Abstract
Background:
Candida albicans is one of the microorganisms which harbor the oral cavity, especially in elderly. However, the incidence of existence of this increases in patients using removable dental prosthesis. There is therefore a need to test the anticandidal efficacy of these cost-effective, easily available products to be used as routine denture cleansers.
Aim and Objectives:
(1) To evaluate antifungal properties of triphala churna on the heat cure denture base material. (2) To evaluate the antifungal effect of chlorhexidine gluconate on the heat cure denture base material. (3) To compare the antifungal effect of triphala churna and chlorhexidine gluconate with a control. (4) To evaluate which among triphala churna and chlorhexidine gluconate has a better antifungal property on the heat cure denture base material.
Materials and Methods:
Study population consisted of sixty dentures wearers from those attending the Outpatient Department of Prosthodontics of the School of Dentistry, Krishna Institute of Medical Sciences Deemed University, Karad. Swabs were collected from the dentures before and after the use of triphala and chlorhexidine. The swabs were cultured on Sabouraud dextrose agar and the total Candida counts were determined.
Conclusion:
Triphala as an antifungal is shown to have more efficacy than the conventional chlorhexidine mouthwash.
Keywords: Candida, chlorhexidine, triphala churna, Candida, chlorexidine, triphala churna
Résumé
Arrière-plan:
Candida albicans est l’un des micro-organismes qui abritent la cavité buccale surtout chez les personnes âgées. Cependant, l’incidence de l’existence de cette augmentation chez les patients utilisant des prothèses dentaires amovibles. Il est donc nécessaire de tester l’efficacité anticancédique de ces produits rentables et faciles à utiliser pour être utilisés comme nettoyants de routine pour prothèses dentaires.
Buts et Objectifs:
(1) Évaluer les propriétés antifongiques de Triphala churna sur le matériau de base de la prothèse thermo-durcissable. (2) Évaluer l’effet antifongique du gluconate de chlorhexidine sur le matériau de base de la prothèse thermo-durcissable. (3) Comparer l’effet antifongique de Triphala churna et du gluconate de chlorhexidine avec un témoin. (4) Évaluer lequel parmi Triphala churna et le gluconate de chlorhexidine a une meilleure propriété antifongique sur le matériel de base de la prothèse de durcissement à chaud.
Matériaux et Méthode:
La population de l’étude était constituée de soixante porteurs de prothèses dentaires de ceux qui fréquentaient le Département de Prosthodontie de l’École des Sciences Dentaires de l’Institut Krishna des Sciences Médicales de l’Université de Karad. Des prélèvements ont été effectués sur les prothèses avant et après l’utilisation de Triphala et de chlorhexidine. On a cultivé les écouvillons sur de l’agar Sabouraud dextrose et on a déterminé le nombre total de candida.
Conclusion:
Triphala comme un anti fongique est démontré pour avoir plus d’efficacité que le lavage de la bouche classique chlorhexidine.
Introduction
In India, the size of the elderly population age about 60 years and above is on the rise. This poses various problems such as socioeconomic front, health-care expenditures, and medical and psychological.[1] With this, India is becoming an aging society. However, about 75% of the elderly stay in rural areas.[2] Inadequate income is a major problem of elderly in India; another distressing fact is that elderly people are dependent on others for their living.[1] As the size of the dependent elderly population is fast growing, there is an emerging need to pay greater attention to aging-related oral health issues.
Among the elderly in the age group between 65 and 74 years, about 10.2% of the population had prosthesis in the upper arch and 11.1% of them had prosthesis on the lower arch and the use of complete denture was prevalent.[3] Candida-associated denture stomatitis is a common inflammatory process affecting around 60%–65% of denture wearers and is usually found on the palatal mucosa beneath the fitting surface of the upper denture. It has multifactorial etiology, but poor denture hygiene habit is one of the most prominent contributing factors.[4] Denture cleansing is an important aspect of denture maintenance for the maintenance of oral health. There are various commercial products available in the market. However, the rural and dependent elderly have minimum access to these. Hence, there is a need to for an alternative antimicrobial which is readily available in the rural setup.
