Abstract
Purpose:
The purpose of this study is to assess the repeatability and agreement of five imaging devices, namely, the Pentacam (Oculus), Sirius (CSO), Orbscan IIz (Bausch and Lomb), Corvis (Oculus), and ultrasound pachymetry (UP, Tomey) in measuring steep keratometry (sKm), flat keratometry (fKm), central corneal thickness (CCT), thinnest corneal thickness (TCT), and anterior chamber depth (ACD) in healthy individuals.
Design:
This was prospective, comparative study.
Subjects:
Forty-six healthy Indian patients.
Materials and Methods:
Forty-six eyes of 46 healthy participants underwent three consecutive scans on each device by a single examiner. Within-subject standard deviation, test–retest repeatability (TRT), and coefficient of variation (COV) for assessing repeatability and Bland–Altman plots for the agreement between the mean measurements of each machine were analyzed.
Main Outcome Measures:
The repeatability and agreement between the five devices for the measurements of sKm, fKm, CCT, TCT, and ACD.
Results:
The TRT of sKm measurements ranged between 0.23 diopter (D) (with Pentacam) and 0.83 D (with Orbscan). The same of fKm, TCT, ACD, and CCT measurements ranged between 0.28 D (with Pentacam) and 0.74 D (with Sirius), 7.78 μm (Sirius) and 19.81 μm (Orbscan), 0.05 mm (Orbscan) and 0.07 (Sirius), and 7.36 μm (Sirius) and 18.02 μm (Orbscan), respectively. The TRT of sKm and fKm measurements with Pentacam was significantly lower than those with Orbscan and Sirius. The TRT of TCT measurement with Sirius was significantly lower than that with Pentacam (4.53 μm) and Orbscan (7.15 μm). There were statistically significant differences in the mean measurements of all parameters between the devices. The 95% limit of agreement on the Bland–Altman analysis was wide for the measurement pairs with all the devices. Significant proportional bias in the agreement was detected for TCT measurements with all the device pairs and for the ACD measurements between Sirius and Pentacam.
Conclusions:
The repeatability estimates of sKm, fKm, TCT, ACD, and CCT measurements with Pentacam, Orbscan, Sirius, Corvis, and UP in Indian eyes were good. However, the differences in the measurements between the devices were statistically significant and the same cannot be used interchangeably for anterior segments measurements.
Key words: Central corneal thickness, instruments, keratometry
Since the advent of keratorefractive surgery, a large number of topographers have made their way into the market. It is imperative for a keratorefractive surgeon to determine an accurate estimation of anterior segment parameters by these devices as well as a sound repeatability by each machine to assess a patient's cornea before refractive surgery. This is necessary to avoid disastrous outcomes of other uncomplicated procedure.[1,2,3,4]
In clinical practice, it is not feasible to obtain direct measurements of characteristics such as corneal thickness or refractive power. Therefore, indirect measurements are used as surrogate measures of the same.[5] The central corneal thickness (CCT) is one of the most important parameters that needs to be assessed before planning refractive surgery and a variety of sophisticated instruments have been developed over the past years to measure it, namely, the scanning slit topography, Scheimpflug methods, specular microscopy, confocal microscopy, and anterior segment optical. However, ultrasound pachymetry (UP) is still considered the gold standard.[1] Since it is a contact pachymetry, there is a risk of injuring the cornea and increasing the potential for spread of infections.[6] Accurate measurements of these parameters are also importance for the cataract surgeon as they are used to calculate the power of the intraocular lens (IOL).
Anterior chamber depth (ACD) assessment is important for the screening of primary angle-closure glaucoma and before surgery to avoid endothelial damage.[7] It is also essential for the preoperative planning of phakic IOL implantation as well as postoperatively for the assessment of the vault. Until now, there are no reports that have compared the steep keratometry (sKm), flat keratometry (fKm), CCT, thinnest corneal thickness (TCT), and ACD using five different devices. The purpose of this study was to evaluate the agreement and repeatability of Corvis (Oculus Optikgerate GmbH, Germany), Orbscan (Bausch and Lomb Surgical Inc., San Dimas, CA), Pentacam (Oculus, Wetzlar, Germany), Sirius (Costruzione Strumenti Oftalmici, Italy), and UP (SP 3000, Tomey Corporation and Noritake-Shinmachi, Japan) for these measurements in healthy individuals.
