Summary
We present a middle aged pregnant woman who developed signs and symptoms of acute liver failure and was found to have herpes simplex virus hepatitis. Patient had an emergent delivery and was started on antiviral therapy, but unfortunately due to the severity of her liver failure, she passed away. The importance of reporting this case is to emphasize on the importance of considering herpes simplex infection in pregnant women who present with acute liver failure, and the importance of early administration of antiviral therapy.
Keywords: Herpes simplex hepatitis, acute liver failure, hepatitis in pregnancy
1. Introduction
Pregnant women are at increased risk for herpes simplex virus (HSV) hepatitis, particularly in the third trimester of pregnancy (1). Hepatitis can result from acute or latent infection with either HSV serotype 1 or serotype 2. Approximately half of cases lack typical HSV mucocutaneous lesions and the disease can arise in patients with no known history of genital or oral HSV infections. The differential diagnosis for HSV hepatitis is quite broad and includes acute fatty liver of pregnancy, severe preeclampsia/Hemolysis Elevated Liver enzymes and Low Platelets (HELLP) syndrome, other viral infections, and exogenous exposures, including drug reactions (2). Possible distinguishing clinical characteristics include markedly elevated liver enzymes with normal bilirubin and coagulopathy (2–4). The first adult case of hepatic dysfunction due to herpes virus was reported in 1969 by Flewett et al. (5). Although considered rare, herpes hepatitis is a fatal condition if not considered early with a mortality rate of 74.4% in the general population (6). To the best of our knowledge, 36 cases of HSV hepatitis during pregnancy have been reported, although those with autopsy examination remains outstanding (2,3,5–14). We present a case with autopsy examination findings of fatal herpes simplex hepatitis.
2. Case Report
A 41-year old woman with no significant past medical history was 30-weeks pregnant when she presented to an outside hospital with a two-day history of cough, nausea and vomiting. She sought medical attention (day 1) and her urinalysis showed trace leukocyte esterase so she was treated initially for possible urinary tract infection versus upper respiratory infection with amoxicillin. Laboratory testing also revealed mildly elevated aspartate aminotransaminase (AST) and alanine aminotransaminas (ALT) (90 and 61 U/L, respectively). By day 5 the patient's AST and ALT increased to 5,652 and 1,559 U/L, respectively. Additionally, her serum creatinine increased to 3.2 mg/dL, hemoglobin decreased to 8.9 gm/dL, platelets decreased to 129,000/mm3, and International Normalized Ratio (INR) increased to 2.3, all from normal baseline.
On day 6, she became acutely encephalopathic (grade 3) with tachycardia (120 beats per minute) and tachypnea (30 breaths per minute). Plasma ammonia was elevated at 102 µmol/L. Workup for acute liver failure included laboratory testing for hepatitis A (IgM and RNA), B (surface antigen, core antibody IgM and IgG and DNA), and C (surface antibody and RNA), Epstein-Barr virus (EBV), cytomegalovirus (CMV), and parvovirus serologies, all of which were negative. Therefore, she was transferred to a tertiary center for further management on that day. She was taken on arrival for emergent Cesarean section with no intraoperative complications noted and she delivered a male infant. She remained intubated postoperatively; continuous renal replacement (CRRT) was initiated for acidosis, hyperkalemia, and other electrolyte abnormalities.
Laboratory testing were repeated and revealed markedly elevated AST and ALT (7,161 U/L and 2,176 U/L, respectively), as well as elevated bilirubin (1.8 mg/dL total bilirubin, 1.7 mg/dL direct bilirubin), alkaline phosphatase (ALP, 370 U/L) and gamma-glutamyltransferase (GGT, 46 U/L). Serum creatinine was elevated at 3.4 mg/dL. Differential diagnosis of acute liver failure were reconsidered and included: Acute fatty liver of pregnancy, acute viral hepatitis, autoimmune hepatitis, Wilson's disease and Hemolysis Elevated Liver Enzymes and Low platelets (HELLP) syndrome. Serologies for infectious etiologies were again obtained, this time including HEV and HSV. Patient was started on empiric acyclovir (450 mg q12hours, intravenously).
