SUMMARY
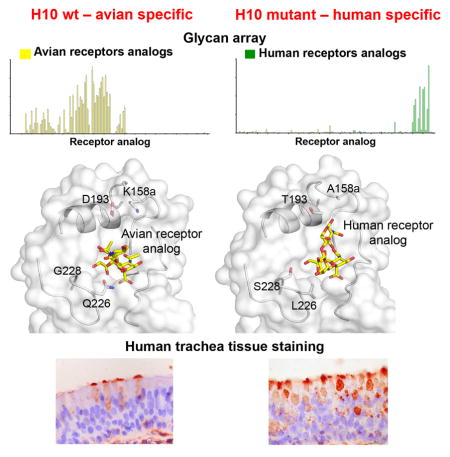
Adaptation of influenza A viruses to new hosts are rare events, but are the basis for emergence of new influenza pandemics in the human population. Thus, understanding the processes involved in such events is critical for anticipating potential pandemic threats. In 2013, the first case of human infection by an avian H10N8 virus was reported, yet the H10 HA maintains avian receptor specificity. However, the 150-loop of H10 HA, as well as related H7 and H15 subtypes, contains a two-residue insert that can potentially block human receptor binding. Mutation of the 150-loop on the background of Q226L and G228S mutations, which arose in the receptor-binding site of human pandemic H2 and H3 viruses, resulted in acquisition of human-type receptor specificity. Crystal structures of H10 HA mutants with human and avian receptors analogs, receptor binding studies, and tissue staining experiments illustrate the important role of the 150-loop in H10 receptor specificity.
Graphical abstract
INTRODUCTION
Three cases of human infection by H10N8 avian influenza A virus (IAV) (A/Jiangxi/IPB13a/b/c/2013) have been reported in China since December 2013, two of which were fatal (Chen et al., 2014; Garcia-Sastre and Schmolke, 2014). The prevailing evidence suggested that the H10N8 virus was of avian origin (Garcia-Sastre and Schmolke, 2014; Parry, 2014). Beside H10N8, two additional avian-origin viruses, H7N9 and H6N1, were isolated from human patients during 2013 making it a remarkable year for novel avian IAVs that crossed the species barrier and infected humans. The increase in human infections by new avian-origin influenza subtypes (also including H9N2 and H5N1) of avian origin in the last two decades (Freidl et al., 2014) has raised concern that these additional avian subtypes could give rise to novel human pandemic viruses.
Influenza viruses contain two surface glycoproteins, hemagglutinin (HA) and neuraminidase (NA). Based on serology, influenza A HA and NA proteins are classified into subtypes. So far 16 HA (H1–16) and 9 NA (N1–9) subtypes have been identified in wild aquatic birds (Fouchier et al., 2005; Gamblin and Skehel, 2010). Beside wild aquatic and domestic birds, influenza viruses can circulate in a variety of mammalian hosts, including humans, horses, pigs, dogs and marine mammals (Osterhaus et al., 2000; Webster et al., 1992). While circulating human-adapted viruses cause seasonal epidemics, zoonotic influenza viruses have the potential to initiate new pandemics. Throughout the last century, several avian and swine origin influenza viruses were able to cross the host specificity barrier and infect humans, but only three subtypes have caused pandemics: Spanish (1918 H1N1), Asian (1957 H2N2), Hong Kong (1968 H3N2) and novel swine 2009 H1N1. To transmit in the human population, the pandemic viruses required a shift in their receptor specificity to human-type sialosides (Matrosovich et al., 2009; Parrish and Kawaoka, 2005). The most important determinant in binding specificity is the linkage between the terminal sialic acid and the penultimate galactose. For avian viruses, the HAs preferentially bind glycans containing sialic acid in an α2–3 linkage to galactose, whereas human viruses bind predominantly to α2–6 linked sialosides (avian- and human-type receptors, respectively) (Matrosovich et al., 2009).
The HA receptor binding site (RBS) is a broad, shallow pocket located in the apex of the HA head domain and framed by four structural elements: the 130-loop, 150-loop, 190-helix, and 220-loop. The heart of the RBS is comprised of Tyr98, Trp153, His183, and Tyr195 (H3 numbering), which are highly conserved in HAs from different subtypes (Ha et al., 2001; Skehel and Wiley, 2000). Understanding which mutations facilitate a switch in receptor specificity is crucial for development of effective preventive and therapeutic measures. Previous studies on pandemic influenza strains have shown that two different pairs of substitutions of four key RBS residues were all that were required to switch HA receptor specificity (E190D and G225D for 1918 and 2009 H1N1 and Q226L and G228S for 1957 H2N2 and 1968 H3N2). However, neither pair of mutations is sufficient to switch specificity in HAs from other avian subtypes that have caused human infections. Indeed, for avian H5N1, E190D and G225D mutations abolished receptor binding, while Q226L and G228S mutations enabled only partial recognition of α2–6 linked receptors without loss of α2–3 binding (Stevens et al., 2006b). Further mutation at Thr160 or a double mutation at Asn158 (N158D, loss of glycosylation) and Gln224 (N224K), switched preference to human receptors, albeit with low affinity (Chen et al., 2012; de Vries et al., 2014; Herfst et al., 2012; Imai et al., 2012; Xiong et al., 2013a; Zhang et al., 2013).
In the last decade, glycan arrays have become a powerful tool to investigate influenza receptor specificity (Paulson and de Vries, 2013; Stevens et al., 2006a). Recently, we developed expanded, custom glycan arrays (Nycholat et al., 2013; Peng et al., 2012) that included extended linear and branched O-linked glycans as well as bi- and tri-antennary N-linked glycans with poly-N-acetyl-lactosamine extensions (2 to 5 repeats of Galβ1–4GlcNAc (LN)) capped with either α2–3 or α2–6 linked sialic acids (Peng et al., 2016). Such extended sialosides have been observed in a human airway epithelial cell line and in human and ferret upper airway tissues (Chandrasekaran et al., 2008; Jia et al., 2014; Walther et al., 2013), and provide a broader range of biologically relevant glycans for analysis of human-type receptor specificity. Weak or loss of binding to human-type receptors has been reported for more recent H3N2 isolates (Lin et al., 2012; Medeiros et al., 2001; Nobusawa et al., 2000; Yang et al., 2015), but our expanded glycan array shows that these viruses bind strongly to human-type receptors, with preference for extended branched N- and O-linked glycans (Peng et al., 2016; Bateman et al., 2010; de Vries et al., 2011).
