Abstract
Background:
Informal care giving can be burdensome particularly where the option of institutionalized informal care scarcely exist.
Objective:
To look at the burden of informal caregivers of stroke survivors using the Zarit burden interview (ZBI).
Method:
64 stroke survivors were assessed for demographics of age, gender, duration of follow-up since discharged from in-patient care, modified Rankin score at the time of discharge and at the time of evaluation for this study and the most important informal care giver at home was also assessed for whether care giving was telling on their health or life in any negative way. All the caregivers were subsequently assessed with the ZBI.
Results:
Mean age of most important informal care givers was 40.67 ± 14.27 years and the sex distribution was 33(51.6%) female and 29(45.4%) males. 21(32.8%) reported that caregiving was a health burden. Mean ZBI scores were significantly higher (30.19 ± 14.81 vs 20.30 ± 12.96, P < 0.01) in those that reported that caregiving was telling on their health. ZBI overall rating of burden of caregiving was also significantly associated with whether caregiving was telling on the health of caregiver (P = 0.01) and also symmetrically agreed with whether the burden of caregiving was telling on health (k = 0.33, P < 0.01). The sensitivity and specificity of ZBI were 70% and 68.4% respectively on ROC statistics (AUC = 0.67, P = 0.017).
Conclusion:
Reported burden of informal caregiving of about 33% is in our opinion huge. The moderate sensitivity and specificity of the ZBI means it could be safely used in the population studied.
Keywords: Burden, caregiver, stroke, survivors, Zarit Burden Interview, Fardeau, aidant, accident vasculaire cérébral, survivants, Zarit Burden Interview
Résumé
Contexte:
La prise en charge informelle peut être lourde, surtout lorsque l’option des soins informels institutionnalisés n’existe pratiquement pas.
Objectif:
Examiner le fardeau des soignants informels des survivants d’AVC en utilisant l’interview Zarit fardeau (ZBI).
Méthode:
64 survivants d’un AVC ont été évalués pour Les données démographiques relatives à l’âge, au sexe, à la durée du suivi depuis le congé des patients hospitalisés, au score de Rankin modifié au moment du Le moment de l’évaluation de cette étude et le plus important dispensateur de soins informels à domicile a également été évalué pour savoir si La santé ou la vie de manière négative. Tous les soignants ont ensuite été évalués avec la ZBI.
Résultats:
Âge moyen des soins informels les plus importants Des donneurs était de 40,67 ± 14,27 ans et la répartition par sexe était de 33 (51,6%) femmes et de 29 (45,4%) hommes. 21 (32,8%) ont déclaré que la prestation de soins charge. Les scores moyens de ZBI étaient significativement plus élevés (30,19 ± 14,81 vs 20,30 ± 12,96, P < 0,01) chez ceux qui indiquaient que les soins donnaient santé. ZBI évaluation globale du fardeau de caregiving a également été significativement associée à savoir si la prestation de soins était révélateur sur la santé de l’aidant naturel (P = 0,01) et aussi symétriquement d’accord avec la question de savoir si le fardeau de la prestation de soins était révélateur sur la santé (k = 0,33, P < 0,01). La sensibilité et la spécificité De ZBI étaient 70% et 68.4% respectivement sur les statistiques de ROC (AUC = 0.67, P = 0.017).
Conclusion:
Le fardeau de la prestation de soins informels 33% est à notre avis énorme. La sensibilité et la spécificité modérées de la ZBI signifient qu’elle pourrait être utilisée en toute sécurité dans la population étudiée.
