Abstract
Objective: This article describes the contributions of medical librarians, as members of the Family Physicians' Inquiries Network (FPIN), to the creation of a database of clinical questions and answers that allows family physicians to practice evidence-based medicine using high-quality information at the point of care. The medical librarians have contributed their evidence-based search expertise and knowledge of information systems that support the processes and output of the consortium.
Methods: Since its inception, librarians have been included as valued members of the FPIN community. FPIN recognizes the search expertise of librarians, and each FPIN librarian must meet qualifications demonstrating appropriate experience and training in evidence-based medicine. The consortium works collaboratively to produce the Clinical Inquiries series published in family medicine publications.
Results: Over 170 Clinical Inquiries have appeared in Journal of Family Practice (JFP) and American Family Physician (AFP). Surveys have shown that this series has become the most widely read part of the JFP Website. As a result, FPIN has formalized specific librarian roles that have helped build the organizational infrastructure.
Conclusions: All of the activities of the consortium are highly collaborative, and the librarian community reflects that. The FPIN librarians are valuable and equal contributors to the process of creating, updating, and maintaining high-quality clinical information for practicing primary care physicians. Of particular value is the skill of expert searching that the librarians bring to FPIN's products.
BACKGROUND
The Family Physicians' Inquiries Network (FPIN) is an international, not-for-profit consortium of academic family physicians, family medicine residency programs and departments, health sciences librarians, medical informatics specialists, computer scientists, other primary care providers, and consultants dedicated to using information technology to improve health care. FPIN authors provide brief evidence-based answers to actual clinical questions from practicing clinicians. These questions are voted on by their peers for their clinical value and are published with answers as the Clinical Inquiries in the Journal of Family Practice (JFP) and the American Family Physician (AFP). FPIN emphasizes the promotion of evidence-based practice and provides opportunities to faculty and residents in family medicine residency programs to participate in scholarly activity through writing and reviewing Clinical Inquiries. FPIN is endorsed by a number of family medicine organizations, including the American Academy of Family Physicians (AAFP).
History of Family Physicians' Inquiries Network (FPIN)
FPIN was conceptualized in May 1998 as part of a grant application to AAFP from the Department of Family and Community Medicine at the University of Missouri–Columbia (MU). The grant supported the establishment of a family medicine–based research center at MU: the Center for Family Medicine Science. In April 2001, FPIN was incorporated as a self-governing mutual benefit corporation with a governing board and president, independent of MU's Center for Family Medicine Science. MU became the first of seven initial FPIN founding members, who made a five-year commitment and contributed the equivalent of one full-time physician per year in effort (Appendix A). FPIN has thrived as a grassroots community of health care professionals and health sciences librarians with a goal of creating change in the culture of medical practice.
FPIN community mission
FPIN is a community of inclusion that is committed to engaging every organization and all qualified individuals who wish to join. At the present time, the primary participants in the network are family medicine departments, family medicine residency programs, and health sciences librarians and health sciences libraries. As the community grows, participants benefit from the contributions of practitioners asking questions, providing clinical perspective, and participating in research. A primary focus is on writing reviews and publishing them in the Clinical Inquiries series. In addition, new initiatives are underway, including new types of publications, collaboration with other medical information providers, and development of an information delivery system for FPIN's products. Future goals include answering critical questions necessary to translate research into practice at the point of care and tailored to the needs of primary care physicians and practice-based research networks. A plan for identifying questions that necessitate further research before an adequate answer can be written will provide the family medicine community with direction for additional research opportunities. These efforts will attract a broader membership and further expand the FPIN community as a whole.
METHODOLOGY
Librarian involvement in FPIN had its roots in the MU Family and Community Medicine Departmental Library, the Missouri Integrated Advanced Information Management Systems Project, and the MU School of Medicine curriculum. The MU Family and Community Medicine Department had long ago integrated librarian support into its culture, so inclusion of librarians in the development of the Center for Family Medicine Science was natural. The Family Medicine Department had a long history of study in question framing, query development, and question categorization. The early stages of what would become FPIN centered on the study of question refinement and time requirements for finding answers to questions [1–7]. Librarians participated in these efforts, which were published in a paper that became known as the “Just-in-Time” study [8]. Out of that study, the physicians developed an appreciation for information-seeking skills and the time required to find the best information.
