Abstract
Solid tumors are complex organ-like structures. The potential of normal neighboring cells to contribute to the initiation, progression and metastasis of epithelial-derived carcinomas has long been appreciated. However, the role of host cells has proven complex. Through multiple local and systemic mechanisms, nontransformed host cells can promote transition from a tumor-resistant to tumor-permissive environment, drive neoplastic transformation of epithelial cells, promote tumor growth, progression, and metastasis, but also constrain tumorigenesis. This complexity reflects the spatially and temporally dynamic involvement of multiple cell types and processes, including the development and recruitment of inflammatory, immune, endothelial, and mesenchymal stromal cells, and the remodeling of extracellular matrix. Our mechanistic understanding, as well as our ability to translate advances in our understanding of these mechanisms for therapeutic benefit, is rapidly advancing. Further insights will depend on delineating pathways that mediate the communication networks between inflammatory and immune cells with tumor and mesenchymal stromal cells and extracellular matrix. Herein we discuss the diversity of mesenchymal stromal cell populations and how context can dictate either their promotion or constraint of tumorigenesis. We review evidence for plasticity that allows for reprograming of stromal cells and how tumor immunogenicity and desmoplasia influence the balance of immune-independent and immune-dependent regulation of tumor growth. The pivotal roles of matrix and mesenchymal stromal cells in modulating inflammation, anti-tumor immunity, and the efficacy of immune-based therapies are discussed. These concepts have emerged from data obtained from tumors of multiple organs, but we focus most on studies of pancreatic ductal adenocarcinomas (PDA).
Background and Rationale
The initiation and evolution of epithelial-derived solid tumors (i.e., carcinomas) involves extensive communication between epithelial cells and various non-transformed host cells such as mesenchymal stromal cells (MSCs), fibroblasts, endothelial cells, and inflammatory and immune infiltrates (1–5). As reviewed in a prior Masters in Immunology article that also focused on carcinoma-associated fibroblasts (CAFs) (6), tumor-associated stromagenesis shares many aspects of wound-healing, in which fibroblasts play critical roles in orchestrating inflammation, angiogenesis and extracellular matrix (ECM) remodeling required for tissue repair. Many human carcinomas are characterized by CAFs that deposit and organize a matrix rich in collagens, hyaluronic acid (HA), and fibronectin, much like that found in wounds. Unlike in wounds, however, this pathophysiologic response fails to resolve, resulting in the desmoplastic microenvironment common to many carcinomas (7,8). However the degree of desmoplasia in tumors can vary dramatically.
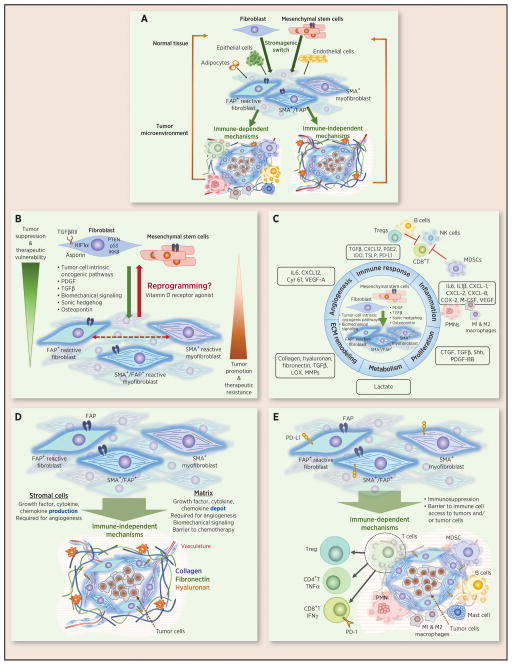
The conventional paradigm regarding the role of cancer-associated stromal cells (CASCs) is that, regardless of invoking individual molecular mechanisms that can have opposing effects that either promote or constrain tumor growth and metastasis, their net effect is protumorigenic. But in fact, their net effect reflects the balance between protumorigenic and antitumorigenic activities that can vary depending on tumor type, regionally within tumors and depends on the ecology of the host milieu. Another important factor is the stage in evolution of a particular tumor. Stroma is an important factor in the tumor nonpermissive state of normal tissue that transitions to a tumor permissive state with perturbation and tumor progression (Figure 1A and B). Thus, like the immune and vascular systems, tumor progression is associated with a stromagenic switch. Transition of all three compartments are integrally related with progression from immune editing to a state of immune equilibrium, to immune escape (9) and angiogenesis occurring in concert with the reprogramming of stromal cells and matrix remodeling in an interdependent manner. Indeed, stromal cells have emerged as important drivers of immune modulation through their release of cytokines, chemokines, and other soluble factors such as prostaglandin E2, and their expression of ligands for inhibitory receptors such as CTLA-4 and PD-1 (Figure 1B). In addition, stromal cells deposit the extracellular matrix that can present a physical barrier to immune cell infiltration but also provides the substratum essential to the interstitial migration of immune cells (10).
FIGURE 1. Evolution of tumor stroma and its immune-dependent and immune-independent control of tumor growth.
(A) Overview. (B) Multiple stromal cell types found in normal tissues, including fibroblasts, mesenchymal stem cells, adipocytes, endothelial cells, and epithelial cells can (trans)differentiate into cancer-associated fibroblasts (CAFs)/stromal cells. This stromagenic switch that transitions a tumor suppressive environment to a tumor promoting environment is driven by multiple factors, including those indicated, and may be reversible based on recent evidence of reprogramming following treatment with the vitamin D receptor agonist calcitriol. Two prominent subclasses are myofibroblasts, characterized by the expression of proteins of the contractile apparatus such as α-SMA, and FAP+ reactive fibroblasts. These two subpopulations are distinct but overlap to varying degrees in different tumor types and can have opposing effects on tumorigenesis, at least in pancreatic cancer. (C) The products regulated in CAFs relative to normal fibroblasts that promote cell proliferation: a shift from oxidative phosphorylation to glycolysis, matrix remodeling, angiogenesis, inflammation, and immune suppression in the tumor microenvironment are shown. The indicated pathways regulate tumor growth through immune-independent (D) and immune-dependent (E) mechanisms.
CASCs are phenotypically and functionally heterogeneous, raising the possibility that some of the opposing effects on tumor and immune cell behavior might be propagated by distinct subpopulations, or by cells at different stages as they co-evolve with their neighbors. Evidence indeed has emerged to support this latter concept in models of pancreatic cancer, as discussed below. CASCs can impact tumorigenesis via mechanisms defined broadly as immune-independent and immune-dependent (Figure 1A, D and E). In both cases myriad mechanisms, some with potentially opposing effects on tumor cell behavior, appear to be involved. In addition, the stroma can play major roles in resistance to therapy. Thus, a systematic understanding of the role of the distinct subpopulations involved and the complex networks of stromal cell–dependent intracellular, cell-matrix, and soluble factor–mediated biochemical signaling pathways and biomechanical forces underlying tumorigenesis and the immune response to cancer has important implications for the advancement of cancer prevention, diagnostics, prognostics, and development of novel targeted therapies. In particular, understanding the stromagenic response in cancer has important implications for the development of immune-based cancer therapies that rather than being effective in relatively small subpopulations of patients, might be effective in the vast majority of patients afflicted with a broad array of solid tumor types.
Heterogeneity of cancer-associated fibroblasts (CAFs)
CAFs are found in virtually all human carcinomas but their prevalence varies dramatically. They are typically prevalent in pancreatic, non-small-cell lung, colorectal, breast and prostate cancers but relatively sparse in ovarian, thyroid, renal, brain, and head and neck cancers (11,12). CAFs are often identified morphologically by their elongated spindle-like fibroblastic appearance. There is as of yet no consensus on the molecular definition of CAFs but several markers have been used to identify them, including fibroblast-specific protein 1 (FSP-1), vimentin, desmin, neuron-glial antigen-2 (NG2), platelet-derived growth factor receptor-β (PDGFRβ), podoplanin, fibroblast-associated antigen, prolyl 4-hydroxylase (4,13–16) and the two that we focus on herein, alpha-smooth muscle actin (α-SMA) and the plasma membrane serine protease fibroblast activation protein (FAP). Alpha-SMA is a well-established marker for myofibroblasts (MFs) and MF-like cells in the tumor microenvironment (17) but is also expressed in visceral smooth muscle cells, perivascular smooth muscle cells, and pericytes (18). FAP is a robust CAF marker originally found highly expressed in various solid tumors but not most quiescent stromal cells (12,19). However, as discussed in detail in Dr. Fearon’s Masters of Immunology article (6) it is also expressed in mesodermal cells in multiple tissue types under homeostatic conditions and in tissues that undergo active remodeling (20–24).