We have previously shown that human-isolated H10N8 HA retains a strong preference for avian receptor analogs (Zhang et al., 2015). Introduction of mutations that enabled adaption of receptor specificity in human pandemic viruses failed to switch receptor specificity in H10N8. Here, we identify and characterize mutations in the H10 RBS that switch receptor specificity. Based on sequence and structural analysis of the H10 HA RBS, we hypothesized that the extended 150-loop of H10 HA might block binding of human receptors to the RBS. Thus, we explored modifications of the H10 150-loop to elucidate any changes in receptor specificity using our expanded sialoside glycan array, by binding to epithelial cells of human trachea, and by x-ray crystallography.
RESULTS
Characterization of the Elongated 150-loop of H10 HA
IAV HAs can be phylogenetically divided into two groups (Air, 1981; Nobusawa et al., 1991; Wu et al., 2014), and further subdivided into sub-clades. H10 HAs are members of the H7–H10–H15 subgroup of group 2 (Figure S1B). Sequence alignment of human H10N8 HA with human pandemic strains and with viruses that have caused sporadic human infections reveals that the H10 150-loop contains a two-residue insertion, Lys158a and Gly158b (Figure S1A), which is present only in H7, H10 and H15 subtypes (Figure 1A). Superposition of the human H10 RBS subdomain (HA1 residues 117–265) onto other human and avian HAs shows that the extended H10 150-loop folds back over the RBS, as in H7 HA (Figure 1B). Moreover, Lys158a forms a roof over the upper part of the RBS.
Figure 1. The Role of the 150-loop in Receptor Specificity of H10 HA.
(A) Sequence alignment of the HA 150-loop sequences of representative IAV from all HA subtypes. The alignment shows the elongation of the 150-loop by two amino acids (designated 158a and 158b) in H7, H10 and H15 HAs (insert colored in black). (B) Superposition of the RBS subdomains of H10 HA (red), pandemic H1 (yellow, PDB 3AL4), pandemic H2 (green, PDB 3KU5), pandemic H3 (cyan, PDB 4FNK), VN1203 H5 (pink, PDB 2FK0), A/Taiwan/2/2013 H6 (magenta, PDB 4XKD) and Sh2H7 (gray, PDB 4N5J) HAs. The conserved secondary structural elements of the HA RBS (130-loop, 150-loop, 190-helix and 220-loop) and H10 Lys158a are labeled. (C) Glycan microarray analysis of recombinant wild-type and H10 HA RBS mutants. The H10K158aA (C2) and H10K158aG (C3) mutants bind specifically to α2–3 linked sialosides, similar to H10 wt HA (C1). (C4) The H10LS double mutant binds poorly to α2–3 and α2–6 linked sialosides. (C5) Mutating Lys158a to Ala on the background of H10LS now results in binding to α2–6 linked sialosides with only weak binding to α2–3 linked sialosides. (C6) Mutating Asp193 to Thr on the background of the H10LS-K158aA mutant reveals a complete switch in binding from α2–3 to α2–6 linked sialosides. The mean signal and standard error were calculated from six independent replicates on the array. α2–3 linked sialosides are shown in yellow bars (# 11 to 79 on the x axis) and α2–6 linked sialosides in green (# 80 to 135). Glycans 1 to 10 are non-sialylated controls (gray). (D) Binding of H10N8 wt and H10LS-K158aA-D193T mutant HAs to α2–3 and α2–6 linked receptors, as determined by glycan ELISA. H10 wt (left panels) binds selectively to glycans terminating in α2–3-linked sialic acids with no significant binding to α2–6 receptors. H10LS-K158aA-D193T (right panels) shows only slightly reduced avidity for avian α2–3 receptors but gain of strong binding to human α2–6 sialoglycans. All tested glycans are biantennary, N-linked receptor analogs with one to four Gal-GlcNAc repeats (LN1-4) after the terminal sialic acid. An asialo, mono-LN (LN-L) receptor was used as a negative binding control for each HA. The numbers of the glycans in the list of glycans imprinted on the microarray (Table S1) are indicated in brackets. See also Figure S1.
Human-type receptor analogs (α2–6 sialosides) generally bind in a cis conformation (with reference to the Sia-Gal bond), similar to the minimum energy solution conformation, that directs sialosides longer than three sugars toward the 190 helix and upper part of the RBS. In contrast, α2–3 linked sialosides exhibit an extended conformation that directs avian receptors out of the RBS (Chandrasekaran et al., 2008; Eisen et al., 1997; Elli et al., 2014; Sabesan et al., 1991). Modeling of human receptor analog LSTc (from pandemic strain A/Singapore/1/1957(H2N2), PDB entry 2WR7 as a representative of a human receptor analog in human HAs structures) to the H10 HA RBS (Figure S1C) reveals potential steric clashes (blue) indicating that this elongated loop might inhibit human receptor binding to the H10 RBS.
The Role of K158a in Host Specificity of H10 HA
To assess the role of K158a in receptor binding, H10 HAs with K158a mutated to Ala or Gly were expressed and then analyzed using our custom sialoside glycan array comprised of diverse α2–3 (#11–79) and α2–6 (#80–135) sialosides (Peng et al., 2016). A/Beijing/353/1989 H3N2 and A/Vietnam/1203/2004 H5N1 HA (VN1203) strains served as controls for human and avian specificity (Figure S1D). The H10K158aA and H10K158aG mutants retained α2–3 specificity with no detectable binding to α2–6 glycans (Figure 1C1–3) demonstrating that mutation of K158a is not sufficient by itself to convert H10 HA to human-type specificity.