The FPIN librarian team emerged from a core group of three MU librarians, who met to discuss issues relevant to creating a more effective method for information delivery at the point of care. As the form of publishing Clinical Inquiries developed, the librarians developed a process that yielded uniform quality and produced bibliographies based on a search hedge. Librarians from other institutions tested the model, and their input led to refinements. By October 2001, the team was ready to recruit other interested librarians, and they invited participation through a fall meeting of three chapters of the Medical Library Association (Midcontinental, South Central, and Southern Chapters).
An effort of this magnitude could not be accomplished without consortium staff. In September 2001, a membership coordinator was hired, and, in February 2002, the first librarian was hired. The librarian's responsibilities were split between librarian support and managing editor functions to facilitate publication of the Clinical Inquiries. The role of executive director grew from that of membership coordinator and is now supported by two additional staff members. These staff members provide support for the activities of the FPIN librarian community as well.
A significant landmark for the FPIN librarian community was the recommendation by an ad hoc group of librarians, informaticians, and physicians from the University of Missouri and the University of Washington, approved by the editorial team in spring 2002, to list librarians as coauthors of the Clinical Inquiries. This decision was based on the concept that expert searching by librarians added a quality component to the entire process. Performing systematic searches of the literature required a good deal more time than did the typical clinical question search, thus librarian searchers received recognition for their contributions.
Pairing the librarians with clinician authors at the same institution is a logical way to connect the librarians and their institutions' family medicine residency programs. This local partnering strengthens the librarians' service to a constituent group and frequently leads to activities that further enhance their relationship. FPIN also welcomes participation from qualified librarians whose family medicine programs have no FPIN ties. These librarians are partnered with clinician authors in other institutions and use email and telephone to carry out their work. The role of the librarian as expert searcher has led to additional roles such as process design consultant, instructor, Web page editor, and partner with clinicians in the transition to a new culture of evidence-based practice.
Organization of the librarian community
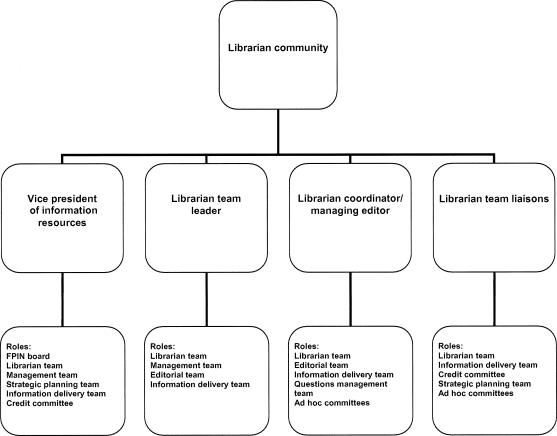
The FPIN librarian community consists of volunteer librarians from a number of institutions (Figure 1). They are geographically dispersed and have relationships based on a sense of common purpose and collegiality. Communication is facilitated through an email discussion list; coordination of the Clinical Inquiries is provided by the librarian coordinator/managing editor; and planning is carried out by the librarian team and their link to the FPIN board through the vice president for information resources.
Figure 1.
Organization of the Family Physician's Inquiries Network librarian community
The extent to which librarians have been woven into the structure of the FPIN organization is evidence of the librarians' value. The vice president for information resources is a library director at a resource library of the National Network of Libraries of Medicine (NN/ LM). She is a member of the FPIN board, the management team, the librarian team, the credit committee, the strategic planning committee, and the information delivery system committee (IDS). She participates in infrastructure development and policy decisions and serves as advisor to the librarian team.
