Abstract
Background
Thyroidectomy and parathyroidectomy are the most commonly performed endocrine operations, and increasingly are completed on a same-day basis. Little data exists regarding the outpatient post-operative pain requirement of these patients. We aimed to describe the outpatient narcotic medication needs for patients undergoing thyroid and parathyroid surgery, and to identify predictors of higher requirement.
Method
We examined patients undergoing thyroid and parathyroid surgery at two large academic institutions from January1-May 30, 2014. Prospective data was collected on pain scores and the oral morphine equivalents (OMEQ) taken by these patients by their post-operative visit.
Results
313 adult patients underwent thyroidectomy or parathyroidectomy during the study period. 83% of patients took 10 or fewer OMEQ, and 93% took 20 or fewer OMEQ. Patients who took more than 10 OMEQ were younger (p<0.001) and reported significantly higher overall mean pain scores at their post-operative visit (p<0.001) than patients who took fewer than 10 OMEQ. A multivariate model was constructed on pre and intraoperative factors that may predict usage of greater than 10 OMEQ post-operatively. Age < 45 years (p=0.002), previous narcotic use (p=0.037) and whether parathyroid or thyroid surgery was performed (p=0.003) independently predicted the use of more than 10 OMEQ after surgery. A subgroup analysis was then performed on thyroidectomy only patients.
Conclusion
93% of patients undergoing thyroidectomy and parathyroidectomy require 20 or fewer OMEQ by their post-operative visit. We therefore recommend these patients be discharged with 20 oral morphine equivalents, both to minimize waste and increase patient safety.
Synopsis
Outpatient thyroidectomy and parathyroidectomy are increasingly performed with little information on outpatient oral narcotic requirements. We reviewed our experience with 313 consecutive patients, and recommend prescribing 20 oral morphine equivalents, which meets the post-operative needs of 93% of these patients.
Introduction
Thyroidectomy and parathyroidectomy are common endocrine operations with demonstrated safety on an outpatient basis.1–3 Our discharge criteria for ambulatory thyroidectomy include return to baseline activity, pain controlled on oral pain medications, the ability to tolerate a diet, void spontaneously with adequate social support and understanding of instructions. Specific discharge criteria include assessment of the neck wound and voice.2,4 While several studies have examined the impact of timing5 and types6–8 of local anesthesia during thyroidectomy or parathyroidectomy on post-operative pain, the primary endpoints have focused on minimizing the use of IV narcotics while the patient remains in the hospital. However, most patients undergoing thyroid or parathyroid surgery are now discharged on the day of surgery. To our knowledge, no data exist regarding the outpatient postoperative narcotic pain requirements for these patients, or on predictors of such needs. With no guidance, the prescribed medications, doses, and quantities are commonly left to the discretion of the discharging physician or provider.
Increasing trends of unintentional drug poisoning in the United States, especially from opioid analgesics is currently at the forefront of the public health agenda.9 Additionally, as care pathways are increasingly being developed and used, a standardization of outpatient prescribing practices would be helpful. This would permit more precise preoperative patient education, and limit potential risks associated with the over-prescription of opioids such as drug sharing, abuse and overdose. In addition, standardization can assist providers in detecting excessive pain medication requirements, which may be indicative of a post-operative complication.
The primary aim of this study was to examine the outpatient narcotic medication requirement after thyroid and parathyroid surgery at two large endocrine surgery centers. Our secondary aim was to identify factors that could be predictive of requiring greater than 10 oral morphine equivalents (OMEQ).
Material and Methods
A total of 313 consecutive patients over the age of 18 were identified as undergoing thyroid or parathyroid surgery between January 1 and May 31, 2014. Operations were performed at one of two large academic medical centers, the University of Rochester or the University of Wisconsin, by four endocrine surgeons. All operations were done under general anesthesia, supplemented with local anesthetic. Post-operative pain was assessed via a visual analog scale at three time points: on post-operative day (POD) 0, POD 1, and at their post-operative follow-up visit which usually occurs two weeks after surgery. Pain scores from POD1 were obtained retrospectively at the time of post-operative follow-up for those patients who were discharged the same-day, and prospectively if the patient was monitored overnight. The overall mean pain score from these three encounters were then calculated for comparison.