As we have previously shown (Zhang et al., 2015), introducing Q226L, G228S or Q226L-G228S (H10LS) mutations in WT H10 HA results in loss of binding to α2–3 sialosides with no gain in binding to human-type α2–6 receptors (Figure 1C4; Figure S1D3–4). However, Lys158a to Ala or Gly on the H10LS double mutant (H10LS-K158aA and H10LS-K158aG) resulted in gain of binding to human-type receptors and dramatically reduced binding to avian-type receptors (Figures 1C5 and S1D5).
Asp193 is also directed into the H10 RBS and might also interfere with human analog binding (Figure S1E). D193T on wt H10 reduced binding to avian-type receptors (Figure S1D6) and on H10LS resulted in gain of binding to human-type receptors with only weak residual binding to avian-type receptors (Figure S1D7). Significantly, D193T on H10LS-K158aA (H10LS-K158aA-D193T) produced strong binding to human-type receptors (Figure 1C6) represented by long, branched, N-linked glycans (#121–131) (Table S1) similar to A/Cal/04/09 pandemic H1N1 (Peng et al., 2016) and A/Beijing/353/1989 H3N2 HAs (Figure S1D2). In some analyses, preferential binding to α2–6 linked sialosides was accompanied with weak residual binding to avian-type receptors. Similar results were obtained by introducing D193T onto H10LS-K158aG where binding was also observed to long, branched, O-linked human-type receptors (# 107–111) (Figure S1D8).
To quantify the change in the avidity of the H10 mutants, we used a glycan ELISA-type assay to assess binding of H10 wt and H10LS-K158aA-D193T to biantennary, N-linked sialosides with one to four LN repeats (LN1-4) (Figure 1D). H10 wt was selective for α2–3 sialosides (Kd apparent of 0.79–0.62 μg/ml, Table S2), with no detectable binding to α2–6 sialosides. For H10LS-K158aA-D193T, a significant increase in binding to α2–6 sialosides was detected (Kd 24.8–0.49 μg/ml), with slight reduction to α2–3 sialosides (Kd 1.55–0.84 μg/ml).
Structural Characterization of H10 HA Mutants with Human and Avian Receptor Analogs
To investigate the structural basis for change in receptor specificity, crystal structures of H10LS-K158aA-D193T, H10LS-K158aA and H10LS-D193T mutants were determined (Table S3) and were very similar to H10 wt (Ca RMSD of 0.38 Å), but with the RBS being more accessible to human-type receptors, especially for the K158aA mutants (Figure S2A).
The crystal structure of H10LS-K158aA-D193T HA with human receptor analogue 6′-SLNLN (NeuAcα2–6Galβ1–4GlcNAcβ1–3Galβ1–4GlcNA) (Figure 2A; Table S3) exhibited electron density for three of the five sugars in the RBS of protomers A and C (Figure S2B), but only Sia-1 in protomer B. As in H10 wt with human analog 6′-SLN (PDB 4XQO), Sia-1 makes hydrophobic interactions with Trp153 and hydrogen bonds to the conserved Tyr98, the 130-loop and 190-helix (Figures 2A and 2B). However, Sia-1 interactions with the 220-loop differ from wt H10 HA due to the Q226L and G228S mutations that result in loss of two hydrogen bonds to Sia-1. In addition, the G228S mutation displaces Sia-1 ~1 Å from the 220-loop towards the 130-loop (Figure 2C) and loss of interaction with His183 (Figure S2C).
Figure 2. Crystal Structure of the H10LS-K158aA-D193T Mutant in Complex with Human and Avian Receptor Analogs.
(A–C) The interactions between human receptor analog 6′-SLNLN and H10 HA RBS. The glycan structure of the 6′-SLNLN analog is represented in the upper part of the figure. The RBS conserved secondary structural elements are labeled and shown as ribbons. Selected RBS residues and the receptor analog are labeled and shown in sticks. Hydrogen bonds are indicated by black dashes between the human analog and the RBS of the H10LS-K158aA-D193T mutant (A) and H10 wt (B). (C) Superposition of the human receptor analog from the H10 wt HA complex (cyan) onto that of the H10LS-K158aA-D193T mutant (white) indicating slight displacement of the human analog in the RBS and conformational changes arising from a slight rotation around the linkage between Sia-1 and Gal-2. The superposition was done on the RBS subdomain. For clarity, only the RBS of the H10LS-K158aA-D193T mutant is presented. (D–F) Interactions between avian analog 3′-SLN and the H10 HA RBS. Hydrogen bonds are indicated between 3′-SLN and the RBS of H10LS-K158aA-D193T mutant (D) and H10 wt (E). (F) Superposition of the 3′-SLN analog from the H10 wt HA complex (cyan) onto that of the H10LS-K158aA-D193T mutant (white) indicates displacement of the avian analog in the RBS and isomerization of the Sia-Gal bond (from trans to cis in the mutant complex) as a consequence of the Q226L and G228S mutations. See also Figure S2.
6′-SLNLN binds in a cis conformation and Gal-2 and GlcNAc-3 extend toward the 190 helix and upper part of the RBS akin to human analogs with pandemic influenza HAs (Figure S2D). As a consequence of the Q226L mutation, hydrophobic interaction between Leu226 and Gal-2 C6 stabilizes binding of the human analog. In addition, two hydrogen bonds are formed between Gal-2 to Gly225 and Arg137 (Figure 2A). Superposition of the H10LS-K158aA-D193T mutant with H10 wt reveals differences in the human analog conformation mainly arising from changes in the phi (from ~35 ° in wt to ~76 ° in the mutant) and psi (from ~173 ° to ~155 °) angles of the Sia-Gal bond (Figure 2C).