On Day 7, HSV RNA was detected in blood obtained on day 6. Her postoperative course was complicated by significant vaginal bleeding with hemodynamic instability requiring pressor support. Bleeding could not be controlled by tamponade of the cervix and massive blood transfusion protocol was started. She underwent bilateral uterine artery embolization by interventional radiology but bleeding continued. Liver transplantation (LT) and hysterectomy were considered but unfortunately due to rapidly progressive clinical deterioration with a clear evidence of disseminated intravascular coagulopathy (DIC) from liver failure, she had cardiac arrest. Cardiopulmonary resuscitation was started but despite maximal resuscitative efforts, restoration of spontaneous circulation was never achieved. After discussion with family, resuscitation was stopped and patient was declared dead. The clinical course of the case is summeraized in Figure 1.
Figure 1.
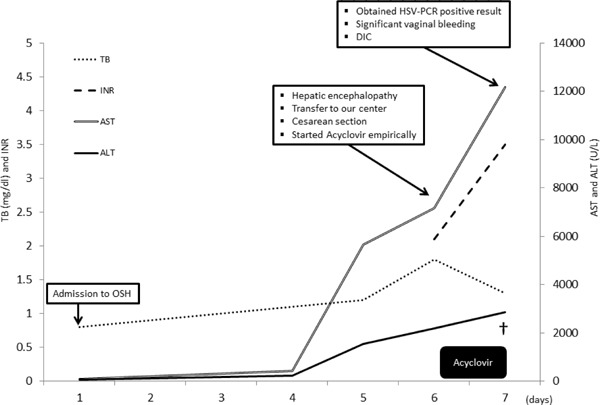
The clinical course of the case. The case with acute liver failure due to HSV developed rapidly progressive clinical deterioration despite empiric administration of acyclovir and passed away (†: time of death).
Autopsy examination of the liver revealed pale, punctate lesions diffusely scattered throughout the parenchyma. Microscopically, these lesions corresponded to non-zonal foci of hepatocyte necrosis with minimal associated inflammation. Ringing the necrotic areas were hepatocytes showing distinct HSV viral cytopathic effect. Immunohistochemistry performed on liver sections for HSV-1 was positive. The adrenal glands also showed scattered foci of punctate necrosis and HSV-1 positivity by immunohistochemistry. No mucocutaneous lesions were identified, and there was no other evidence of visceral organ involvement (Figures 2A, B and C).
Figure 2.
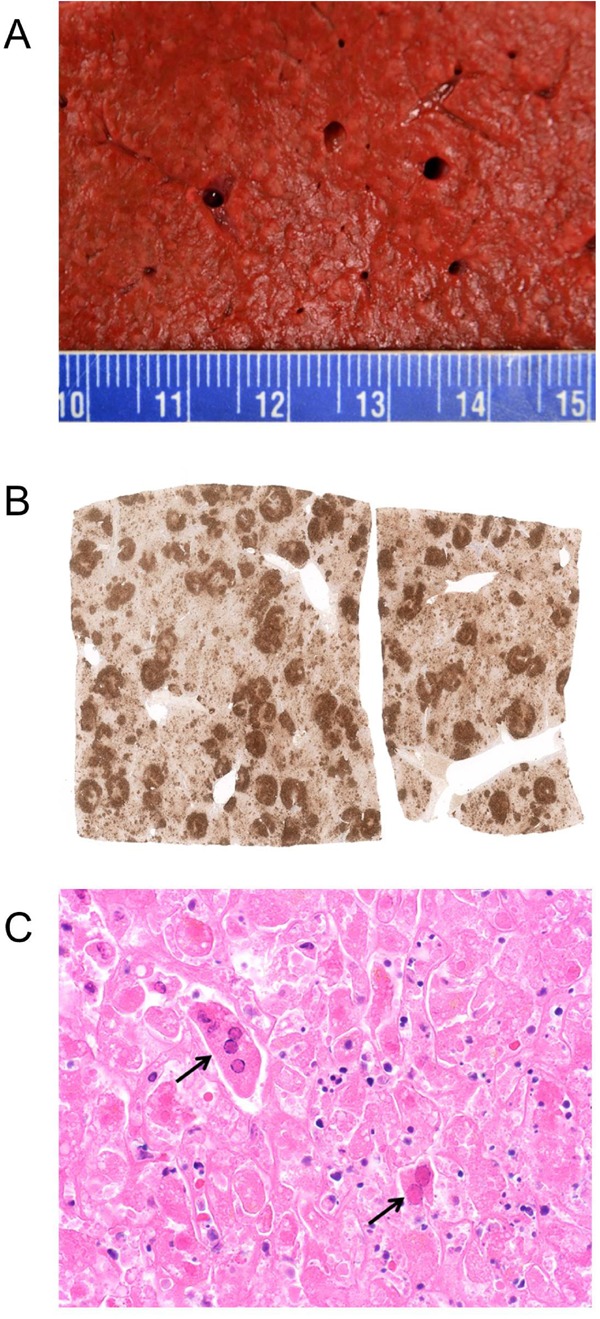
The autopsy findings. (A) The cut surface of the liver demonstrated innumerable 2–4 mm cream colored, soft nodules; (B) On histopathology, these proved to represent foci of geographic necrosis, highlighted here with an HSV immunostain; (C) High power photomicrograph demonstrates two hepatocytes with typical HSV cytopathic effect (arrows) characterized by multinucleation, margination (i.e., peripheral displacement) of chromatin, and ground-glass nuclei.
3. Discussion