The librarian team leader, a practicing clinical librarian in family medicine, provides leadership for the activities of the librarian team, which meets on a monthly basis via teleconference. She is responsible for training and mentoring new FPIN librarians as they become accustomed to their roles in FPIN, and she coordinates all FPIN librarian activities related to development of the evidence-based search hedges and search processes in support of the Clinical Inquiries. The team leader works closely with the vice president for information resources and the librarian coordinator/managing editor to help guide the policies and work of the librarian community. She is a member of the FPIN management team, the editorial team, and the IDS executive committee.
FPIN also supports a full-time librarian coordinator/managing editor, who performs a broad range of functions, including: assigning and tracking librarians, expert searching to support the Clinical Inquiries, editing and reviewing references, indexing the Clinical Inquiry topics, and archiving all of the librarians' search strategies. In this role, she supports the work of the expert searchers. She assumes a more comprehensive role as managing editor of the production process from author assignment to the point at which the FPIN associate editor receives the completed work. While the librarian coordinator and managing editor roles are quite distinct, the two areas do overlap, which greatly facilitates the entire process. As a librarian, expert searcher, and managing editor, this individual adds to quality assurance in identifying issues concerning potential accuracy and publication rights at the outset. The librarian coordinator/managing editor serves on the librarian team, the editorial team, the IDS, and several ad hoc committees.
The librarian team currently consists of these three individuals joined by one liaison from each of the founding member departments and one librarian from the community at large. This group of ten individuals has been crucial to the development of librarians' processes and initiatives. The team emerged from the original core group that grew to include a wider range of voices from the community and achieved a dual purpose: providing broad-based input into the growth of the librarian community and strengthening librarian involvement in the consortium. Members of the team also participate in consortium-wide activities, serving on the IDS, the strategic planning committee, and the credit committee.
RESULTS
The FPIN librarian community has grown over the last four years to include more than fifty members from all parts of the country as well as the United Kingdom and Canada and from both academic health sciences libraries and hospital libraries. Ninety-four percent of these librarians are associated with departments that are FPIN members; others are affiliate members whose institutions are not FPIN members. One librarian works for the BMJ Publishing Group's Clinical Evidence, providing a conduit for information exchange between the two groups and giving FPIN its first international participant. The recent addition of McGill University as a founding member brings Canadian librarians into FPIN as well.
All librarians must meet the qualifications of education and experience described on the FPIN Website: two years of experience searching electronic databases and Internet resources, including MEDLINE, applicable to FPIN searches; a basic understanding of evidence-based medicine; experience performing clinically oriented searches for point-of-care questions; and a master's degree in library science. Because these librarians are experienced searchers who have a foundational understanding of evidence-based medicine, they create a strong cadre of support and quality for the Clinical Inquiries.
For some librarians, participation in FPIN has led to other opportunities, and these activities are regularly reported at the librarian team monthly meetings. Librarians in North Carolina and Washington have become involved in departmental instruction in evidence-based medicine and the process of writing evidence-based summaries. The family medicine department at one institution has begun to support a portion of a librarian's salary, and this practice is being considered by others. The FPIN librarian team leader has copresented continuing medical education programs for evidence-based medicine alongside family medicine faculty at regional and national meetings. Both the FPIN librarian team leader and the FPIN librarian coordinator/managing editor team-taught “Writing Clinical Inquiries” with physicians at the 2003 annual meeting of the North American Primary Care Research Group (NAPCRG).
The University of Washington's PrimeAnswers project <www.primeanswers.org> has partnered with FPIN in creating the portal for the FPIN Website. PrimeAnswers, a National Library of Medicine (NLM) information technology grant project, is a simple, context-sensitive Web interface to a filtered set of content designed to make it easier and faster for primary care physicians to find answers to questions in their daily management of patients. The FPIN portal has been based on the PrimeAnswers' research and development, and this effort is acknowledged at the portal. Librarians elsewhere are beginning to report that their participation in the consortium is a catalyst for improved relations with their local family medicine departments, and they have gained local recognition for the librarians' search and evidence-based medicine expertise.
