Abstract
BACKGROUND
Repeated head trauma has been associated with risk of neurodegenerative diseases. Few studies have evaluated the long-term risk of neurodegenerative diseases in collision sports like football.
OBJECTIVE
To assess whether athletes who played American varsity high-school football between 1956 and 1970 have an increased risk of neurodegenerative diseases later in life.
PATIENTS AND METHODS
We identified all male varsity football players between 1956 and 1970 in the public high schools of Rochester, Minnesota, compared to non-football-playing male varsity swimmers, wrestlers or basketball players. Using the records-linkage system of the Rochester Epidemiology Project, we ascertained the incidence of late-life neurodegenerative diseases: dementia, parkinsonism, or amyotrophic lateral sclerosis. We also recorded medical record-documented head trauma during high school years.
RESULTS
We identified 296 varsity football players and 190 athletes engaging in other sports. Football players had an increased risk of medically documented head trauma, especially if they played football for more than one year. Compared to non-football athletes, football players did not have an increased risk of neurodegenerative disease overall, nor the individual conditions of dementia, parkinsonism, or amyotrophic lateral sclerosis.
CONCLUSION
In this community based study, varsity high school football players from 1956 to 1970 did not have an increased risk of developing neurodegenerative diseases compared with athletes engaged in other varsity sports. This was from an era where there was a generally nihilistic view of concussion dangers, less protective equipment and without prohibition of spearing (head-first tackling). However, size and strength of players from prior eras may not be comparable to current high-school athletes.
Keywords: high-school football, concussions, degeneration
INTRODUCTION
For more than a century, head trauma has been linked to subsequent risks of neurodegenerative disease later in life1 and, specifically, dementia/Alzheimer’s disease,1 Parkinson’s disease (PD)2 and amyotrophic lateral sclerosis (ALS).3 These conditions have been reported to be substantial among those engaged in contact sports.4 Recent publicity has focused on the dangers of American football, especially as played at the professional and college levels, with later risk of the dementia of chronic traumatic encephalopathy.5
Football is arguably America’s most popular sport and is played in nearly every high school. Football is a “collision” sport, where concussions commonly occur and where sub-concussions may be routine, at least at college and professional levels.6 This may have implications for brain health later in life with theoretical risks for dementia or other neurodegenerative disorders. The importance of the topic has societal implications, with some authorities questioning the wisdom of youth football.7 On the other hand, high school sports have certain redeeming features, most notably the benefits of fitness training, which not only favors cardiovascular health but may also have a neuroprotective effect against later neurodegenerative diseases including dementia and Parkinson’s disease.8,9
We previously investigated long-term neurologic outcomes of a cohort of high school football players from 1946 to 1956 and found no increased risks of dementia, PD, or ALS, compared to non-football playing high school classmates or to the general population.10 The goal of the current study is to extend the investigations to another cohort of varsity high school football players from the next era, 1956 to 1970. This was a time when rules, regulations, and the physical ability of the football players were evolving to mirror more closely the present era. Still in this era, football-related concussions were often minimized or dismissed as “getting your bell rung.” In the current study, a cohort of high-school football players was compared to a cohort of non-football-playing, male high-school athletes (swimmers, basketball players, wrestlers) to assess the long-term neurologic outcomes of dementia, parkinsonism and ALS.
METHODS
Study design
This study design mirrored our previous investigation of a varsity high-school football cohort who played between 1946–1956.10 In the present study, we utilized the same methodology and reviewed all yearbooks of the two public high schools in the city of Rochester, Minnesota, between 1956 and 1970: Mayo High School and Rochester High School (now called John Marshall High School). All information contained in the yearbooks is in the public domain and was freely accessible at The History Center of Olmsted County, MN. We used these yearbooks to document the rosters of varsity football players plus the comparison-cohort of male high-school classmates playing varsity basketball, swimming or wrestling. The yearbooks contained relevant demographic information including sport and activity engagement. Soccer, tennis, boxing, and hockey were not consistently available sports during these study years, and female sports programs were not consistently offered in these schools.