Patients self-reported at the post-operative visit the number of narcotic tablets they had taken since surgery. This was incorporated into routine post-operative questions to minimize recall bias. As different types of oral narcotics were prescribed, all prescriptions were converted into oral morphine equivalents (OMEQ) using an online calculator.10 (Table 1) OMEQ has been shown to better reflect clinical dosing and to provide greater insight into opioid consumption.11 As 83% of our patient cohort required 10 or fewer OMEQ, we chose greater than 10 OMEQ as the cut-off to define higher narcotic requirement. Patients were then stratified by greater or less than 10 OMEQ and univariate analysis was performed. Categorical variables were analyzed using Χ2 or Fisher’s exact-test, and independent t-tests were used to compare continuous variables. Using pre-operative and intraoperative factors, a multivariate logistic regression model was constructed to determine variables that could independently predict the use of more than 10 OMEQ. Subgroup analysis further evaluated thyroidectomy patients. All statistical calculations were performed using SPSS (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.)
Table 1.
Calculation of oral morphine equivalents (OMEQ)
| Oral Narcotic | OMEQ |
|---|---|
| 5mg Hydrocodone | 1 |
| 5mg Oxycodone | 1.5 |
| 1mg Hydromorphone | 4 |
| 5mg Codeine | 0.15 |
| 5mg Tramadol | 0.20 |
Results
Patient characteristics
313 patients underwent thyroid and parathyroid surgery at two major academic medical centers. Partial or total thyroidectomy was performed in 166 (53%) cases, of which 48 (29%) were for thyroid cancer. 253/313 (81%) of our patients were female with mean length of stay less than one day as most cases were performed on an outpatient basis. The average age of our cohort was 55 ± 0.85 years. Age was made a categorical variable using the cutoff of 45 years, the 25% quartile, and we found an association between younger age and higher OMEQ use (p<0.001). (Table 2A)
Table 2.
| A. Patient cohort stratified by greater than 10 morphine equivalents | |||||
|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | ||||
| Variable | More than 10 equivalents (n=54) |
10 equivalents or less (n=259) |
p-value | OR (95%CI) | p-value |
| Age < 45 years | 26 (48.1%) | 56 (21 6%) | <0.001 | 0.31 (0.15–0.65) | 0.002 |
| Institution A | 52 (96.3%) | 158 (610%) | <0.001 | 0.05 (0.01–0.19) | <0.001 |
| Female | 48 (88.9%) | 205 (79.2%) | 0.098 | 1.50 (0.55–4.09) | 0.428 |
| LOS (days) | 0.5 [0–1.01] | 0.5 [0–1.01] | 0.263 | - | - |
| Extent of Surgery* | |||||
| Unilateral | 21 (38.9%) | 124 (47.9%) | 0.228 | 0.63 (0.31–1.31) | 0.217 |
| Bilateral | 33 (61.1%) | 135 (52.1%) | |||
| Parathyroid Surgery | 13 (24.5%) | 134 (52.3%) | |||
| Thyroid Surgery† | 40 (75.5%) | 122 (47.7%) | <0.001 | 0.31 (0.14–0.66) | 0.003 |
| History of narcotic use‡ | n=53 6 (11.3%) |
n=221 7 (3.2%) |
0.012 | 4.15 (1.09–15.81) | 0.037 |
| Local Anesthetic | |||||
| Pre-incision | 2 (3.7%) | 101 (39.0%) | <0.001 | - | - |
| Post-incision | 52 (96.3%) | 158 (61.0%) | |||
| Number of equivalents prescribed | 30 [13–45] | 20 [10–30] | <0.001 | - | - |
| Ice used | 42 (77.8%) | 180 (69.5%) | 0.223 | - | - |
| Pain adjuncts§ used | 10 (18.5%) | 15 (5.8%) | 0.002 | - | - |
| Mean pain score | 3 [1–5] | 2 [0–4] | <0.001 | - | - |
| B. Thyroidectomy patients stratified by greater than 10 morphine equivalents | |||||
|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | ||||
| Variable | More than 10 equivalents (n=40) |
10 equivalents or less (n=122) |
p-value | OR (95%CI) | p-value |
| Age < 45 years | 23 (57.5%) | 43 (35.2%) | 0.013 | 0.28 (0.12−0.67) | 0.004 |
| Institution A | 39 (95%) | 65 (53.3%) | <0.001 | 0.04 (0.01–0.20) | <0.001 |
| Female | 36 (90%) | 102 (83.6%) | 0.323 | 1.86 (0.48–7.20) | 0.370 |
| LOS (days) | 1 [0.5–1.51 | 1 [0.5–1.51 | 0.986 | - | - |