FAP+ and α-SMA+ cells represent overlapping but distinct populations of cancer-associated stromal cells with the degree of overlap ranging from several percent (e.g., in breast or pancreatic cancer) to virtually a hundred percent (e.g., lung squamous cell carcinoma) depending on the tumor type (25–28). FAP is also expressed on a subset of M2-like (CD11b+F4/80highCD206+ “M2-like” tumor-associated macrophages (25,26,29) which must be taken into account when interpreting studies aimed at defining the role of FAP+ cells that include CAFs and this subset of macrophages versus other populations such as αSMA+ cells. Gastric tumors from reporter mice expressing red fluorescent protein driven by the SMA promoter contain multiple phenotypically distinct subsets of tumor stromal cells, including SMA− MSCs, (30), whereas others showed that MSCs express FAP (24). Therefore, MSCs likely account for at least a portion of the FAP+SMA− cells observed in the microenvironment of many human and murine carcinomas. Interestingly, these cells were shown to have the capacity to both self-renew, as well as differentiate into SMA+ myofibroblasts, both in wound healing and the tumor microenvironment (30,31), suggesting a lineage relationship exists between some terminally differentiated SMA+ myofibroblasts and mesenchymal progenitor cells that at some stage may express both SMA and FAP, but at least some of which may later down regulate or lose FAP expression, but retain SMA. Similar analyses of other markers provide further evidence for the heterogeneity of CAFs.
One source of heterogeneity of CAFs is the multiple cells from which they can be generated (5) including resident fibroblasts, stellate cells and bone marrow–derived and local mesenchymal stem cells (MSCs) or by trans-differentiation of epithelial or endothelial cells (Figure 1) (30,32–38). CAFs can also originate from adipocytes or adipose tissue-associated stromal cells (39–41). Additionally, bone marrow–derived fibrocytes or MSCs can be recruited into tumors and differentiate into CAFs (30,39,42,43).
Regardless of the source, the phenotypic heterogeneity of CAFs raises the interesting question as to their potential to exert distinct effects on tumorigenesis which has important implications for developing stromal cell targeted therapies. Indeed, taken together, the results of three recent independent studies discussed in detail below, indicate that although FAP+ cancer-associated stromal cells promote tumorigenesis, αSMA expressing MFs may constrain the aggressiveness of tumors in related models of pancreatic cancer (27,28,44).
The stromagenic switch
Normal fibroblasts and MSCs, analogous to the immune system, have the capacity to protect against the emergence of neoplastic epithelial cells (Figure 1B) (45,46). The conditional inactivation of the TGFβ type II receptor gene in mouse fibroblasts allowed epithelial tumors to develop, which indicated that normal fibroblasts can constrain epithelial tumorigenesis and that genetically modified fibroblasts can be sufficient to drive tumorigenesis (47). This concept is reinforced by the demonstration that PTEN, p53, and IKKβ signaling pathways in fibroblasts also play critical roles in restraining the tumorigenic potential of multiple solid tumors (48–50). In addition, fibroblast-derived HIF-1α and asporin inhibit breast cancer tumorigenesis and progression, respectively (51,52). Taken together, in addition to the immune-mediated tumor-suppressive mechanisms, stromal surveillance programs may also prevent tumorigenesis or impose a dormant state (53). Whether any such stromal-dependent pathways impact tumorigenesis at least in part through immune-dependent mechanisms has yet to be fully explored.
Both preneoplastic cells and established tumors evolve in part by overcoming stroma-mediated barriers and by driving transition of tumor-suppressive fibroblasts into tumor-promoting CAFs. Indeed, many studies have demonstrated that normal fibroblasts are functionally distinct from CAFs (Figure 1C). Prostatic CAFs are more proliferative and less prone to contact inhibition than normal prostate fibroblasts (54). Moreover, prostatic CAFs are more dependent on anaerobic glycolysis and produce more lactate relative to normal prostatic fibroblasts (55). Colonic CAFs enhance the proliferation and migration of tumor cells to a greater extent than do normal colonic fibroblasts (56). Metabolic competition can contribute to immune-suppression in the tumor microenvironment and thus may be another mechanism by which the stroma impacts antitumor immunity (57–59). Normal fibroblasts can be reprogrammed into CAFs that drive tumor progression, invasion, and metastasis by modulating various aspects of the tumor microenvironment, including ECM remodeling, angiogenesis, and inflammatory and immune responses (60–67). For example, CAFs have a greater capacity to drive inflammation and angiogenesis relative to their normal counterparts (30,68). These functional differences between CAFs and their normal counterparts reflect transcriptional regulation, genetic, and epigenetic programs that drive evolution of the gene expression profiles in fibroblasts (67,69–73). It should be noted that CAFs may retain some tumor inhibitory mechanisms as well. For instance, some primary CAF lines derived from breast cancer secrete Slit ligands that bind Robo1 expressed by breast cancer cells. Robo1 signaling inhibits PI3K/Akt signaling and thereby restrains tumor growth (74).
An important question is whether the transition of fibroblasts to an activated and protumorigenic state is preventable or reversible which might present an opportunity to reprogram stromal cells as a therapeutic approach. In wound repair, resolution is associated with apoptosis of activated fibroblasts. In contrast, in pathologic fibrosis and tumors, activated fibroblasts persist. However, the differentiation of fibroblasts to the fibrotic and protumorigenic state may indeed be reversible. Specifically, the vitamin D receptor agonist calcipotriol reversed the stellate cell response in hepatic fibrosis (75) and pancreatitis (76). Calcipotriol also reduced markers of inflammation and fibrosis and when given in combination with gemcitabine, reduced tumor volume and increased survival in a model of pancreatic cancer (Figure 1B) (76).
Modulation of inflammation and immunity
Inflammation is increasingly appreciated as an important contributing factor in promoting the development of a wide range of malignancies, including colon, gastric, liver, lung, and pancreatic cancers (77–81). Studies indicate that crosstalk between inflammatory cells and tumor stroma regulates the desmoplastic response in tumors and the desmoplastic response may limit infiltration and regulate the function of infiltrating leukocytes. CAFs orchestrate the inflammatory response by secreting cytokines such as IL6 and IL1-β (Figure 1). Secreted chemokines such as CXCL1 and CXCL2 recruit tumor-associated neutrophils and macrophages (68,82). Carcinomas, including breast, lung, and pancreatic cancers, exhibit CAF-mediated NF-κB–dependent pro-inflammatory gene signatures (68,83,84). CAFs promote survival and polarization of tumor-associated myeloid cells to a M2 macrophage phenotype (85). This alternative activation of macrophages is likely due to the overexpression of IL6, TGFβ. and CCL2 by CAFs (86–88).
Activated pancreatic stellate cells (PSCs) can secrete SDF-1α/CXCL12 to promote CD8+ T cell chemotaxis towards the juxtatumoral stroma, thereby preventing CD8+ T cells from accessing tumor nests. Knock-down of SDF-1α/CXCL12, or treatment of activated PSCs with all-trans retinoic acid, rendered PSCs quiescent, abrogated CD8+ T cell chemotaxis towards PSCs, while enhancing CD8+ T cell proximity to neoplastic cells in pancreatic cancer (89). In contrast, SDF-1α/CXCL12 derived from FAP+ CAFs bound to pancreatic cancer cells and inhibited T cell access to tumor cells. Inhibition of CXCR4 (a receptor for SDF-1α/CXCL12) by AMD3100 reversed immune-suppression and potentiated the efficacy of checkpoint-blockade with anti–PD-L1 to restrain the growth of pancreatic tumors (44). Additionally, cancer-associated PSCs can promote the differentiation of peripheral blood mononuclear cells into myeloid-derived suppressor cells (MDSCs) by secreting pro-inflammatory cytokines including IL6, M-CSF, VEGF, and SDF-1α/CXCL12. IL6 and STAT3 signaling were required for PSC-induced MDSC differention that in turn inhibited T-cell activation, thereby contributing to tumoral immune-suppression (90). Depleting granulocytic MDSCs with anti-Ly-6G antibody treatment increased intratumoral accumulation of activated CD8+ T cells, enhanced tumor cell apoptosis, and remodeled the tumor stroma in pancreatic tumors (91). Cancer-associated fibroblasts can also impair activation, cytokine production and cytotoxicity of NK and T cells through secretion of prostaglandin E2 and indoleamine 2,3-dioxygenase (92,93).
Conversely, inflammatory myeloid cells can promote CAF activation and desmoplasia. The IL6 or SDF-1α/CXCL12 secreted by M2 macrophages can promote human prostatic fibroblast activation, as measured by α-SMA expression (88). Treatment with the anti-inflammatory drug dexamethasone reduces the recruitment of Gr-1+CD11b+ cells, decreases CAF accumulation, and decreases collagen deposition, thereby attenuating squamous carcinoma progression (85). CAFs and M2 macrophages also act in concert to activate endothelial cells to enhance angiogenesis (88).
Finally, desmoplastic stroma can represent a physical barrier for naturally occurring antitumor immunity and T-cell based cancer immunotherapy. Tumor stroma precludes T cell infiltration and migration into tumor cell nests in human lung cancers ex vivo. Collagenase treatment augments T cell mobilization and increases the accessibility of T cells to tumor cell nests (94). Expression of heparanase, which degrades heparan sulfate proteoglycans in the ECM, can potentiate tumor infiltration of CAR-redirected T cells and augments the anti-tumor activity(95).