CLINICAL INQUIRIES
More than 170 Clinical Inquiries have been published in JFP since the series began in January 2001. From an initial offering of two per month, the number is six per month as of this writing, with a goal of eight to ten per month in 2005. At any given time, more than fifty Clinical Inquiries are in various stages of the writing or editing process. An important distinction is that, while Clinical Inquiries are not considered to be systematic reviews, they are produced using a systematic, evidence-based, expert search process.
Librarian coauthors for Clinical Inquiries find that their responsibilities encompass a good deal more than simply doing a search. As a coauthor, the FPIN librarian is obligated to read the entire manuscript and be prepared to assume public accountability for the librarian's knowledge of the search results, the description of the search methods used, the manuscript's content as it relates to the interpretation of the search results by the author, the accuracy of the references, and any other content in the document that the librarian feels qualified to address. Coauthorship recognizes that the librarian's search expertise contributes value through standardization and knowledge of database structures and information retrieval.
Clinician authors review the librarian's search and the best articles it has retrieved as they write the Clinical Inquiries. They have two months to write each Clinical Inquiry and must assign a grade from the Oxford Centre for Evidence Based Medicine to the presented evidence. The format of each Clinical Inquiry consists of a brief, succinct “Evidence-based Answer,” which presents the bottom line conclusion up front, followed by the lengthier “Evidence Summary,” which reviews and describes the supporting studies. The final portion, “Recommendations from Others,” generally summarizes appropriate guidelines or consensus statements. The entire text is approximately 600 to 700 words. Each Clinical Inquiry goes through a non-blinded, peer-review process using volunteer peer reviewers; each also has a brief published companion piece, the “Clinical Commentary,” which applies the information to practice. Appendix B shows a sample Clinical Inquiry.
The librarian coordinator/managing editor, assistant editor, and associate editor review the work for accuracy and completeness. The assistant and associate editor roles are held by members of the consortium as part of a credit system, which supports the future sustainability of the effort. Institutions base their membership contribution annually on a mix of work effort and funding, with the incentive that the greater the effort, the lower the membership fee, up to a given point. While FPIN currently publishes in the traditional journal outlets, this content is copyrighted by FPIN and is made available through other electronic means. In this way, FPIN makes a contribution to the changing scholarly communication paradigm.
In the development phase of FPIN, the librarian team's goal was to create a systematic approach to literature searching that would achieve a standard of uniformity in retrieval and quality of content. The outcome of this work includes the FPIN systematic search protocol, which outlines the required databases, a uniform search strategy with therapeutic and diagnostic hedges, a systematic search process, and a search summary form to provide a structured report submitted to the clinician author.
Search protocol
FPIN librarians run systematic searches against an established list of databases. This “protocol” includes key evidence-based resources identified by librarians and physicians and consists of two database tiers. The first tier contains the databases required for each search, and the second tier contains recommended, additional databases that may be searched based on the librarian's professional judgment. The librarians who developed the FPIN protocol also sought input from FPIN physicians to ensure that the protocol contained the very best resources for evidence-based content.
Search hedge
The FPIN search strategies are hedges designed for evidence-based retrieval of topics related to diagnosis and therapy. The therapeutic hedge was developed by a core team of librarians at MU, based on the work of McKibbon and Haynes [9, 10]. Over time, the search strategy evolved, and it was implemented while working on Clinical Inquiries with clinician authors.
Once the librarian team was officially organized, it drew upon suggestions from librarian experts at the University of Washington, the University of North Carolina, and the University of Colorado, who provided guidance in the development of the diagnostic hedge [11–14]. Based on this input, both hedges were customized for use by searchers on the PubMed and OVID search systems. The end result was a set of systematic search hedges that a librarian at almost any institution could use to contribute search work to the consortium. Complete information on the hedges and the search protocol is available on the FPIN Website <www.fpin.org>. In addition to the diagnosis and therapy hedges, the team plans to develop MEDLINE hedges for topics related to etiology, harm, and prognosis in the near future.