| Extent of Surgery | |||||
| Thyroid Lobectomy | 15 (37.5%) | 36 (29.5%) | 0.345 | 0.36 (0.14–0.91) | 0.031 |
| Total Thyroidectomy | 25 (62.5%) | 86 (30.5%) | |||
| Neck dissection performed | 4 (10%) | 8 (6.6%) | 0.493 | 2.65 (0.47–15.10) | 0.272 |
| Drain used | 3 (7.5%) | 9 (7.4%) | 0.979 | 2.18 (0.34–14.22) | 0.414 |
| Local Anesthetic | |||||
| Pre-incision | 2 (5%) | 57 (46.7%) | <0.001 | - | - |
| Post-incision | 38 (95%) | 65 (53.3%) | |||
| Number of equivalents prescribed | 30 [16–44] | 20 [10–30] | 0.003 | - | - |
| Ice used | 32 (80%) | 96 (78.7%) | 0.860 | - | - |
| Pain adjunct* used | 7 (17.5%) | 7 (5.7%) | 0.022 | - | - |
| Mean pain score | 3 [1–5] | 2 [0–4] | <0.001 | - | - |
| History of narcotic use† | 2 (5%) | n=98 3 (3.1%) |
0.627 | - | - |
Univariate analysis represented as median [IQR], or n (%)
LOS = length of stay, OR = odds ratio, CI = confidence interval, IQR = interquartile range
Extent of Surgery defined as unilateral (thyroid lobectomy and unilateral parathyroidectomy) or bilateral (total thyroidectomy or bilateral parathyroidectomy or both thyroid and parathyroid surgery)
Concomitant thyroid and parathyroid surgery (n=4) excluded from this variable
n provided for each group due to missing data
Adjunct refers to any method to treat pain other than opioid analgesia
Univariate analysis represented as median [IQR], or n (%)
LOS = length of stay, OR = odds ratio, CI = confidence interval, IQR = interquartile range
Adjunct refers to any method to treat pain other than opioid analgesia
n provided due to missing data
Perioperative factors
Patients underwent thyroid lobectomy, total thyroidectomy, unilateral or bilateral parathyroidectomy, or a combined operation including both thyroidectomy and parathyroidectomy. In most cases, the strap muscles were separated in the midline. Rarely in cases of large goiters, the straps were divided to facilitate exposure at the discretion of the surgeon, but we have no means of identifying which or how many of the patients had these muscles divided.
Our two centers differed in their intraoperative management algorithms. In one center, a single surgeon routinely performed pre-incision bilateral superficial cervical nerve blocks using 30mL of 1% lidocaine and 0.25% bupivacaine. In the other center, three surgeons injected 20 or 30mL of 0.25% bupivacaine into the incision prior to skin closure. Intraoperative analgesic medications were given at the discretion of the anesthesia team. An ice pack was ordered for all patients postoperatively. On univariate analysis, whether thyroid or parathyroid surgery was performed (p<0.001) as well as the timing of injection of local anesthetic (p<0.001) were associated with increased OMEQ requirement. (Table 2A)
Oral Morphine Equivalent (OMEQ) use
Hydrocodone/acetaminophen 5/325mg (1 OMEQ) was the most commonly prescribed oral narcotic medication, given to 89.8% (281/313) of patients, followed by oxycodone/acetaminophen 5/325 mg in 4.2% (13/313). Patients were prescribed a median of 30 OMEQ at discharge with a range of 0–120. The median OMEQ taken was 3 (range 0–60), and the mode was zero (99/313, 31.6%). Only 7% of patients took more than 20 OMEQ. (Figure 1)
Figure 1.

Distribution of outpatient narcotic pain medication utilization at post-operative visit for thyroid and parathyroid surgery patients, reference lines drawn at 20 oral morphine equivalents
During the post-operative visit, patients were also asked to give a reason for taking prescription pain medication. 214 (68.4%) patients took at least 1 OMEQ after surgery, most commonly for incisional pain (60%). Interestingly, 3 patients (1%) reported taking narcotics because they were instructed to despite having no pain. (Figure 2A) Of the patients who took more than 10 OMEQ, 46 (85%) reported doing so for incisional pain. (Figure 2B)
Figure 2.