We identified two different groups of male high-school athletes in the yearbooks: 1) Students who played varsity football; 2) Student-athletes who never played football but were varsity swimmers, basketball players or wrestlers. Athletes who played other sports in addition to football were included in the football group (Figure 1).
Figure 1. Flowchart of the study.
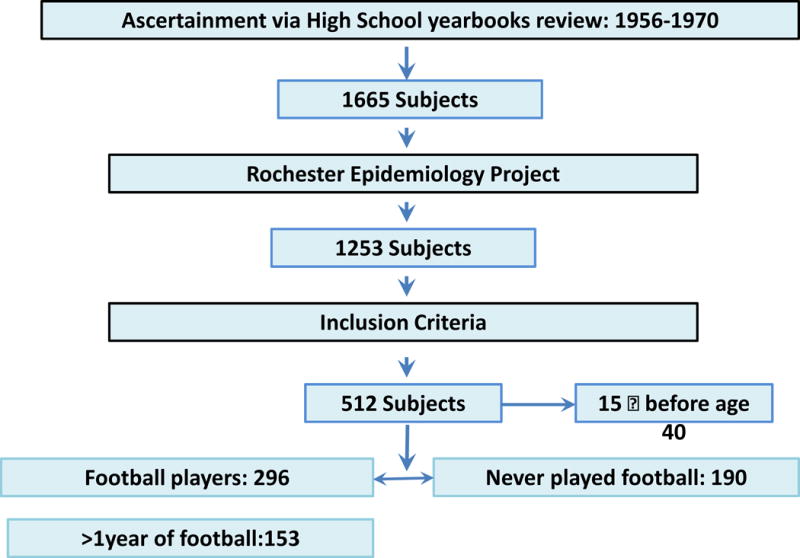
Footnote: ¶ deceseased students. §: all students that ever participated in football °swimmers, basketball players, and wrestlers.
We utilized the records-linkage system of the Rochester Epidemiology Project (REP), which provided access to the medical records of each included individual. The REP is a unique medical records-linkage system that encompasses the care delivered to all the residents of Olmsted County, Minnesota. Individuals visiting any of the county care providers generate records in the system. This is an active records-linkage system that spans from the early 1900s to the present. Further details on the REP have been reported elsewhere.11,12,13 The REP includes a tool that allows searching for individuals on the basis of their names and the year of birth. We searched for each person on our compiled lists, using his full name and the approximate year of birth (assuming that students graduated at age 18+/−2 years) as in the previous study.10 The Institutional Review Boards of Mayo Clinic and Olmsted Medical Center approved the study.
We limited our cohort of subjects to individuals who had a constant and prolonged medical presence in the REP and received their medical care at the Mayo Clinic, Olmsted Medical Center or other Olmsted County facilities. We only included students with updated medical records to 2005 or later. We excluded students who had left the county or who did not have continuous evidence of medical records up to at least 2005 in the REP.
Neurological outcomes
We reviewed the entire medical record of each student and compared the long-term neurological outcomes of the football players with the non-football groups. We focused on the development of neurological diseases: parkinsonism; dementias of all types; ALS. We also abstracted medically documented head trauma.
We used a two-step process to abstract the medical records. First, we screened the electronic medical indexes of the records-linkage system using the REP tools. We reviewed each individual medical record, identifying dementia of any type, parkinsonism of any type, and ALS as well as medically-documented head trauma occurred in the athletes during the study period. Second, one of the researchers (PJ), unaware of the athletic group of the students (football players vs non–football players), reviewed the complete available medical charts of all those who ever received one of the diagnoses in order to confirm the electronic-based diagnosis.
To determine the reliability of the clinical diagnosis of the abstractor, we compared his diagnoses with the diagnoses made by a senior neurologist (RS). There were no statistical differences between the diagnoses made by the neurologist and the diagnoses by the first abstractor.