Search process
The librarians run a comprehensive search in MEDLINE, using the appropriate evidence-based search hedge in combination with Medical Subject Headings (MeSH) terms and text-words. Librarians who have access to Current Contents also have a specific evidence-based search hedge. In other required evidence-based sources, such as the Cochrane Library and Clinical Evidence, the search strategy consists of keywords identified by the searcher. The librarians review the results and structure the output to provide low retrieval with high precision in evidence-based literature.
Search report form
As the systematic search process was developed, it became apparent to the librarian team that a comparable systematic means was necessary for reporting search results, and a search summary form was designed to facilitate reporting. The search summary form is used to provide a means for the librarian to present the search output to the author in a concise, manageable format. This form continues to evolve due to the diverse modes of information delivery that exist in the various institutions where physician-librarian teams work together. For example, the librarians at the University of Washington use a PubMed “cubby” format with links to the full text. This format is different from the Word-based one used by other librarians in the community. An example of the search report form is available on the FPIN Website.
Update process
The librarian team is developing a process to update the published Clinical Inquiries. This effort will include a means for identifying and prioritizing previously published Clinical Inquiries that require updating and then working with the original authors and coauthors as they review the updated literature relevant to their Clinical Inquiries. Currently, the librarian coauthor accepts the responsibility of permanently storing each search strategy for Clinical Inquiries to use in updating, but, with the implementation of the team's update plan, all Clinical Inquiry searches will be stored on a centralized server. An automatic update of each Clinical Inquiry search will be generated, and results will be delivered to the appropriate author, coauthor, and editors. FPIN is launching a new computerized editorial management system that will facilitate systematic generation of updated searches and streamline the updating process. It is anticipated that all Clinical Inquiries will be updated within the next two years.
Clinician and librarian communication
Effective communication with clinician coauthors is a key issue encountered by most librarians. In many instances, librarians work with clinician authors who are located at other institutions throughout the consortium, so maintaining a meaningful flow of correspondence regarding search information can be challenging. To overcome some of these communication challenges, the FPIN librarian coordinator/managing editor makes every attempt to connect librarian searchers with local clinician authors. Additionally, recruitment efforts have been directed at partnering librarians with clinicians at the local level, and this approach has improved communications throughout the production process. Distance, however, is not always a barrier. There are examples of excellent communication between librarian and clinician authors at distant sites that result in successful output. A unique example of this collaborative process was the provision of articles using Loansome Doc to a Clinical Inquiry author who was on active military duty in Iraq.
FPIN LIBRARIAN PROFESSIONAL DEVELOPMENT
In 2002, MU received a grant from NN/LM to further the activities of the FPIN librarian community. Of the project goals, two related specifically to expert searching:
to create an online training package for librarians new to FPIN
to develop continuing education opportunities that can be included in portfolios for professional advancement
To achieve the first goal, a training program has been developed and tested by a small group of new FPIN librarians. The training program, available at the FPIN Website, guides the new librarian through the communication and search process. The training incorporates the search protocol, hedges, and search summary form and uses practical examples based on an actual search question.
As part of the training program, both the librarian team leader and the librarian coordinator/managing editor serve as mentors to review and discuss search issues with new librarian coauthors. This mechanism has produced positive feedback in terms of identifying issues, questions, and stumbling blocks that the novice FPIN librarian might encounter.
As a quality control measure, the librarian team leader reviews the first three searches done by a novice FPIN librarian. This review ensures adherence to the systematic search process. The team leader reviews the search and provides any necessary feedback to the librarian searcher. When a librarian has performed searches for at least three Clinical Inquiries, the search summaries are then sent directly to the librarian coordinator/managing editor.
