Abstract
Background and aims
Endoscopic resection techniques require use of submucosal injection. The aim of this study was to assess a new solution that combines hyaluronic acid, chondroitin sulfate, and poloxamer 407 for submucosal injection.
Methods
A total of 48 gastric submucosal cushions were created in fresh porcine stomachs using gelafundin (n = 16) or the new solution diluted at 50 % (n = 16), or 80 % (n = 16). The duration of mucosal elevation was measured. In an in vivo model, 10 gastric submucosal cushions were created by injecting 2 mL of the new solution at 80 % and the animal was euthanized 30 minutes after the last injection.
Results
Submucosal cushions with the new solution at 80 % and 50 % concentration lasted longer than with gelafundin (23.13 ± 15.57, 13.1 ± 6.6, 3.94 ± 1.53 minutes, respectively; P = 0.000). In the in vivo study, no damage or necrosis was observed in the mucosa or muscularis propria.
Conclusion
The combination of hyaluronic acid, chondroitin sulfate, and poloxamer 407 produces a long-lasting submucosal cushion and does not seem to induce acute damage in the tissue making it suitable for submucosal injection.
Introduction
Endoscopic mucosal resection (EMR) and submucosal dissection (ESD) are widely used as therapeutic methods for resection of non-polypoid lesions of the gastrointestinal tract, including early cancer. Both techniques require a submucosal injection to separate the lesion from the muscularis propria and thus reduce complications such as thermal injury and perforation 1 . However, available solutions for submucosal injection are not very long lasting, require multiple injections in order to adequately perform a complete ESD or a large EMR, and none have consistently been shown to be more effective or safer than others 2 . Aside from duration, the different compositions and viscosities of these solutions could potentially damage the submucosa and muscularis propria resulting in impaired healing or delayed complications 3 4 5 6 7 .
Recently, a new treatment for gastroesophageal reflux that combines hyaluronic acid, chondroitin sulfate, and poloxamer 407 (Ziverel, Norgine, UK) was approved in Spain. Poloxamers are reverse-phase polymers that undergo a temperature-dependent liquid-to-gel transformation and can be used for medical applications. Poloxamers have also been demonstrated to provide a more durable submucosal cushion in ex vivo and in vivo porcine models 8 . However, there is no information about potential tissue damage by these polymers.
The objective of this study was to assess the efficacy and safety of this new substance as a submucosal injection solution.
Methods
Evaluation of the efficacy
In the ex vivo experiment, a total of 48 gastric submucosal cushions were created in fresh ex vivo porcine stomachs using gelafundin (Gelaspan, Braun, Germany) (n = 16) or Ziverel diluted with saline solution at two different concentrations: 50 % (n = 16) and 80 % (n = 16). Each submucosal injection was performed by injecting 2 mL of solution using a 21-gauge intramuscular needle and the duration of the cushions was measured 9 . The time for the cushion to disappear was recorded using a stopwatch. Timing began immediately after withdrawal of the needle and ended when the bleb had flattened completely 10 . All stomachs were placed on thermal pads at a temperature of 37°C 8 . The investigator was blinded to the type of solution injected.
Evaluation of immediate tissue damage
In the in vivo model, we created 10 submucosal cushions in the upper third of a single pig’s stomach by injecting 2 mL of 80 % Ziverel at separate sites using a standard gastroscope and a 23-gauge catheter injection needle. After a visually adequate submucosal elevation had been achieved, endoclipping was carried out near the injection sites for further identification of the locations. The pig was euthanized 30 minutes after the last injection, and a necropsy was performed 9 . The retrieved stomach was fixed with formalin and was cut at the different injection sites, taking 3-mm-thick slices of each cushion for histology. Paraffin tissue blocks were obtained from each injection site. Afterwards, 2-µm-thick histologic sections from each paraffin block were stained with H&E and examined. The study was approved by the Ethics Animal Committee of Barcelona University.
