Abstract
This study aims to report the use of mini-scleral contact lens in the management of mucous membrane pemphigoid (MMP) with persistent epithelial defects. A 68-year-old male with a history of ocular pain and declining visual acuity was referred to our clinic with a diagnosis of MMP. His corrected distance visual acuity (CDVA) was 20/200 in the right eye and 20/100 in the left eye. Despite being on lubricants, topical steroids and intravenous cyclophosphamide, the patient developed persistent corneal epithelial defects in both eyes. He was then given a trial of mini-scleral lenses. Within 4 weeks, corneal epithelial defects healed, and at 6 months, the CDVA had improved to 20/50 in the right eye and 20/40 in the left eye. By improving the corneal surface integrity and visual function, mini-scleral lenses can play a role in the visual rehabilitation of patients with MMP.
Key words: Epithelial defects, mini-scleral lens, mucous membrane pemphigoid
Chronic cicatricial conjunctivitis is a group of diseases characterized by progressive scarring of the ocular surface with autoimmune diseases such as mucous membrane pemphigoid (MMP) being important causes.[1] Ocular MMP, also known as ocular cicatricial pemphigoid, is a sight-threatening, subepithelial, blistering disease characterized by bilateral, asymmetrical, chronic, progressive or relapsing conjunctivitis with cicatrization, corneal vascularization, and opacification.[2] Treatment options including preservative-free artificial tears, topical cyclosporine A, punctal plugs, and scleral contact lenses to improve the health of the ocular surface and visual function.[2,3,4] This case report describes the use of Rose K2 mini-scleral lenses (Menicon Co. Ltd., Nagoya, Japan) for successful treatment of a persistent corneal epithelial defect secondary to MMP that was not responsive to conventional therapy.
Case Report
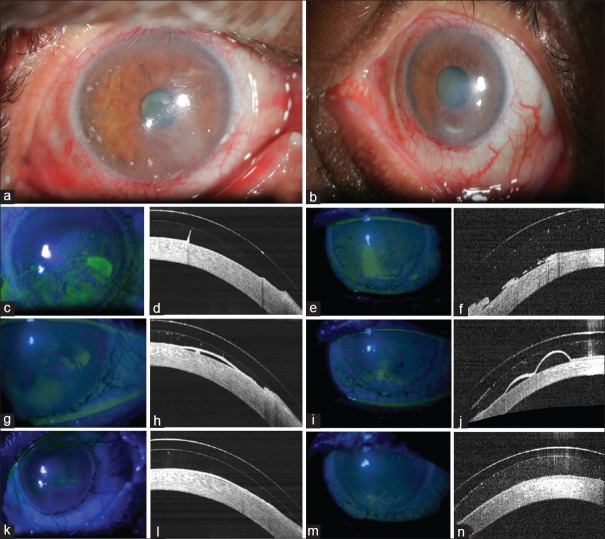
A 68-year-old male diagnosed with MMP presented with complaints of dryness in both eyes. On examination, his corrected distance visual acuity (CDVA) was 20/200 in the right eye and 20/100 in the left eye. The patient had been using topical carboxymethyl cellulose 0.5% (Optive, Allergan, Irvine CA, USA) four times a day, hydroxyl propyl methyl cellulose gel at night, and oral mycophenolate mofetil 1000 mg and cyclophosphamide 50 mg, both twice daily. He had received intravenous cyclophosphamide 50 mg infusion on multiple occasions previously. Slit lamp examination showed a symblepharon, shorting of the inferior fornix, meibomian gland dysfunction, and marginal corneal superficial vascularization in both eyes. An epithelial defect 2.5 mm × 1.5 mm in the right eye [Fig. 1a] and 2 mm × 1 mm [Fig. 1b] in the left eye was noted. A therapeutic contact lens (Air-Optix Aqua, Alcon, TX, USA) trial failed to heal the epithelial defect despite several attempts. The poor ocular surface caused the contact lens to dislodge frequently.
Figure 1.
(a and b) The both eye cornea had an epithelial defect. (c-f) Rapid reepithelization was observed after starting mini-scleral lens, epithelial defect decreasing to 1.5 mm × 1 mm after 4 days. (g-j) 0.5 mm decreasing after 8 days. (k-n) Complete resolution of the epithelial defect after 4 weeks in both eyes
The patient was then fitted with a Rose K2 mini-scleral contact lens in an attempt to alleviate symptoms and promote healing. The lenses, made of Menicon Z, had a base curve of 6.60 mm, diameter of 14.6 mm, and power of −5.50 D for both eyes. He was advised to wear them during the waking hours and to switch to soft contact lenses at night. He was asked to soak them in Boston Simplus solution (Bausch and Lomb, Rochester, NY, USA) and clean the lens periodically. Rapid reepithelization was observed, and the size of corneal epithelial defect decreasing to 1.5 mm × 1 mm within 4 days [Fig. 1c–f] and 0.5 mm in 8 days [Fig. 1g–j] in both eyes. Complete resolution of the epithelial defect was seen after 4 weeks in both eyes [Fig. 1k–n]. In addition, the CDVA improved to 20/50 in the right eye and 20/40 in the left eye. The patient's visual acuity and corneal surface integrity have remained stable for 6 months of follow-up. He is currently on topical lubricants and tablet endotoxin 100 mg once daily.