Continuing education
The work of the consortium depends on highly motivated professionals who have proven experience in continuing education. This experience is demonstrated by the teaching that librarians provide to clinicians and other librarians. Examples include: The FPIN librarian team leader participated in the Medical Library Association's (MLA's) satellite teleconference on expert searching; two FPIN librarian community leaders prepared a workshop on evidence-based medicine for MLA's annual meeting in 2004; and librarian liaisons from three institutions collaborated to create a series of links from the FPIN Website to educational resources for use by clinicians, librarians, and others. The role of the expert searcher is thus providing a foundation for librarians as educators.
All FPIN librarians should have a common understanding of evidence-based medicine and its relevant searching and evaluation techniques. The librarian team is exploring several ideas for professional development in evidence-based medicine, which include participating in relevant course work, continuing education programs, journal clubs, other discussion groups, and online instruction. Several FPIN librarians have solid experience in teaching evidence-based medicine in their institutions and could help define standards for continuing education for librarians.
FUTURE ROLES FOR FPIN LIBRARIANS
Answering clinicians' point-of-care questions through the FPIN database will require a large number of Clinical Inquiries. The consortium has created other publications that appear in AFP and the EBP Newsletter. These publications are shorter in length than the original Clinical Inquiries and have a more focused search of the evidence-based sources. The librarians are engaged in the discussions about the future process and output of the Clinical Inquiries series. New initiatives in FPIN continue to emerge and, with them, opportunities for librarians to be involved and to apply their expertise to support the change of evidence-based medicine from new trend to endorsed practice.
CONCLUSION
FPIN has enhanced the role of the librarian as an expert searcher through its collaborative structure and inclusion of librarians as coauthors for the Clinical Inquiries. New roles for librarians have developed as a result of this experience. The FPIN librarians in general find that their relationships with FPIN clinicians have been enhanced by this collaboration. The recognition of the librarians' value to the FPIN organization has raised the profile of librarianship in an exciting and innovative endeavor.
Acknowledgments
The authors acknowledge the help and support of Bernard Ewigman, whose vision of answering the “little” questions, sparked the development of FPIN. They also thank the FPIN staff.
APPENDIX A
Family Physicians' Inquiries Network (FPIN) institutions
FPIN founding member institutions:
McGill University
* Michigan State University
Oregon Health Sciences University
* SUNY-Upstate Medical University
University of Chicago
* University of Colorado
* University of Missouri–Columbia
* University of North Carolina
* University of Washington
University of Wisconsin
* Wayne State University
* Indicates initial founding member
FPIN librarians are located at the following institutions:
Baylor College of Medicine/Texas Medical Center, Houston, TX
Charlotte Area Health Education Center (AHEC), Charlotte, NC
Christiana Care Health System, Wilmington, DE
Clinical Evidence, BMJ Publishing Group, London, United Kingdom
Coastal AHEC, Wilmington, NC
East Carolina University/Eastern AHEC, Greenville, NC
* Family Physicians' Inquiries Network, Iowa City, IA
Forbes Regional Hospital, Monroeville, PA
Greensboro AHEC, Greensboro, NC
Group Health Cooperative, Seattle, WA
Harborview Medical Center, Seattle, WA
Louisiana State University–New Orleans
McGill University, Montreal, QC, Canada
Medical College of Ohio–Toledo
Medical College of Wisconsin–Milwaukee
* Michigan State University–East Lansing
Mountain AHEC, Asheville, NC
Northwestern AHEC, Winston-Salem, NC
Oregon Health Sciences University–Portland
St. Joseph Regional Medical Center, South Bend, IN
Stanford University, Stanford, CA
Tulane University, New Orleans, LA
* University of Colorado–Denver
* University of Missouri–Columbia
* University of North Carolina–Chapel Hill
University of Texas-Southwestern–Dallas
* University of Virginia–Charlottesville
* University of Washington–Seattle
University of Wisconsin–Madison
Wayne State University, Detroit
* Member of FPIN librarian team
APPENDIX B
Example of a clinical inquiry
This Clinical Inquiry was published in the January 2002 Journal of Family Practice, page 22.
Clinical question
What is the initial approach to the treatment of undifferentiated shoulder pain?
