating environmental obstacles (often required to participate in community activities), performing activities in the community, as well as managing social situations. There was a small but significant association between the WheelCon-P and ATOP/M-A, which likely reflects the WheelCon-P items related to performing activities in the wheelchair. Similarly, there was a small but significant association between the WheelCon-P and life-space mobility (LSA). In this regard, WheelCon-P scores may have a direct influence on life space mobility, in addition to the indirect influence they have via wheelchair skills. The relationship among wheelchair confidence, wheelchair skills and life-space mobility is not unexpected, because self-efficacy has been hypothesized to moderate the relationship between capacity and performance (26). A similar relationship among wheelchair skills, life-space mobility and frequency of participation has been found among facility residents who use wheelchairs as their primary means of mobility (20, 39).
Three paths were not as we anticipated in the model. First, wheelchair skills were not significantly correlated with ATOP participation, and therefore this path was excluded from the model we tested. This is likely because the latter tool focuses on perceived difficulty with productive roles and leisure, whereas the WST-P includes more functionally related items on wheelchair maneuvering over different surfaces, negotiating obstacles and transfers in and out of the device. Second, the path between perceived difficulty performing activity and life-space mobility was not significant, which likely reflects the weak correlation (r=0.25) between these measures. The strength of this association may reflect the limited overlap between how these constructs were measured, in that the sub-scales that comprise ATOP/M-A include physical performance (e.g. difficulty walking, running, jumping, transferring) and IADLs (e.g. difficulty preparing meals, doing housework), whereas life-space mobility measures the frequency and extent of mobility (16). Although the path between the two subscales of the ATOP - perceived difficulty performing activity and perceived difficulty performing participation - was not significant, the covariance between the error terms of the ATOP sub-scales suggests that the two variables are functioning together like a single latent variable.
The results of this study suggest that the power wheelchair outcomes toolkit provides useful information about the outcomes of power wheelchair use and potential factors associated with them. Although causation cannot be assumed in light of the cross-sectional nature of the data, the findings suggest areas for potential interventions. The importance of wheelchair skills training seems relatively intuitive in terms of its potential influence on mobility and ultimately participation. By improving wheelchair confidence, users may develop the self-efficacy needed to implement and to integrate into practice the wheelchair skills they have the capacity to perform. Interventions aimed at addressing barriers in the social environment, either by training power mobility users or through public awareness campaigns may also be considered. This is important, given that both wheelchair skills and wheelchair confidence are modifiable factors that can be improved with training (21, 40, 41). Although it may be that perceived limitations in participation are related to frequency of participation, a self-fulfilling prophecy might also be in effect. So interventions that attempt to increase users’ internal locus of control might conceivably increase their participation. However, the efficacy of these aforementioned interventions would need to be confirmed with future empirical research.
Limitations of the Toolkit/Model
Some limitations of the toolkit/model need to be identified. The measures included in the current toolkit are not exhaustive, and do not include other potentially relevant variables such as device satisfaction, psychosocial impact, wheelchair fit, or measures of physical or social barriers to power mobility use, which may also be helpful in predicting the frequency of participation. Such measures may also be useful to identify areas where additional interventions might be beneficial. As well, although the LLDI represents a useful generic measure, participation may vary considerably from person to person. In this regard, a more client-specific measure of participation, like the Wheelchair Outcome Measure (42) may be helpful to identify areas of participation that are most relevant to individual power mobility users. Finally, although completion of the toolkit would take additional time, as most are self-report measures, and a self-report version of the WST-P is available, these could be completed prior to a clinic visit.
Study limitations
Several limitations of the study should be noted. A social desirability bias may have influenced results from self-report measures. Although the sample size was sufficient to conduct the analyses, a larger sample would have increased the power of the study and decreased the likelihood of type I error. Furthermore, given the nature of path analysis, it is not possible to model bidirectional relationships, which may be the case for many of the relationships in the model. Finally, participants represent a sample of convenience and results may not generalize to other power wheelchair users.