Introduction
Informal caregivers are non-medically trained persons who offer supportive care to persons who have medical conditions that affect their ability to carry out basic activities of daily living (ADL). Their role(s) in caring for the invalid can be huge and complementary in chronic conditions like in those recuperating from a manifest stroke with disability severe enough to affect ADL.[1] It is estimated that there are about 60 million stroke survivors in the world and about a third to two-thirds of these are dependent with a modified Rankin score of 3 and above.[2] The disability-adjusted life year, which is the sum of the number of years lost to ill-health and the number of years lost from life expectancy, is higher in stroke survivors and stroke is also the leading cause of non-accidental chronic disability.[3]
Caring for stroke survivors informally can be burdensome and particularly so in climes where institutionalized informal care is not readily available.[1,4,5,6] The corollary is that informal care devolves on close relatives of the invalid. Informal caregiving could cause man-hour losses, physical, mental, and emotional strain and in extreme cases a burnt-out feeling in the caregiver.[7,8,9]
There are well-established tools for the assessment of informal caregivers’ burden, and this has been done in western and other climes. The Zarit Burden Interview (ZBI) is an example of a widely used tool for this purpose.[10,11,12] Although originally used in the assessment of caregivers’ burden in caring for the elderly, its use has been expanded since it was first published about four decades ago.[13] ZBI is originally a 22-item tool that is grouped into six sections which document the informal caregiver's assessment of the burden of caregiving. It also has a second part that allows for global rating of the burden of care, thereby offering the user both quantitative and qualitative assessment of the burden of caregiving. Several short versions that are user-friendly have been developed from the original unabridged version [Appendix for ZBI].
This study assessed informal caregivers’ burden in stroke survivors in a neurology outpatient clinic in sub-Saharan Africa using the ZBI and validated it in the process.
Methods
Sixty-four stroke survivors on follow-up in a neurology outpatient clinic were consecutively assessed with a questionnaire for demographics of age, gender, level of education and stroke type, duration of follow-up since discharged from inpatient care, modified Rankin score at the time of discharge and modified Rankin score at the time of evaluation in the clinic for this study and the most important informal caregiver at home was also assessed for age, gender, level of education, relationship to patient, whether caregiver is on stipend or not, duration of care, whether there are other caregivers(s) or not, number of hours of caregiving in 24 h. Furthermore, the caregiver was assessed for whether caregiving was telling on their health or life in any negative way and whether they wanted to be relieved of the caregiving duties or not.
All the caregivers were subsequently assessed with the ZBI, and their scores were recorded in a pro forma. The study was approved by the research and ethics committee of the institution where the study was done.
Data were entered into a spreadsheet and exported to SPSS version 21. Data were presented as proportions and percentages for categorical and discrete variables and mean and standard deviations and median and interquartile range (IQR) for normally and skewed continuous variables, respectively. Data were compared between caregivers that reported that caregiving was telling on their health and those that reported it was not. Categorical variables were compared with Pearson's Chi-square and continuous variables with independent t-test or median test as appropriate. Symmetric agreement between ZBI score and ZBI global rating and the effect of caregiving on health or life as reported by caregiver was tested on crosstab kappa statistics. The sensitivity and specificity of ZBI score were tested on receiver operated characteristics curve. P < 0.05 was taken as statistically significant for all tests.
Results
The mean age of stroke survivors was 66.11 ± 11.60 years, and sex distribution was 21 (32.8%) females and 43 (67.2%) males. 57 (89.1%) had cerebral infarct, and 7 (10.9%) had cerebral hemorrhage. The median duration of follow-up since discharge from in-patient care was 330 days, (IQR 730–39). Median modified Rankin score at discharge and at the time of evaluation in clinic were 4 (IQR 5–3) and 3 (IQR 4–3), respectively [Table 1].
Table 1.
Basic characteristics of stroke survivors
| Parameters | Value |
|---|---|
| Mean age±SD (years) | 66.11±11.60 |
| Sex (female/male), n (%) | 21/43 (32.8/67.2) |
| Stroke type, n (%) | |
| Cerebral infarct | 57 (89.1) |
| Intracerebral hemorrhage | 7 (10.9) |
| Median duration of followup in days (IQR) | 330 (730-39) |
| Median Rankin score at discharge in days (IQR) | 4 (5-3) |
| Median Rankin score at evaluation in clinic for study in days (IQR) | 3 (4-3) |
SD=Standard deviation, IQR=Interquartile range
Mean age of most important informal caregivers was 40.67 ± 14.27 years and the sex distribution was 33 (51.6%) females and 29 (48.4%) males. Only 4 (6.2%) of caregivers were not biologically related to the stroke survivors; 14 (21.9%) of caregivers were on stipends; 21 (32.8%) reported that caregiving was telling on their health; and 11 (17.2%) reported that they wanted relief from the burden of caregiving [Table 2].