Materials and Methods
This prospective, comparative study was conducted in a tertiary care eye hospital in India. The study was approved by the Institutional Review Board and carried out in accordance with the guidelines laid down by the Declaration of Helsinki. Written informed consents were obtained from all the patients before the commencement of the study. Forty-six eyes of 46 healthy participants were part of the study. Inclusion criteria included age more than 16 years with a refractive error up to ± 6 diopter (D) sphere and ±2 D cylinder. The exclusion criteria included a history of corneal pathology, previous intraocular surgery, corneal endothelial decompensation, corneal scarring, glaucoma, and use of contact lenses within the last 1-month of the study.
All patients underwent a complete ophthalmic examination including visual acuity assessment, intraocular pressure (IOP) measurement with a noncontact tonometer, and anterior segment and fundus evaluation. All tests were conducted in a darkened room by a single experienced examiner (Mukesh Kumar) with three sets of measurements per device for each eye in a random order. Randomization was performed using http://www.randomization.com. The patients were randomized between the Orbscan, Pentacam, Sirius, and Corvis followed by the UP. Only measurements that received an “OK” quality score on the Pentacam were included in the analysis. The Orbscan does not provide a quality score, but instead automatically rejects measurements deemed to be of an unacceptable quality. Measurements of sKm, fKm, CCT, TCT, and ACD were assessed for agreement between the devices. For the purpose of uniformity, the ACD used in this study was defined as the depth from the endothelium to the anterior lens capsule for all devices.
Instruments
Corvis
Corvis is a noncontact tonometer equipped with an optical pachymetry function that measures the IOP and CCT using an air puff. The device increases the air pressure puffed onto the cornea in proportion to time and applanates the shape of the cornea from the normal convex surface to a concave one. During the air puff, the eye is illuminated by a 9 mm slit and a high-speed built-in camera records the movement of the eye at the rate of 4000 images/s. The camera captures a sequence of 140 Scheimpflug images of the applanated cornea, which are analyzed by the system software. The device then calculates the time that was required to applanate the cornea.
Orbscan
The Orbscan topographer works on the principle of scanning slit technology. It produces multiple slit-lamp images of the anterior segment using a camera moving horizontally. The CCT is then calculated by the difference in elevation between the anterior and posterior surfaces. An acoustic equivalent correction of 0.92 is used as the default setting to calculate the final corneal thickness value.
Sirius
The Sirius system combines a monochromatic 360° rotating Scheimpflug camera with a Placido disk-based corneal topographer. A series of 25 Scheimpflug images and a Placido top-view image are analyzed to produce the anterior corneal, posterior corneal, and anterior lens surface profiles. The ring edges are detected on the Placido image so that the height, slope, and curvature data are calculated using the arc-step method with conic curves. The system can measure 35,632 points from the anterior cornea and 30,000 points from the posterior corneal surface. A pachymetric map is then reconstructed using the data from both corneal surfaces.
Pentacam
The Pentacam machine uses a rotating Scheimpflug camera and a monochromatic slit-light source that rotate together around the optical axes of the eye to calculate a three-dimensional model of the anterior segment. For better comparability with Sirius, a scan setting of 25 was chosen for the Pentacam as well. A total of 25 images are captured within 2 s, with each slit image composed of 25,000 points including 500 true elevation points. We used the four-map refractive map of the Pentacam to plot the anterior corneal and pachymetry parameters.
Ultrasound pachymetry
The UP is a contact method used to measure the CCT. Three values were obtained from each point with a standard deviation of <2 µm while using an ultrasound velocity of 1640 m/s. The mean CCT value was used for comparison between different devices.