HSV hepatitis is a rare, frequently fulminant disease that typically affects immunocompromised patients including pregnant women (15). Clinical presentation of fever with abdominal pain and hepatic dysfunction in a pregnant woman should prompt immediate consideration of herpes hepatitis and work up should be initiated to exclude other common causes like HELLP and acute fatty liver of pregnancy (3). Unfortunately signs and symptoms are non-specific and can be vague, and the gold standard for diagnosis is liver biopsy with histopathology, electron microscopy, and viral culture. Pathognomic findings include: hemorrhagic necrosis and enlarged ground glass nuclei with marginalized chromatin (15). However, liver biopsy in this setting (especially due to maternal coagulopathy) is a significant risk of adverse events related to bleeding. Thus the histopathological findings obtained from autopsy examinations still remain outstanding. Development of alternative diagnostic modalities are desired (3).
Although the efficacy of antiviral therapy has not been proven in randomized controlled trial, intravenous acyclovir — a synthetic guanosine analogue- has been used for treating herpesviruses. Those have different degrees of susceptibility to acyclovir, with HSV type 1 (HSV-1) being most susceptible, followed by HSV type 2 (HSV-2) and VZV, and to a lesser extent Epstein-Barr virus (EBV). In cases of resistance, the use of foscarnet had been advised (16).
Despite supportive care and administration of antiviral therapy to the most susceptible genotype (HSV-1), our patient's condition continued to deteriorate with multi-organ failure that led to her death. The immunosuppressive effects of pregnancy make pregnant women infected by HSV at risk of disseminated disease (4). The prognosis was initially reported to be poor (39% mortality rate) in 1999, but the more recently, from 2000, it seemed to be improving (9% mortality rate amoung 11 cases) (3). Treatment of acute liver failure due to HSV infection include antiviral therapy and LT, and in one report therapeutic plasma exchange (17). Norvell et al. (6) conducted a retrospective analysis on 134 patients with HSV hepatitis including 32 (23%) pregnant women. The following variables were statistically associated with need for LT or death compared to spontaneous recovery: age > 40 year old, male gender, coagulopathy, any immunocompromised state, encephalopathy, ALT > 5,000 U/L, platelet count < 75,000 U and lack of acyclovir treatment. A total of 7 patients underwent LT and 3 of them survived at one year. In our case, despite the effort of a multidisciplinary team, the fast progression of events and rapid worsening of clinical status in the presence of dissiminated intravascular coagulopathy made transplant a difficult option to pursue. Acyclovir was given in our case, but only after her presentation to our center, which was 6 days after the onset of symptoms.