For H10LS-K158aA and H10LS-D193T, electron density was observed for three sugars of 6′-SLNLN (Figure S2B). The human analog conformation in H10LS-K158aA resembles that in H10LS-K158aA-D193T but, in H10LS-D193T, the electron density is weaker and the Sia-Gal phi angle differs slightly (from ~76 ° to ~67 °) indicating that this change only slightly reduces the steric clash between Lys158a and 6′-SLNLN (Figures S2E and S2F).
To evaluate the reduced binding of the H10 mutants to avian analogs, we determined the crystal structure of H10LS-K158aA-D193T with 3′-SLN (NeuAcα2–3Galβ1–4GlcNAc); electron density was observed for all three sugars (Figure S2B; Table S3). Sia-1 makes a hydrophobic interaction with Trp153 and hydrogen bonds with Tyr98, 130-loop and 190-helix, but not with the 220-loop, due to the Q226L and G228S mutations. In contrast to the trans conformation in the H10 wt complex, 3′-SLN binds in a cis conformation, where Gal-2 and GlcNAc-3 exit the RBS lower down and just above the 220-loop (Figures 2D–2F), thereby eliminating potential steric clashes between Leu226 and the Sia-Gal bond of 3′-SLN, resulting in loss of the hydrogen bond between Gal-2 and Arg137, and a new H-bond between Gal-2 and Gly225 main chain (Figure 2F).
The Role of the 150-loop in Host Specificity of Group-2 HAs
Since the 150-loop of the H10 clade has an insertion of two residues compared to H3 HA (Figure 1B), we further investigated its contribution to host specificity by shortening the extended 150-loop. Deletion of either K158a (H10ΔK158a), or K158a and G158b (H10ΔK158a-ΔG158b), resulted in similar binding to avian analogs as for wt H10 HA (Figure S3A), whereas these deletions on H10LS and H10LS-D193T resulted in gain of binding to human analogs with minimal binding to avian analogs (Figures 3A and S3A3). Thus, K158a deletion is similar to K158aA mutation on the same background (Figure 1C).
Figure 3. The Role of the 150-loop in Receptor Specificity of H10, H7 and H3 HAs.
Glycan microarray analysis was used to determine the role of the 150-loop in the binding specificity of group-2 HAs. (A) Deletion of K158a on the background of H10LS and H10LS-D193T mutants results in binding to α2–6 linked sialosides with only weak binding to α2–3 linked sialosides. (B) Sh2H7 HA binds to avian receptor analogs. Mutation of Asp158a to Ala on the background of the G228S mutation results in gain of binding to human receptors analogs, but no loss in binding to avian analogs. (C) Schematic representation of insertion of Ser and Lys (between positions 157 and 158) into the 150-loop of pandemic HK68 and A/Wyoming/3/2003 H3 HAs. (D) The insertion reveals no change in binding specificity compared to wt. See also Figure S3.
Human-isolated H7N9 HAs also contain an extended 150-loop, but with Asp at position 158a (Figure 1A) that can also result in potential steric clashes with human analogs (Russell et al., 2006). Modeling the binding of LSTc (PDB 2WR7) into the Sh2 H7N9 HA (PDB 4N5J) (Xu et al., 2013) shows that H7 Asp158a covers the upper part of the RBS, similar to H10 K158a (Figure S3B). Sh2H7 HA already contains Leu at position 226, but mutation of Gly226 to Ser still maintains avian specificity (Schrauwen et al., 2016; de Vries et al., submitted). To examine the 150-loop in H7, we mutated Asp158a to Ala on the background of G228S, which resulted in gain of binding to human receptor analogs, although binding to avian analogs was maintained (Figure 3B).
The H3 HAs are the only group-2 HAs that do not contain an insertion in the 150-loop (Figure 1A). We therefore extended the 150-loop of pandemic A/Hong Kong/1/1968 (HK68 H3) and A/Wyoming/3/2003 H3 HAs by insertion of two amino acids (Ser and Lys) at position 158 (Figure 3C) to maximize the sequence similarity to H10. The mutated H3 HAs retained human specificity with no significant changes in their binding profiles (Figure 3D). However, the crystal structure of HK68 H3 HA with the 150-loop insertion revealed a different conformation compared to H10 HA (Figure S3C; Table S4), where the 150-loop extends away from the binding site and, thus, does not influence human receptor binding.
Binding of H10 Mutants to Human Trachea Tissue
To further examine the role of the 150-loop, we assessed the ability of the H10 mutants to bind to epithelial cells on human trachea tissue sections. The upper regions of the human respiratory tract is rich in α2–6 linked sialic acids (Figure S4A), whereas the lower respiratory tract expresses a mixture of α2–6 and α2–3 linked sialic acids (Shinya et al., 2006). The lack of α2–3 ‘avian-type’ receptors in the human upper respiratory tract is believed to contribute to the inability of avian IAV to transmit in the human population (de Graaf and Fouchier, 2014; Imai and Kawaoka, 2012). Compared to weak binding of VN1203 H5 HA and strong binding of human A/Cal/04 H1 HA to human trachea epithelium (Figure 4A), the H10 HA displays some binding to human trachea (Figures 4B1 and 4C1), as previously reported (Wang et al., 2015). This latter result contrasts with lack of binding to human receptors on glycan arrays or in ELISA, and may reflect binding to mucin-type glycoproteins or glycans not present on the glycan microarray. The H10K158aA mutant has reduced binding to human trachea (Figure 4B2) that coincides with more restricted binding on the glycan array (Figure 1C2). Addition of the LS mutations (H10LS-K158aA) showed increased binding equivalent to H10wt (Figure 4B3). Further introduction of D193T (H10LS-K158aA-D193T) strongly increased binding to human trachea epithelium (Figure 4B4). In contrast to its binding to human trachea, the H10LS-K158aA-D193T mutant exhibited markedly reduced binding to chicken trachea epithelium relative to H10 wt HA (Figure S4 D1 vs D2), although staining with higher concentrations of HA exhibited clear binding to chicken trachea epithelium (Figure S4E2), consistent with weak binding in glycan arrays and strong binding in the glycan ELISA (Figure 1D). To establish that binding to human trachea is sialic acid dependent, binding of H10wt and H10LS-K158aA-D193T was assessed after treatment with sialidase (Figures 4C3 and 4C4), which abolished binding to epithelial cells. Together, the results show that the combined 190-helix and 150-loop mutations increase binding to human-type receptors in glycan array and ELISA-type assays as well as direct binding to human trachea tissues.