Table 2.
Basic characteristics of caregivers
| Parameter | Value, n (%) |
|---|---|
| Mean age±SD (years) | 40.67±14.27 |
| Sex (female/male) | 33/29 (51.6/48.4) |
| Caregivers biologically related to stroke survivors | 60 (93.8) |
| Caregivers on stipends | 14 (21.9) |
| Caregivers that reported that caregiving was telling on health | 21 (32.8) |
| Caregivers that reported they wanted relief | 11 (17.2) |
SD=Standard deviation
Data were subsequently compared between caregivers who reported that caregiving was telling on their health and those that reported it was not.
Caregivers who reported that burden of caregiving was telling on their health compared to those that did not report, did not differ significantly in age (P = 0.17), sex (P = 0.61), educational level (P = 0.16), duration of caregiving (P = 0.32), number of hours of caregiving per day (P = 0.74), and modified Rankin score of stroke survivors both at discharge and at the time of evaluation for the study (P = 0.60), and (P = 0.86), respectively [Table 3].
Table 3.
Comparing characteristics of caregivers who reported that caregiving was telling on their health versus those that reported otherwise
| Parameter | Caregivers that reported caregiving was telling on health (n=43) | Caregivers that reported caregiving was not telling on health (n=21) | P |
|---|---|---|---|
| Mean age±SD, (years) | 63.40±12.39 | 67.70±11.08 | 0.17 |
| Sex (female/male) | 24/19 | 10/11 | 0.61 |
| Educational level | |||
| No formal education | 5 | 1 | 0.16 |
| Primary | 8 | 5 | |
| Secondary | 4 | 6 | |
| Tertiary | 26 | 9 | |
| Median duration of caregiving in months (IQR) | 12 (24-1) | 24 (36-6.5) | 0.32 |
| Median number of hours of caregiving per day (IQR) | 15 (24-8) | 16 (24-12) | 0.74 |
| Median modified Rankin score at discharge in days (IQR) | 4 (5-3) | 5 (5-3) | 0.60 |
| Median modified Rankin score at evaluation in clinic in days (IQR) | 3 (4-2) | 3 (4-2) | 0.86 |
| Mean ZBI score±SD | 30.14±14.81 | 20.30±12.96 | <0.01 |
SD=Standard deviation, IQR=Interquartile range, ZBI=Zarit Burden interview
However, mean ZBI score was significantly higher in those that reported that caregiving was telling on their health (30.19 ± 14.81 vs. 20.30 ± 12.96; P < 0.01) [Table 3]. ZBI global rating of burden of caregiving symmetrically agreed with whether the burden of caregiving was telling on health or not (k = 0.33, P < 0.01) [Table 4].
Table 4.
Symmetric agreement between Zarit Burden interview global rating of burden of caregiving and caregivers’ report of effect of caregiving on health
| Parameters | κ | P |
|---|---|---|
| ZBI global rating of burden of caregiving | 0.33 | <0.01 |
| Effect of caregiving on health |
ZBI=Zarit Burden interview
The sensitivity and specificity of ZBI numerical scale were70% and 68.4%, respectively, area under the curve = 0.69, P = 0.01 [Figure 1].
Figure 1.