Evidence-based answer
There is some limited evidence supporting the use of nonsteroidal anti-inflammatory drugs (NSAIDs) in the initial treatment of shoulder pain. There is no evidence in support of most other therapies, including intra-articular or subacromial corticosteroid injection, intra-articular NSAID injection, oral corticosteroid treatment, physiotherapy, ultrasound, heat or ice therapy, laser treatment, electrotherapy, and iontophoresis.
Grade B recommendation based on extrapolation from systematic reviews and randomized clinical trials with inconsistent and inconclusive results
Evidence summary
Because of a lack of uniformity in the definition of shoulder disorders and a wide variation in outcomes assessed in clinical trials, there is limited opportunity to compare and pool the results of individual trials. Even when studies define the disorders and outcomes similarly, the heterogeneity of the interventions, timing of outcome assessment, inadequate reporting of results, and small sample sizes limit the inference of specific therapeutic recommendations for shoulder pain.
A recent Cochrane Review concluded that there is little evidence to either support or refute the efficacy of most common interventions for shoulder pain [1]. The pooled analyses of 2 studies of rotator cuff tendinitis suggested that NSAIDs may be superior to placebo in improving the range of abduction, but there was no significant weighted difference between pain scores [2, 3]. Another randomized controlled trial [4] found 14-day treatment with oral NSAIDs superior to placebo for relieving acute shoulder pain (86% vs. 56%; absolute risk reduction 30%; 95% confidence interval, 10%–50%).
A randomized single-blind study of primary care patients reported superiority of manipulative therapy over classic physiotherapy in the treatment of shoulder pain (70% vs. 10% cure rate at 5 weeks) [5]. Manipulative therapy as performed by general practitioners or physiotherapists included mobilization and manipulation of the upper spine and ribs, acromioclavicular joint, and the glenohumeral joint. Classic physiotherapy as performed by physiotherapists included only exercise therapy, massage, and physical applications. For the patients with synovial pain, intra-articular corticosteroid injection was superior to both manipulative therapy and classic physiotherapy (cure rates of 75% vs. 40% and 20%, respectively, at 5 weeks), yet many primary care physicians may not have enough experience to specifically diagnose synovial pain.
Recommendations from others
We found no guidelines, recommendations, or consensus statements from specialty organizations on this topic.
References
1. Green S, Buchbinder R, Glazier R, Forbes A. Interventions for shoulder pain. The Cochrane Library 2001(3). Oxford, UK: Update Software.
2. Petri M, Dobrow R, Neiman R, Whiting-O'Keefe Q, Seamen WE. Randomized, double-blind, placebo-controlled study of the treatment of the painful shoulder. Arthritis Rheum 1987;30:1040–5.
3. Adebajo AO, Nash P, Hazleman BL. A prospective double blind dummy placebo controlled study comparing triamcinolone hexacetonide injection with oral diclofenac 50 mg TDS in patients with rotator cuff tendinitis. J Rheumatol 1990;7:1207–10.
4. Mena HR, Lomen PL, Turner LF, Lamborn KR, Brinn EL. Treatment of acute shoulder syndrome with flurbiprofen. Am J Med 1986;80:141–4.
5. Winters JC, Sobel JS, Groenier KH, Arendzen HJ, Meyboom-de Jong B. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: randomised, single blind study. BMJ 1997;314:1320–5.
Clinical commentary
Most ambulatory patients with primary nontraumatic shoulder pain have rotator cuff tendonitis. Mild, acute disease usually responds to initial rest from movements that aggravate the pain, followed by a gradual return to full activity as tolerated. Time remains a strong ally in this setting. I have found NSAIDs and corticosteroid injections helpful in reducing pain and improving range of motion, but only in the subacute and chronic forms of rotator cuff tendonitis and osteoarthritis. Physiotherapy, although of uncertain analgesic benefit, may minimize the muscular atrophy and loss of flexibility associated with joint injury. The studies above specifically address pain arising from the shoulder joint itself. Pain may also be referred to the shoulder from a remote site (as in atypical angina or other intrathoracic pathology). The initial management of shoulder pain requires consideration of such secondary causes as well.