Triphala is a tridoshic herbal formulation consisting of fruits of Terminalia bellirica (TB), Terminalia chebula (TC), and Emblica officinalis (EO) in a 1:1:1 ratio known for their medicinal properties being traditionally used in India as therapeutic and antimicrobial aids in various ailments and being potent antifungal products effective against Candida.[5]
Chlorhexidine is a gold standard against which other antimicrobials are tested. It is a cationic chlorophenyl bisbiguanide that binds to negatively charged surfaces. It has a broad spectrum of antimicrobial activity including Candida albicans. It is a biocide used extensively as a topical antiseptic in hospitals and for the treatment of periodontal diseases. Chlorhexidine has a broad spectrum of activity against a variety of organisms, including C. albicans. Susceptibility of C. albicans biofilms to chlorhexidine was shown to be significantly reduced compared to its action against suspended organisms.[6]
Hence, the objective of this study was to compare the anticandidal efficacy of triphala churna and 0.2% chlorhexidine on randomly selected complete denture wearers.
Materials and Methods
This study was conducted on a random sample of sixty dentures wearers who were selected among the patients visiting the Department of Prosthodontics of the School of Dentistry, Krishna Institute of Medical Sciences Deemed University, Karad, Maharashtra. Ethical clearance was obtained from the University's Ethical Committee. All patients were informed about the study procedure in their mother tongue and made aware of the experimental design. Their written informed consent was taken before they enrolled in the study.
Inclusion criteria
Volunteers consenting to participate in the study and those who have a complete heat polymerized acrylic dentures.
Exclusion criteria
Partially dentate patient who had existing fixed partial dentures
Patients with existing removable partial dentures
Patients seeking or with existing implant dental prosthesis
Patients seeking or with existing maxillofacial prosthesis
Patients who have used a denture cleanser at least 2 weeks before enrolment in the study
Patients already on antifungal agents or antiseptic mouthwashes
Patients with denture stomatitis.
The total sample size was divided into two groups using a simple randomization method:
Group I: Thirty patients who were asked clean the denture using cotton soaked in chlorhexidine (0.2%) (Hexidine, ICPA Health Products Ltd., Gujarat, India). Mouthwash by rubbing the material over all the surfaces of the denture and then dip in water
Group II: Thirty patients who were asked to clean the denture by scrubbing the triphala churna (triphala churna, Dabur India Ltd, New Delhi, India) using fingers gently over the intaglio and outer surface of the dentures and then dipping the denture in water.
A baseline swab was taken at the first visit from the dentures of patients in both experimental groups and subjected to microbial analysis to establish a baseline for the number of Candida colonies as outlined below in the section on microbial analysis.
Patients in both groups were then instructed to clean their dentures, following the instructions given to them for 30 days and report back to the department on the 31st day for sample collection.
Microbial analysis of the dentures
Swab samples were taken from experimental Groups I and II. Swab samples were taken by rolling sterile cotton swabs across the tissue surface of the upper and lower dentures [Figure 1]. The swabs were placed in a test tube which was covered with a cotton plug [Figure 2]. Then, using a 4-mm loop, the swab sample was immediately smeared onto the surface of culture plate with Sabouraud dextrose agar (SDA) (with 10% chloramphenicol). All plates were aerobically incubated at 37°C for 72 h. Culture plates which were negative for candidal growth were left on the bench for further 72 h and then examined again before being discarded as negative.
Figure 1.
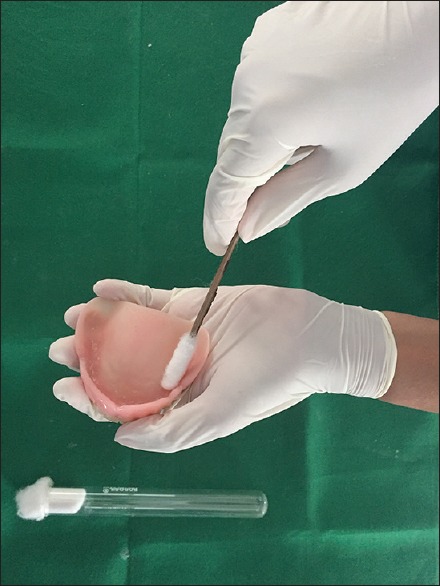
Materials for sample collection - Test tube and swab stick
Figure 2.
Sample collection from intaglio surface of dentures
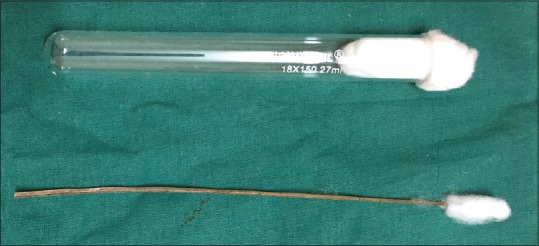
The colonies were identified as follows:
-
Colony morphology:
Number of colonies: Number of Candida colonies was determined by counting colony forming units on SDA plates. The difference in the number of colony forming units of microorganisms between first swab (baseline before use of cleanser) and second swab (after use of cleanser) was noted to assess the effectiveness of cleansers in reducing the total Candida count.