Data analysis
Descriptive summaries were reported as frequencies and percentages for categorical variables. Our primary analysis compared whether any exposure to playing football (yes, no) was a predictor for developing neurodegenerative disorders. Secondary analysis examined football played more than one year versus no football, as well as students engaged only in football (primary sport) and students engaged in football plus other sports, (yes, no). Between-group comparisons were performed using Fisher’s exact test as appropriate. The association between the exposure to playing football and the development of neurodegenerative diseases later in life was reported as an incidence rate ratio (IRR). IRR is a ratio of incidence rate among exposed to unexposed, where incidence rate is calculated as the number of events divided by person years of follow-up. Incidence rates were calculated using Poisson distribution due to rare events (i.e., fewer number of patients with neurodegenerative disease). All tests were two-sided, and p-values less than 0.05 were considered statistically significant. Analyses were performed by a statistician (JM) using SAS version 9.3 (SAS Institute Inc, Cary, NC).
RESULTS
We identified 1,665 men from high-school yearbooks meeting criteria (1290, Rochester High School; 375, Mayo High School). Of this initial group, 1,253 were identified in the REP-browser (the others had no medical records or lack of correspondence with names). We excluded 752 students whom we could not match with certainty in the REP (common names, lack of first name, same year of age, etc.). The excluded students were equally distributed among all the sports considered (football, swimming, basketball, and wrestling). Another fifteen students were deceased before the age of 40 (n=15) and were excluded from the neurological outcome analyses. (None of the fifteen deceased had a diagnosis consistent with neurodegenerative diseases.)
Ultimately, we were able to successfully identify 486 high school athletes with sufficient medical documentation. This study cohort consisted of men aged 62 through 78 years at the time of the outcome analysis. Of these 486 high school athletes, 296 (61%) played football and most of these 296 football players played only football (253; 85%). Approximately half of this group, 153 students, played more than one year of football whereas 143 played only one year (Figure 1). The comparison group consisted of 190 varsity swimmers, basketball players or wrestlers.
Head trauma was documented in 48 athletes. This included 34 cases in the football group and 14 in the non-footballers. The median length of followup in our study (birth to death or last follow-up was 64.64 years IQR: 62.25, 68.73); thus each student was observed for about 40 years after the participation in high school sports. Among all the high school athletes, we identified 14 cases of dementia/MCI (3 dementia and 11 MCI), 7 cases of parkinsonism, and no cases of ALS. Among students who had played football for one or more years there were 2 cases of dementia, 5 cases of MCI, 3 of parkinsonism, and 0 cases of ALS. Among the non-football players (swimmers, basketball players, wrestlers) there was 1 case of dementia, 4 cases of MCI, 3 of parkinsonism, and 0 cases of ALS (Table 1). In total, 10 of 296 varsity football players developed a neurodegenerative outcome (3%) whereas 8 of 190 non-football varsity athletes (4%) developed a neurodegenerative outcome.
Table 1.
Comparison between frequency of dementia, MCI, ALS, parkinsonism, and head trauma between football players and non-football players and comparison between students who played football >1 year as compared with the non-football players
| Football (N=296) | No Football (N=190) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Disease | Count | Person Years | Incidence Rate Ratio | 95% CI | Count | Person Years | Rate | 95% CI | Incidence Rate Ratio | 95% CI | p-value |
| Dementia / MCI | 7 | 19226.28 | 3.64 | (1.46, 7.50) | 4 | 12362.34 | 3.24 | (0.88, 8.28) | 2.13 | (0.45, 2.32) | 1.68 |
| ALS | 0 | 19261.46 | 0.00 | (0.00, 1.92) | 0 | 12374.73 | 0.00 | (0.00, 2.98) | NA | NA | NA |
| Parkinsonism | 4 | 19250.80 | 2.08 | (0.57, 5.32) | 3 | 12361.68 | 2.43 | (0.50, 7.09) | 0.86 | (0.23, 2.19) | 1.00 |
| Head Trauma | 34 | 17542.99 | 19.38 | (13.42, 27.08) | 14 | 11670.70 | 12.00 | (6.56, 20.13) | 1.62 | (1.12, 2.26) | <.001 |
When we compared the frequency of individual neurological disorders, we found no significant differences between varsity football players (ever-played) versus non-football athletes in any of the three neurodegenerative outcomes: dementia/MCI (IRR: 1.29; 95% Confidence Interval (CI): 0.45–2.32, p = .69); parkinsonism (IRR: 0.86; 95% CI: 0.23–2.19, p= 1); ALS (no cases observed). Medically documented head trauma was significantly more frequent in the football players compared to the other athletes (IRR: 1.62; 95% CI: 1.12–2.26, p=.008).