Statistical analysis
Statistical comparisons between the three groups were made using the Kruskal-Wallis non-parametric test followed by a one-way analysis of variance (ANOVA) for independent data and a Tukey test for post-ANOVA pairwise comparisons. A P value < 0.05 was considered statistically significant. Calculations were performed with SPSS software (SPSS 21.0 for Windows, SPSS, Inc., Chicago, IL, United States).
Results
In the ex vivo study, submucosal cushions created using Ziverel with the two different concentrations lasted longer than those created using gelafundin ( Table 1 , Fig. 1 ). We did not observe any leakage of fluid from the injection puncture with any solution.
Table 1. Duration of the submucosal cushions.
| Gelafundin | 50 % Ziverel | 80 % Ziverel | ANOVA | |
| Time, mean ± SD (range), min | 3.9 ± 1.5 (2 – 7) | 13.1 ± 6.6 (4 – 25) | 23.1 ± 15.6 (7 – 68) | 0.000 1 |
Post-ANOVA test: 80 % Ziverel vs gelafundin, P = 0.000; 80 % Ziverel vs 50 % Ziverel, P = 0.018; 50 % Ziverel vs gelafundin, P = 0.03.
Fig. 1.
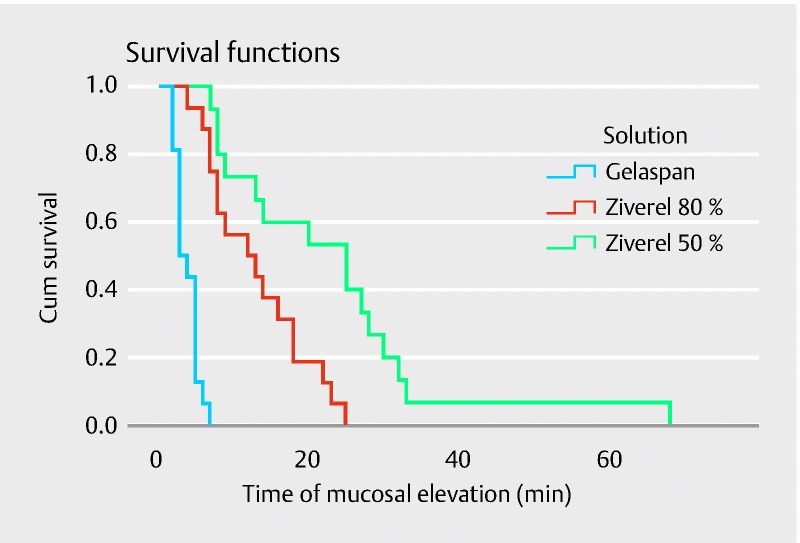
Chronological disappearance of submucosal cushions. Both formulations of Ziverel maintained the mucosal elevation longer than gelafundin ( P = 0.000).
In the in vivo study, the whole procedure lasted 30 minutes from the first injection to the last one. Each submucosal cushion had a median duration of 49.5 minutes (range 35 – 65 minutes) before the animal was euthanized. All of the cushions apart from the first one were macroscopically visible at the time of necropsy ( Fig. 2 ). Macroscopic examination of the specimens showed a gross submucosal bleb in them all apart from the first one ( Fig. 3 ). The most significant histological change was edema and vascular ectasia in the submucosa which progressively decreased with time after injection ( Fig. 4 ). Mucosal changes consisted of mild edema and vascular ectasia. No muscle damage or necrosis was identified in any section.
Fig. 2.

The retrieved stomach is stretched flat on a cork board with pins. It was possible to identify the 10 endoclips that indicate the sites of the injections.
Fig. 3.