Statistical analysis
Statistical Package for the Social Sciences version 17.0 (SPSS, Inc., Chicago, IL, USA) was used for the statistical analysis. Normality of data was confirmed using the Kolmogorov–Smirnov test and graphical methods. A P < 0.05 was considered statistically significant. Repeatability was assessed by within-subject standard deviation (Sw), test-retest repeatability (TRT), and within-subject coefficient of variance (COV = 100 × Sw/overall mean). The Sw was calculated as the square root of the within-subject mean square error (the unbiased estimator of the component of variance due to random error) in a one-way random effects model. The TRT was calculated as 2.77 times Sw. The COV was calculated according to the root mean square method.
The mean parameter measurements with different instruments were compared by repeated measures ANOVA in the case of normally distributed variables and Friedman's test in the case of nonnormally distributed variables. Bland–Altman plots were used to assess the limit of agreement (LoA) between the measurements with the two devices as plotted against their mean. The mean difference between the measurements on the Bland–Altman plot is an estimate of the fixed bias in the measurements, which is the relationship of the difference in the measurements and the mean of the measurements. The presence of proportional bias indicates that the devices do not agree equally through the range of measurements. Proportional bias was formally evaluated by regressing the difference between the measurements with two devices on the average of the measurements with two devices.
Results
Forty-six eyes of 22 female and 24 male patients with a mean age of 24.05 ± 5.24 (range 15–37) years were analyzed. Demographic detail of the participants is included in Table 1. There were 24 right eyes and 22 left eyes, chosen according to a table of random numbers. Table 2 shows the Sw, TRT, and COV for sKm, fKm, CCT, TCT, and ACD measurements. The Sw and TRT of sKm and fKm measurements of Pentacam were statistically significantly (P < 0.001) lower than those of Sirius and Orbscan. The Sw and TRT of CCT measurements of Sirius were lower than those of Pentacam, Orbscan, Corvis, and UP. The Sw and TRT of TCT measurements of Sirius were lower than the rest of the four instruments. The Sw and TRT of ACD measurements of Orbscan were comparable to those of Sirius and Pentacam. The COV of sKm and fKm measurements of Pentacam were significantly lower than those of Sirius and Orbscan. The COV of CCT measurements of Sirius and Corvis were lower than those of Pentacam, Orbscan, and UP. The COV of TCT measurement of Sirius was the lowest, followed by Pentacam and then Orbscan. The COV of ACD measurements of Sirius and Orbscan were lower than that of Pentacam. Table 3 shows the mean readings obtained by the instruments for all the anterior segment parameters. There were statistically significant differences (P < 0.05) noted in the parameter measurements between all the devices. Differences in the measurements between the device pairs are shown in Table 4. Table 4 also shows the agreement between the ocular parameters determined by the five instruments, including the fixed and proportional bias for pair-wise comparisons. Orbscan significantly overestimated (P < 0.001) sKm readings compared to Sirius and Pentacam, whereas it underestimated fKm (P < 0.001), ACD (P < 0.001), and TCT (P > 0.001) compared to the two. Differences between Sirius and Pentacam for all five ocular variables were statistically significant (P < 0.05), with Sirius yielding higher measurements for sKm, fKm, and ACD and Pentacam for TCT and CCT. Orbscan measured a higher CCT compared to Sirius, Pentacam, and Corvis except when compared to UP. Corvis measured a lower CCT when compared to Sirius, Pentacam, and Orbscan but not with UP. There was a statistical significant (P < 0.05) difference in CCT measured by all the five instruments except for Sirius-Corvis, Pentacam-Orbscan, and Orbscan-UP comparisons. The pair-wise comparisons for each of the five ocular variables showed significantly high correlations between the instruments. Fixed bias was present in the agreement between device pairs for fKm, ACD, and TCT measurements. Proportional bias was absent in the agreement between device pairs for sKm and fKm measurements.