In order to study more substantial, prolonged exposure to possible head trauma, we excluded all the students that played football for only one year and compared the football players with more than one year of football to the non-football athletes. Despite the presence of an increase in head trauma in the football group (IRR: 2.27; 95% CI: 1.45–3.38, p= <.001), we did not observe any significant differences in neurodegenerative disorders between the two groups (Table 1–2).
Table 2.
Comparison between frequency of dementia, MCI, ALS, parkinsonism, and head trauma between students who played football as primary sport and students who played football not as primary sport
| >1 year of playing football (N=153) | No Football (N=190) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | Person Years | Rate | 95% CI | Count | Person Years | Rate | 95% CI | Rate Ratio | 95% CI | p-value | |
| Dementia / MCI | 5 | 10013.97 | 4.99 | (1.62, 11.65) | 4 | 12362.34 | 3.24 | (0.88, 8.28) | 1.54 | (0.50, 3.60) | .26 |
| ALS | 0 | 10032.67 | 0.00 | (0.00, 3.68) | 0 | 12374.73 | 0.00 | (0.00, 2.98) | NA | NA | NA |
| Parkinsonism | 3 | 10022.59 | 2.99 | (0.62, 8.75) | 3 | 12361.68 | 2.43 | (0.50, 7.09) | 1.23 | (0.25, 3.61) | .52 |
| Head trauma | 24 | 8818.31 | 27.22 | (27.44, 40.50) | 14 | 11670.70 | 12.00 | (6.56, 20.13) | 2.27 | (1.45, 3.38) | <.01 |
DISCUSSION
Our cohort of high-school varsity football athletes playing between 1956 and 1970 did not have an overall increased risk of neurodegenerative outcomes, nor individual risks of dementia/MCI, parkinsonism, or ALS compared with non-football playing classmates. This was despite significantly more medically documented head trauma among the football players.
It should be noted that in this prior era, concussions tended to be overlooked; medical documentation of head trauma likely captured only the most severe cases. The potential implications of concussions were unrecognized and likely, many footballers played after having their “bell rung”. The concept of subconcussions6 had not yet surfaced.
The rationale for this investigation was based on a growing literature indicating that repeated head trauma/concussions may cause subsequent irreversible neurological conditions.14,15 Early concerns were raised in the context of “dementia pugilistica”16 (or parkinsonism) as an outcome of boxing. Epidemiological studies have documented that a history of head trauma is associated with an increased later risk of dementia,1 Parkinson’s disease,8 and possibly ALS.17 Professional football players in the United States are at an increased risk of neurodegenerative diseases,18 and selected cases of dementia in the context of chronic traumatic encephalopathy have recently been publicized.5 Apparently, mortality due to neurodegenerative diseases among National Football League players is three times higher than that of the US general population; mortality from Alzheimer’s disease (AD) and ALS is 4 times higher.12
The present study confirms previous findings among high-school football players from the same community in the prior decade (1946–1956): dementia, parkinsonism and ALS incidences were similar in the football versus the control group.10 Note, however, that high school football from the period between 1956 and 1970 was likely more similar to the present era, including body weight, athletic performance and equipment. Nonetheless, the helmets and football rules from 1956–1970 were not optimally designed to protect the athletes; only in 1980 did the National Operating Committee on Standards for Athletic Equipment (NOCSAE) implement the first football-helmet standards.20 Moreover, spearing (leading with the head when blocking or tackling) was not prohibited until 1976. The major causes of football-related death between 1945 and 1999 was brain injury (69%), and most fatalities occurred from 1965 to 1969.21 With the adoption of NOCSAE standards, fatalities decreased by 74%.12
In comparison to the high school football players analyzed in the prior decade (1946–1956)10, high-school football players from 1956 to 1970 no longer used dog-ear or “leatherhead” helmets but rather more protective polyester helmets (Figure 2). However, helmets certainly do not eliminate concussions and may provide players with a false sense of protection, The 1956–1970 athletes were presumably bigger and generally more muscular than their 1946–1956 counterparts, whereas spearing was still allowed (i.e., striking with the head). Thus, better head protection could have had unintended consequences, making it ostensibly safer and less painful to strike opponents with the head.
