Abstract
Dural arteriovenous fistula (DAVF) in a sinus of the lesser sphenoid wing (SLSW) is rarely reported. Here, we report a case of an isolated SLSW DAVF treated by coils placed into the sinus through the feeding artery. A 68-year-old man was admitted to our hospital with headache. Magnetic resonance images and an angiogram showed a varix in the right middle cranial fossa. A DAVF, consisting of three main feeders and the isolated SLSW, was diagnosed based on the angiogram findings. Retrograde leptomeningeal venous drainage to the deep middle cerebral vein was observed. Given the remarkable extent of cortical venous ectasia together with the presence of headache and right abducens nerve paralysis, endovascular treatment was initiated. A transvenous approach through the right inferior petrosal sinus was not feasible because of difficulty associated with inserting the microcatheter into the SLSW. Thus, we tried a transarterial approach and were able to advance the microcatheter beyond the fistula into the isolated SLSW, through the artery of the foramen rotundum. The isolated sinus and feeding arteries were embolized with coils. The postoperative angiogram showed the total occlusion of the SLSW DAVF. This case demonstrates the feasibility of transarterial sinus packing for an isolated SLSW DAVF.
Keywords: dural arteriovenous fistula, transarterial sinus embolization, sinus of the lesser sphenoid wing, coil embolization
Introduction
Dural arteriovenous fistula (DAVF) in a sinus of the lesser sphenoid wing (SLSW) is rarely reported. The primary therapeutic strategies for a DAVF in this region currently consist of transarterial embolization (TAE) and transvenous embolization (TVE).1,2) If the DAVF cannot be cured by such endovascular treatment, direct surgery may be required.1)
TVE is generally a curative treatment for a DAVF. However, a transvenous approach to a SLSW is not always achievable because of the limited access route.2) In such cases, TAE is the accepted therapeutic alternative.3,4) TAE typically involves the occlusion of the feeding arteries, fistula, sinus, and outlet of the cortical vein using embolic materials, such as n-butyl 2-cyanoacrylate, coils, or the Onyx Liquid Embolic System (ev3 Neurovascular, Irvine, CA, USA), from the arterial side.3,4) However, there are few reports in the literature of transarterial sinus packing with coils, in which the microcatheter is passed through the fistula and placed in the sinus.
Here, we present the first case of an isolated SLSW DAVF treated with coils transarterially.
Case Report
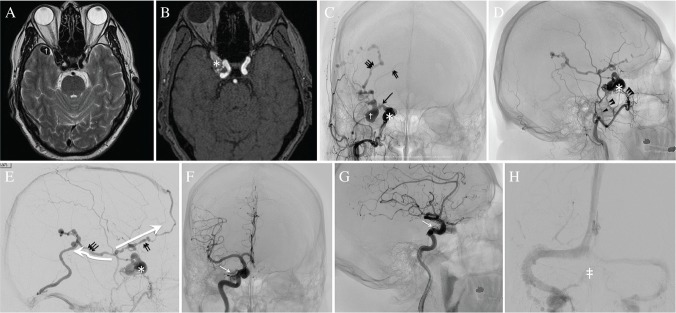
A 68-year-old man was admitted to our hospital because his magnetic resonance (MR) images and angiogram showed a varix in the right middle cranial fossa (Figs. 1A and 1B). Based on the angiogram findings, he was diagnosed with an isolated SLSW DAVF (Figs. 1C–1H). There were three main feeders from the right external carotid artery (ECA), comprising the accessory meningeal artery (AMA), middle meningeal artery (MMA), and artery of the foramen rotundum (AFR) (Fig. 1D). In addition, some small feeders from the meningohypophyseal trunk (MHT) and ophthalmic artery were observed on his right internal carotid angiogram (ICAG) (Figs. 1F and 1G). On the venous side (Fig. 1E), retrograde leptomeningeal venous drainage (RLVD) was first observed from the right SLSW to the right deep middle cerebral vein (DMCV) via a bridging vein. Second, the RLVD from the DMCV was drained with venous ectasia, into the frontal cortical vein and then the superior sagittal sinus (SSS) anteriorly, and into the posterior insular vein and then the transverse sinus (TS) through the temporal cortical vein posteriorly. No connection between the SLSW and the cavernous sinus (CS) or middle meningeal vein was observed. The ICAG showed that the right CS and inferior petrosal sinus (IPS) were patented in the late venous phase (Figs. 1F–1H). Given the remarkable ectasia of the draining vein, accompanied by the presence of headache as well as right abducens nerve paralysis, endovascular treatment was initiated.