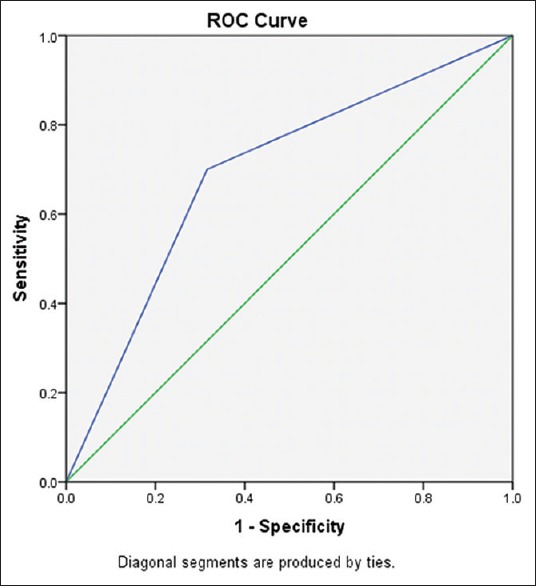
ROC curve showing sensitivity and specificity of Zarit Burden Interview
Discussion
The mean age of the stroke survivors and the preponderance of males are consistent with similar studies as well as the predominance of cerebral infarcts as the stroke type.[14] The long median duration of follow-up (330 days) and higher median Rankin score at the time of discharge and evaluation in clinic for the stroke survivors are remarkable as they provided ample opportunity to assess the burden of informal caregivers in predominantly dependent (Rankin score of 3 and above) subjects. The burden of informal caregiving is known to be affected by the level of dependence of the subject being cared for and also by the duration of caregiving.[1,13,15,16] The relative younger age of the caregivers and the female sex preponderance are also noteworthy; it may be reflective of the age range of fitness of the individuals who can offer caregiving and the general tendency to have more females in informal caregiving and home nursing.[13,15,17] That the majority of caregivers were biologically related to the stroke survivors is indicative of the relative scarcity of institutionalized informal caregiving in the clime in which the study was carried out. Institutionalized informal caregiving scarcely exists in sub-Saharan Africa hence caregiving by biologic relatives is the rule rather than the exception.[18,19] This is corroborated by the small number (about a fifth) of caregivers that received stipends for caregiving.
Remarkably, about a third (32.1%) of caregivers reported that the burden of caregiving was telling on their health and about a fifth (17.2%) said they wanted to be relieved of their caregiving duties. The proportion of those that reported that caregiving was affecting their health in a negative way is huge in our opinion, and particularly so in a clime where social security like health insurance is almost not existent for the large majority. The social effect of this is that the caregivers have to seek help on their own and this adds to the societal burden of disease.
| Coordinates of the curve Test result variable(s): Overall | ||
|---|---|---|
| Positive if greater than or equal to | Sensitivity | 1 - Specificity |
| 0.0000 | 1.000 | 1.000 |
| 1.5000 | 0.700 | 0.316 |
| 3.0000 | 0.000 | 0.000 |
The test result variable(s): Overall has at least one tie between the positive actual state group and the negative actual state group
| Area | P | 95% CI | |
|---|---|---|---|
| Lower bound | Upper bound | ||
| 0.692 | 0.01 | 0.547 | 0.837 |
CI=Confidence interval
The absence of significant differences between the demographic characteristics of age, sex, educational level, and modified Rankin scores of stroke survivors whose caregivers reported that caregiving was telling on their health and those that reported it was not, suggests that factors inherent in the caregivers might be more prevalent in determining the effect of caregiving on health in this study.[19] However, related studies have shown that the age, sex, educational level, and level of functional independence as measured by modified Rankin score of the stroke survivor and the age and educational level of the caregiver and hours per day of caregiving are determinants of the burden of caregiving.[14,20,21]
It is noteworthy that ZBI measure of caregivers’ burden was numerically and qualitatively (global rating) higher in caregivers that reported that caregiving was telling on their health. This assesses the burden of caregiving as reported by the caregiver. The 33% symmetric agreement between ZBI global rating of the burden of caregiving and caregivers’ assessment of the effect of caregiving on their health may appear low, but that it achieved statistical significance deserves to be mentioned. Although the sensitivity and specificity of ZBI score were significantly moderate (70 and 68.4%, respectively), it, however, shows that it could safely be used to objectively assess the burden of caregiving as have been profusely done in similar studies in other climes.[22] Its use in populations of similar composition is therefore recommended.
The small sample size of study participants is an obvious limitation in this work.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the contributions of other members and support staff of the neurology outpatient department of the University of Benin Teaching Hospital, Benin City, Nigeria.
APPENDIX: Zarit's burden interview (abridged version)
Instructions:
The following is a list of statements which reflect how people sometimes feel when taking care of another person.