Table 1.
Demographics of participants
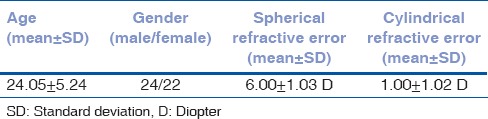
Table 2.
Repeatability estimates of different parameters (mean and 95% confidence interval) with Sirius, Pentacam, Orbscan, Corvis, and ultrasound pachymetry
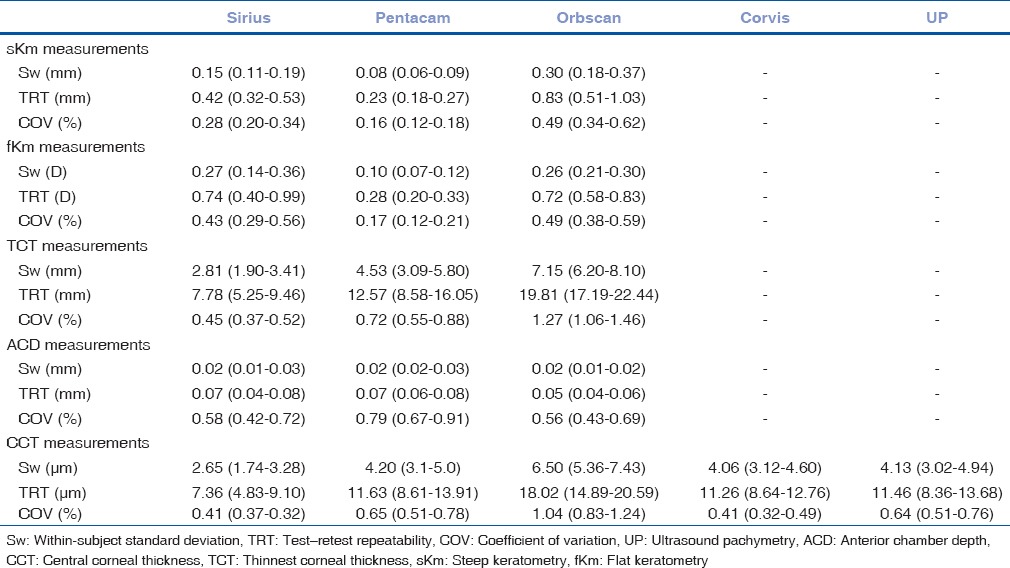
Table 3.
Steep keratometry, flat keratometry, thinnest corneal thickness, anterior chamber depth, and central corneal thickness measurements with Sirius, Pentacam, Orbscan, Corvis, and ultrasound pachymetry
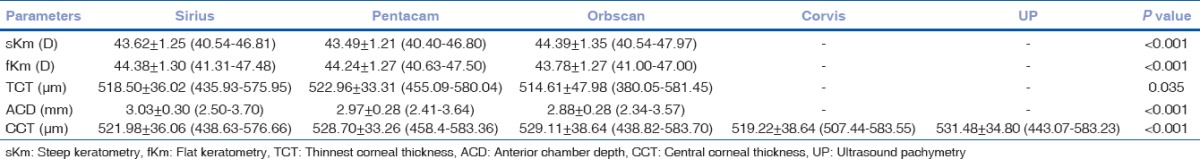
Table 4.