Figure 4. Binding of H10 Mutants to Human Trachea Tissue.
Binding of recombinant H10 HAs to sections of human trachea tissue. The VN1203 H5N1 (A1) and A/Cal/04 H1N1 (A2) HAs were used as controls for avian and human HAs. Whereas the H10K158aA mutant (B2) shows no binding to human trachea tissue and the H10 wt (B1 and C1) and the H10LS-K158aA (B3) mutants show weak binding, the H10LS-K158aA-D193T mutant (B4 and C2) exhibits increased binding to human trachea tissue. HA binding of H10 wt and the H10LS-K158aA-D193T mutant to tissue sections was destroyed by treatment of the tissue with sialidase (C3 and C4). Each panel (A, B and C) represents results from an independent experiment. See also Figure S4.
DISCUSSION
Although more than a hundred different subtypes of IAV have been isolated from birds, only three, H1N1, H2N2 and H3N2, have been able to cross the species barrier and transmit in the human population. Crossing the species barrier and becoming a successful pathogen in a new host is a rare event that requires several adaptation steps, including acquisition of specific binding to the new host cells (Parrish and Kawaoka, 2005). Defining and understanding these steps can allow us to anticipate and control emerging viruses in early stages of adaptation to a new host to prevent a major pandemic.
Two of the three new influenza subtypes isolated during 2013 are members of the H7, H10 and H15 subgroup (Figure S1B) that have a two-residue insert in the 150-loop. The extension of the 150 loop contains large, polar amino acids that can sterically clash with human receptors. Here, based on structural and receptor binding studies, we identified mutations in the RBS that enable a switch in receptor specificity for H10 HA (Figures 1 and 3). Similarly, mutating H7 Asp158a to Ala along with G228S enhanced binding of H7N9 HA to human receptors, but with no loss of binding to avian receptors. In contrast, extending the 150 loops of human H3 HAs by two residues (Figure 3) did not block binding to human receptors indicating that the role and conformation of the extended 150-loop in human receptor specificity is characteristic only of the H10, H7 and H15 subgroups.
Previous structural analysis has shown that the base of the human RBS appears to be wider (i.e. distance between 220- and 130-loops) compared to avian HAs (Ha et al., 2001). Comparison of the apo structures of the H10 wt and mutants (i.e. with no receptor analogs bound) reveals no significant difference in this distance, but the upper part of the RBS becomes more accessible for binding of human receptors in the K158aA and D193T mutants (Figure S2A). Crystal structures of a human analog with the H10 mutants illustrates that its conformation is similar to its minimum energy conformation in solution and similar to that in pandemic HAs (Figure S2D). The 220-loop mutations create more favorable binding interactions with the hydrophobic face of the human receptor and mutation of Lys158a eliminates steric clashes of the 150-loop (Figure 2). A similar phenotype for change in conformation of the human receptor analog was reported for the switch in receptor specificity of the airborne transmissible H5N1 HA (Xiong et al., 2013a; Zhang et al., 2013) and also for A/Taiwan/2/2013 H6N1 HA (Tzarum et al., 2013; de Vries et al., submitted).
In contrast, avian receptors extend toward the 220-loop out of the binding pocket. Thus, the 150-loop extension of H10 HAs probably has no influence on avian receptor binding (Figure 1). In the H10 mutants, loss of binding to avian receptors arises from the 220-loop mutations (Figure 1C). Comparison of the structures of H10 wt and the H10LS-K158aA-D193T mutant with avian analogs indicates a change in the Sia-Gal bond rotation that creates a favorable interactions with Leu226 and eliminates steric clashes with the polar oxygen of the Sia-Gal bond, as in ferret-transmissible H5 HA (Xiong et al., 2013a; Zhang et al., 2013) and human H7N9 HA with Leu226 (Shi et al., 2013; Xiong et al., 2013b; Xu et al., 2013) (Figure S2).
The acquisition of human-type receptor specificity by the H10LS-K158aA-D193T mutant is seen in all assays utilized including the glycan array, ELISA, and tissue binding. As we have noted previously, the glycan array assay is more stringent that the ELISA (Chen et al., 2012; Paulson and de Vries, 2013). In the glycan array, the mutant HA shows strong preferential binding to α2–6 linked sialosides. In contrast, in ELISA, although a significant increase is observed in binding to α2–6 linked glycans, binding to α2–3 linked glycans was reduced only in two-fold relative to wt HA (for long glycans, Table S2). Such differences were also observed using these assays for the ferret-transmissible H5 HAs (Xiong et al., 2013a; Zhang et al., 2013). The qualitative differences in the two assays likely arise from the different coupling chemistries and glycan presentation on glass slides or streptavidin-coated surfaces.
Evaluation of the binding of wt and mutant H10 HAs to sections of human and chicken trachea tissues provides biological validation for the increased binding to human-type receptors. Relative to wt HA, the mutant binds with increased avidity to human trachea (Figure 4), and significantly weaker binding to chicken trachea (Figure S4). The next logical step is to analyze the impact of these mutations on transmission in the ferret model of human influenza, which supports respiratory droplet transmission of influenza viruses with human but not avian-type receptor specificity (Belser et al., 2011; Herfst et al., 2012; Imai et al., 2012). However, such gain-of-function studies with avian viruses fall under the current moratorium for dual use research of concern and are not permitted. Notwithstanding, we show here that the extended 150-loop of H10 and also H7 HAs is a key element in human receptor binding specificity and should be taken into consideration for design of influenza vaccines and therapies.