In conclusion, herpes hepatitis is a fatal condition, and should be considered in all pregnant patients with concern for evolving hepatic failure and early administration of antiviral therapy should be considered.
References
- 1. Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014; 370:2211-2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allen RH, Tuomala RE. Herpes simplex virus hepatitis causing acute liver dysfunction and thrombocytopenia in pregnancy. Obstet Gynecol. 2005; 106:1187-1189. [DOI] [PubMed] [Google Scholar]
- 3. Herrera CA, Eichelberger KY, Chescheir NC. Antiviral-resistant fulminant herpes hepatitis in pregnancy. AJP Rep. 2013; 3:87-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kang AH, Graves CR. Herpes simplex hepatitis in pregnancy: A case report and review of the literature. Obstet Gynecol Surv. 1999; 54:463-468. [DOI] [PubMed] [Google Scholar]
- 5. Flewett TH, Parker RG, Philip WM. Acute hepatitis due to Herpes simplex virus in an adult. J Clin Pathol. 1969; 22:60-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Norvell JP, Blei AT, Jovanovic BD, Levitsky J. Herpes simplex virus hepatitis: An analysis of the published literature and institutional cases. Liver Transpl. 2007; 13:1428-1434. [DOI] [PubMed] [Google Scholar]
- 7. Mortelé KJ, Barish MA, Yucel KE. Fulminant herpes hepatitis in an immunocompetent pregnant woman: CT imaging features. Abdom Imaging. 2004; 29:682-684. [DOI] [PubMed] [Google Scholar]
- 8. Nagappan R, Parkin G, Simpson I, Sievert W. Fulminant hepatic failure from herpes simplex in pregnancy. Med J Aust. 2002; 176:595-596. [DOI] [PubMed] [Google Scholar]
- 9. Lazar P. An interesting herpes simplex infection. Arch Dermatol. 1977; 113:145-149. [DOI] [PubMed] [Google Scholar]
- 10. Frederick DM, Bland D, Gollin Y. Fatal disseminated herpes simplex virus infection in a previously healthy pregnant woman. A case report. J Reprod Med. 2002; 47:591-596. [PubMed] [Google Scholar]
- 11. Halliday J, Lokan J, Angus PW, Gow P. A case of fulminant hepatic failure in pregnancy. Hepatology. 2010; 51:341-342. [DOI] [PubMed] [Google Scholar]
- 12. Thurman RH, König K, Watkins A, Weerasiri T, Permezel M. Fulminant herpes simplex virus hepatic failure in pregnancy requiring liver transplantation. Aust N Z J Obstet Gynaecol. 2010; 50:492-494. [DOI] [PubMed] [Google Scholar]
- 13. Navaneethan U, Lancaster E, Venkatesh PG, Wang J, Neff GW. Herpes simplex virus hepatitis - it's high time we consider empiric treatment. J Gastrointestin Liver Dis. 2011; 20:93-96. [PubMed] [Google Scholar]
- 14. Nienaber JH, McNamara DR, Banerjee R, Pritt BS, Karre T, Sohail MR. Fulminant gestational hepatitis due to primary herpes simplex type 2 infection: Use of serum HSV polymerase chain reaction for noninvasive diagnosis. Diagn Microbiol Infect Dis. 2012; 72:181-184. [DOI] [PubMed] [Google Scholar]
- 15. Kaufman B, Gandhi SA, Louie E, Rizzi R, Illei P. Herpes simplex virus hepatitis: Case report and review. Clin Infect Dis. 1997; 24:334-338. [DOI] [PubMed] [Google Scholar]
- 16. Razonable RR. Antiviral drugs for viruses other than human immunodeficiency virus. Mayo Clin Proc. 2011; 86:1009-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Holt EW, Guy J, Gordon SM, Hofmann JC, Garcia-Kennedy R, Steady SL, Bzowej NH, Frederick RT. Acute liver failure caused by herpes simplex virus in a pregnant patient: Is there a potential role for therapeutic plasma exchange? J Clin Apher. 2013; 28:426-429. [DOI] [PubMed] [Google Scholar]