Figure 2.

John Marshall High School players, circa 1968–69, wearing a more modern helmet. (John Marshall High School Yearbook, 1969; Courtesy of Rochester Public Schools and The History Center of Olmsted County)
This study should not be interpreted as evidence that football-related head trauma is benign. The literature on chronic traumatic encephalopathy among college and professional football players seems irrefutable, with reports of devastating outcomes. However, there may be a gradient of risk, with low potential among high school football players.
It should be noted that despite the mounting literature on the long-term consequences of head trauma in athletes, there are clear benefits of physical fitness on cardiovascular health and mortality.19 Indeed, studies have suggested a possible neuroprotective effect against neurodegenerative diseases, in particular dementia and Parkinson’s disease.8,9
Despite the merits of the study, there are a number of limitations. Unfortunately we were able to identify only 75% of students in our cohort using the REP, and in addition, we limited the definitive study population to the 30% for whom we have a prolonged medical record up to 2005. This could have led to selection bias; however, our method of case ascertainment was the same as we used in the previous study.10 In addition, we were unable to include information regarding the positions and the time spent on the field of the football players. Thus, we considered all players to be of equal likelihood to have been exposed to head trauma. We do not know whether any of the athletes continued to participate in contact sports after high school. A major limitation is the lack of power to detect the difference in neurodegenerative diseases between football players and non-football players (swimmers, basketball players or wrestlers). In fact, in order to obtain 809% of power we should need about 9000 students: our study is underpowered. Therefore, our findings should be interpreted cautiously.
The goal of this investigation was to study high-school athletes, not college or professional football players. The intensity of the game and the size and speed of college and professional football players is not at all comparable to football at the high-school level. Current evidence clearly attests to chronic traumatic encephalopathy risk among at least some college and professional football players.5
Conclusions
Our study does not support an association between playing high school football between 1956 and 1970 and risk of PD, dementia, and ALS. Additional studies are needed to explore more recent eras as well as involve players who participate at the collegiate and professional levels.
Acknowledgments
We would like to thank Dacy C. Lea for the formatting and editing support
Financial Support: This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Boeve reports personal fees from Scientific Advisory Board of the Tau Consortium and Isis Pharmaceuticals and grants from GE Healthcare, NIH, Mangurian Foundation, Cephalon, Inc., FORUM Pharmaceuticals, and C2N Diagnostics, all outside the submitted work. Dr. Mielke consults for Lysosomal Therapeutics, Inc., and holds a grant from the Michael J. Fox Foundation, both outside the submitted work. Mr. Janssen and Drs. Ahlskog, Joseph, Mandrekar, and Savica report no conflict of interest. Mr. Janssen completed the study while on leave from Radboud University.