Immune-dependent and -independent mechanisms
The role of stromal cell populations in tumorigenesis has primarily been determined by depleting them in established tumors. Early studies used FAP vaccines and antibody-based targeting. A dendritic cell-based FAP vaccine inhibited the growth of multiple tumor types (96). Depletion of CD8+ T cells partially abrogated the antitumor effects of this vaccine. However, it was not determined whether this was due to the elimination of the subpopulation of CD8+ T cells specific for FAP+ stromal cells (induced by the vaccine) or the loss of antitumor CD8+ T cells that had been unleashed by reducing the number of FAP+ stromal cells. An oral FAP vaccine suppressed primary tumor growth and metastasis in mouse models of colon and breast carcinoma (97). FAP+ stromal cells played an important role in matrix remodeling as evidenced by a significant reduction in collagen in tumor tissues of FAP-vaccinated mice. Although the mechanisms involved were not determined, this study also provided early evidence that targeting tumor stroma could enhance uptake of chemotherapeutic drugs. Tumor growth could also be inhibited by other approaches, such as immunoconjugates based on antibodies to FAP (98), and using a FAP-activated pro-drug to target carcinoma-associated stromal cells (99). No overt toxicity was observed in any of these studies other than a modest delay in wound healing in the first vaccine study.
Two other direct approaches can delete stromal cell subpopulations. Genetic approaches have been used to conditionally ablate either SMA+ cells in mouse models of pancreatic cancer (27) or FAP+ stromal cells in related models of pancreatic cancer as well as a syngeneic transplant model of lung cancer (100). The former employed transgenic mice expressing a thymidine kinase gene under the control of the α-SMA promoter. Upon administration of gangcyclovir, a subset of α-SMA+ CASC were depleted. These investigators posited that proliferating myofibroblasts were preferentially deleted, whereas α-SMA+ vascular smooth muscle cells, pericytes and myoepithelial cells were spared. This approach led to negligible loss of FAP+ stromal cells, consistent with evidence for minimal overlap between FAP+ and α-SMA+ stromal cell subsets in PDA. Contrary to expectations based on evidence that stromal cells in established tumors are on balance protumorigenic, conditional ablation of this subset of α-SMA+ CASC was associated with a more aggressive tumor phenotype and reduced animal survival. Tumors were invasive and undifferentiated, with enhanced hypoxia, epithelial-to-mesenchymal transition, and had more cancer stem cells. In retrospect this result is perhaps not surprising, given that fewer myofibroblasts in tumors correlates with reduced survival in PDA patients. The impact on tumorigenesis was associated with suppressed immune surveillance and increased CD4+Foxp3+ Tregs and a reduction in collagen, but not HA. Although tumors in α-SMA+ cell depleted mice did not respond to gemcitabine, which may require loss of HA (101,102), anti-CTLA-4 immunotherapy reversed the disease progression and prolonged survival.
In marked contrast, conditional ablation of FAP+ stromal cells inhibited tumor growth in both a lung and a pancreatic tumor model. BAC transgenic mice were constructed that express the human diphtheria toxin receptor (DTR) under control of a FAP promoter (FAP.DTR mice). Upon administration of diphtheria toxin to tumor bearing FAP.DTR mice, FAP+ stromal cells were ablated. Depletion of FAP+ cells inhibited tumor growth of established tumors derived from Lewis lung cancer cells expressing ovalbumin (OVA) as a nominal antigen. Inhibition of tumor growth was achieved in spite of FAP+ stromal cells representing a very small minority of total tumor cells in this model. Depletion of FAP+ cells using this approach also inhibited the growth of established tumors in a transplant model of PDA (100). Although the role of immune-independent mechanisms was not investigated in this study, immune-mediated mechanisms were implicated. Specifically, although intratumoral T cell populations did not change, the effect of FAP+ stromal cell depletion in the lung tumor model was negated by neutralizing antibodies to TNFα and IFNγ. FAP+ stromal cell depletion had no effect on PDA tumors transplanted into immune incompetent RAG-deficient mice, in apparent contradiction to results from other studies in which immune-based FAP+ stromal cell depletion inhibited the growth of transplanted PDA tumors to a similar extent in immune competent and immune incompetent NSG mice (28). Subsequent studies from the same group implicated FAP+ hemoxygenase expressing macrophages in both the lung and PDA transplant models (29). Furthermore, SDF-1α/CXCL12 derived from FAP+ fibroblasts was implicated as a mediator of immune suppression in the KPC autochthonous model of PDA. Consistent with a role of stromal cell derived SDF-1α/CXCL12, blockade of SDF-1α/CXCL12 synergized with immune checkpoint inhibitors (anti-PD-L1) in controlling tumor growth following conditional ablation of FAP+ cells (44).
Finally, several groups have used adoptive transfer of FAP-specific redirected T cells to deplete FAP+ stromal cells in a variety of tumor models (25,28,103–106). The majority of these studies utilized adoptive transfer of FAP-specific chimeric antigen receptor expressing (FAP-CAR) T cells. FAP-CAR have been generated using single chain Fv regions based on the sequence of three different monoclonal antibodies (mAbs) to FAP, two of which, 73.3 (25) and MO36 (105), inhibited tumor growth in multiple tumor models and exhibited little if any toxicity unless administered repeatedly or expressed in hyperfunctional T cells (25,28,104). The loss of antitumor activity of 73.3 FAP-CAR T cells in FAP-deficient mice established the specificity of these CAR–T cells and demonstrated that the antitumor activity was dependent on expression of FAP by host stromal cells. The third, based on FAP5, showed no significant antitumor activity and at the same time caused significant toxicity (107). The toxicity of this particular CAR appears to be attributable to recognition of a distinct epitope on FAP that resulted in depletion of any cell expressing FAP, regardless of amount, whereas 73.3FAP-CAR selectively depletes FAPhigh cells (25,28). Consistent with this possibility, toxicity was also noted after extended periods of time in naïve or tumor bearing FAP.DTR mice that had been treated with diphtheria toxin and therefore lacked all FAP+ cells (108). Depletion mediated by 73.3FAP-CAR was not just partial, but transient, which again may limit toxicity. Collectively, with the one exception, these studies of FAP-CAR T cell–mediated depletion implicate FAP+ stromal cells as potential targets across a broad spectrum of solid tumors.
The studies described above show that inhibition of tumor growth after depleting FAP+ cells can occur through both immune-dependent and immune-independent mechanisms (Figure 1A, D and E). Deletion of FAP+ cells enhanced both spontaneous and vaccine-induced endogenous immunity (25,100) and enhanced the antitumor effect of checkpoint inhibitors (44). The degree to which immune-dependent versus immune-independent mechanisms contributed relates to the immunogenicity and degree of desmoplasia, with the latter directly related to the prevalence of FAP+ stromal cells (28). Thus, the elimination of stromal cell–mediated immune suppression resulted in enhanced endogenous and vaccine-induced antitumor immunity that contributed to inhibition of tumor growth in immunogenic tumors. On the other hand, the inhibition of growth of highly desmoplastic nonimmunogenic tumors in immune-competent mice and moderately and highly desmoplastic human xenografts in immune-incompetent mice, was attributed to immune-independent mechanisms. The immune-independent mechanisms involved stromal cell depletion and the disruption of matrix that led to reduced angiogenesis, stromagenesis and tumor cell proliferation, and increased tumor cell apoptosis.
In the one study where it was analyzed, depletion of FAP+ also led to depletion of α-SMA+ cells, even in models of PDA where only a small proportion of the stromal cells co-express α-SMA and FAP(28). This indicates that either α-SMA+ CASCs are derived from FAP+ progenitors and/or that FAP+ cell are required for the generation or recruitment of α-SMA+ cells to the tumor microenvironment. In either case, loss of FAP+ cells overcame the protumorigenic effect of depleting α-SMA+ stromal cells. Tumor growth was inhibited with no evidence of more aggressive tumor phenotypes. It will of course be of interest to define the relationship between various stromal subsets in future studies.
Potential risks and benefits
Tumor cells exhibit intratumoral heterogeneity and genomic instability, in many cases rendering tumors resistant to therapeutic intervention and ultimately causing treatment failure. In contrast, nontransformed cancer-associated stromal cells are genetically stable, making them appealing targets for developing therapeutic strategies. Stromal cells in many solid tumor types share properties, and therapies targeting them can potentially synergize with other tumor cell and immune-targeted therapies.