Future research
The study lays the groundwork for additional research in this area. With a larger sample, factor analysis could be used to identify the latent constructs that are being evaluated with these measures to detect items that offer limited contributions. Further research is needed to study whether these associations remain stable over time. Finally, intervention studies are needed to determine whether the associations identified are causal in nature.
CONCLUSION
This study provides some empirical support for the measures included as part of the power wheelchair outcomes toolkit. They appear to provide complementary information on constructs related to power wheelchair use. Findings suggest that interventions aimed at improving wheelchair confidence and wheelchair skills may decrease perceived difficulty in participation and improve life-space mobility and frequency of participation. Further research is needed to verify the effectiveness of these interventions and to extend the toolkit so that it includes measures that capture more contextual factors
Acknowledgments
Funding sources and related paper presentations
The Canadian Institutes of Health Research (CIHR) CanWheel Emerging team in Wheeled Mobility for Older Adults supported this work (grant number AMG 100925-1). Personal support was provided to Dr. Mortenson via a Banting post-doctoral fellowship. Dr. Routhier was supported by a Fonds de recherche du Québec - Junior Scholar Award. Dr. Rushton was supported by a CIHR Institute of Aging Fellowship.
ABBREVIATIONS
- ATOP/M-A
Assistive Technology Outcomes Profile for Mobility - Activity
- ATOP/M-P
Assistive Technology Outcomes Profile for Mobility - Participation
- CMIN/DF
Chi-square, minimum sample discrepancy function
- IADLs
Instrumental skills of daily living
- LLDI
Late Life Disability Index
- LSA
Life-space Assessment
- NFI
Normed Fit Index
- RMSEA
Root mean square error of approximation
- WheelCon-P
Wheelchair Use Confidence Scale for powered mobility users
- WST-P
Wheelchair Skills Test for powered wheelchair users
References
- 1.Statistics Canada. The 2006 participation and activity limitation survey: Disability in Canada. Government. Ottawa, ON: Statistics Canada; 2006. Report No.: 89-628-X. [Google Scholar]
- 2.Seeman TE, Merkin SS, Crimmins EM, et al. Disability trends among older Americans: National health and nutrition examination surveys, 1988–1994 and 1999–2004. Am J Public Health. 2010;100(1):100–7. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gardener EA, Huppert FA, Guralnik JM, et al. Middle-Aged and Mobility-Limited: Prevalence of disability and symptom attributions in a national survey. J Gen Intern Med. 2006;21(10):1091–6. doi: 10.1111/j.1525-1497.2006.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batavia M. The wheelchair evaluation: A clinician’s guide. Mississauga, ON: Jones & Bartlett Learning; 2009. [Google Scholar]
- 5.Mortenson WB, Miller WC, Boily J, et al. Perceptions of power mobility use and safety within residential facilities. Can J Occup Ther. 2005;72(3):142–52. doi: 10.1177/000841740507200302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Auger C, Demers L, Gelinas I, et al. Powered mobility for middle-aged and older adults: Systematic review of outcomes and appraisal of published evidence. Am J Phys Med Rehabil. 2008;87(8):666–80. doi: 10.1097/PHM.0b013e31816de163. [DOI] [PubMed] [Google Scholar]
- 7.Mortenson WB, Miller WC. The wheelchair procurement process: Perspectives of clients and prescribers. Can J Occup Ther. 2008;75(3):167–75. doi: 10.1177/000841740807500308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garber SL, Bunzel R, Monga TN. Wheelchair utilization and satisfaction following cerebral vascular accident. J Rehabil Res Develop. 2002;39(4):521–34. [PubMed] [Google Scholar]