References
- 1.Mortimer JA, van Duijn CM, Chandra V, Fratiglioni L, Graves AB, Heyman A, et al. Head trauma as a risk factor for Alzheimer’s disease: a collaborative reanalysis of case-control studies. EURODEM Risk Factors Research Group. Int J Epidemiol. 1991;20(Suppl 2):S28–35. doi: 10.1093/ije/20.supplement_2.s28. [DOI] [PubMed] [Google Scholar]
- 2.Bower JH, Maraganore DM, Peterson BJ, McDonnell SK, Ahlskog JE, Rocca WA. Head trauma preceding PD: a case-control study. Neurology. 2003;60(10):1610–1615. doi: 10.1212/01.wnl.0000068008.78394.2c. [DOI] [PubMed] [Google Scholar]
- 3.Vanacore N, Binazzi A, Bottazzi M, Belli S. Amyotrophic lateral sclerosis in an Italian professional soccer player. Parkinsonism & related disorders. 2006;12(5):327–329. doi: 10.1016/j.parkreldis.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Gardner RC, Yaffe K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci. 2015;66(Part B):75–80. doi: 10.1016/j.mcn.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKee AC, Stern RA, Nowinski CJ, Stein TD, Alvarez VE, Daneshvar DH, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136(Pt 1):43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McAllister TW, Ford JC, Flashman LA, Maerlender A, Greenwald RM, Beckwith JG, et al. Effect of head impacts on diffusivity measures in a cohort of collegiate contact sport athletes. Neurology. 2014;82(1):63–69. doi: 10.1212/01.wnl.0000438220.16190.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albin RL, Edlow BL, Rosenthal ES, Hinson HE. Blowing the whistle on sports concussions: Will the risk of dementia change the game? Neurology. 2016;86(20):1929–1930. doi: 10.1212/01.wnl.0000484015.90990.ab. [DOI] [PubMed] [Google Scholar]
- 8.Ahlskog JE. Does vigorous exercise have a neuroprotective effect in Parkinson disease? Neurology. 2011;77(3):288–294. doi: 10.1212/WNL.0b013e318225ab66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahlskog JE, Geda YE, Graff-Radford NR, Petersen RC. Physical exercise as a preventive or disease-modifying treatment of dementia and brain aging. Mayo Clin Proc. 2011;86(9):876–884. doi: 10.4065/mcp.2011.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Savica R, Parisi JE, Wold LE, Josephs KA, Ahlskog JE. High school football and risk of neurodegeneration: a community-based study. Mayo Clin Proc. 2012;87(4):335–340. doi: 10.1016/j.mayocp.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011;173(9):1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., III History of the Rochester Epidemiology Project: Half a Century of Medical Records Linkage in a US Population. Mayo Clin Proc. 2012;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med. 2011;30(1):179–188. xi. doi: 10.1016/j.csm.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goodwin L. Dementia pugilistica. J Insur Med. 2006;38(4):300–302. [PubMed] [Google Scholar]
- 17.Chio A, Benzi G, Dossena M, Mutani R, Mora G. Severely increased risk of amyotrophic lateral sclerosis among Italian professional football players. Brain. 2005;128(Pt 3):472–476. doi: 10.1093/brain/awh373. [DOI] [PubMed] [Google Scholar]
- 18.Abel EL. Football increases the risk for Lou Gehrig's disease, amyotrophic lateral sclerosis. Percept Mot Skills. 2007;104(3 Pt 2):1251–1254. doi: 10.2466/pms.104.4.1251-1254. [DOI] [PubMed] [Google Scholar]
- 19.Kokkinos P. Physical activity, health benefits, and mortality risk. ISRN Cardiol. 2012;2012:718789. doi: 10.5402/2012/718789. Available at http://www.hindawi.com/journals/isrn/2012/718789/ Accessed June 23, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clarke KS, Powell JW. Football helmets and neurotrauma–an epidemiological overview of three seasons. Med Sci Sports. 1979;11(2):138–145. [PubMed] [Google Scholar]
- 21.Levy ML, Ozgur BM, Berry C, Aryan HE, Apuzzo ML. Analysis and evolution of head injury in football. Neurosurgery. 2004;55(3):649–655. doi: 10.1227/01.neu.0000134598.06114.89. [DOI] [PubMed] [Google Scholar]