Summary statistics between five devices for central anterior segments parameter measurements
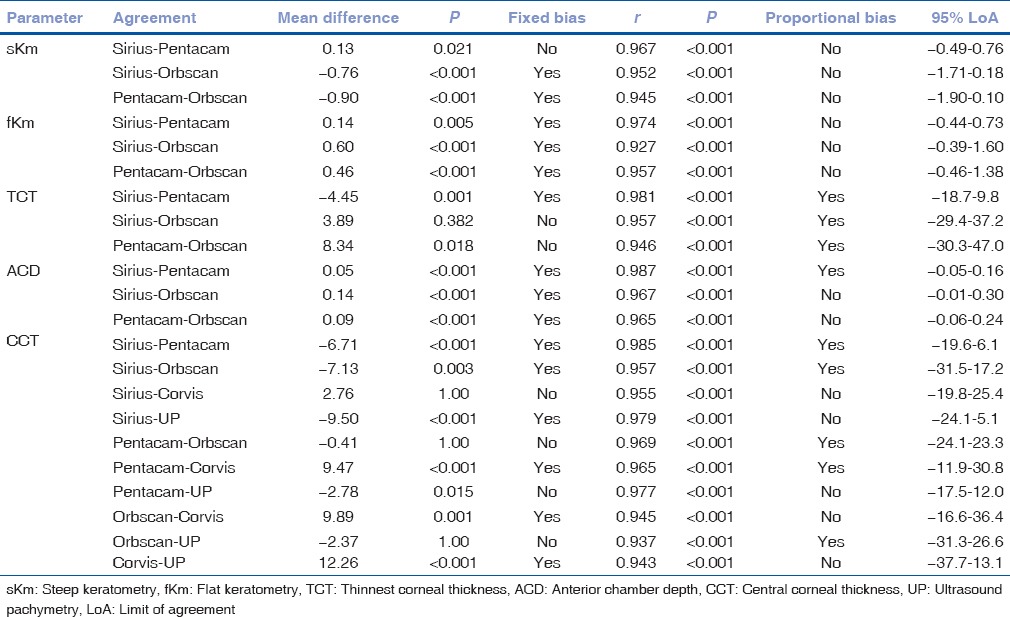
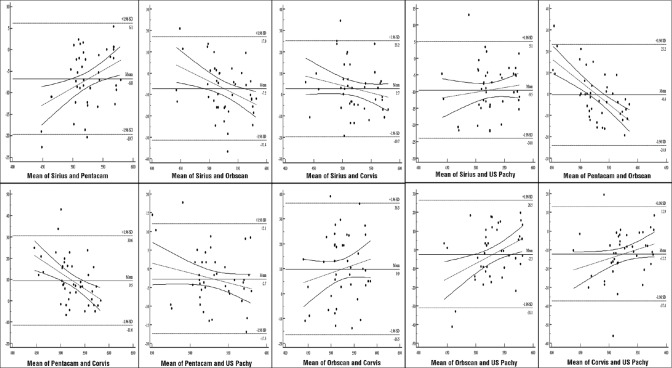
Fig. 1 shows the Bland–Altman plots with 95% LoA between devices pairs for CCT measurements.
Figure 1.
Bland–Altman plots showing the agreement among Sirius, Pentacam, Orbscan, Corvis, and ultrasound pachymetry techniques for the central corneal thickness measurements. The solid line represents the regression line difference and dotted curved lines represent its 95% confidence interval
Discussion
An accurate measurement of the anterior eye parameters including steep and fKm, central and thinnest corneal pachymetry, and ACD is important with on-going advancements for corneal refractive surgeries and phakic IOL implantation procedures.[8] In our study, we compared the CCT from five different optical devices including the UP to assess whether these devices produce comparable results for the healthy eyes. We have also studied the other ocular parameters such as sKm, fKm, TCT, and ACD with Sirius, Pentacam, and Orbscan to determine if they can be used interchangeably in routine clinical practice.