Author information
Clinical author: David Weismantel
Librarian coauthor: Susan Meadows
Clinical commentator: Nicholas Solomos
Associate editor: Bernard Ewigman
Assistant editor: Erik Lindbloom
Footnotes
* This work was supported in part by a National Network of Libraries of Medicine grant, “Enhancement of the FPIN Librarian Community.”
Contributor Information
Deborah Ward, Email: warddh@missouri.edu.
Susan E. Meadows, Email: MeadowsS@health.missouri.edu.
Joan E. Nashelsky, Email: joan@fpin.org.
REFERENCES
- Ely JW, Osheroff JA, Ebell MH, Chambliss ML, Vinson DC, Stevermer JJ, and Pifer EA. Obstacles to answering doctors' questions about patient care with evidence: qualitative study. BMJ. 2002 Mar 23; 324(7339):710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely JW. Why can't we answer our questions? J Fam Pract. 2001 Nov; 50(11):974–5. [PubMed] [Google Scholar]
- Ely JW, Osheroff JA, Gorman PN, Ebell MH, Chambliss ML, Pifer EA, and Stavri PZ. A taxonomy of generic clinical questions: classification study. BMJ. 2000 Aug 12; 321(7258):429–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely JW, Osheroff JA, Ebell MH, Bergus GR, Levy BT, Chambliss ML, and Evans ER. Analysis of questions asked by family doctors regarding patient care. BMJ. 1999 Aug 7; 319(7206):358–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely JW, Osheroff JA, Ferguson KJ, Chambliss ML, Vinson DC, and Moore JL. Lifelong self-directed learning using a computer database of clinical questions. J Fam Pract. 1997 Nov; 45(5):382–8. [PubMed] [Google Scholar]
- Chambliss ML, Conley J. Answering clinical questions. J Fam Pract. 1996 Aug; 43(2):140–4. [PubMed] [Google Scholar]
- Ely JW, Burch RJ, and Vinson DC. The information needs of family physicians: case-specific clinical questions. J Fam Pract. 1992 Sep; 35(3):265–9. [PubMed] [Google Scholar]
- Alper BS, Stevermer JJ, White DS, and Ewigman BG. Answering family physicians' clinical questions using electronic medical databases. J Fam Pract. 2001 Nov; 50(11):960–5. [PubMed] [Google Scholar]
- McKibbon A, Eady A, and Marks S. PDQ: evidence-based principles and practice. Hamilton, ON, Canada: B. C. Decker, 1999. [Google Scholar]
- Haynes RB, Wilczynski N, McKibbon KA, Walker CJ, and Sinclair JC. Developing optimal search strategies for detecting clinically sound studies in MEDLINE. J Am Med Inform Assoc. 1994 Nov–Dec; 1(6):447–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deville WL, Bezemer PD, and Bouter LM. Publications on diagnostic test evaluation in family medicine journals: an optimal search strategy. J Clin Epidemiol. 2000 Jan; 53(1):65–9. [DOI] [PubMed] [Google Scholar]
- Evidence-based filters for OVID Medline. [Web document]. Rochester, NY: Edward G. Miner Library, University of Rochester, 2002. [rev 5 Mar 2004; cited 19 Mar 2004]. <http://www.urmc.rochester.edu/hslt/miner/digital_library/tip_sheets/OVID_eb_filters.pdf>. [Google Scholar]
- Vincent S, Greenley S, and Beaven O. Clinical evidence diagnosis: developing a sensitive search strategy to retrieve diagnostic studies on deep vein thrombosis: a pragmatic approach. Health Info Libr J. 2003 Sep; 20(3):150–9. [DOI] [PubMed] [Google Scholar]
- Glover J. Searching for the evidence using PubMed. Med Ref Serv Q. 2002 Winter; 21(4):57–65. [DOI] [PubMed] [Google Scholar]