Figure 3.

(a and b) Candidal growth on Sabouraud dextrose agar plate (streaking method)
Figure 4.
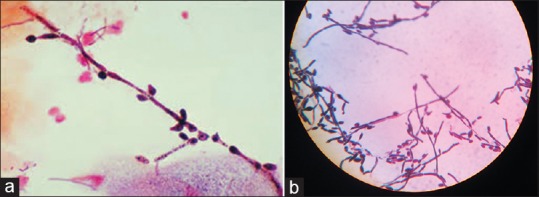
(a and b) Positive Gram staining showing budding of candidal species
Figure 5.

Germ tube test showing Candida albicans
Results
A total of sixty denture wearers participated in the study, of which 30 N belonged to Group I (22 N [73.33%] males and 8 [26.67%] N females) were instructed to use chlorhexidine and the remaining thirty belonged to Group II (21 [70%] males and 9 [30%] females) were instructed to use triphala churna [Figures 6 and 7 and Table 1].
Figure 6.
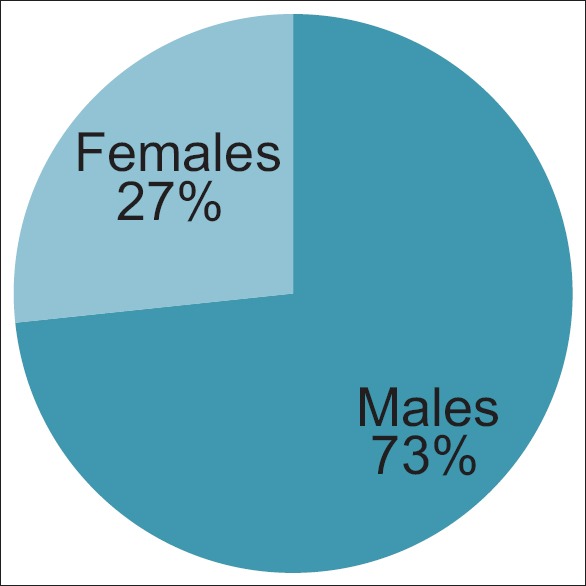
Sex-wise distribution of patients using chlorhexidine gluconate
Figure 7.
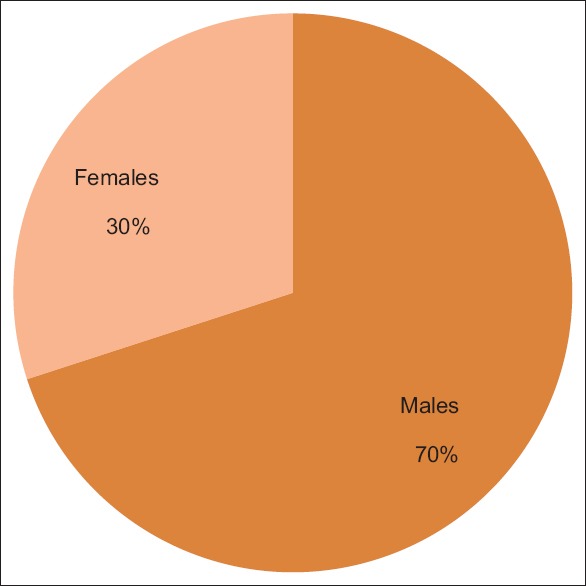
Sex-wise distribution of patients using triphala churna
Table 1.
Gender distribution details of the study participants
| Sex | Chlorhexidine gluconate (Group I) number(%) | Triphala churna (Group II) number(%) |
|---|---|---|
| Males | 22 (73.33) | 21 (70) |
| Females | 08 (26.67) | 09 (30) |
| Total | 30 | 30 |
Table 2 and Figure 8 show the age distribution of the study participants. The study participants were divided into five groups; ≥55, 56–60, 61–65, 66–70, ≥71. According to Kuppuswamy scale of socioeconomic status of the study participants, Table 3 shows that there were 21 (70%) patients in upper lower class in Group I and 23 (76.7%) patients belonged to the same from Group II. About 6 (20%) and 5 (16.7%) patients were in lower middle class for Groups I and II, respectively. Only 3 (10%) and 2 (6.7%) were in upper middle class for Groups I and II, respectively [Figure 9].