In addition to revealing the role of specific subpopulations and the mechanisms by which they modulate tumorigenesis, preclinical models of stromal cell depletion can guide the development of selective depletion therapies in patients. However, preclinical studies have provided reason to proceed with caution, given two associated risks. First, some subpopulations of stromal cells are protective. It will be necessary to identify them, keeping in mind that these may differ in the context of various tumor types or in different stages of disease. This concern is highlighted by the evidence that whereas targeting FAP+ stromal cells in PDA may prove therapeutic, targeting SMA+ cells in this tumor type might in fact be detrimental (27,28,44). In any case, because α-SMA is localized to the cytoplasm, it is not readily apparent how current technologies could be used to efficiently target SMA+ cells. This practical concern however, does not apply in the case of FAP that localizes to the surface of stromal cells. Deletion of FAP+ cells has now been analyzed in preclinical models of multiple tumor types and resulted in inhibition of tumor growth in every case save one, with no evidence that this approach enhances tumor aggressiveness. In the one exception, deletion had neither a beneficial nor a detrimental impact on tumor progression. Longer term studies however, will be required to evaluate the impact on metastatic disease.
The second major potential concern is of on-target/off-tumor effects. In the case of α-SMA this may be a moot point in the face of the evidence that targeting α-SMA+ CASCs may be contraindicated, at least in the one tumor type studied thus far. However, this concern does apply to targeting FAP+ cells. FAP+ stromal cells reside in many tissues of the adult mouse, including skin, bone marrow, skeletal muscle, pancreas, adipose, and lymph node. They can serve homeostatic functions as well as important positive roles in reparative responses, such as tissue remodeling in wound healing. Indeed, genetic ablation (108), or immune-targeting studies using mAb FAP5–based FAP-CAR T cells (107), have shown that depletion of FAP+ stromal cells induces bone marrow hypoplasia, cachexia, and anemia. FAP+ stromal cells from skeletal muscle are also a major source of follistatin, a protein that can promote muscle growth. FAP+ stromal cells in the bone marrow produce SDF-1α and KitL, which are essential in regulating B-lymphopoiesis and erythropoiesis(108). Fibroblastic reticular cells in lymph nodes also express FAP, and experimental ablation of these cells in mice disrupts lymph node homeostasis and can impair the launch of an effective immune response to clear influenza virus infection(109).
Thus, FAP+ stromal cells are important in the maintenance of normal muscle mass, lymph node homeostasis, and hematopoiesis. Nonetheless, although caution is warranted, the data suggest that partial and/or transient depletion of FAP+ stromal cells may provide a therapeutic window in which tumor growth can be inhibited with little to no toxicity. Although this approach may be limited in efficacy when used as a monotherapy, intriguing early evidence indicates that this approach can synergize in combination with chemotherapies or other immune-based therapies such as tumor vaccines and immune checkpoint inhibitors. Multiple approaches are also under development to spatially and temporally control CAR T cell activity as a means to circumvent off-tumor activity(110–114).
Defining molecular pathways
Although a detailed analysis is beyond the scope of this article, it is important to address an alternative approach to targeting stromal cells for depletion. An intense focus is underway to define stroma-dependent molecular pathways amenable to targeting, which would inhibit protumorigenic mechanisms and to overcome therapeutic resistance. In this regard, FAP itself, which functions as a cell surface protease involved in matrix remodeling, has been explored as a potential therapeutic target. Genetic deletion of FAP and pharmacologic inhibition of its protease activity inhibits primary growth in syngeneic transplant models of lung, and colon cancer, and a KRAS-driven autochthonous model of lung cancer (115). Its role in metastasis is actively being investigated. FAP is a type II transmembrane cell surface proteinase belonging to the prolyl dipeptidyl aminopeptidase (DPP) family, which cleaves amino-terminal dipeptides from polypeptides with proline or alanine in the penultimate position (P1Pro or P1Ala) (116). FAP also exhibits endopeptidase activity that preferentially cleaves after the Gly-Pro sequence motif (P2GlyP1Pro) (117). Although FAP was initially discovered in membrane-bound form, low concentrations of circulating soluble FAP, also known as α2-antiplasmin-cleaving enzyme (APCE), have been reported in human and mouse serum (118–120). FAP protease activity in vitro has been studied extensively, but its substrate repertoire in vivo is not fully defined. In vitro screening identified neuropeptide Y, B-type natriuretic peptide, substance P, and peptide YY as potential substrates. Moreover, CCL22/MDC, CXCL2/Groβ and CXCL12/SDF-1α can be cleaved by FAP, albeit less efficiently (121). FAP’s endopeptidase activity is capable of modifying gelatin, type I and type III collagens, FGF21 and α2-antiplasmin (118–120,122–124). Many of these substrates have been implicated in tumor progression; for instance, CXCL12/SDF-1α is crucial for promoting tumor cell invasion, angiogenesis, and T-cell exclusion (44,89,125,126); collagen is important in enhancing tumor cell proliferation, invasion, and metastasis (127–129). Nonetheless, the functional consequences of FAP-dependent proteolytic processing in the context of the tumor microenvironment, other than its direct role in matrix remodeling, remain to be explored.
Another pathway that has drawn attention is Sonic hedgehog (Shh), a soluble ligand critical for driving the formation of desmoplastic stroma that is overexpressed by pancreatic tumor cells. Deletion and pharmacologic inhibition of Shh reduces stromal contents in autochthonous pancreatic tumors. However, Shh-deficient tumors developed earlier and were more aggressive, exhibiting undifferentiated histology and heightened levels of angiogenesis and proliferation. Administration of VEGFR blocking antibody improved survival of Shh-deficient tumor-bearing mice, indicating that Hedgehog-driven stromagenesis suppresses tumor growth in part by restraining tumor angiogenesis (130). Together, these studies raise substantial concerns as to whether targeting Shh is in fact a promising direction for pancreatic cancer.
The SDF1α/CXCL12-CXCR axis is yet another pathway of interest as discussed previously in this venue (6). Finally, promising data have been obtained using a pegylated hyaluronidase (PEGPH20) to disrupt the HA-rich matrix in pancreatic cancer. All told, although explorations of targeting stromal-dependent molecular pathways are in their infancy, they hold great potential. Studies suggest that the evolution of stromal cells to a protumorigenic state may be reversible (Figure 1B). Future efforts will therefore undoubtedly include attempts to reprogram CASCs to shut down their protumorigenic functions and activate or reactivate antitumorigenic functions at primary tumor sites and maintain or restore a tumor nonpermissive environment in target organs of metastases.
All of these are promising avenues to pursue in the quest to enhance the antitumor activity of conventional tumor-targeted therapies, whether they are dependent on antitumor immunity or act through immune-independent mechanisms, or both, and to improve the response rate to, and efficacy of, rapidly emerging immunotherapies for cancer.
Future Directions
Over the past several decades the identification of malignant cell intrinsic oncogenic and tumor suppressive pathways has been extremely successful. This has led to the birth of targeted therapies for cancer. Here we have tried to convey a sense of our burgeoning understanding of the significance of extrinsic factors in tumorigenesis and the potential wealth of new therapeutic targets they present. Future studies will be required to test the assumption that targeting stromal pathways will synergize with malignant cell targeted chemotherapies, radiation therapy and immunotherapies in solid tumors. In addition, the concept that stromal targets may be shared between tumor types and between primary and metastatic disease will need to be tested. The appreciation of the role of stroma-dependent pathways also begs the question as to how they interface with risk factors such as ageing, obesity and smoking. Elucidating the molecular pathways that mediate the impact of stroma on tumorigenesis will lay the ground work required to understand and manage cancer risk (Box 1).
Box 1. Future directions.
Do changes in stroma contribute to the increase in cancer risk associated with ageing?
Do stromal-dependent mechanisms play a role in obesity-associated increased cancer risk?
Does stroma provide common therapeutic targets across tumor types?
Does stroma provide therapeutic targets common to primary tumors and metastatic disease?
Can targeting stroma overcome resistance to chemotherapy and immunotherapy for cancer?
Learning Objectives.
Cross-talk between multiple types of nontransformed host cells and tumor cells determines, in a spatially and temporally dynamic fashion, the relative resistance versus permissiveness of tissues to tumor initiation. It also determines the propensity toward tumor latency and dormancy versus progression and the emergence of metastatic disease. Through completion of this activity, the participant will gain a fundamental understanding of the communication networks between heterogeneous cancer-associated stromal cells and immune cells in the context of solid tumors. The potential for extracellular matrix remodeling and stromal cell targeting to modulate antitumor immunity and the efficacy of immune-based therapies will also become evident.
Acknowledgments
Financial or Other support
This work was supported by NIH R01 CA141144 (Ellen Puré) and a Cancer Research Institute Fellowship (Albert Lo).
The authors thank Ms. Sarah E. Rauers for generating graphics and preparing the manuscript.
Footnotes
Disclosures of Potential Conflicts of Interest
The laboratory of E. Puré received research support from Novartis and shares inventor status on a pending patent.