Keratometry is extensively used in the diagnosis and management of eye diseases. From contact lens fitting to orthokeratology, all need a precise corneal curvature measurement. In addition, the flat and sKm measurements are crucial for several surgical interventions such as refractive surgery and IOL power calculation for the cataract surgery. In this study, we have demonstrated that Sirius, Pentacam, and Orbscan measured significantly different sKm and fKm readings for healthy individuals.[2,3,9,10] We also found that between the three instruments, Pentacam determined the lowest Sw, TRT, and COV for all the ocular parameters, which is contradictory to the previous reports.[9] Between the two Scheimpflug camera systems, Pentacam, which employs slit-scanning photography, showed better repeatability measures compared to Sirius that uses Placido disc photography. However, better inter-instrument agreement in keratometry was noted between these two imaging systems compared to that with Orbscan in paired comparisons. This was more prominent with the sKm, which showed borderline mean differences (P = 0.02), high correlation with no fixed or proportional bias. This might be due to the Scheimpflug technology being used by the two imaging systems, which is consistent with an earlier report in keratoconus eyes.[11] Our results showed that the COV values determined for the fKm and sKm with Sirius were lower compared to the previous reports in healthy eyes[12] indicating a lower frequency of distribution. Fixed bias was present in all the paired comparisons in keratometry except Sirius-Pentacam, while Orbscan consistently underestimated fKm and overestimated sKm. The absence of any proportional bias in keratometry measurements indicates a lack of systemic disagreement between the compared instruments and methods.
An accurate CCT measurement is important for various corneal pathologies, IOP measurement and to assess a patient's eligibility for refractive surgery. The observations in this study suggest that CCT measurements obtained by these different devices were statistically significantly different (P < 0.05).[2,3,11,13,14,15,16,17] We found significantly lower CCT values with the Corvis when compared to Pentacam, Orbscan, and UP. Pair-wise comparisons showed that the Sirius-Corvis, Orbscan-Pentacam, and Orbscan-UP comparisons were not statistically significant (P = 1.000), indicating that these methods could be used interchangeably during CCT measurements for the healthy eyes. While CCT measured with Sirius showed the lowest Sw, TRT, and COV indicating better repeatability estimates, Orbscan showed the highest estimates. We found that these measures were grossly comparable between Pentacam, Corvis, and UP indicating similar precision for CCT measurement in healthy eyes. Five different instruments measured CCT and showed good correlation. With UP considered to be the gold standard in pachymetry, Orbscan provided the closest noncontact CCT (2.37 µm; P = 0.001). However, Orbscan performed poorly with wider repeatability measures for CCT.
TCT can be very close to CCT in healthy eyes wherein the central cornea is the thinnest zone. However, in corneal ectatic conditions or postrefractive surgery, the TCT can vary. This study shows that the Orbscan measured the lowest TCT compared to Sirius and Pentacam with a mean difference of 3.89 and 8.34 µm respectively. Our results yielded a better agreement between Sirius and Pentacam with LoAs ranging between −18.7 and 9.8 µm compared to the results reported by Savini et al.[18] which showed higher 95% LoAs (−34.68 to −48.87 µm). This agreement between the two Scheimpflug imaging systems was better than their agreements with Orbscan. Masoud et al.[12] and Montalbán et al.[19] investigated the repeatability and reproducibility of TCT in healthy eyes using the Sirius and found a higher Sw and COV. Both fixed and proportional bias was present in pair-wise comparison between the Sirius-Pentacam suggesting that in almost every participant Pentacam provided higher values, and the difference changed according to changes in TCT readings. Orbscan determined significantly lower TCT values compared to the Scheimpflug imaging systems with no fixed bias.
ACD measurement is an integral part of the preoperative assessment in cataract and refractive surgery for sophisticated IOL power calculation methods and phakic IOL implantation.[20] Salouti et al.[21] have found that Orbscan is not interchangeable with Galilei and Pentacam as it measures the ACD significantly higher. In contrast, our results showed that Orbscan determined significantly lower ACD values compared to Pentacam and Sirius. Fixed bias was present in this comparison suggesting that Orbscan underestimated ACD, but the difference was consistent throughout all the measurements. We found significant differences in ACD measurements between the Pentacam, Sirius, and Orbscan, which is similar to a previous report by Anayol et al.[22] All pair-wise comparisons for the ACD were statistically significant. Hence, these three devices cannot be used interchangeably for the ACD measurements.
Our study has few limitations. First, a single examiner did all the measurements; although this eliminates the risk of interobserver error, it may contribute to bias. Second, we have not included pathological or postoperative conditions.