Table 2.
Age distribution of the study participants
| Age group (in years) | No | % |
|---|---|---|
| ≤55 | 4 | 6.7 |
| 56-60 | 13 | 21.7 |
| 61-65 | 20 | 33.3 |
| 66-70 | 15 | 25.0 |
| ≥71 | 8 | 13.3 |
| Total | 60 | 100 |
Figure 8.

Age-wise distribution of patients using chlorhexidine gluconate and triphala churna
Table 3.
Socio economic status of the study participants
| Socio economic class | Chlorhexidine gluconate (Group I) No. (%) | Triphala churna (Group II) No. (%) |
|---|---|---|
| Lower | 0 (0) | 0 (0) |
| Upper Lower | 21 (70) | 23 (76.7) |
| Lower Middle | 6 (20) | 5 (16.7) |
| Upper Middle | 3 (10) | 2 (6.7) |
| Upper | 0 (0) | 0 (0) |
Figure 9.
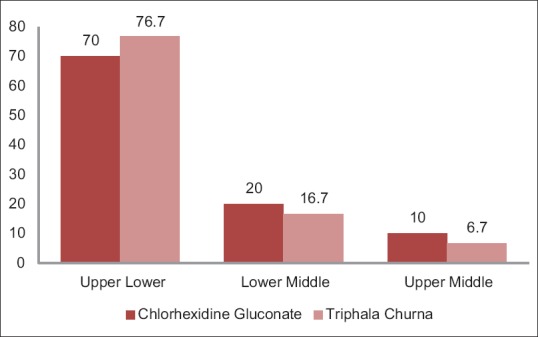
Socioeconomic class-wise distribution of patients using chlorhexidine gluconate and triphala churna
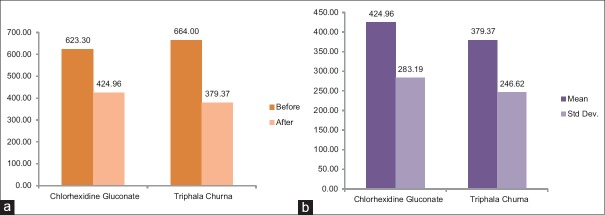
Table 4 shows the mean of Candida colony count of Group I before providing denture cleanser was 623.30 ± 315.45. After using medicine, it decreased to mean 424.96 ± 283.19. The paired t-test was used to test the significant difference between before and after using denture cleanser. It was found that there was significant decrease in Candida after having chlorhexidine gluconate (P = 0.00) [Figure 10].
Table 4.
Comparison of mean of candidal count before and after the use of both the denture cleansers
| Denture cleansers | Chlorhexidine gluconate (0.2%) | Triphala churna | Comparison | ||
|---|---|---|---|---|---|
| Before use | After use | Before use | After use | ||
| Mean | 623.30 | 424.96 | 664.00 | 379.37 | |
| Std. Dev. | 315.45 | 283.19 | 355.24 | 246.62 | |
| Confidence interval | 505.53-741.08 | 319.20-530.67 | 531.37-796.63 | 287.29-471.44 | |
| T statistic | 3.64 | 7.22 | 0.66 | ||
| P value | 0.00 | 0.00 | 0.50 | ||
Figure 10.

Candida colony count wise distribution of patients using chlorhexidine gluconate before and after treatment
The mean of Candida colony count of Group II before providing medicinal herb (triphala churna) was 664 ± 355.24. After using medicine, it decreased to mean 379.37 ± 246.62. The paired t-test was used to test the significant difference between before and after having medicinal herb (triphala churna). It was found that there was significant decrease in Candida after having triphala churna (P = 0.00) [Figure 11]. The unpaired t-test was done to find out the significant difference between the antifungal effect of chlorhexidine gluconate and triphala churna. It was found that there was no significant difference between the two medicines (P = 0.50), which means that the two medicinal herbs are equally efficient.
Figure 11.
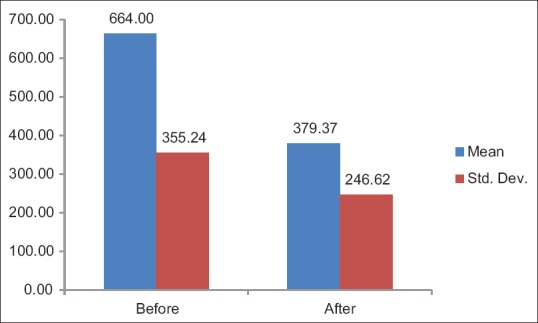
Candida colony count-wise distribution of patients using triphala churna before and after treatment
The mean Candida colony count in patients having triphala churna was slightly lower than patients using chlorhexidine gluconate [Figure 12a and b].