References
- 1.Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332–7. doi: 10.1038/nature03096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Egeblad M, Nakasone ES, Werb Z. Tumors as organs: complex tissues that interface with the entire organism. Dev Cell. 2010;18:884–901. doi: 10.1016/j.devcel.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–22. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Kalluri R, Zeisberg M. Fibroblasts in cancer. Nat Rev Cancer. 2006;6:392–401. doi: 10.1038/nrc1877. [DOI] [PubMed] [Google Scholar]
- 5.Jacob M, Chang L, Pure E. Fibroblast activation protein in remodeling tissues. Curr Mol Med. 2012;12:1220–43. doi: 10.2174/156652412803833607. [DOI] [PubMed] [Google Scholar]
- 6.Fearon DT. The carcinoma-associated fibroblast expressing fibroblast activation protein and escape from immune surveillance. Cancer Immunol Res. 2014;2:187–93. doi: 10.1158/2326-6066.CIR-14-0002. [DOI] [PubMed] [Google Scholar]
- 7.Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. New Engl J Med. 1986;315:1650–9. doi: 10.1056/NEJM198612253152606. [DOI] [PubMed] [Google Scholar]
- 8.Dvorak HF. Tumors: wounds that do not heal-redux. Cancer Immunol Res. 2015;3:1–11. doi: 10.1158/2326-6066.CIR-14-0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3:991–98. doi: 10.1038/ni1102-991. [DOI] [PubMed] [Google Scholar]
- 10.Mrass P, Kinjyo I, Ng LG, Reiner SL, Pure E, Weninger W. CD44 mediates successful interstitial navigation by killer T cells and enables efficient antitumor immunity. Immunity. 2008;29:971–85. doi: 10.1016/j.immuni.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith NR, Baker D, Farren M, Pommier A, Swann R, Wang X, et al. Tumor stromal architecture can define the intrinsic tumor response to VEGF-targeted therapy. Clin Cancer Res. 2013;19:6943–56. doi: 10.1158/1078-0432.CCR-13-1637. [DOI] [PubMed] [Google Scholar]
- 12.Garin-Chesa P, Old LJ, Rettig WJ. Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc Natl Acad Sci USA. 1990;87:7235–9. doi: 10.1073/pnas.87.18.7235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orimo A, Weinberg RA. Heterogeneity of stromal fibroblasts in tumors. Cancer Biol Ther. 2007;6:618–9. doi: 10.4161/cbt.6.4.4255. [DOI] [PubMed] [Google Scholar]
- 14.Pietras K, Ostman A. Hallmarks of cancer: interactions with the tumor stroma. Exp Cell Res. 2010;316:1324–31. doi: 10.1016/j.yexcr.2010.02.045. [DOI] [PubMed] [Google Scholar]
- 15.Ohlund D, Elyada E, Tuveson D. Fibroblast heterogeneity in the cancer wound. J Exp Med. 2014;211:1503–23. doi: 10.1084/jem.20140692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoshino A, Ishii G, Ito T, Aoyagi K, Ohtaki Y, Nagai K, et al. Podoplanin-positive fibroblasts enhance lung adenocarcinoma tumor formation: podoplanin in fibroblast functions for tumor progression. Cancer Res. 2011;71:4769–79. doi: 10.1158/0008-5472.CAN-10-3228. [DOI] [PubMed] [Google Scholar]
- 17.Desmouliere A, Guyot C, Gabbiani G. The stroma reaction myofibroblast: a key player in the control of tumor cell behavior. Int J Dev Biol. 2004;48:509–17. doi: 10.1387/ijdb.041802ad. [DOI] [PubMed] [Google Scholar]
- 18.Wendling O, Bornert JM, Chambon P, Metzger D. Efficient temporally-controlled targeted mutagenesis in smooth muscle cells of the adult mouse. Genesis. 2009;47:14–8. doi: 10.1002/dvg.20448. [DOI] [PubMed] [Google Scholar]
- 19.Scanlan MJ, Raj BK, Calvo B, Garin-Chesa P, Sanz-Moncasi MP, Healey JH, et al. Molecular cloning of fibroblast activation protein alpha, a member of the serine protease family selectively expressed in stromal fibroblasts of epithelial cancers. Proc Natl Acad Sci USA. 1994;91:5657–61. doi: 10.1073/pnas.91.12.5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niedermeyer J, Garin-Chesa P, Kriz M, Hilberg F, Mueller E, Bamberger U, et al. Expression of the fibroblast activation protein during mouse embryo development. Int J Dev Biol. 2001;45:445–7. [PubMed] [Google Scholar]
- 21.Mathew S, Scanlan MJ, Mohan Raj BK, Murty VV, Garin-Chesa P, Old LJ, et al. The gene for fibroblast activation protein alpha (FAP), a putative cell surface-bound serine protease expressed in cancer stroma and wound healing, maps to chromosome band 2q23. Genomics. 1995;25:335–7. doi: 10.1016/0888-7543(95)80157-h. [DOI] [PubMed] [Google Scholar]
- 22.Wang XM, Yao TW, Nadvi NA, Osborne B, McCaughan GW, Gorrell MD. Fibroblast activation protein and chronic liver disease. Front Biosci. 2008;13:3168–80. doi: 10.2741/2918. [DOI] [PubMed] [Google Scholar]
- 23.Acharya PS, Zukas A, Chandan V, Katzenstein AL, Pure E. Fibroblast activation protein: a serine protease expressed at the remodeling interface in idiopathic pulmonary fibrosis. Hum Path. 2006;37:352–60. doi: 10.1016/j.humpath.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 24.Bae S, Park CW, Son HK, Ju HK, Paik D, Jeon CJ, et al. Fibroblast activation protein alpha identifies mesenchymal stromal cells from human bone marrow. Brit J Haematol. 2008;142:827–30. doi: 10.1111/j.1365-2141.2008.07241.x. [DOI] [PubMed] [Google Scholar]
- 25.Wang LC, Lo A, Scholler J, Sun J, Majumdar RS, Kapoor V, et al. Targeting fibroblast activation protein in tumor stroma with chimeric antigen receptor T cells can inhibit tumor growth and augment host immunity without severe toxicity. Cancer Immunol Res. 2014;2:154–66. doi: 10.1158/2326-6066.CIR-13-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tchou J, Zhang PJ, Bi Y, Satija C, Marjumdar R, Stephen TL, et al. Fibroblast activation protein expression by stromal cells and tumor-associated macrophages in human breast cancer. Hum Path. 2013;44:2549–57. doi: 10.1016/j.humpath.2013.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ozdemir BC, Pentcheva-Hoang T, Carstens JL, Zheng X, Wu CC, Simpson TR, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719–34. doi: 10.1016/j.ccr.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lo A, Wang LC, Scholler J, Monslow J, Avery D, Newick K, et al. Tumor-Promoting Desmoplasia Is Disrupted by Depleting FAP-Expressing Stromal Cells. Cancer Res. 2015;75:2800–10. doi: 10.1158/0008-5472.CAN-14-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arnold JN, Magiera L, Kraman M, Fearon DT. Tumoral immune suppression by macrophages expressing fibroblast activation protein-alpha and heme oxygenase-1. Cancer Immunol Res. 2014;2:121–6. doi: 10.1158/2326-6066.CIR-13-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quante M, Tu SP, Tomita H, Gonda T, Wang SS, Takashi S, et al. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell. 2011;19:257–72. doi: 10.1016/j.ccr.2011.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee CH, Shah B, Moioli EK, Mao JJ. CTGF directs fibroblast differentiation from human mesenchymal stem/stromal cells and defines connective tissue healing in a rodent injury model. J Clin Invest. 2010;120:3340–9. doi: 10.1172/JCI43230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ronnov-Jessen L, Petersen OW. Induction of alpha-smooth muscle actin by transforming growth factor-beta 1 in quiescent human breast gland fibroblasts. Implications for myofibroblast generation in breast neoplasia. Lab Invest. 1993;68:696–707. [PubMed] [Google Scholar]
- 33.Kojima Y, Acar A, Eaton EN, Mellody KT, Scheel C, Ben-Porath I, et al. Autocrine TGF-beta and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proc Natl Acad Sci USA. 2010;107:20009–14. doi: 10.1073/pnas.1013805107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kordes C, Sawitza I, Haussinger D. Hepatic and pancreatic stellate cells in focus. Biol Chem. 2009;390:1003–12. doi: 10.1515/BC.2009.121. [DOI] [PubMed] [Google Scholar]
- 35.Bachem MG, Schneider E, Gross H, Weidenbach H, Schmid RM, Menke A, et al. Identification, culture, and characterization of pancreatic stellate cells in rats and humans. Gastroenterology. 1998;115:421–32. doi: 10.1016/s0016-5085(98)70209-4. [DOI] [PubMed] [Google Scholar]
- 36.Petersen OW, Lind Nielsen H, Gudjonsson T, Villadsen R, Ronnov-Jessen L, Bissell MJ. The plasticity of human breast carcinoma cells is more than epithelial to mesenchymal conversion. Breast Cancer Res. 2001;3:213–7. doi: 10.1186/bcr298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest. 2002;110:341–50. doi: 10.1172/JCI15518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zeisberg EM, Potenta S, Xie L, Zeisberg M, Kalluri R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007;67:10123–8. doi: 10.1158/0008-5472.CAN-07-3127. [DOI] [PubMed] [Google Scholar]