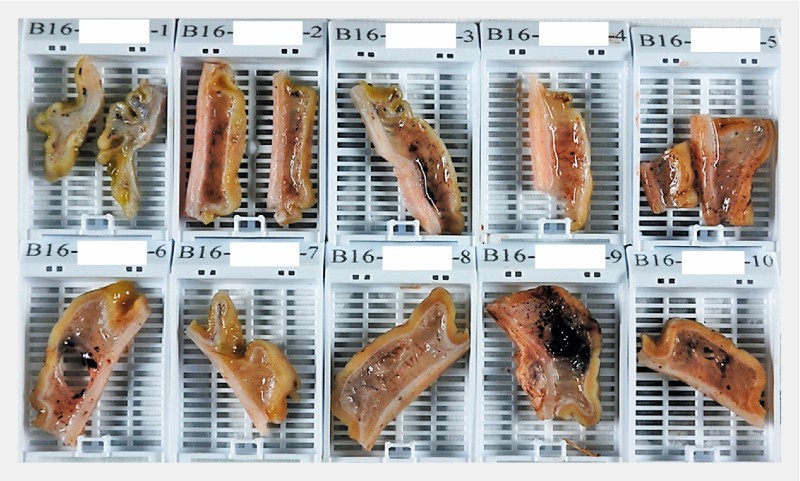
Macroscopic examination of the specimens showing a gross submucosal bleb in all specimens apart from the first one (top left; number B16-16915-1).
Fig. 4.
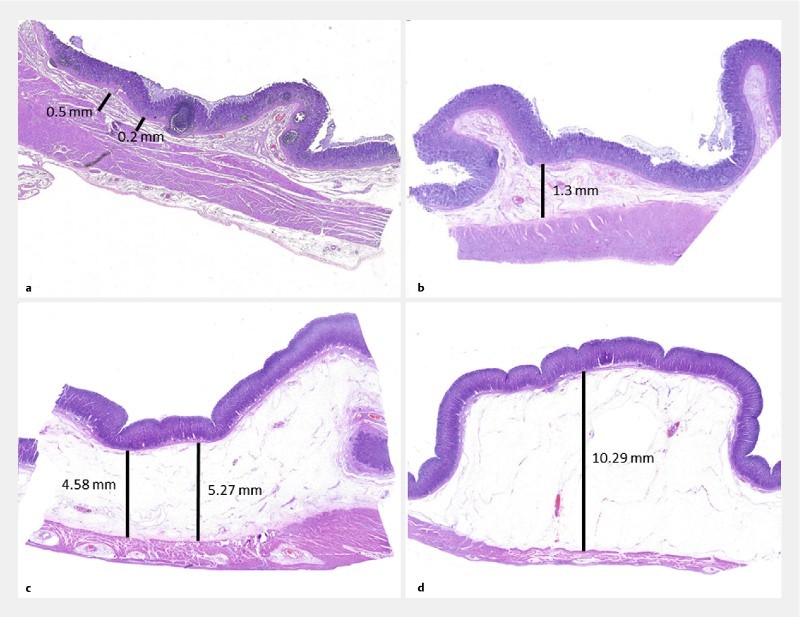
Microscopic findings at the level of the injections show that the thickness of the submucosa decreases with time after injection. a normal mucosa without injection: 0.5 mm; b 65 minutes after injection: 1.3 mm; c 50 minutes after injection: 5.27 mm. d 35 minutes after injection: 10.29 mm.
Discussion
The most effective and simplest way to prevent complications during EMR and ESD is to create a sufficiently thick submucosal layer by endoscopic injection of fluid into the submucosa. In two comparative studies with several solutions performed in porcine models, hyaluronic acid lasted longer 10 11 . In our study, the combination of hyaluronic acid with chondroitin sulfate and poloxamer 407 lasted longer than the colloid solution and the duration of elevation was similar to the results obtained in other ex vivo studies using hyaluronic acid alone 10 . Remarkably, in the in vivo stomachs, the duration of elevation was twice as long and the cushion was still visible up to 60 minutes after the injection. To our knowledge, these results demonstrate the longest durability reported so far compared with other solutions.