EXPERIMENTAL PROCEDURES
Expression and Purification of HAs for Glycan Microarray Analyses
Codon-optimized H3, H5, H7 and H10 were cloned into a pFastBac vector and HAs expressed as described (Stevens et al., 2006a). HA0 was purified via His-tag affinity chromatography and then by gel filtration chromatography.
Expression and Purification of H10 HAs for Crystallization
The HA0s were expressed as above and purified via His-tag affinity chromatography, cleaved with trypsin to produce uniformly cleaved (HA1/HA2) and removal of the trimerization domain and His6-tag, and then purified further by gel filtration chromatography. The HA eluted as a trimer and was concentrated to 5 mg/ml.
Crystallization and Structural Determination of H10 HAs
Crystals of H10 HA mutants were obtained using sitting drop vapor diffusion at 4 °C. HA complexes with receptor analogues were obtained by soaking HA crystals with reservoir solution that contained glycan ligands at 5 mM. Diffraction data were collected at the Advanced Photon Source (APS) and Stanford Synchrotron Radiation Lightsource (SSRL) (Table S3).
Glycan Microarray Analysis of HAs
Purified HA was pre-complexed with (HRP)-linked anti-His-tag antibody and with Alexa488-linked anti-mouse IgG and then incubated on the array surface in a humidified chamber. Slides were subsequently washed, dried, and immediately scanned for an FITC signal. Fluorescent signal intensity was measured using Imagene and mean intensity minus mean background was calculated.
Tissue Staining
Tissue sections of formalin-fixed, paraffin-embedded human trachea were rehydrated through a gradient from ethanol to distilled water, boiled in citrate buffer pH 6.0, and washed in PBS with 0.1% Tween. Tissue sections were then incubated overnight with 3% BSA in PBS. On the next day, purified HA was mixed with mouse anti-strep-tag and goat anti-mouse IgG HRP antibodies and incubated in ice for 20 minutes. The precomplexed HA was applied onto tissues and incubated for 90 minutes at RT. Sections were then washed, incubated with 3-amino-9-ethyl-carbazole, counterstained with hematoxylin, mounted with Aquatex and then imaged.
Supplementary Material
Acknowledgments
This work was funded in part by NIH Grants R56 AI117675 (to I.A.W) and AI114730 (to J.C.P). RPdV is a recipient of VENI and Rubicon grants from the Netherlands Organization for Scientific Research (NWO). M.H.V is a recipient of a MEERVOUD grant from the NWO. We thank R. Stanfield, X. Dai, and M. Elsliger for crystallographic and computational support, H. Tien of the Robotics Core at the Joint Center for Structural Genomics for automated crystal screening (supported by NIH Grant U54 GM094586), and staff at the APS beamline 23ID-B (GM/CA CAT) and SSRL beamlines 12-2. GM/CA CAT is funded in whole or in part with federal funds from NIH NCI (Y1-CO-1020) and NIGMS (Y1-GM-1104). The APS was supported by the U.S. Department of Energy (DOE), Basic Energy Sciences, Office of Science, under contract DE-AC02–06CH11357. SSRL is a Directorate of Stanford Linear Accelerator Center National Accelerator Laboratory and an Office of Science User Facility operated for the U.S. DOE Office of Science by Stanford University. The SSRL Structural Molecular Biology Program is supported by DOE Office of Biological and Environmental Research and by the NIH NIGMS (including P41GM103393) and the National Center for Research Resources (P41RR001209). This is manuscript 29334 from The Scripps Research Institute.
Footnotes
AUTHOR CONTRIBUTIONS
Project design by N.T., R.P.dV, J.C.P. and I.A.W.; HA expression, x-ray structure determination and analysis by N.T., X.Z., and W.Y.; glycan array studies by N.T., and R.M.; tissue staining studies by R.P.dV., K.B. and M.H.V.; glycan ELISA by A.J.T. and N.T.; manuscript written by N.T., J.C.P. and I.A.W.
ACCESSION NUMBERS
Atomic coordinates and structure factors have been deposited in the Protein Data Bank (PDB) under accession codes 5TGO for H10LS-K158aA-D193T mutant HA in apo form and 5TGU and 5TGV with 6′-SLNLN and 3′-SLN respectively, 5TH0 for H10LS-K158aA mutant HA in apo form and 5TH1 with 6′-SLNLN, 5THB for H10LS-D193T mutant HA in apo form and 5THC with 6′-SLNLN and 5THF for the H3 HK68 Insert KS structure.
Supplemental Information includes four figures and four tables and can be found within this article online at http://dx.doi........