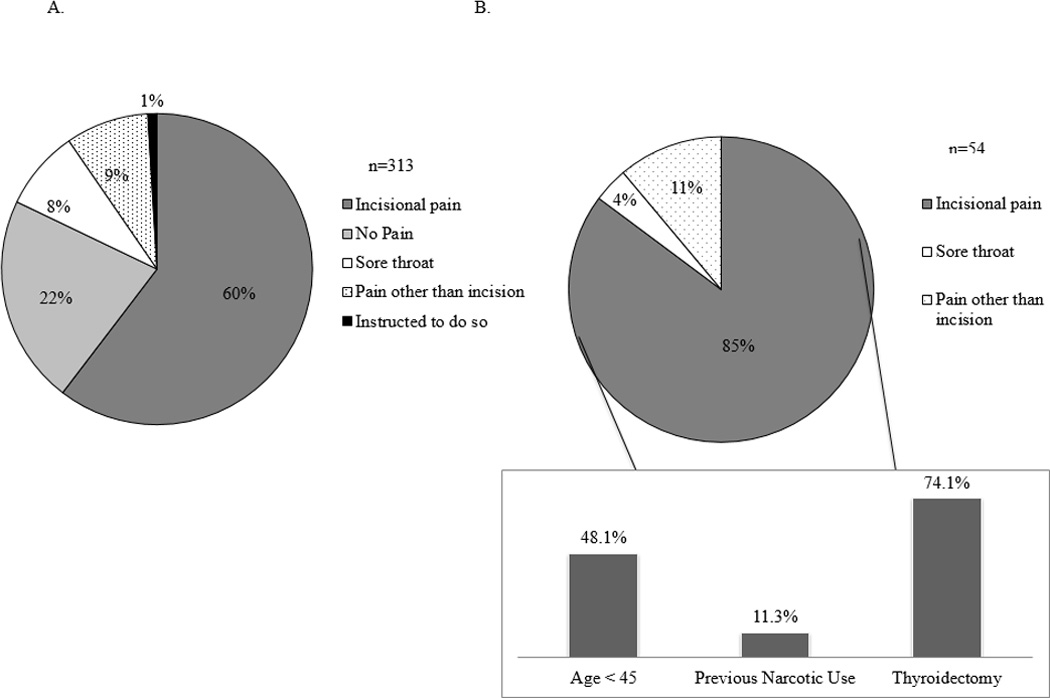
Patient reasons for taking narcotic pain medication after thyroid and parathyroid surgery A. all patients B. Patients who took ≥ 10 morphine equivalents, insert shows percentage distributions by select variable of the patients who required ≥ 10 MEQ
Factors Predictive of Higher Narcotic Requirement
On univariate analysis, age less than 45 years (p<0.001), whether parathyroid or thyroid surgery was performed (p<0.001), timing of local anesthetic (p<0.001), the use of pain adjuncts (p=0.002) and prior history of narcotic use (p=0.012) were associated with greater than 10 OMEQ use. (Table 2A) The median age and interquartile range (IQR) of patients who required more than 10 tablets was 46.5 [25.5–67.5], whereas the median age for patients who required 10 or fewer OMEQ was 57 [40–74] (p<0.001). (Figure 3A) Not surprisingly, patients who required more than 10 OMEQ also reported higher mean pain scores (p<0.001). (Figure 3B)
Figure 3.