- 39.Kidd S, Spaeth E, Watson K, Burks J, Lu H, Klopp A, et al. Origins of the tumor microenvironment: quantitative assessment of adipose-derived and bone marrow-derived stroma. PloS One. 2012;7:e30563. doi: 10.1371/journal.pone.0030563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bochet L, Lehuede C, Dauvillier S, Wang YY, Dirat B, Laurent V, et al. Adipocyte-derived fibroblasts promote tumor progression and contribute to the desmoplastic reaction in breast cancer. Cancer Res. 2013;73:5657–68. doi: 10.1158/0008-5472.CAN-13-0530. [DOI] [PubMed] [Google Scholar]
- 41.Jotzu C, Alt E, Welte G, Li J, Hennessy BT, Devarajan E, et al. Adipose tissue-derived stem cells differentiate into carcinoma-associated fibroblast-like cells under the influence of tumor-derived factors. Anal Cell Pathol. 2010;33:61–79. doi: 10.3233/ACP-CLO-2010-0535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Direkze NC, Hodivala-Dilke K, Jeffery R, Hunt T, Poulsom R, Oukrif D, et al. Bone marrow contribution to tumor-associated myofibroblasts and fibroblasts. Cancer Res. 2004;64:8492–5. doi: 10.1158/0008-5472.CAN-04-1708. [DOI] [PubMed] [Google Scholar]
- 43.Mishra PJ, Mishra PJ, Humeniuk R, Medina DJ, Alexe G, Mesirov JP, et al. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Cancer Res. 2008;68:4331–9. doi: 10.1158/0008-5472.CAN-08-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feig C, Jones JO, Kraman M, Wells RJ, Deonarine A, Chan DS, et al. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc Natl Acad Sci USA. 2013;110:20212–7. doi: 10.1073/pnas.1320318110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stoker MG, Shearer M, O’Neill C. Growth inhibition of polyoma-transformed cells by contact with static normal fibroblasts. J Cell Sci. 1966;1:297–310. doi: 10.1242/jcs.1.3.297. [DOI] [PubMed] [Google Scholar]
- 46.Flaberg E, Markasz L, Petranyi G, Stuber G, Dicso F, Alchihabi N, et al. High-throughput live-cell imaging reveals differential inhibition of tumor cell proliferation by human fibroblasts. Int J Cancer. 2011;128:2793–802. doi: 10.1002/ijc.25612. [DOI] [PubMed] [Google Scholar]
- 47.Bhowmick NA, Chytil A, Plieth D, Gorska AE, Dumont N, Shappell S, et al. TGF-beta signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science. 2004;303:848–51. doi: 10.1126/science.1090922. [DOI] [PubMed] [Google Scholar]
- 48.Trimboli AJ, Cantemir-Stone CZ, Li F, Wallace JA, Merchant A, Creasap N, et al. Pten in stromal fibroblasts suppresses mammary epithelial tumours. Nature. 2009;461:1084–91. doi: 10.1038/nature08486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lujambio A, Akkari L, Simon J, Grace D, Tschaharganeh DF, Bolden JE, et al. Non-cell-autonomous tumor suppression by p53. Cell. 2013;153:449–60. doi: 10.1016/j.cell.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pallangyo CK, Ziegler PK, Greten FR. IKKbeta acts as a tumor suppressor in cancer-associated fibroblasts during intestinal tumorigenesis. J Exp Med. 2015;212:2253–66. doi: 10.1084/jem.20150576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim JW, Evans C, Weidemann A, Takeda N, Lee YS, Stockmann C, et al. Loss of fibroblast HIF-1alpha accelerates tumorigenesis. Cancer Res. 2012;72:3187–95. doi: 10.1158/0008-5472.CAN-12-0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maris P, Blomme A, Palacios AP, Costanza B, Bellahcene A, Bianchi E, et al. Asporin Is a Fibroblast-Derived TGF-beta1 Inhibitor and a Tumor Suppressor Associated with Good Prognosis in Breast Cancer. PLoS Med. 2015;12:e1001871. doi: 10.1371/journal.pmed.1001871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bissell MJ, Hines WC. Why don’t we get more cancer? A proposed role of the microenvironment in restraining cancer progression. Nat Med. 2011;17(3):320–9. doi: 10.1038/nm.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Madar S, Brosh R, Buganim Y, Ezra O, Goldstein I, Solomon H, et al. Modulated expression of WFDC1 during carcinogenesis and cellular senescence. Carcinogenesis. 2009;30:20–7. doi: 10.1093/carcin/bgn232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fiaschi T, Marini A, Giannoni E, Taddei ML, Gandellini P, De Donatis A, et al. Reciprocal metabolic reprogramming through lactate shuttle coordinately influences tumor-stroma interplay. Cancer Res. 2012;72:5130–40. doi: 10.1158/0008-5472.CAN-12-1949. [DOI] [PubMed] [Google Scholar]
- 56.Berdiel-Acer M, Sanz-Pamplona R, Calon A, Cuadras D, Berenguer A, Sanjuan X, et al. Differences between CAFs and their paired NCF from adjacent colonic mucosa reveal functional heterogeneity of CAFs, providing prognostic information. Mol Oncol. 2014;8:1290–305. doi: 10.1016/j.molonc.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chang CH, Qiu J, O’Sullivan D, Buck MD, Noguchi T, Curtis JD, et al. Metabolic Competition in the Tumor Microenvironment Is a Driver of Cancer Progression. Cell. 2015;162:1229–41. doi: 10.1016/j.cell.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ho PC, Bihuniak JD, Macintyre AN, Staron M, Liu X, Amezquita R, et al. Phosphoenolpyruvate Is a Metabolic Checkpoint of Anti-tumor T Cell Responses. Cell. 2015;162:1217–28. doi: 10.1016/j.cell.2015.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Siska PJ, Rathmell JC. T cell metabolic fitness in antitumor immunity. Trends Immunol. 2015;36:257–64. doi: 10.1016/j.it.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Valencia T, Kim JY, Abu-Baker S, Moscat-Pardos J, Ahn CS, Reina-Campos M, et al. Metabolic reprogramming of stromal fibroblasts through p62-mTORC1 signaling promotes inflammation and tumorigenesis. Cancer Cell. 2014;26:121–35. doi: 10.1016/j.ccr.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mitra AK, Zillhardt M, Hua Y, Tiwari P, Murmann AE, Peter ME, et al. MicroRNAs reprogram normal fibroblasts into cancer-associated fibroblasts in ovarian cancer. Cancer Discov. 2012;2:1100–8. doi: 10.1158/2159-8290.CD-12-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang D, Wang Y, Shi Z, Liu J, Sun P, Hou X, et al. Metabolic reprogramming of cancer-associated fibroblasts by IDH3alpha downregulation. Cell Rep. 2015;10:1335–48. doi: 10.1016/j.celrep.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 63.Bronisz A, Godlewski J, Wallace JA, Merchant AS, Nowicki MO, Mathsyaraja H, et al. Reprogramming of the tumour microenvironment by stromal PTEN-regulated miR-320. Nat Cell Biol. 2012;14:159–67. doi: 10.1038/ncb2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shimoda M, Principe S, Jackson HW, Luga V, Fang H, Molyneux SD, et al. Loss of the Timp gene family is sufficient for the acquisition of the CAF-like cell state. Nat Cell Biol. 2014;16:889–901. doi: 10.1038/ncb3021. [DOI] [PubMed] [Google Scholar]
- 65.Procopio MG, Laszlo C, Al Labban D, Kim DE, Bordignon P, Jo SH, et al. Combined CSL and p53 downregulation promotes cancer-associated fibroblast activation. Nat Cell Biol. 2015;17:1193–204. doi: 10.1038/ncb3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee KW, Yeo SY, Sung CO, Kim SH. Twist1 is a key regulator of cancer-associated fibroblasts. Cancer Res. 2015;75:73–85. doi: 10.1158/0008-5472.CAN-14-0350. [DOI] [PubMed] [Google Scholar]
- 67.Scherz-Shouval R, Santagata S, Mendillo ML, Sholl LM, Ben-Aharon I, Beck AH, et al. The Reprogramming of Tumor Stroma by HSF1 Is a Potent Enabler of Malignancy. Cell. 2014;158:564–78. doi: 10.1016/j.cell.2014.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Erez N, Truitt M, Olson P, Arron ST, Hanahan D. Cancer-Associated Fibroblasts Are Activated in Incipient Neoplasia to Orchestrate Tumor-Promoting Inflammation in an NF-kappaB-Dependent Manner. Cancer Cell. 2010;17:135–47. doi: 10.1016/j.ccr.2009.12.041. [DOI] [PubMed] [Google Scholar]
- 69.Campbell I, Polyak K, Haviv I. Clonal mutations in the cancer-associated fibroblasts: the case against genetic coevolution. Cancer Res. 2009;69:6765–8. doi: 10.1158/0008-5472.CAN-08-4253. discussion 69. [DOI] [PubMed] [Google Scholar]