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Air GM. Sequence relationships among the hemagglutinin genes of 12 subtypes of influenza A virus. Proc Natl Acad Sci USA. 1981;78:7639–7643. doi: 10.1073/pnas.78.12.7639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman AC, Karamanska R, Busch MG, Dell A, Olsen CW, Haslam SM. Glycan analysis and influenza A virus infection of primary swine respiratory epithelial cells: the importance of NeuAcα2–6 glycans. J Biol Chem. 2010;285:34016–34026. doi: 10.1074/jbc.M110.115998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Katz JM, Tumpey TM. The ferret as a model organism to study influenza A virus infection. Dis Model Mech. 2011;4:575–579. doi: 10.1242/dmm.007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekaran A, Srinivasan A, Raman R, Viswanathan K, Raguram S, Tumpey TM, Sasisekharan V, Sasisekharan R. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nat Biotechnol. 2008;26:107–113. doi: 10.1038/nbt1375. [DOI] [PubMed] [Google Scholar]
- Chen H, Yuan H, Gao R, Zhang J, Wang D, Xiong Y, Fan G, Yang F, Li X, Zhou J, et al. Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: a descriptive study. Lancet. 2014;383:714–721. doi: 10.1016/S0140-6736(14)60111-2. [DOI] [PubMed] [Google Scholar]
- Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology. 2012;422:105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Graaf M, Fouchier RA. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J. 2014;33:823–841. doi: 10.1002/embj.201387442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries RP, de Vries E, Moore KS, Rigter A, Rottier PJ, de Haan CA. Only two residues are responsible for the dramatic difference in receptor binding between swine and new pandemic H1 hemagglutinin. J Biol Chem. 2011;286:5868–5875. doi: 10.1074/jbc.M110.193557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries RP, Zhu X, McBride R, Rigter A, Hanson A, Zhong G, Hatta M, Xu R, Yu W, Kawaoka Y, et al. Hemagglutinin receptor specificity and structural analyses of respiratory droplet-transmissible H5N1 viruses. J Virol. 2014;88:768–773. doi: 10.1128/JVI.02690-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen MB, Sabesan S, Skehel JJ, Wiley DC. Binding of the influenza A virus to cell-surface receptors: structures of five hemagglutinin-sialyloligosaccharide complexes determined by X-ray crystallography. Virology. 1997;232:19–31. doi: 10.1006/viro.1997.8526. [DOI] [PubMed] [Google Scholar]
- Elli S, Macchi E, Rudd TR, Raman R, Sassaki G, Viswanathan K, Yates EA, Shriver Z, Naggi A, Torri G, et al. Insights into the human glycan receptor conformation of 1918 pandemic hemagglutinin-glycan complexes derived from nuclear magnetic resonance and molecular dynamics studies. Biochemistry. 2014;53:4122–4135. doi: 10.1021/bi500338r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouchier RA, Munster V, Wallensten A, Bestebroer TM, Herfst S, Smith D, Rimmelzwaan GF, Olsen B, Osterhaus AD. Characterization of a novel influenza A virus hemagglutinin subtype (H16) obtained from black-headed gulls. J Virol. 2005;79:2814–2822. doi: 10.1128/JVI.79.5.2814-2822.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freidl GS, Meijer A, de Bruin E, de Nardi M, Munoz O, Capua I, Breed AC, Harris K, Hill A, Kosmider R, et al. Influenza at the animal-human interface: a review of the literature for virological evidence of human infection with swine or avian influenza viruses other than A(H5N1) Euro Surveill. 2014;19(18) doi: 10.2807/1560-7917.es2014.19.18.20793. [DOI] [PubMed] [Google Scholar]
- Gamblin SJ, Skehel JJ. Influenza hemagglutinin and neuraminidase membrane glycoproteins. J Biol Chem. 2010;285:28403–28409. doi: 10.1074/jbc.R110.129809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Sastre A, Schmolke M. Avian influenza A H10N8 - a virus on the verge? Lancet. 2014;383:676–677. doi: 10.1016/S0140-6736(14)60163-X. [DOI] [PubMed] [Google Scholar]
- Ha Y, Stevens DJ, Skehel JJ, Wiley DC. X-ray structures of H5 avian and H9 swine influenza virus hemagglutinins bound to avian and human receptor analogs. Proc Natl Acad Sci USA. 2001;98:11181–11186. doi: 10.1073/pnas.201401198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Kawaoka Y. The role of receptor binding specificity in interspecies transmission of influenza viruses. Curr Opin Virol. 2012;2:160–167. doi: 10.1016/j.coviro.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia N, Barclay WS, Roberts K, Yen HL, Chan RW, Lam AK, Air G, Peiris JS, Dell A, Nicholls JM, et al. Glycomic characterization of respiratory tract tissues of ferrets: implications for its use in influenza virus infection studies. J Biol Chem. 2014;289:28489–28504. doi: 10.1074/jbc.M114.588541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YP, Xiong X, Wharton SA, Martin SR, Coombs PJ, Vachieri SG, Christodoulou E, Walker PA, Liu J, Skehel JJ, et al. Evolution of the receptor binding properties of the influenza A(H3N2) hemagglutinin. Proc Natl Acad Sci USA. 2012;109:21474–21479. doi: 10.1073/pnas.1218841110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matrosovich M, Stech J, Klenk HD. Influenza receptors, polymerase and host range. Rev Sci Tech. 2009;28:203–217. doi: 10.20506/rst.28.1.1870. [DOI] [PubMed] [Google Scholar]
- Medeiros R, Escriou N, Naffakh N, Manuguerra JC, van der Werf S. Hemagglutinin residues of recent human A(H3N2) influenza viruses that contribute to the inability to agglutinate chicken erythrocytes. Virology. 2001;289:74–85. doi: 10.1006/viro.2001.1121. [DOI] [PubMed] [Google Scholar]
- Nobusawa E, Aoyama T, Kato H, Suzuki Y, Tateno Y, Nakajima K. Comparison of complete amino acid sequences and receptor-binding properties among 13 serotypes of hemagglutinins of influenza A viruses. Virology. 1991;182:475–485. doi: 10.1016/0042-6822(91)90588-3. [DOI] [PubMed] [Google Scholar]
- Nobusawa E, Ishihara H, Morishita T, Sato K, Nakajima K. Change in receptor-binding specificity of recent human influenza A viruses (H3N2): a single amino acid change in hemagglutinin altered its recognition of sialyloligosaccharides. Virology. 2000;278:587–596. doi: 10.1006/viro.2000.0679. [DOI] [PubMed] [Google Scholar]