After each statement, indicate how often you feel that way: never, rarely, sometimes, quite frequently, or nearly always. There are no right or wrong answers.
1. Do you feel that your relative asks for more help than he or she needs?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
2. Do you feel that, because of the time you spend with your relative, you don’t have enough time for yourself?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
3. Do you feel stressed between caring for your relative and trying to meet other responsibilities for your family or work?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
4. Do you feel embarrassed about your relative's behavior?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
5. Do you feel angry when you are around your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
6. Do you feel that your relative currently affects your relationship with other family members?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
7. Are you afraid about what the future holds for your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
8. Do you feel that your relative is dependent upon you?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
9. Do you feel strained when you are around your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
10. Do you feel that your health has suffered because of your involvement with your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
11. Do you feel that you don’t have as much privacy as you would like, because of your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
12. Do you feel that your social life has suffered because you are caring for your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
13. Do you feel uncomfortable having your friends over because of your relative?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
14. Do you feel that your relative seems to expect you to take care of him or her, as if you were the only one he or she could depend on?
0. Never 1 Rarely 2 Sometimes 3 Quite Frequently 4 Nearly Always
Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980;20:649-55.
Scoring:
The Burden Interview is scored by adding the numbered responses of the individual items.
Higher scores indicate greater caregiver distress. The Burden Interview, however, should not be taken as the only indicator of the caregiver's emotional state. Clinical observations and other instruments, such as measures of depression, should be used to supplement this measure.
Norms for the Burden Interview have not been computed, but estimates of the degree of burden can be made from preliminary fifindings. These are:
0–20: Little or no burden
21–40: Mild to moderate burden
41–60: Moderate to severe burden
61–88: Severe burden.
Sources:
Brown JL, Potter JF, Foster BG. Caregiver burden should be evaluated during geriatric assessment. J Am Geriatr Soc 1990;38:455-60.
Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, et al. Guidelines for managing Alzheimer's disease: Part I-Assessment. Am Fam Physician 2002;65: 2263-72.
Physicians and family caregivers: A model for partnership: Council on Scientific Affairs, American Medical Association. JAMA 1993;269:1282-84.
Rankin ED, Haut MW, Keefover RW, Franzen MD. The establishment of clinical cutoffs in measuring caregiver burden in dementia. Gerontologist 1994;34:828-32.
Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980;20:649-55.
References
- 1.Rigby H, Gubitz G, Eskes G, Reidy Y, Christian C, Grover V, et al. Caring for stroke survivors: Baseline and 1-year determinants of caregiver burden. Int J Stroke. 2009;4:152–8. doi: 10.1111/j.1747-4949.2009.00287.x. [DOI] [PubMed] [Google Scholar]
- 2.Hong KS. Disability-adjusted life years analysis: Implications for stroke research. J Clin Neurol. 2011;7:109–14. doi: 10.3988/jcn.2011.7.3.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lemogoum D, Degaute JP, Bovet P. Stroke prevention, treatment, and rehabilitation in sub-saharan Africa. Am J Prev Med. 2005;29(5 Suppl 1):95–101. doi: 10.1016/j.amepre.2005.07.025. [DOI] [PubMed] [Google Scholar]
- 4.Sales E. Family burden and quality of life. Qual Life Res. 2003;12(Suppl 1):33–41. doi: 10.1023/a:1023513218433. [DOI] [PubMed] [Google Scholar]