- 70.Qiu W, Hu M, Sridhar A, Opeskin K, Fox S, Shipitsin M, et al. No evidence of clonal somatic genetic alterations in cancer-associated fibroblasts from human breast and ovarian carcinomas. Nature Genet. 2008;40:650–5. doi: 10.1038/ng.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Walter K, Omura N, Hong SM, Griffith M, Goggins M. Pancreatic cancer associated fibroblasts display normal allelotypes. Cancer Biol Ther. 2008;7:882–8. doi: 10.4161/cbt.7.6.5869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hosein AN, Wu M, Arcand SL, Lavallee S, Hebert J, Tonin PN, et al. Breast carcinoma-associated fibroblasts rarely contain p53 mutations or chromosomal aberrations. Cancer Res. 2010;70:5770–7. doi: 10.1158/0008-5472.CAN-10-0673. [DOI] [PubMed] [Google Scholar]
- 73.Hu M, Yao J, Cai L, Bachman KE, van den Brule F, Velculescu V, et al. Distinct epigenetic changes in the stromal cells of breast cancers. NatGenet. 2005;37:899–905. doi: 10.1038/ng1596. [DOI] [PubMed] [Google Scholar]
- 74.Chang PH, Hwang-Verslues WW, Chang YC, Chen CC, Hsiao M, Jeng YM, et al. Activation of Robo1 signaling of breast cancer cells by Slit2 from stromal fibroblast restrains tumorigenesis via blocking PI3K/Akt/beta-catenin pathway. Cancer Res. 2012;72:4652–61. doi: 10.1158/0008-5472.CAN-12-0877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ding N, Yu RT, Subramaniam N, Sherman MH, Wilson C, Rao R, et al. A vitamin D receptor/SMAD genomic circuit gates hepatic fibrotic response. Cell. 2013;153:601–13. doi: 10.1016/j.cell.2013.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sherman MH, Yu RT, Engle DD, Ding N, Atkins AR, Tiriac H, et al. Vitamin D receptor-mediated stromal reprogramming suppresses pancreatitis and enhances pancreatic cancer therapy. Cell. 2014;159:80–93. doi: 10.1016/j.cell.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pikarsky E, Porat RM, Stein I, Abramovitch R, Amit S, Kasem S, et al. NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 2004;431:461–6. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- 78.Peek RM, Jr, Crabtree JE. Helicobacter infection and gastric neoplasia. J Pathol. 2006;208:233–48. doi: 10.1002/path.1868. [DOI] [PubMed] [Google Scholar]
- 79.Guerra C, Schuhmacher AJ, Canamero M, Grippo PJ, Verdaguer L, Perez-Gallego L, et al. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 2007;11:291–302. doi: 10.1016/j.ccr.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 80.Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138:2101–14. e5. doi: 10.1053/j.gastro.2010.01.058. [DOI] [PubMed] [Google Scholar]
- 81.Pine SR, Mechanic LE, Enewold L, Chaturvedi AK, Katki HA, Zheng YL, et al. Increased levels of circulating interleukin 6, interleukin 8, C-reactive protein, and risk of lung cancer. J Natl Cancer I. 2011;103:1112–22. doi: 10.1093/jnci/djr216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Torres S, Bartolome RA, Mendes M, Barderas R, Fernandez-Acenero MJ, Pelaez-Garcia A, et al. Proteome profiling of cancer-associated fibroblasts identifies novel proinflammatory signatures and prognostic markers for colorectal cancer. Clin Cancer Res. 2013;19:6006–19. doi: 10.1158/1078-0432.CCR-13-1130. [DOI] [PubMed] [Google Scholar]
- 83.Rudisch A, Dewhurst MR, Horga LG, Kramer N, Harrer N, Dong M, et al. High EMT Signature Score of Invasive Non-Small Cell Lung Cancer (NSCLC) Cells Correlates with NFkappaB Driven Colony-Stimulating Factor 2 (CSF2/GM-CSF) Secretion by Neighboring Stromal Fibroblasts. PloS One. 2015;10:e0124283. doi: 10.1371/journal.pone.0124283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Vicent S, Sayles LC, Vaka D, Khatri P, Gevaert O, Chen R, et al. Cross-species functional analysis of cancer-associated fibroblasts identifies a critical role for CLCF1 and IL-6 in non-small cell lung cancer in vivo. Cancer Res. 2012;72:5744–56. doi: 10.1158/0008-5472.CAN-12-1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Stairs DB, Bayne LJ, Rhoades B, Vega ME, Waldron TJ, Kalabis J, et al. Deletion of p120-catenin results in a tumor microenvironment with inflammation and cancer that establishes it as a tumor suppressor gene. Cancer Cell. 2011;19:470–83. doi: 10.1016/j.ccr.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sierra-Filardi E, Nieto C, Dominguez-Soto A, Barroso R, Sanchez-Mateos P, Puig-Kroger A, et al. CCL2 shapes macrophage polarization by GM-CSF and M-CSF: identification of CCL2/CCR2-dependent gene expression profile. J Immunol. 2014;192:3858–67. doi: 10.4049/jimmunol.1302821. [DOI] [PubMed] [Google Scholar]
- 87.Gong D, Shi W, Yi SJ, Chen H, Groffen J, Heisterkamp N. TGFbeta signaling plays a critical role in promoting alternative macrophage activation. BMC Immunol. 2012;13:31. doi: 10.1186/1471-2172-13-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Comito G, Giannoni E, Segura CP, Barcellos-de-Souza P, Raspollini MR, Baroni G, et al. Cancer-associated fibroblasts and M2-polarized macrophages synergize during prostate carcinoma progression. Oncogene. 2014;33:2423–31. doi: 10.1038/onc.2013.191. [DOI] [PubMed] [Google Scholar]
- 89.Ene-Obong A, Clear AJ, Watt J, Wang J, Fatah R, Riches JC, et al. Activated pancreatic stellate cells sequester CD8+ T cells to reduce their infiltration of the juxtatumoral compartment of pancreatic ductal adenocarcinoma. Gastroenterology. 2013;145:1121–32. doi: 10.1053/j.gastro.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mace TA, Ameen Z, Collins A, Wojcik S, Mair M, Young GS, et al. Pancreatic cancer-associated stellate cells promote differentiation of myeloid-derived suppressor cells in a STAT3-dependent manner. Cancer Res. 2013;73:3007–18. doi: 10.1158/0008-5472.CAN-12-4601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stromnes IM, Brockenbrough JS, Izeradjene K, Carlson MA, Cuevas C, SImmons RM, et al. Targeted depletion of an MDSC subset unmasks pancreatic ductal adenocarcinoma to adaptive immunity. Gut. 2014;63:1769–81. doi: 10.1136/gutjnl-2013-306271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li T, Yang Y, Hua X, Wang G, Liu W, Jia C, et al. Hepatocellular carcinoma-associated fibroblasts trigger NK cell dysfunction via PGE2 and IDO. Cancer Lett. 2012;318:154–61. doi: 10.1016/j.canlet.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 93.Balsamo M, Scordamaglia F, Pietra G, Manzini C, Cantoni C, Boitano M, et al. Melanoma-associated fibroblasts modulate NK cell phenotype and antitumor cytotoxicity. P Natl Acad Sci USA. 2009;106:20847–52. doi: 10.1073/pnas.0906481106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Salmon H, Franciszkiewicz K, Damotte D, Dieu-Nosjean MC, Validire P, Trautmann A, et al. Matrix architecture defines the preferential localization and migration of T cells into the stroma of human lung tumors. J Clin Invest. 2012;122:899–910. doi: 10.1172/JCI45817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Caruana I, Savoldo B, Hoyos V, Weber G, Liu H, Kim ES, et al. Heparanase promotes tumor infiltration and antitumor activity of CAR-redirected T lymphocytes. Nat Med. 2015;21:524–9. doi: 10.1038/nm.3833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lee J, Fassnacht M, Nair S, Boczkowski D, Gilboa E. Tumor immunotherapy targeting fibroblast activation protein, a product expressed in tumor-associated fibroblasts. Cancer Res. 2005;65:11156–63. doi: 10.1158/0008-5472.CAN-05-2805. [DOI] [PubMed] [Google Scholar]
- 97.Loeffler M, Kruger JA, Niethammer AG, Reisfeld RA. Targeting tumor-associated fibroblasts improves cancer chemotherapy by increasing intratumoral drug uptake. J Clin Invest. 2006;116:1955–62. doi: 10.1172/JCI26532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ostermann E, Garin-Chesa P, Heider KH, Kalat M, Lamche H, Puri C, et al. Effective immunoconjugate therapy in cancer models targeting a serine protease of tumor fibroblasts. Clin Cancer Res. 2008;14:4584–92. doi: 10.1158/1078-0432.CCR-07-5211. [DOI] [PubMed] [Google Scholar]
- 99.Brennen WN, Rosen DM, Wang H, Isaacs JT, Denmeade SR. Targeting carcinoma-associated fibroblasts within the tumor stroma with a fibroblast activation protein-activated prodrug. J Natl Cancer I. 2012;104:1320–34. doi: 10.1093/jnci/djs336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kraman M, Bambrough PJ, Arnold JN, Roberts EW, Magiera L, Jones JO, et al. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science. 2010;330:827–30. doi: 10.1126/science.1195300. [DOI] [PubMed] [Google Scholar]