Figure 12.
(a and b) comparison of Candida colony count-wise distribution of patients using chlorhexidine gluconate and triphala churna before and after treatment
Discussion
Dental prosthesis is defined as an artificial replacement of one or more teeth and associated dental/alveolar structures.[7] The care and maintenance of the removable dental prosthesis are of utmost importance. If the proper home care protocol of the prosthesis is not followed on, serious health issues could result. There are various denture cleansers available in the market, of which chlorhexidine is marked as the gold standard.[6] Chemical cleansers may be defined as alkaline hypochlorites, alkaline peroxides, and dilute acids.[8] In various studies, many commercially available antimicrobials have been tested for its efficacy on Candida[9,10,11,12,13] and chlorhexidine is considered to be the “gold standard” antiplaque mouth rinses due to their prolonged broad-spectrum antimicrobial activity and plaque inhibitory potential.[6,10] However, chlorhexidine is known to produce brown discoloration of the teeth, restoration, and dorsum of tongue.[14,15]
Ayurveda is a medicinal science that has helped the humankind cure their ailments since time immemorial. The pharmacopoeias of many countries include a large number of drugs of plant origin. As the times are changing and like every aspect of life, even the health care system has also seen tremendous changes. However, Ayurveda is one such field which has stood the test of time. Even today, this particular field of medicine plays an important role in curing the oral diseases.[16,17,18,19] It has been reported in a number of in vitro studies that the herbals that are used to cure infectious diseases have wide antimicrobial spectrum.[20,21,22,23,24] However, in the light of today's world, lack of standardization and quality control are the major drawbacks that this form of medicine is facing however that about 80% of the population residing in the developing countries still has faith in this form of naturopathy.[25]
Every surface in the oral cavity, natural or synthetic, becomes covered within about 30 min with a 0.5–1.5 µ-thick precipitate of salivary glycoprotein and immunoglobulin that is termed “pellicle.”[26,27,28] The pellicle in turn provides a substrate to which oral debris (such as mucin, food particles, and desquamated epithelial cells) and microorganisms (bacteria and fungi) readily adhere.[29] This becomes even more important in patients wearing complete or partial removable dental prosthesis as the surface of the dental prosthesis provides a conducive atmosphere for the microorganisms to “house in,” of special consideration being the Candida harbor in the oral cavity. Candida is an important oral pathogen which can grow both on the hard and soft tissues. It forms complex biofilms which are aided by the surface texture of the denture base.[4] Radford et al.[30] described C. albicans as an asexual diploid fungus, which is yeast like with a unicellular method of growth and development.[30] Many studies have been done relating the surface texture of the denture base materials and the candidal growth.[31,32,33] High percentage of denture wearers are predisposed to the denture stomatitis.[34] Denture wearing is a predisposing factor for oral colonization by Candida and its prevalence can increase from 60% to 100%.[35]
Triphala is a tridoshic herbal formulation consisting of fruits of TB, TC, and EO in a 1:1:1 ratio.[5] This formulation is shown to have various medicinal properties which promote health, longevity of life when used in a proper manner. It is also shown to have anti-inflammatory, antioxidant, and antimicrobial properties (because of the gallic acid content), and is a known to be Hepatoprotective in nature.[36,37,38,39] It corrects constipation thus helping to improve digestion.[36] It can be ingested over a long period of time without any side effects. The phenolic and nonphenolic composition of triphala are active against both pathogenic and nonpathogenic bacterial strains;[40,41] when used as mouth wash, it effectively reduced the number of mutant streptococci in saliva.[42]
Various studies have been done to evaluate the antifungal property of triphala.[43,44,45,46] The present study was done to check the efficacy and ayurvedic composition against Candida on denture wearers. The results of this are in direct agreement with another study done by. Gautam et al.,[47] who through their study described that triphala had good antifungal potential. In a similar study done by Bajaj and Tandon,[48] they reported strong antifungal activity of triphala. Apoorva et al.[49] through their study suggested that triphala was effective against gingivitis. In the present study, majority were male population educating who would be easier compared to the rural female population, mean age of people was 64 years, and also, the majority belonged to the upper lower class showing the older age and low-income group, for whom acceptance of herbal composition is easier. Hence, in continuation and in agreement with the results of the other studies, the present study contributes to the fact that triphala has immense potential toward becoming a great denture cleanser as well a mouthwash. However, more studies are required to give a suitable concoction for its use as an antifungal mouthwash or a denture cleanser.