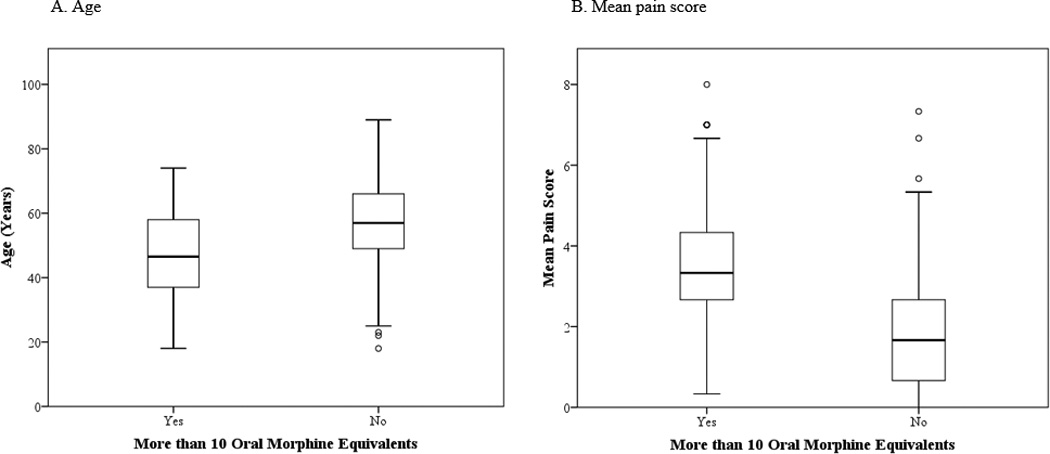
Distribution of select variables with respect to morphine equivalents
We also found a center effect on outpatient OMEQ needs (p<0.001). As we could not determine whether this difference was due to nursing care or instructions, the timing or amount of local anesthetic administration, or from the overall random effects of two different centers, we adjusted for institution in our model. Our multivariate logistic regression model found that age less than 45 years (p=0.002, OR 0.31 95% CI 0.15–0.65), whether parathyroid or thyroid surgery was performed (p=0.003, OR 0.31 95% CI 0.14–0.66), and history of previous narcotic use (p=0.037, CI 4.15 95% CI 1.09–15.81) were independently predictive of taking more than 10 OMEQ. (Table 2A)
Subgroup Analysis of Thyroidectomy Patients
Thyroidectomy was associated with greater than 10 OMEQ therefore a subgroup analysis looking at these patients was performed. Limited sample size precluded a similar examination of parathyroidectomy patients, and 4 patients who underwent both parathyroidectomy and thyroidectomy were also excluded. 162 patients underwent thyroid surgery, with 40 patients reporting more than 10 OMEQ. (Table 2B) Looking exclusively at thyroidectomy patients also allowed inclusion of additional perioperative variables such as a cancer diagnosis, neck dissection, and drain use. Our multivariate model on thyroidectomy patients revealed that age less than 45 (p=0.004, OR 0.28 95% CI 0.12–0.67) and total thyroidectomy (p=0.031, OR 0.36 CI 0.14–0.91) were predictive of higher OMEQ use. (Table 2B)
Discussion
The vast majority of patients undergoing thyroidectomy and parathyroidectomy demonstrated a minimal requirement for outpatient narcotics with 93% of patients requiring 20 or fewer OMEQ. The overall mean pain score after surgery was 2 [IQR 0–4] indicating mild pain, if any, by the first post-operative visit. We also discovered that even between our two institutions, there was no standard prescribing pattern with a wide range of prescriptions, and number of equivalents dispensed. Based upon our results, we have changed our practices to discharge all patients undergoing parathyroid or thyroid surgery and request an oral narcotic prescription with no more than 20 equivalents. This translates to 20 tablets of 5/325 hydrocodone/acetaminophen.
Standardizing prescribing practices for these commonly performed endocrine operations will not only reduce waste, but also promote patient safety. The abuse and misuse of prescription narcotics is of continued public health concern, with opioids as the leading reason behind deaths from overdose in the United States.12 The rise in unintentional deaths from prescription drugs have paralleled the increase in opioid sales across the United States.9 This not only harms the narcotic user, but also results in inadvertent exposure of small children from having such medications in the home.13 Additionally, by prescribing a median of 30 OMEQ to our patients, we may be influencing expectations of the amount of post-operative pain.
Previous studies evaluating pain after thyroidectomy have focused on reducing postoperative pain with different adjuncts, most commonly with the use of local anesthetic. Several double-blind randomized studies have evaluated the role of bilateral superficial cervical plexus blocks in thyroidectomy with conflicting results.6, 14 Despite differing study designs, these studies highlight the lack of consensus in terms of ideal volumes, and types of local anesthetic used in thyroid surgery. The literature has also examined different concentrations of local anesthetic, as well as the timing of injection. Herbland et al conducted a randomized trial evaluating the timing of bilateral superficial cervical plexus blocks using 0.75% ropivacaine with epinephrine injected either prior to incision or after thyroidectomy completion.8 That study concluded that the addition of local anesthetic did not improve post-operative pain control in either the proportion of patients requiring post-operative analgesia or in the total amount of narcotics required. All of the aforementioned studies, however, used inpatient IV morphine as the primary endpoint to assess analgesic effect, but failed to examine the amount of oral narcotics required once the patient was discharged. A formal evaluation on the timing of local anesthetic during thyroid and parathyroid surgery in effecting post-operative outpatient pain requirements has yet to be performed.