- 101.Provenzano PP, Cuevas C, Chang AE, Goel VK, Von Hoff DD, Hingorani SR. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21:418–29. doi: 10.1016/j.ccr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jacobetz MA, Chan DS, Neesse A, Bapiro TE, Cook N, Frese KK, et al. Hyaluronan impairs vascular function and drug delivery in a mouse model of pancreatic cancer. Gut. 2013;62:112–20. doi: 10.1136/gutjnl-2012-302529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moon E, Wang LC, Dolfi DV, Wilson CB, Ranganathan R, Sun J, et al. Multifactorial T cell hypofunction that is reversible can limit the efficacy of chimeric antigen receptor transduced human T cells. Clin Cancer Res. 2014;20:4262–73. doi: 10.1158/1078-0432.CCR-13-2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang E, Wang LC, Tsai CY, Bhoj V, Gershenson Z, Moon E, et al. Generation of Potent T-cell Immunotherapy for Cancer Using DAP12-Based, Multichain, Chimeric Immunoreceptors. Cancer Immunol Res. 2015;3:815–26. doi: 10.1158/2326-6066.CIR-15-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kakarla S, Chow K, Mata M, Shaffer DR, Song XT, Wu MF, et al. Antitumor effects of chimeric receptor engineered human T cells directed to tumor stroma. Mol Ther. 2013;21:1611–20. doi: 10.1038/mt.2013.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Petrausch U, Schuberth PC, Hagedorn C, Soltermann A, Tomaszek S, Stahel R, et al. Re-directed T cells for the treatment of fibroblast activation protein (FAP)-positive malignant pleural mesothelioma (FAPME-1) BMC Cancer. 2012;12:615. doi: 10.1186/1471-2407-12-615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tran E, Chinnasamy D, Yu A, Morgan RA, Lee CCR, Restifo NP, et al. Immune targeting of fibroblast activation protein triggers recognition of multipotent bone marrow stromal cells and cachexia. J Exp Med. 2013;210:1125–35. doi: 10.1084/jem.20130110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Roberts EW, Deonarine A, Jones JO, Denton AE, Feig C, Lyons SK, et al. Depletion of stromal cells expressing fibroblast activation protein-alpha from skeletal muscle and bone marrow results in cachexia and anemia. J Exp Med. 2013;210:1137–51. doi: 10.1084/jem.20122344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Denton AE, Roberts EW, Linterman MA, Fearon DT. Fibroblastic reticular cells of the lymph node are required for retention of resting but not activated CD8+ T cells. Proc Natl Acad Sci USA. 2014;111:12139–44. doi: 10.1073/pnas.1412910111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhao Y, Moon E, Carpenito C, et al. Multiple injections of electroporated autologous T cells expressing a chimeric antigen receptor mediate regression of human disseminated tumor. Cancer Res. 2010;70:9053–61. doi: 10.1158/0008-5472.CAN-10-2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wu CY, Roybal KT, Puchner EM, Onuffer J, Lim WA. Remote control of therapeutic T cells through a small molecule-gated chimeric receptor. Science. 2015;350:aab4077. doi: 10.1126/science.aab4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fedorov VD, Themeli M, Sadelain M. PD-1- and CTLA-4-based inhibitory chimeric antigen receptors (iCARs) divert off-target immunotherapy responses. Sci Transl Med. 2013;5:215ra172. doi: 10.1126/scitranslmed.3006597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kloss CC, Condomines M, Cartellieri M, Bachmann M, Sadelain M. Combinatorial antigen recognition with balanced signaling promotes selective tumor eradication by engineered T cells. Nat Biotechnol. 2013;31:71–5. doi: 10.1038/nbt.2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Roybal KT, Rupp LJ, Morsut L, Walker WJ, McNally KA, Park JS, et al. Precision Tumor Recognition by T Cells With Combinatorial Antigen-Sensing Circuits. Cell. 2016 doi: 10.1016/j.cell.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Santos AM, Jung J, Aziz N, Kissil JL, Pure E. Targeting fibroblast activation protein inhibits tumor stromagenesis and growth in mice. J Clin Invest. 2009;119:3613–25. doi: 10.1172/JCI38988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Park JE, Lenter MC, Zimmermann RN, Garin-Chesa P, Old LJ, Rettig WJ. Fibroblast activation protein, a dual specificity serine protease expressed in reactive human tumor stromal fibroblasts. J Biol Chem. 1999;274:36505–12. doi: 10.1074/jbc.274.51.36505. [DOI] [PubMed] [Google Scholar]
- 117.Edosada CY, Quan C, Tran T, Pham V, Wiesmann C, Fairbrother W, et al. Peptide substrate profiling defines fibroblast activation protein as an endopeptidase of strict Gly(2)-Pro(1)-cleaving specificity. FEBS Lett. 2006;580:1581–6. doi: 10.1016/j.febslet.2006.01.087. [DOI] [PubMed] [Google Scholar]
- 118.Lee KN, Jackson KW, Christiansen VJ, Chung KH, McKee PA. A novel plasma proteinase potentiates alpha2-antiplasmin inhibition of fibrin digestion. Blood. 2004;103:3783–8. doi: 10.1182/blood-2003-12-4240. [DOI] [PubMed] [Google Scholar]
- 119.Lee KN, Jackson KW, Christiansen VJ, Lee CS, Chun JG, McKee PA. Antiplasmin-cleaving enzyme is a soluble form of fibroblast activation protein. Blood. 2006;107:1397–404. doi: 10.1182/blood-2005-08-3452. [DOI] [PubMed] [Google Scholar]
- 120.Keane FM, Yao TW, Seelk S, Gall MG, Chowdhury S, Poplawski SE, et al. Quantitation of fibroblast activation protein (FAP)-specific protease activity in mouse, baboon and human fluids and organs. FEBS Open Bio. 2013;4:43–54. doi: 10.1016/j.fob.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Keane FM, Nadvi NA, Yao TW, Gorrell MD. Neuropeptide Y, B-type natriuretic peptide, substance P and peptide YY are novel substrates of fibroblast activation protein-alpha. FEBS J. 2011;278:1316–32. doi: 10.1111/j.1742-4658.2011.08051.x. [DOI] [PubMed] [Google Scholar]
- 122.Levy MT, McCaughan GW, Abbott CA, Park JE, Cunningham AM, Muller E, et al. Fibroblast activation protein: a cell surface dipeptidyl peptidase and gelatinase expressed by stellate cells at the tissue remodelling interface in human cirrhosis. Hepatology. 1999;29:1768–78. doi: 10.1002/hep.510290631. [DOI] [PubMed] [Google Scholar]
- 123.Christiansen VJ, Jackson KW, Lee KN, McKee PA. Effect of fibroblast activation protein and alpha2-antiplasmin cleaving enzyme on collagen types I, III, and IV. Arch Biochem Biophys. 2007;457:177–86. doi: 10.1016/j.abb.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhen EY, Jin Z, Ackermann BL, Thomas MK, Gutierrez JA. Circulating FGF21 Proteolytic Processing Mediated by Fibroblast Activation Protein. Biochem J. 2015 doi: 10.1042/BJ20151085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Maroni P, Bendinelli P, Matteucci E, Desiderio MA. HGF induces CXCR4 and CXCL12-mediated tumor invasion through Ets1 and NF-kappaB. Carcinogenesis. 2007;28:267–79. doi: 10.1093/carcin/bgl129. [DOI] [PubMed] [Google Scholar]
- 126.Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121:335–48. doi: 10.1016/j.cell.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 127.Aguilera KY, Rivera LB, Hur H, Carbon JG, Toombs JE, Goldstein CD, et al. Collagen signaling enhances tumor progression after anti-VEGF therapy in a murine model of pancreatic ductal adenocarcinoma. Cancer Res. 2014;74:1032–44. doi: 10.1158/0008-5472.CAN-13-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang K, Corsa CA, Ponik SM, Prior JL, Piwnica-Worms D, Eliceiri KW, et al. The collagen receptor discoidin domain receptor 2 stabilizes SNAIL1 to facilitate breast cancer metastasis. Nat Cell Biol. 2013;15:677–87. doi: 10.1038/ncb2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Valencia K, Ormazabal C, Zandueta C, Luis-Ravelo D, Anton I, Pajares MJ, et al. Inhibition of collagen receptor discoidin domain receptor-1 (DDR1) reduces cell survival, homing, and colonization in lung cancer bone metastasis. Clin Cancer Res. 2012;18:969–80. doi: 10.1158/1078-0432.CCR-11-1686. [DOI] [PubMed] [Google Scholar]
- 130.Rhim AD, Oberstein PE, Thomas DH, Mirek ET, Palermo CF, Sastra SA, et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25:735–47. doi: 10.1016/j.ccr.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]