Fig. 1.
MR images (A, B), external carotid angiograms (C–E) and internal carotid angiograms (F–H) before endovascular treatment. A T2-weighted (A) and time-of-flight (B) MR images show a varix (dagger) in the right middle cranial fossa and dural arteriovenous fistula (DAVF) in a lesion at a lateral location of the cavernous sinus (asterisk). (C, D, E) The right external carotid angiogram (ECAG) reveals a DAVF in a sinus of the lesser sphenoid wing (SLSW) (asterisk), the retrograde leptomeningeal venous drainage (RLVD) with the varix (dagger) and cortical venous ectasia, and three main feeders; middle meningeal artery (arrowhead), the accessory meningeal artery (double arrowhead), and artery of the foramen rotundum (triple arrowhead). The right ECAG in the late venous phase shows the RLVD from the isolated SLSW to the deep middle cerebral vein (DMCV) via a bridging vein (arrow). The RLVD from the DMCV is drained into two routes (large white arrows), comprising the frontal cortical vein (double arrow) and posterior insular vein (triple arrow) with venous ectasia. The frontal cortical vein is connected to the superior sagittal sinus. The posterior insular vein is finally drained into the transverse sinus through the temporal cortical vein. (F, G) The right ICAG in the arterial phase shows some small feeders from the meningohypophyseal trunk and ophthalmic artery (white arrow). (H) The right ICAG in the venous phase reveals the patent right cavernous sinus (double dagger) and inferior petrosal sinus.
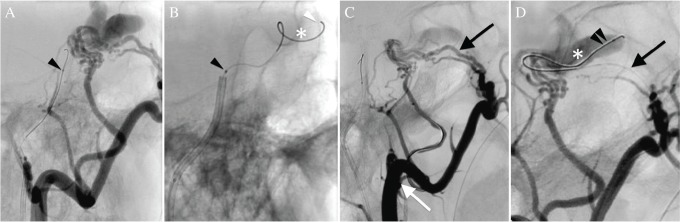
Initially, a transvenous approach via the IPS was tried. While a 5Fr ENVOY (Johnson & Johnson, Miami, FL, USA) guiding catheter could be placed in the proximal right IPS, and a microguidewire, either ASAHI CHIKAI Black (ASAHI INTECC, Nagoya, Japan) or GT WIRE (Terumo, Tokyo, Japan), could be placed in the SLSW (Fig. 2A) through the CS (probably passing through the occluded venous connection between the CS and SLSW), none of the tested microcatheters, e.g., Excelsior SL-10STR (Stryker, Kalamazoo, MI, USA) and Headway 17 (Terumo, Tokyo, Japan), could be advanced into the SLSW (Fig. 2B). Therefore, this approach failed. A contralateral IPS approach also failed. Thus, as an alternative to TVE, we tried a transarterial approach (Fig. 2C).
Fig. 2.
The lateral view of the right external carotid angiograms (ECAG) during the endovascular treatment. (A) A Headway 17 microcatheter (arrowhead) was navigated into the IPS with a GT microguidewire for the transvenous embolization. (B) It was not achievable to introduce any microcatheters into the sinus of the lesser sphenoid wing (SLSW) (arrowhead) along the microguidewire (white arrowhead) in the SLSW (asterisk) (C) A 6Fr FUBUKI guiding catheter was placed in the internal maxillary artery (white arrow) for transarterial embolization through the artery of the foramen rotundum (AFR) (arrow). (D) The SL-10 microcatheter (double arrowhead) was easily advanced beyond the fistula into the SLSW (asterisk) through the AFR (arrow).