Gelafundin (succinylated gelatin) was used as the control injection solution because it is used to perform large EMRs in our unit due to its durability, widespread availability in our country, and low price.
Damage to the resected specimen can limit precise histological diagnosis of a targeted lesion, and hyaluronic acid has been shown to be the least harmful 12 . Furthermore, tissue damage to the muscle layer may result in delayed bleeding or perforation. The addition of poloxamer to hyaluronic acid in the present study did not lead to any damage to the mucosa, muscularis mucosa, or the muscularis propria, confirming its safety.
Ziverel has the beneficial effect of reducing the permeability of injured mucosa which is enhanced by the fact that poloxamer 407 facilitates product adhesion to the esophageal mucosa prolonging its action 13 . Based on these properties, we hypothesize that Ziverel could also facilitate the healing process in the scar left after EMR or ESD and expect an early proliferation of collagen and elastic fibers as described with other solutions 14 15 . Similar to a previous study in which Ziverel was applied over the mucosa, we do not expect any organ-specific toxicity. In addition, the cost of Ziverel is significantly lower than hyaluronic acid (0.085 and 10 euro per mL, respectively) and its use could decrease the final cost of the procedure (for instance, considering that for a gastric ESD, at least 50 mL of submucosal solution would be needed, the total cost would be 4.25 euro with Ziverel compared with 500 euro with hyaluronic acid).
The main inconvenience of injecting poloxamer is its high viscosity and this makes injection fairly difficult without a balloon dilator gun 8 . Although we were able to inject Ziverel through a 23G sclerotherapy needle at both concentrations, the injection was subjectively easier with the more dilute concentration but, despite this, the duration of the submucosal cushion was still longer than with the control solution. In the ex vivo study, we used a 21G needle in order to facilitate the injection.
In this study, we did not perform any endoscopic resection and we do not know how use of this solution could affect the outcomes and speed of EMR and ESD. We also do not know how this solution might affect the settings of the electrosurgical units although, based on initial experience with poloxamer 8 , we do not expect any differences. Moreover, we do not know the impact of Ziverel in the prevention of bleeding and perforation, which are the main clinical complications of endoscopic resection.
This study has several strengths. One is that the endoscopist who produced the submucosal cushions and timed the blebs was blinded to which solution was being tested. However, there were noticeable differences in the viscosities of the different solutions during injection and this made it easy to guess which one was being used. The second strength is that the study was performed in resected and living stomachs in order to assess the influence of blood flow and absorption from the tissue confirming that in living animals, the duration of mucosal elevation with 80 % Ziverel was even longer than in explanted stomachs.
With regard to limitations, we did not measure the change in height of cushions as reported in other studies 11 16 . This could be a more objective measure of cushion duration. On the other hand, we only analyzed the immediate potential tissue damage and this does not exclude long-term tissue damage, especially after performing an endoscopic resection. However, long-term (1 week) tissue damage has only been associated with the use of hypertonic solutions with high osmolality.
In conclusion, the present study demonstrates the potential use of a combination of hyaluronic acid, chondroitin sulfate, and poloxamer 407 as a solution for submucosal injection, not only because it lasted longer than other solutions but also because it did not induce acute tissue damage. Further studies are needed to assess its efficacy and safety when performing in vivo endoscopic resections.
Acknowledgments
The authors are grateful for funding from the CERCA Programme, Generalitat de Catalunya.