Conclusion
The results of the present study shows that among triphala churna and chlorhexidine gluconate, when used as a denture cleanser, triphala has a better antifungal property on the heat cure denture base material. Its availability in the rural setup, cost-effectiveness, and tremendous advantages makes this magical herb one of the best alternatives to the current antimicrobials that are being used. This study however has its limitations. The sample size used was small and the subjects were selected based on certain criteria that might limit the generalization of the results. It is doubtful whether patients strictly adhered to the set protocols although they were personally instructed to do so. More studies are required to evaluate the long-term effects of these natural-based products as denture cleansers. In the recent light of triphala emerging as an anticancer drug, it could be of some use in the oral cancer treatment, along with which triphala could also be breakthrough in terms of a mouthwash or a denture cleanser. Its easy availability and low cost make it a clear contender for this stake. In future, it can be rolled into the production of mouthwash which can be preserved for longer duration. For developing countries like India and many others worldwide where majority of the population is in the middle income range and elderly population is on the rise, this cost-effective and time-tested herb could prove as an effective mouthwash and a denture cleanser.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge the Department of Microbiology, Krishna Institute of Medical Sciences Deemed University, Karad, India.
References
- 1.Jeyalakshmi S, Chakrabarti S, Gupta N. Situation Analysis of the Elderly in India. Central Statistics Office Ministry of statistics and Programme Implementation Government of India. 2011:1–63. [Google Scholar]
- 2.Kujur D, Ekka RP. Socio-economic status of elderly people in India. Int Refereed Res J. 2010;2:3–6. [Google Scholar]
- 3.Shetty PJ, Hegde V, Gomes L. Anticandidal efficacy of denture cleansing tablet, Triphala, Aloe vera, and Cashew leaf on complete dentures of institutionalized elderly. J Ayurveda Integr Med. 2014;5:11–4. doi: 10.4103/0975-9476.128847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Govindswamy, Rodrigues S, Shenoy VK, Shenoy S, Shenoy R, Yadav T. The influence of surface roughness on the retention of Candida albicans to denture base acrylic resins – An in vitro study. J Nepal Dent Assoc. 2014;14:1–9. [Google Scholar]
- 5.Singh RL, Gupta R, Dwivedi N. A review on anti-microbial activities of Triphala and its constituents. World J Pharm Pharm Sci. 2016;5:535–58. [Google Scholar]
- 6.Balagopal S, Arjunkumar R. Chlorhexidine: The gold standard antiplaque agent. J Pharm Sci Res. 2013;5:570–4. [Google Scholar]
- 7.Academy of Prosthodontics. Glossory of prosthodontic terms. J Prosthet Dent. 2005;94:30. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Dhamande MM, Pakhan AJ, Thombare RU, Ghodpage SL. Evaluation of efficacy of commercial denture cleansing agents to reduce the fungal biofilm activity from heat polymerized denture acrylic resin: An in vitro study. Contemp Clin Dent. 2012;3:68–72. doi: 10.4103/0976-237X.96820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chassot AL, Poisl MI, Samuel SM. In vivo and in vitro evaluation of the efficacy of a peracetic acid-based disinfectant for decontamination of acrylic resins. Braz Dent J. 2006;17:117–21. doi: 10.1590/s0103-64402006000200006. [DOI] [PubMed] [Google Scholar]
- 10.Aneja KR, Joshi R, Sharma C. The antimicrobial potential of ten often used mouthwashes against four dental caries pathogens. Jundishapur J Microbiol. 2010;3:15–27. [Google Scholar]
- 11.Siqueira AB, Rodrigues L, Karine BR. Antifungal activity of propolis against Candida species isolated from cases of chronic periodontitis. Braz Oral Res. 2015;29:1807–3107. doi: 10.1590/1807-3107BOR-2015.vol29.0083. [DOI] [PubMed] [Google Scholar]