As pain is subjective, it remains challenging to evaluate and treat. Several clinical trials have examined the role of varying adjuncts to narcotics in providing acceptable analgesia. Preemptive anesthesia remains controversial regarding its effectiveness with respect to post-procedural pain.15A randomized trial demonstrated decreases in post-operative pain scores and IV morphine use in patients who received gabapentin 2 hours prior to thyroidectomy or parathyroidectomy.16 Another trial explored the effect of music therapy on same-day inguinal herniorrhaphy patients and found a significant decrease in plasma cortisol levels in those who received music postoperatively compared to the control group .17 A recent randomized study demonstrated the effectiveness of ice packs in reducing postoperative pain and morphine use in patients undergoing laparotomy.18 Other non-opioid analgesics include over the counter medications such as ibuprofen, and actupuncture.19 In our study, patients who required more than 10 OMEQ were significantly more likely to use adjunctive measures; however, the impetus to do so is unclear.
Our study has several limitations. First, we included the breadth of endocrine neck operations from minimally invasive parathyroidectomy to total thyroidectomy with neck dissection. Parathyroidectomy patients likely require even fewer OMEQ than thyroidectomy patients. However, the number of parathyroidectomy patients reporting more than 10 OMEQ did not allow further analysis. Second, the use of non-opioid analgesics is certainly a potential confounder to not only the reported pain scores, but also the number of OMEQ taken and this was not specifically examined in this study. Though our study is unable to draw any specific conclusions on the role of adjunctive measures in treating post-operative pain, this is an important subject for future work. Our analysis also revealed institutional differences, for which the exact cause cannot be discerned, but was adjusted for in our predictive modeling. Performance of a cervical plexus block as related to pain is a clear confounder, however as the two institutions were complete opposites in practice, this variable could not specifically be examined. Additionally, we had missing data on previous narcotic use and limited availability of past psychiatric history, both of which have been associated with higher narcotic requirements and higher reported pain scores.20 Lastly, although our data on pain scores and OMEQ taken was prospectively collected, the information was based upon patient recollection and was analyzed in a retrospective manner. Notwithstanding these limitations, our study is the first to examine outpatient narcotic pain medication use after thyroid and parathyroid surgery. A standardized practice of prescribing stands to increase patient safety and minimize risks of dependence and overdose. We found that 97% of patients used 20 OMEQ or less, and that this number was inclusive of the most patients. Reduced waste is also one of the ways prescribing providers can help control health care costs. In addition, our adjusted data from two large academic centers of varying geographic location make these recommendations more generalizable. Our findings in OMEQ are also translatable to whichever oral narcotic individual providers are most comfortable with prescribing.
In conclusion, 93% of patients across two large academic institutions required 20 or fewer OMEQ after thyroid or parathyroid surgery, and nearly 1/3 of patients required none. Age less than 45 years, thyroid surgery, and a previous history of narcotic use were independent predictors on multivariate analysis for more than 10 OMEQ. Therefore, patients undergoing thyroid and parathyroid surgery should be prescribed 20 OMEQ to minimize waste, and to increase patient safety.
Acknowledgments
Source of Funding:
Irene Lou is currently receiving grant support from 5T32CA090217-15
David F. Schneider is currently receiving grant support from NIH UL1TR000427 and NIH KL2TR000428
Footnotes
Conflicts of Interest
For the remaining authors, none are declared.