Footnotes
Competing interests None
References
- 1.ASGE TECHNOLOGY COMMITTEE . Kantsevoy S V, Adler D G, Conway J D et al. Endoscopic mucosal resection and endoscopic submucosal dissection. Gastrointest Endosc. 2008;68:11–18. doi: 10.1016/j.gie.2008.01.037. [DOI] [PubMed] [Google Scholar]
- 2.Ferreira A O, Moleiro J, Torres J et al. Solutions for submucosal injection in endoscopic resection: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E1–E16. doi: 10.1055/s-0034-1393079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamamoto H, Kawata H, Sunada K et al. Successful en-bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy. 2003;35:690–694. doi: 10.1055/s-2003-41516. [DOI] [PubMed] [Google Scholar]
- 4.Katsinelos P, Kountouras J, Paroutoglou G et al. Endoscopic mucosal resection of large sessile colorectal polyps with submucosal injection of hypertonic 50 percent dextrose-epinephrine solution. Dis Colon Rectum. 2006;49:1384–1392. doi: 10.1007/s10350-006-0611-5. [DOI] [PubMed] [Google Scholar]
- 5.Lee S-H, Park J-H, Hyun Park D et al. Clinical efficacy of EMR with submucosal injection of a fibrinogen mixture: a prospective randomized trial. Gastrointest Endosc. 2006;64:691–696. doi: 10.1016/j.gie.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 6.Varadarajulu S, Tamhane A, Slaughter R L. Evaluation of dextrose 50% as a medium for injection-assisted polypectomy. Endoscopy. 2006;38:907–912. doi: 10.1055/s-2006-944664. [DOI] [PubMed] [Google Scholar]
- 7.Uraoka T, Fujii T, Saito Y et al. Effectiveness of glycerol as a submucosal injection for EMR. Gastrointest Endosc. 2005;61:736–740. doi: 10.1016/s0016-5107(05)00321-4. [DOI] [PubMed] [Google Scholar]
- 8.Fernández-Esparrach G, Shaikh S N, Cohen A et al. Efficacy of a reverse-phase polymer as a submucosal injection solution for EMR: a comparative study (with video) Gastrointest Endosc. 2009;69:1135–1139. doi: 10.1016/j.gie.2008.07.032. [DOI] [PubMed] [Google Scholar]
- 9.Fujishiro M, Yahagi N, Kashimura K et al. Tissue damage of different submucosal injection solutions for EMR. Gastrointest Endosc. 2005;62:933–942. doi: 10.1016/j.gie.2005.07.052. [DOI] [PubMed] [Google Scholar]
- 10.Conio M, Rajan E, Sorbi D et al. Comparative performance in the porcine esophagus of different solutions used for submucosal injection. Gastrointest Endosc. 2002;56:513–516. doi: 10.1067/mge.2002.128107. [DOI] [PubMed] [Google Scholar]
- 11.Fushiro M, Yahagi N, Kashimura K et al. Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy. 2004;36:579–583. doi: 10.1055/s-2004-814517. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto H, Sekine Y, Higashizawa T et al. Successful en bloc resection of a large superficial gastric cancer by using sodium hyaluronate and electrocautery incision forceps. Gastrointest Endosc. 2011;54:629–632. doi: 10.1067/mge.2001.118643. [DOI] [PubMed] [Google Scholar]
- 13.Di Simone M P, Vasina V, Scorrano F et al. Barrier effect of Esoxx on esophageal mucosal damage: experimental study on ex-vivo swine model. Clin Exp Gastroenterol. 2012;5:103–107. doi: 10.2147/CEG.S31404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bures J, Kopácová M, Kvetina J et al. Different solutions used for submucosal injection influenced early healing of gastric endoscopic mucosal resection in a preclinical study in experimental pigs. Surg Endosc. 2009;23:2094–2101. doi: 10.1007/s00464-008-0207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uraoka T, Ochiai Y, Fujimoto A et al. A novel fully synthetic and self-assembled peptide solution for endoscopic submucosal dissection induced ulcer in the stomach. Gastrointest Endosc. 2016;83:1259–1264. doi: 10.1016/j.gie.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Kusano T, Etoh T, Akagi T et al. Evaluation of 0.6% sodium alginate as a submucosal injection material in endoscopic submucosal dissection for early gastric cancer. Dig Endosc. 2014;26:638–645. doi: 10.1111/den.12268. [DOI] [PubMed] [Google Scholar]