- 9.Mortenson WB, Hurd Clarke L, Best K. Prescribers’ experiences with powered mobility prescription among older adults. Am J Occup Ther. 2013;67(1):100–7. doi: 10.5014/ajot.2013.006122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hastings J, Robins H, Griffiths Y, et al. The differences in self-esteem, function, and participation between adults with low cervical motor tetraplegia who use power or manual wheelchairs. Arch Phys Med Rehabil. 2011;92(11):1785–8. doi: 10.1016/j.apmr.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 11.Sund T, Iwarsson S, Anttila H, Brandt A. Effectiveness of Powered Mobility Devices in Enabling Community Mobility-Related Participation: A Prospective Study Among People With Mobility Restrictions. Phys Med Rehabil. 2015:1–12. doi: 10.1016/j.pmrj.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Harris F. Conceptual issues in the measurement of participation among wheeled mobility device users. Disabil Rehabil Assist Technol. 2007;2(3):137–48. doi: 10.1080/17483100701374363. [DOI] [PubMed] [Google Scholar]
- 13.Cook AM, Hussey SM. Assistive Technologies Principles and Practice. St Louis: Mosby; 2002. Seating systems as extrinsic enablers for assistive technologies. [Google Scholar]
- 14.World Health Organization. Towards a common language for functioning, disability and health: ICF. Geneva: WHO; 2002. pp. 1–23. [Google Scholar]
- 15.Routhier F, Claude V, Johanne D, Sylvie N. Mobility of wheelchair users: a proposed performance assessment framework. Disabil Rehabil. 2003;25(1):19–34. [PubMed] [Google Scholar]
- 16.Kirby RL, Smith C, Parker K, et al. Wheelchair Skills Test Manual Version 4.2. Available from: http://www.wheelchairskillsprogram.ca/eng/documents/WST_Manual_version_4.2.1_approved.pdf. [Updated April 3 2013; November 4, 2014]
- 17.Jette AM, Haley SM, Coster WJ, et al. Late life function and disability instrument I. development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci. 2002;57(4):M209–16. doi: 10.1093/gerona/57.4.m209. [DOI] [PubMed] [Google Scholar]
- 18.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51(11):1610–4. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 19.Hammel J, Southall K, Jutai J, et al. Evaluating use and outcomes of mobility technology: A multiple stakeholder analysis. Disabil Rehabil Assist Technol. 2013;8(4):294–304. doi: 10.3109/17483107.2012.735745. [DOI] [PubMed] [Google Scholar]
- 20.Mortenson WB, Miller WC, Backman CL, et al. Association between mobility, participation, and wheelchair-related factors in long-term care residents who use wheelchairs as their primary means of mobility. J Am Geriatr Soc. 2012;60(7):1310–5. doi: 10.1111/j.1532-5415.2012.04038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sakakibara BM, Miller WC, Souza M, et al. Wheelchair skills training to improve confidence with using a manual wheelchair among older adults: A pilot study. Arch Phys Med Rehabil. 2013;94(6):1031–7. doi: 10.1016/j.apmr.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samuelsson K, Wressle E. Powered wheelchairs and scooters for outdoor mobility: A pilot study on costs and benefits. Disabil Rehabil Assist Technol. 2013;9(4):330–4. doi: 10.3109/17483107.2013.827244. [DOI] [PubMed] [Google Scholar]
- 23.Löfqvist C, Pettersson C, Iwarsson S, et al. Mobility and mobility-related participation outcomes of powered wheelchair and scooter interventions after 4-months and 1-year use. Disabil Rehabil Assist Technol. 2012;7(3):211–8. doi: 10.3109/17483107.2011.619224. [DOI] [PubMed] [Google Scholar]
- 24.Auger C, Demers L, Gélinas I, et al. Life-space mobility of middle-aged and older adults at various stages of usage of power mobility devices. Arch Phys Med Rehabil. 2010;91(5):765–73. doi: 10.1016/j.apmr.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 25.Pettersson I, Ahlström G, Törnquist K. The value of an outdoor powered wheelchair with regard to the quality of life of persons with stroke: A follow-up study. Disabil Rehabil Assist Technol. 2007;19(3):143–53. doi: 10.1080/10400435.2007.10131871. [DOI] [PubMed] [Google Scholar]