References
- 1.Mowschenson PM, Hodin RA. Outpatient thyroid and parathyroid surgery: a prospective study of feasibility, safety, and costs. Surgery. 1995;118(6):1051–1053. doi: 10.1016/s0039-6060(05)80113-8. discussion 1053-4. [DOI] [PubMed] [Google Scholar]
- 2.Terris DJ, Snyder S, Carneiro-Pla D, et al. American Thyroid Association statement on outpatient thyroidectomy. Thyroid. 2013;23(10):1193–1202. doi: 10.1089/thy.2013.0049. [DOI] [PubMed] [Google Scholar]
- 3.Irvin GL, Sfakianakis G, Yeung L, et al. Ambulatory parathyroidectomy for primary hyperparathyroidism. Arch Surg. 1996;131(10):1074–1078. doi: 10.1001/archsurg.1996.01430220068015. [DOI] [PubMed] [Google Scholar]
- 4.Flynn MB, Quayyum M, Goldstein RE, et al. Outpatient parathyroid surgery: ten-year experience: is it safe? Am Surg. 2015;81(5):472–477. [PubMed] [Google Scholar]
- 5.Egan RJ, Hopkins JC, Beamish AJ, et al. Randomized clinical trial of intraoperative superficial cervical plexus block versus incisional local anaesthesia in thyroid and parathyroid surgery. Br J Surg. 2013;100(13):1732–1738. doi: 10.1002/bjs.9292. [DOI] [PubMed] [Google Scholar]
- 6.Dieudonne N, Gomola A, Bonnichon P, et al. Prevention of postoperative pain after thyroid surgery: a double-blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg. 2001;92(6):1538–1542. doi: 10.1097/00000539-200106000-00038. [DOI] [PubMed] [Google Scholar]
- 7.Gozal Y, Shapira SC, Gozal D, et al. Bupivacaine wound infiltration in thyroid surgery reduces postoperative pain and opioid demand. Acta Anaesthesiol Scand. 1994;38(8):813–815. doi: 10.1111/j.1399-6576.1994.tb04010.x. [DOI] [PubMed] [Google Scholar]
- 8.Herbland A, Cantini O, Reynier P, et al. The bilateral superficial cervical plexus block with 0.75% ropivacaine administered before or after surgery does not prevent postoperative pain after total thyroidectomy. Reg Anesth Pain Med. 2006;31(1):34–39. doi: 10.1016/j.rapm.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 10.Group WSAMD. Opiod Dose Calculator 2007–2014. Available at: http://agencymeddirectors.wa.gov/mobile.html.
- 11.Svendsen K, Borchgrevink P, Fredheim O, et al. Choosing the unit of measurement counts: the use of oral morphine equivalents in studies of opioid consumption is a useful addition to defined daily doses. Palliat Med. 2011;25(7):725–732. doi: 10.1177/0269216311398300. [DOI] [PubMed] [Google Scholar]
- 12.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 13.Woodcock J. A difficult balance--pain management, drug safety, and the FDA. N Engl J Med. 2009;361(22):2105–2107. doi: 10.1056/NEJMp0908913. [DOI] [PubMed] [Google Scholar]
- 14.Eti Z, Irmak P, Gulluoglu BM, et al. Does bilateral superficial cervical plexus block decrease analgesic requirement after thyroid surgery? Anesth Analg. 2006;102(4):1174–1176. doi: 10.1213/01.ane.0000202383.51830.c4. [DOI] [PubMed] [Google Scholar]
- 15.Kissin I. Preemptive analgesia. Anesthesiology. 2000;93(4):1138–1143. doi: 10.1097/00000542-200010000-00040. [DOI] [PubMed] [Google Scholar]
- 16.Al-Mujadi H, A-Refai AR, Katzarov MG, et al. Preemptive gabapentin reduces postoperative pain and opioid demand following thyroid surgery. Can J Anaesth. 2006;53(3):268–273. doi: 10.1007/BF03022214. [DOI] [PubMed] [Google Scholar]
- 17.Nilsson U, Unosson M, Rawal N. Stress reduction and analgesia in patients exposed to calming music postoperatively: a randomized controlled trial. Eur J Anaesthesiol. 2005;22(2):96–102. doi: 10.1017/s0265021505000189. [DOI] [PubMed] [Google Scholar]
- 18.Watkins AA, Johnson TV, Shrewsberry AB, et al. Ice Packs Reduce Postoperative Midline Incision Pain and Narcotic Use: A Randomized Controlled Trial. J Am Coll Surg. 2014;219(3):511–517. doi: 10.1016/j.jamcollsurg.2014.03.057. [DOI] [PubMed] [Google Scholar]
- 19.White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101(5 Suppl):S5–S22. doi: 10.1213/01.ANE.0000177099.28914.A7. [DOI] [PubMed] [Google Scholar]
- 20.Rapp SE, Ready LB, Nessly ML. Acute pain management in patients with prior opioid consumption: a case-controlled retrospective review. Pain. 1995;61(2):195–201. doi: 10.1016/0304-3959(94)00168-E. [DOI] [PubMed] [Google Scholar]