- 12.Moeintaghavi A, Arab H, Khajekaramodini M, Hosseini R, Danesteh H, Niknami H. In vitro antimicrobial comparison of chlorhexidine, persica mouthwash and miswak extract. J Contemp Dent Pract. 2012;13:147–52. doi: 10.5005/jp-journals-10024-1111. [DOI] [PubMed] [Google Scholar]
- 13.Pusateri CR, Monaco EA, Edgerton M. Sensitivity of Candida albicans biofilm cells grown on denture acrylic to antifungal proteins and chlorhexidine. Arch Oral Biol. 2009;54:588–94. doi: 10.1016/j.archoralbio.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flötra L, Gjermo P, Rölla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res. 1971;79:119–25. doi: 10.1111/j.1600-0722.1971.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 15.Eriksen HM, Nordbø H, Kantanen H, Ellingsen JE. Chemical plaque control and extrinsic tooth discoloration. A review of possible mechanisms. J Clin Periodontol. 1985;12:345–50. doi: 10.1111/j.1600-051x.1985.tb00924.x. [DOI] [PubMed] [Google Scholar]
- 16.Torwane NA, Hongal S, Goel P, Chandrashekar BR. Role of Ayurveda in management of oral health. Pharmacogn Rev. 2014;8:16–21. doi: 10.4103/0973-7847.125518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amruthesh S. Dentistry and Ayurveda-V: An evidence based approach. Indian J Dent Res. 2011;2:3–9. [Google Scholar]
- 18.Cowan MM. Plant products as antimicrobial agents. Clin Microbiol Rev. 1999;12:564–82. doi: 10.1128/cmr.12.4.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmad I, Beg AZ. Antimicrobial and phytochemical studies on 45 Indian medicinal plants against multi-drug resistant human pathogens. J Ethnopharmacol. 2001;74:113–23. doi: 10.1016/s0378-8741(00)00335-4. [DOI] [PubMed] [Google Scholar]
- 20.Saini R, Sharma S, Saini S. Ayurveda and herbs in dental health. Ayu. 2011;32:285–6. doi: 10.4103/0974-8520.92542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh J, Kumar A, Budhiraja S, Hooda A. Ethnomedicine: Use in dental caries. Braz J Oral Sci. 2007;6:21. [Google Scholar]
- 22.Kelmanson JE, Jäger AK, van Staden J. Zulu medicinal plants with antibacterial activity. J Ethnopharmacol. 2000;69:241–6. doi: 10.1016/s0378-8741(99)00147-6. [DOI] [PubMed] [Google Scholar]
- 23.Rao K. Materials for the database of medicinal plants. Bangalore: Karnataka State Council for Science and Technology; 2000. [Google Scholar]
- 24.Chopra RN, Chopra IC, Handa KL, Kapur LD. Chopra's Indigenous Drugs of India. 2nd ed. Calcutta: UN Dhur and Sons; 1958. [Google Scholar]
- 25.Pathak AK. Anti-Candida activity of aqueous extracts of some herbals. Indian J Fundam Appl Life Sci. 2012;2:1–6. [Google Scholar]
- 26.Skjørland KK, Rykke M, Sønju T. Rate of pellicle formation in vivo. Acta Odontol Scand. 1995;53:358–62. doi: 10.3109/00016359509006001. [DOI] [PubMed] [Google Scholar]
- 27.Carlén A, Börjesson AC, Nikdel K, Olsson J. Composition of pellicles formed in vivo on tooth surfaces in different parts of the dentition, and in vitro on hydroxyapatite. Caries Res. 1998;32:447–55. doi: 10.1159/000016486. [DOI] [PubMed] [Google Scholar]
- 28.Amaechi BT, Higham SM, Edgar WM, Milosevic A. Thickness of acquired salivary pellicle as a determinant of the sites of dental erosion. J Dent Res. 1999;78:1821–8. doi: 10.1177/00220345990780120901. [DOI] [PubMed] [Google Scholar]
- 29.Shay K. Denture hygiene: A review and update. J Contemp Dent Pract. 2000;1:28–41. [PubMed] [Google Scholar]
- 30.Radford DR, Challacombe SJ, Walter JD. Denture plaque and adherence of Candida albicans to denture-base materials in vivo and in vitro. Crit Rev Oral Biol Med. 1999;10:99–116. doi: 10.1177/10454411990100010501. [DOI] [PubMed] [Google Scholar]
- 31.Waters MG, Williams DW, Jagger RG, Lewis MA. Adherence of Candida albicans to experimental denture soft lining materials. J Prosthet Dent. 1997;77:306–12. doi: 10.1016/s0022-3913(97)70188-4. [DOI] [PubMed] [Google Scholar]