- 26.Bandura A. Self-efficacy: The exercise of control. New York, NY: W.H. Freeman; 1997. [Google Scholar]
- 27.Sakakibara BM, Miller WC, Eng JJ, et al. Preliminary examination of the relation between participation and confidence in older manual wheelchair users. Arch Phys Med Rehabil. 2013;94(4):791–4. doi: 10.1016/j.apmr.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rushton PW, Demers L, Miller WC, et al. Overview of a power wheelchair outcomes tool kit. Workshop at the Annual Rehabilitation Engineering and Assistive Technology Society of North America Conference; June 20–24; Seattle, WA. 2013. [Google Scholar]
- 29.Rushton PW, Miller WC, Demers L Canwheel Research Team. Measuring power wheelchair outcomes: Psychometric properties of a new toolkit. 41st annual scientific and educational meeting of the Canadian Association on Gerontology; October 18–20; Vancouver, BC. 2012. [Google Scholar]
- 30.Auger C, Demers l, Gélinas I, et al. Development of a French-Canadian version of the Life-Space Assessment (LSA-F): content validity, reliability and applicability for power mobility device users. Disabil Rehabil Assist Technol. 2009;4(1):31–41. doi: 10.1080/17483100802543064. [DOI] [PubMed] [Google Scholar]
- 31.Kline RB. Principles and practice of structural equation modeling. 2. New York: Guilford Press; 2005. [Google Scholar]
- 32.Heitjan DF, Srabashi B. Distinguishing “Missing at Random and “Missing Completely at Random”. Am Stat. 1996;50(3):207–213. [Google Scholar]
- 33.Byrne B. A primer of LISREL: Basic applications and programming for confirmatory factor analytic models, 1989. New York, NY: Springer; 1994. [Google Scholar]
- 34.Sivo SA, Fan X, Witta EL, et al. The search for” optimal” cutoff properties: Fit index criteria in structural equation modeling. J Exp Educ. 2006;74(3):267–88. [Google Scholar]
- 35.Melzer I, Kurz I. Self reported function and disability in late life: A comparison between recurrent fallers and non-fallers. Disabil Rehabil. 2009;31(10):791–8. doi: 10.1080/09638280802309384. [DOI] [PubMed] [Google Scholar]
- 36.Mortenson WB, Miller WC, Backman CL, et al. Predictors of mobility among wheelchair using residents in long-term care. Arch Phys Med Rehabil. 2011;92(10):1587–93. doi: 10.1016/j.apmr.2011.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kirby RL, Dupuis DJ, MacPhee AH, et al. The Wheelchair Skills Test (version 2.4): measurement properties. Arch Phys Med Rehabil. 2004;85:794–804. doi: 10.1016/j.apmr.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 38.Sakakibara BM. Towards an understanding of self-efficacy with using a manual wheelchair [dissertation] British Columbia: University of British Columbia; 2013. [Google Scholar]
- 39.Rushton PW, Miller WC, Kirby RL, et al. Measure for the assessment of confidence with manual wheelchair use (WheelCon-M) version 2.1: Reliability and validity. J Rehabil Med. 2013;45(1):61–7. doi: 10.2340/16501977-1069. [DOI] [PubMed] [Google Scholar]
- 40.Best KL, Kirby RL, Smith C, et al. Wheelchair skills training for community-based manual wheelchair users: a randomized controlled trial. Arch Phys Med Rehabil. 2005;86(12):2316–2323. doi: 10.1016/j.apmr.2005.07.300. [DOI] [PubMed] [Google Scholar]
- 41.Mountain AD, Kirby RL, Smith C, et al. Powered wheelchair skills training for persons with stroke: a randomized controlled trial. Am J Phys Med Rehabil. 2014;93(12):1031–1043. doi: 10.1097/PHM.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 42.Mortenson WB, Miller WC, Miller-Pogar J. Measuring wheelchair intervention outcomes: Development of the wheelchair outcome measure. Disabil Rehabil Assist Technol. 2007;2(5):275–85. doi: 10.1080/17483100701475863. [DOI] [PMC free article] [PubMed] [Google Scholar]