Conclusions
Although Pentacam, Orbscan, Sirius, Corvis, and UP showed repeatable measurements for keratometry, corneal thickness and ACD measurement, there were significant differences in the measurements between each of the devices suggesting that these devices cannot be used interchangeably for all parameters. Sirius and Pentacam showed good inter-instrument agreement compared to others, which may be due to the same imaging technology used in both. Orbscan provided more aligned measurement with Pentacam and gold standard UP for CCT values. While it is hard to comment on which technique is the most accurate, they all vary in a systematic and stochastic manner in healthy eyes. Clinicians should, therefore, be aware that ocular parameter measurements are heavily influenced by the technique and technology used.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Konstantopoulos A, Hossain P, Anderson DF. Recent advances in ophthalmic anterior segment imaging: A new era for ophthalmic diagnosis? Br J Ophthalmol. 2007;91:551–7. doi: 10.1136/bjo.2006.103408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rao HL, Kumar AU, Kumar A, Chary S, Senthil S, Vaddavalli PK, et al. Evaluation of central corneal thickness measurement with RTVue spectral domain optical coherence tomography in normal subjects. Cornea. 2011;30:121–6. doi: 10.1097/ICO.0b013e3181e16c65. [DOI] [PubMed] [Google Scholar]
- 3.Dutta D, Rao HL, Addepalli UK, Vaddavalli PK. Corneal thickness in keratoconus: Comparing optical, ultrasound, and optical coherence tomography pachymetry. Ophthalmology. 2013;120:457–63. doi: 10.1016/j.ophtha.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 4.Reznicek L, Muth D, Kampik A, Neubauer AS, Hirneiss C. Evaluation of a novel scheimpflug-based non-contact tonometer in healthy subjects and patients with ocular hypertension and glaucoma. Br J Ophthalmol. 2013;97:1410–4. doi: 10.1136/bjophthalmol-2013-303400. [DOI] [PubMed] [Google Scholar]
- 5.Bland JM, Altman DG. Measurement error and correlation coefficients. BMJ. 1996;313:41–2. doi: 10.1136/bmj.313.7048.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buehl W, Stojanac D, Sacu S, Drexler W, Findl O. Comparison of three methods of measuring corneal thickness and anterior chamber depth. Am J Ophthalmol. 2006;141:7–12. doi: 10.1016/j.ajo.2005.08.048. [DOI] [PubMed] [Google Scholar]
- 7.Olsen T, Corydon L, Gimbel H. Intraocular lens power calculation with an improved anterior chamber depth prediction algorithm. J Cataract Refract Surg. 1995;21:313–9. doi: 10.1016/s0886-3350(13)80140-x. [DOI] [PubMed] [Google Scholar]
- 8.Savini G, Barboni P, Carbonelli M, Hoffer KJ. Repeatability of automatic measurements by a new scheimpflug camera combined with Placido topography. J Cataract Refract Surg. 2011;37:1809–16. doi: 10.1016/j.jcrs.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 9.De la Parra-Colín P, Garza-León M, Barrientos-Gutierrez T. Repeatability and comparability of anterior segment biometry obtained by the Sirius and the Pentacam analyzers. Int Ophthalmol. 2014;34:27–33. doi: 10.1007/s10792-013-9780-0. [DOI] [PubMed] [Google Scholar]
- 10.Tajbakhsh Z, Salouti R, Nowroozzadeh MH, Aghazadeh-Amiri M, Tabatabaee S, Zamani M. Comparison of keratometry measurements using the Pentacam HR, the Orbscan IIz, and the TMS-4 topographer. Ophthalmic Physiol Opt. 2012;32:539–46. doi: 10.1111/j.1475-1313.2012.00942.x. [DOI] [PubMed] [Google Scholar]