- Nycholat CM, Peng W, McBride R, Antonopoulos A, de Vries RP, Polonskaya Z, Finn MG, Dell A, Haslam SM, Paulson JC. Synthesis of biologically active N- and O-linked glycans with multisialylated poly-N-acetyllactosamine extensions using P. damsela α2–6 sialyltransferase. J Am Chem Soc. 2013;135:18280–18283. doi: 10.1021/ja409781c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterhaus AD, Rimmelzwaan GF, Martina BE, Bestebroer TM, Fouchier RA. Influenza B virus in seals. Science. 2000;288:1051–1053. doi: 10.1126/science.288.5468.1051. [DOI] [PubMed] [Google Scholar]
- Parrish CR, Kawaoka Y. The origins of new pandemic viruses: the acquisition of new host ranges by canine parvovirus and influenza A viruses. Annu Rev Microbiol. 2005;59:553–586. doi: 10.1146/annurev.micro.59.030804.121059. [DOI] [PubMed] [Google Scholar]
- Parry J. H10N8 avian flu virus claims its first known human casualty. BMJ. 2014;348:g1360. doi: 10.1136/bmj.g1360. [DOI] [PubMed] [Google Scholar]
- Paulson JC, de Vries RP. H5N1 receptor specificity as a factor in pandemic risk. Virus Res. 2013;178:99–113. doi: 10.1016/j.virusres.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W, Pranskevich J, Nycholat C, Gilbert M, Wakarchuk W, Paulson JC, Razi N. Helicobacter pylori β1,3-N-acetylglucosaminyltransferase for versatile synthesis of type 1 and type 2 poly-LacNAcs on N-linked, O-linked and I-antigen glycans. Glycobiology. 2012;22:1453–1464. doi: 10.1093/glycob/cws101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W, de Vries RP, Grant OC, Thompson AJ, McBride R, Tsogtbaatar B, Lee PS, Razi N, Wilson IA, Woods RJ, Paulson JC. Recent H3N2 and 2009 pandemic H1N1 viruses share specificity for extended branched human-type receptors. Cell Host Microbe. 2016;21:1–12. doi: 10.1016/j.chom.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell RJ, Stevens DJ, Haire LF, Gamblin SJ, Skehel JJ. Avian and human receptor binding by hemagglutinins of influenza A viruses. Glycoconjugate J. 2006;23:85–92. doi: 10.1007/s10719-006-5440-1. [DOI] [PubMed] [Google Scholar]
- Sabesan S, Bock K, Paulson JC. Conformational analysis of sialyloligosaccharides. Carbohydr Res. 1991;218:27–54. doi: 10.1016/0008-6215(91)84084-r. [DOI] [PubMed] [Google Scholar]
- Schrauwen EJA, Richard M, Burke DF, Rimmelzwaan GF, Herfst S, Fouchier RAM. Amino acid substitutions that affect receptor binding and stability of the hemagglutinin of influenza A/H7N9 virus. J Virol. 2016;90:3794–3799. doi: 10.1128/JVI.03052-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, Zhang W, Wang F, Qi J, Wu Y, Song H, Gao F, Bi Y, Zhang Y, Fan Z, et al. Structures and receptor binding of hemagglutinins from human-infecting H7N9 influenza viruses. Science. 2013;342:243–247. doi: 10.1126/science.1242917. [DOI] [PubMed] [Google Scholar]
- Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem. 2000;69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- Stevens J, Blixt O, Paulson JC, Wilson IA. Glycan microarray technologies: tools to survey host specificity of influenza viruses. Nat Rev Microbiol. 2006a;4:857–864. doi: 10.1038/nrmicro1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science. 2006b;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- Walther T, Karamanska R, Chan RW, Chan MC, Jia N, Air G, Hopton C, Wong MP, Dell A, Malik Peiris JS, et al. Glycomic analysis of human respiratory tract tissues and correlation with influenza virus infection. PLoS Pathog. 2013;9:e1003223. doi: 10.1371/journal.ppat.1003223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzarum N, de Vries RP, Zhu X, Yu W, McBride R, Paulson JC, Wilson IA. Structure and receptor binding of the hemagglutinin from a human H6N1 influenza virus. Cell Host Microbe. 2015;17:369–376. doi: 10.1016/j.chom.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Zhang W, Qi J, Wang F, Zhou J, Bi Y, Wu Y, Sun H, Liu J, Huang C, et al. Structural basis for preferential avian receptor binding by the human-infecting H10N8 avian influenza virus. Nat Commun. 2015;6:5600. doi: 10.1038/ncomms6600. [DOI] [PubMed] [Google Scholar]
- Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. Evolution and ecology of influenza A viruses. Microbiol Rev. 1992;56:152–179. doi: 10.1128/mr.56.1.152-179.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Wu Y, Tefsen B, Shi Y, Gao GF. Bat-derived influenza-like viruses H17N10 and H18N11. Trends Microbiol. 2014;22:183–191. doi: 10.1016/j.tim.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong X, Coombs PJ, Martin SR, Liu J, Xiao H, McCauley JW, Locher K, Walker PA, Collins PJ, Kawaoka Y, et al. Receptor binding by a ferret-transmissible H5 avian influenza virus. Nature. 2013a;497:392–396. doi: 10.1038/nature12144. [DOI] [PubMed] [Google Scholar]
- Xiong X, Martin SR, Haire LF, Wharton SA, Daniels RS, Bennett MS, McCauley JW, Collins PJ, Walker PA, Skehel JJ, et al. Receptor binding by an H7N9 influenza virus from humans. Nature. 2013b;499:496–499. doi: 10.1038/nature12372. [DOI] [PubMed] [Google Scholar]
- Xu R, de Vries RP, Zhu X, Nycholat CM, McBride R, Yu W, Paulson JC, Wilson IA. Preferential recognition of avian-like receptors in human influenza A H7N9 viruses. Science. 2013;342:1230–1235. doi: 10.1126/science.1243761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Carney PJ, Chang JC, Guo Z, Villanueva JM, Stevens J. Structure and receptor binding preferences of recombinant human A(H3N2) virus hemagglutinins. Virology. 2015;477:18–31. doi: 10.1016/j.virol.2014.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, de Vries RP, Tzarum N, Zhu X, Yu W, McBride R, Paulson JC, Wilson IA. A human-infecting H10N8 influenza virus retains a strong preference for avian-type receptors. Cell Host Microbe. 2015;17:377–384. doi: 10.1016/j.chom.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Shi Y, Lu X, Shu Y, Qi J, Gao GF. An airborne transmissible avian influenza H5 hemagglutinin seen at the atomic level. Science. 2013;340:1463–1467. doi: 10.1126/science.1236787. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.