- 5.Camak DJ. Addressing the burden of stroke caregivers: A literature review. J Clin Nurs. 2015;24:2376–82. doi: 10.1111/jocn.12884. [DOI] [PubMed] [Google Scholar]
- 6.Saban KL, Sherwood PR, DeVon HA, Hynes DM. Measures of psychological stress and physical health in family caregivers of stroke survivors: A literature review. J Neurosci Nurs. 2010;42:128–38. doi: 10.1097/jnn.0b013e3181d4a3ee. [DOI] [PubMed] [Google Scholar]
- 7.Carod-Artal FJ, Egido JA. Quality of life after stroke: The importance of a good recovery. Cerebrovasc Dis. 2009;27(Suppl 1):204–14. doi: 10.1159/000200461. [DOI] [PubMed] [Google Scholar]
- 8.King RB, Semik PE. Stroke caregiving: Difficult times, resource use, and needs during the first 2 years. J Gerontol Nurs. 2006;32:37–44. doi: 10.3928/00989134-20060401-07. [DOI] [PubMed] [Google Scholar]
- 9.Gbiri CA, Olawale OA, Isaac SO. Stroke management: Informal caregivers’ burdens and strians of caring for stroke survivors. Ann Phys Rehabil Med. 2015;58:98–103. doi: 10.1016/j.rehab.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 10.Gort AM, Mingot M, Gomez X, Soler T, Torres G, Sacristán O, et al. Use of the Zarit scale for assessing caregiver burden and collapse in caregiving at home in dementias. Int J Geriatr Psychiatry. 2007;22:957–62. doi: 10.1002/gps.1770. [DOI] [PubMed] [Google Scholar]
- 11.Van Durme T, Macq J, Jeanmart C, Gobert M. Tools for measuring the impact of informal caregiving of the elderly: A literature review. Int J Nurs Stud. 2012;49:490–504. doi: 10.1016/j.ijnurstu.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Sonoda S, Shirayama Y, Sakamoto R, Nagai S, Sakurai S. Factors influencing the Zarit Burden Interview in a Japanese community: Activities of daily living and depressive state. Int J Phys Med Rehabil. 2014;2:216. [Google Scholar]
- 13.Bhattacharjee M, Vairale J, Gawali K, Dalal PM. Factors affecting burden on caregivers of stroke survivors: Population-based study in Mumbai (India) Ann Indian Acad Neurol. 2012;15:113–9. doi: 10.4103/0972-2327.94994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Imarhiagbe FA, Abidakun A. Functional motor recovery in stroke survivors-determinants in a sub-Saharan African stroke unit. East Afr Med J. 2014;91:119–24. [PubMed] [Google Scholar]
- 15.Ogunlana MO, Olumide OD, Oyewo OS, Odole OC, Ogunsan MO. Quality of life and burden of informal caregivers of stroke survivors. Hong Kong Physiother J. 2014;32:6–12. [Google Scholar]
- 16.Choi-Kwon S, Kim HS, Kwon SU, Kim JS. Factors affecting the burden on caregivers of stroke survivors in South Korea. Arch Phys Med Rehabil. 2005;86:1043–8. doi: 10.1016/j.apmr.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Yang X, Hao Y, George SM, Wang L. Factors associated with health-related quality of life among Chinese caregivers of the older adults living in the community: A cross-sectional study. Health Qual Life Outcomes. 2012;10:143. doi: 10.1186/1477-7525-10-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fatoye FO, Komolafe MA, Adewuya AO, Fatoye GK. Emotional distress and self-reported quality of life among primary caregivers of stroke survivors in Nigeria. East Afr Med J. 2006;83:271–9. doi: 10.4314/eamj.v83i5.9433. [DOI] [PubMed] [Google Scholar]
- 19.Vincent-Onabajo G, Ali A, Hamzat T. Quality of life of Nigerian informal caregivers of community-dwelling stroke survivors. Scand J Caring Sci. 2013;27:977–82. doi: 10.1111/scs.12017. [DOI] [PubMed] [Google Scholar]
- 20.Scholte Op Reimer WJ, de Haan RJ, Rijnders PT, Limburg M, van den Bos GA. The burden of caregiving in partners of long-term stroke survivors. Stroke. 1998;29:1605–11. doi: 10.1161/01.str.29.8.1605. [DOI] [PubMed] [Google Scholar]
- 21.Nimnual C, Rapin C, Doldao P, Chompunut S. Family burden of stroke patients in Rayong Hospital Thailand. Int J Appl Psychol. 2016;6:15–9. [Google Scholar]
- 22.Schreiner AS, Morimoto T, Arai Y, Zarit S. Assessing family caregiver's mental health using a statistically derived cut-off score for the Zarit Burden Interview. Aging Ment Health. 2006;10:107–11. doi: 10.1080/13607860500312142. [DOI] [PubMed] [Google Scholar]