- 11.Shetty R, Arora V, Jayadev C, Nuijts RM, Kumar M, Puttaiah NK, et al. Repeatability and agreement of three scheimpflug-based imaging systems for measuring anterior segment parameters in keratoconus. Invest Ophthalmol Vis Sci. 2014;55:5263–8. doi: 10.1167/iovs.14-15055. [DOI] [PubMed] [Google Scholar]
- 12.Masoud M, Livny E, Bahar I. Repeatability and intrasession reproducibility obtained by the Sirius anterior segment analysis system. Eye Contact Lens. 2015;41:107–10. doi: 10.1097/ICL.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 13.Chen S, Huang J, Wen D, Chen W, Huang D, Wang Q. Measurement of central corneal thickness by high-resolution scheimpflug imaging, Fourier-domain optical coherence tomography and ultrasound pachymetry. Acta Ophthalmol. 2012;90:449–55. doi: 10.1111/j.1755-3768.2010.01947.x. [DOI] [PubMed] [Google Scholar]
- 14.Cheng AC, Rao SK, Lau S, Leung CK, Lam DS. Central corneal thickness measurements by ultrasound, Orbscan II, and Visante OCT after LASIK for myopia. J Refract Surg. 2008;24:361–5. doi: 10.3928/1081597X-20080401-08. [DOI] [PubMed] [Google Scholar]
- 15.González-Méijome JM, Cerviño A, Yebra-Pimentel E, Parafita MA. Central and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetry. J Cataract Refract Surg. 2003;29:125–32. doi: 10.1016/s0886-3350(02)01815-1. [DOI] [PubMed] [Google Scholar]
- 16.Kumar M, Shetty R, Jayadev C, Dutta D, Nicolsan MD, Nagaraj S, et al. Comparison of intraocular pressure measurement with scheimpflug-based noncontact tonometer with and without hydrogel contact lenses. Indian J Ophthalmol. 2015;63:323–6. doi: 10.4103/0301-4738.158072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uçakhan OO, Ozkan M, Kanpolat A. Corneal thickness measurements in normal and keratoconic eyes: Pentacam comprehensive eye scanner versus noncontact specular microscopy and ultrasound pachymetry. J Cataract Refract Surg. 2006;32:970–7. doi: 10.1016/j.jcrs.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 18.Savini G, Carbonelli M, Sbreglia A, Barboni P, Deluigi G, Hoffer KJ. Comparison of anterior segment measurements by 3 Scheimpflug tomographers and 1 Placido corneal topographer. J Cataract Refract Surg. 2011;37:1679–85. doi: 10.1016/j.jcrs.2011.03.055. [DOI] [PubMed] [Google Scholar]
- 19.Montalbán R, Alió JL, Javaloy J, Piñero DP. Intrasubject repeatability in keratoconus-eye measurements obtained with a new scheimpflug photography-based system. J Cataract Refract Surg. 2013;39:211–8. doi: 10.1016/j.jcrs.2012.10.033. [DOI] [PubMed] [Google Scholar]
- 20.Jahadi Hosseini HR, Katbab A, Khalili MR, Abtahi MB. Comparison of corneal thickness measurements using Galilei, HR Pentacam, and ultrasound. Cornea. 2010;29:1091–5. doi: 10.1097/ICO.0b013e3181cf98e5. [DOI] [PubMed] [Google Scholar]
- 21.Salouti R, Nowroozzadeh MH, Zamani M, Fard AH, Niknam S. Comparison of anterior and posterior elevation map measurements between 2 scheimpflug imaging systems. J Cataract Refract Surg. 2009;35:856–62. doi: 10.1016/j.jcrs.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Anayol MA, Güler E, Yagci R, Sekeroglu MA, Ylmazoglu M, Trhs H, et al. Comparison of central corneal thickness, thinnest corneal thickness, anterior chamber depth, and simulated keratometry using galilei, Pentacam, and Sirius devices. Cornea. 2014;33:582–6. doi: 10.1097/ICO.0000000000000119. [DOI] [PubMed] [Google Scholar]