Discussion
MMP is a group of rare chronic autoimmune disorders affecting mucosal surfaces. The eye and mouth are commonly involved and requires both topical and systemic therapy to control inflammation. Some of the accepted treatment modalities include artificial tear substitutes, steroids, topical cyclosporine, scleral contact lens, and tarsorrhaphy.[5,6] Despite trying all the above options, our patient showed a poor response, thereby posing a therapeutic challenge. Hence, we tried using a new treatment modality, the Rose K2 mini-scleral contact lenses, which are known to provide rapid healing of epithelial defects in similar conditions.[7]
Large diameter fluid-ventilated rigid gas permeable lenses such as the mini-scleral lenses are uniquely designed to provide protection for the entire ocular surface. As they are primarily supported by the sclera, they maintaining a postlens reservoir that continuously lubricates the corneal surface, allowing epithelial defects to heal in addition to protecting the entire cornea surface against irritants and friction generated from eyelid movement. In addition, the mini-scleral lenses have a high oxygen permeability, which may reduce the development of corneal edema. The efficacy of scleral lenses in the treatment of other ocular surface diseases has been previously demonstrated.[8,9,10,11] They have minimal adverse effects and useful for postradiotherapy complications, Stevens–Johnson syndrome, recurrent corneal erosions, and congenital or postsurgical lid defects.[12]
Managing ocular symptoms of MMP can be difficult and frustrating for the patient and treating physician. Rose K2 mini-scleral contact lenses offer improvement in both corneal surface integrity and visual acuity. Considering the risk and morbidity of surgical therapies, these lenses should be considered a viable treatment option in MMP patients with ocular involvement.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chan LS, Ahmed AR, Anhalt GJ, Bernauer W, Cooper KD, Elder MJ, et al. The first international consensus on mucous membrane pemphigoid: Definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol. 2002;138:370–9. doi: 10.1001/archderm.138.3.370. [DOI] [PubMed] [Google Scholar]
- 2.Foster CS, Sainz De La Maza M. Ocular cicatricial pemphigoid review. Curr Opin Allergy Clin Immunol. 2004;4:435–9. doi: 10.1097/00130832-200410000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Schornack MM, Baratz KH. Ocular cicatricial pemphigoid: The role of scleral lenses in disease management. Cornea. 2009;28:1170–2. doi: 10.1097/ICO.0b013e318199fa56. [DOI] [PubMed] [Google Scholar]
- 4.Lemp MA. Advances in understanding and managing dry eye disease. Am J Ophthalmol. 2008;146:350–6. doi: 10.1016/j.ajo.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Miserocchi E, Baltatzis S, Roque MR, Ahmed AR, Foster CS. The effect of treatment and its related side effects in patients with severe ocular cicatricial pemphigoid. Ophthalmology. 2002;109:111–8. doi: 10.1016/s0161-6420(01)00863-6. [DOI] [PubMed] [Google Scholar]
- 6.Romero-Rangel T, Stavrou P, Cotter J, Rosenthal P, Baltatzis S, Foster CS. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000;130:25–32. doi: 10.1016/s0002-9394(00)00378-0. [DOI] [PubMed] [Google Scholar]
- 7.Pullum KW, Stapleton FJ. Scleral lens induced corneal swelling: What is the effect of varying Dk and lens thickness? CLAO J. 1997;23:259–63. [PubMed] [Google Scholar]
- 8.Pullum K, Buckley R. Therapeutic and ocular surface indications for scleral contact lenses. Ocul Surf. 2007;5:40–8. doi: 10.1016/s1542-0124(12)70051-4. [DOI] [PubMed] [Google Scholar]
- 9.Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005;31:130–4. doi: 10.1097/01.icl.0000152492.98553.8d. [DOI] [PubMed] [Google Scholar]
- 10.Schornack MM, Baratz KH, Patel SV, Maguire LJ. Jupiter scleral lenses in the management of chronic graft versus host disease. Eye Contact Lens. 2008;34:302–5. doi: 10.1097/ICL.0b013e318188e205. [DOI] [PubMed] [Google Scholar]
- 11.Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. Am J Ophthalmol. 2000;130:33–41. doi: 10.1016/s0002-9394(00)00379-2. [DOI] [PubMed] [Google Scholar]
- 12.Tappin MJ, Pullum KW, Buckley RJ. Scleral contact lenses for overnight wear in the management of ocular surface disorders. Eye (Lond) 2001;15(Pt 2):168–72. doi: 10.1038/eye.2001.54. [DOI] [PubMed] [Google Scholar]