- 32.Taylor R, Maryan C, Verran J. Retention of oral microorganisms on cobalt-chromium alloy and dental acrylic resin with different surface finishes. J Prosthet Dent. 1998;80:592–7. doi: 10.1016/s0022-3913(98)70037-x. [DOI] [PubMed] [Google Scholar]
- 33.Verran J, Maryan CJ. Retention of Candida albicans on acrylic resin and silicone of different surface topography. J Prosthet Dent. 1997;77:535–9. doi: 10.1016/s0022-3913(97)70148-3. [DOI] [PubMed] [Google Scholar]
- 34.Al-Fahdawi IH. Fungal infection associated denture wearing according to the gender and type of materials. Glob J Med Res. 2015;1:8–9. [Google Scholar]
- 35.Geerts GA, Stuhlinger ME, Basson NJ. Effect of an antifungal denture liner on the saliva yeast count in patients with denture stomatitis: A pilot study. J Oral Rehabil. 2008;35:664–9. doi: 10.1111/j.1365-2842.2007.01805.x. [DOI] [PubMed] [Google Scholar]
- 36.Duke JA, Bogenschutz-Godwin MJ, Ducelliar J, Duke PA. Handbook of Medicinal Herbs. 2nd ed. Boca Raton: CRC Press; 2002. pp. 70–1. [Google Scholar]
- 37.Amala VE, Jeyaraj M. Determination of antibacterial, antifungal, bioactive constituents of Triphala by FT-IR and GC-MS analysis. Int J Pharm Pharm Sci. 2014;6:123–6. [Google Scholar]
- 38.Gupta R, Gupta A, Singh RL. Hepatoprotective activities of Triphala and its constituents. Int J Pharma Res Rev. 2015;4:34–55. [Google Scholar]
- 39.Gupta R, Singh RL, Singh P. Quantification of phytochemicals and evaluation of antioxidant potential of ethanolic leaf extract of Terminalia bellerica, Terminalia chebula and Emblica officinalis vis-a-vis Triphala. Int J Pharm Sci Rev Res. 2015;32:14–22. [Google Scholar]
- 40.Sharma DK, Varshneya C, Mehta M. Total phenolic content and antioxidant activity of Triphala (an Ayurvedic formulation) and its constituents. Am J PharmTech Res. 2012;2:458–65. [Google Scholar]
- 41.Ahmad I, Mehmood Z, Mohammad F. Screening of some Indian medicinal plants for their antimicrobial properties. J Ethnopharmacol. 1998;62:183–93. doi: 10.1016/s0378-8741(98)00055-5. [DOI] [PubMed] [Google Scholar]
- 42.Thomas B, Shetty SY, Shetty AV. Comparative evaluation of antimicrobial activity of Triphala and commercially available toothpaste: An in-vitro study. Int J Public Health Dent. 2011;2:8–12. [Google Scholar]
- 43.Biju T, Sunaina S, Agrima V, Veena S. Comparative evaluation of antimicrobial activity of Triphala and commercially available toothpastes: An in-vitro study. Int J Public Health Dent. 2011;2:8–12. [Google Scholar]
- 44.Sharma S. Triphala powder: A wonder of Ayurveda. Int J Recent Res Aspects. 2015;2:107–11. [Google Scholar]
- 45.Chainani SW, Siddana S, Reddy CV, Thippeswamy M, Maurya M, Rudraswamy S. Antimicrobial activity of Triphala on lactobacilli and Candida albicans: An in vitro study. J Orofac Sci. 2015;7:104–7. [Google Scholar]
- 46.Ruchika G, Chandrashekar BR, Pankaj G, Vrinda S, Sudheer H, Manish J, et al. Antimicrobial efficacy of aqueous and ethanolic extracts of Triphala on primary plaque colonizers: An in vitro study. J Young Pharm. 2014;6:7–13. [Google Scholar]
- 47.Gautam AK, Avasthi S, Sharma A, Bhadauria R. Antifungal potential of triphala churna ingredients against Aspergillus species associated with them during storage. Pak J Biol Sci. 2012;15:244–9. doi: 10.3923/pjbs.2012.244.249. [DOI] [PubMed] [Google Scholar]
- 48.Bajaj N, Tandon S. The effect of Triphala and chlorhexidine mouthwash on dental plaque, gingival inflammation, and microbial growth. Int J Ayurveda Res. 2011;2:29–36. doi: 10.4103/0974-7788.83188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Apoorva SM, Vinaya Shree MP, Suchetha A, Latha G, Sapna N, Bhat D. To compare the effect of Triphala gel formulation and Cinnamomum gel formulation on gingivitis – A clinical study. Int J Appl Dent Sci. 2015;1:136–40. [Google Scholar]