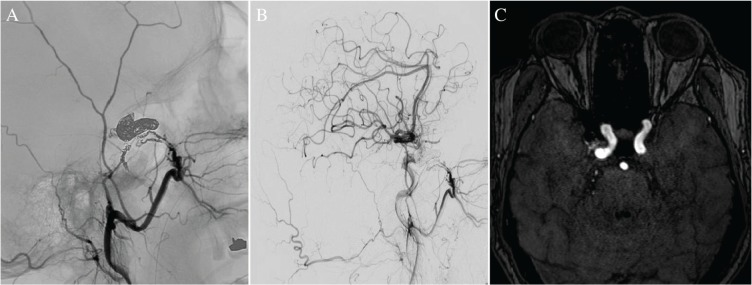
A 6Fr FUBUKI (ASAHI INTECC) guiding catheter was placed in the internal maxillary artery, and an Excelsior SL-10STR (Stryker) was placed into the AFR. A CHIKAI 14 (ASAHI INTECC) microguidewire was then easily passed through the fistula into the isolated SLSW. The SL-10 microcatheter was also advanced beyond the fistula into the isolated SLSW without difficulty (Fig. 2D). The isolated sinus could be embolized with coils. Before complete sinus packing, the SL-10 microcatheter was pushed back in the AFR. Subsequently, there was a slight residual shunt flow in the ECA angiogram. Therefore, the other feeding arteries were additionally occluded with coils (Fig. 3A). The post-embolization angiogram showed the total occlusion of the SLSW (Fig. 3B). After the treatment, the shunt was completely obliterated (Fig. 3C) and no neurological complications were detected.
Fig. 3.
(A) The right external carotid angiogram after sinus embolization (lateral) shows the coil mass in the isolated cavernous sinus and the feeding arteries. (B) The right common carotid angiogram after treatment (lateral) shows total occlusion of the fistula. (C) The postoperative time-of-flight magnetic resonance image confirms the disappearance of the shunt.
Discussion
A SLSW is located under the lesser sphenoid wing, and is stated to be a part of the sphenoparietal sinus.5) It was reported that the incidence rate of SLSW DAVF was 1.54% of all intracranial DAVFs, and suggested that the diagnosis of an SLSW DAVF might be difficult because it could be easily confused with a cavernous sinus DAVF.1)
In our case, the ICAG showed normal venous drainage from the right CS to the IPS in the late venous phase (Fig. 1H), indicating that the CS was not involved in the abnormal venous drainage. In addition, the time-of-flight MR images and ECAG showed that the affected sinus was lateral to the CS (Figs. 1B and 1C). Therefore, we diagnosed SLSW DAVF.
The treatment options for SLSW DAVF have been described in previous reports, and include TAE, TVE, surgical obliteration, and their combinations.1,2,6,7) TVE is the primary therapeutic strategy for the curative treatment of DAVF. However, it was reported that a transvenous approach to an SLSW via the IPS and CS is often impossible because the connection site between the CS and SLSW is not straight.2) As mentioned earlier, a transvenous approach via the IPS and CS failed because of a disconnection between the CS and SLSW in our case. If it is impossible to approach the affected sinus via the IPS, it is necessary to consider the use of another venous access route, such as the facial vein.2,8),9) However, in our case, we could not choose this strategy because there were no other extracranial drainage routes from the affected sinus. Thus, we ceased the TVE.
In cases where TVE is not achievable, TAE can be considered as an alternative strategy.3,4) TAE is a less curative treatment than TVE, because it mostly results in the occlusion of the feeding artery with a residual arteriovenous shunt.3) However, if the microcatheter can be placed in the affected sinus beyond the fistula and complete sinus packing can be achieved, the curative effect is expected to be equal to that of TVE. In our case, the microcatheter could be inserted into the SLSW fortunately, and transarterial “sinus” embolization (TASE) was carried out. In this procedure, control of the microcatheter was difficult in the affected sinus because the microcatheter shaft was placed in a narrow fistula, and it was not possible to achieve complete sinus packing by TASE alone. Accordingly, the microcatheter tip was pushed back on the arterial side before complete sinus packing, and the embolization of the feeding arteries needed to be added, similar to conventional TAE. This may be a difficult point in the performance of TASE.
It was previously reported that fistulas generally range from 30 to 200 μm.10,11) However, microcatheters with diameters ranging from 430 to 830 μm were successfully introduced through fistula sites in the previous reports involving TASE (Table 1).12–19) These findings suggest that the fistula associated with a DAVF is sometimes larger than the previously reported size range, and that in such cases the microcatheter can be advanced into the venous side transarterially. Successful transarterial catheterization through the fistula might depend on the less tortuous nature of the feeding arteries and the large size of the fistula.12,14) It was also suggested that if a feeding artery shows distal enlargement, a larger fistula might exist and TASE may be feasible.18) The most common pathway for TASE was the MMA in previous cases (10/12, 83%), and the reason for the successful catheterization via the MMA may be related to its relatively large size and straight running path, as compared with other feeding arteries.18) In our case, TASE was fortunately performed via the AFR, and this was dependent on the relatively larger size and straight shape of this artery.
Table 1.
Summary of the 12 cases of transarterial sinus embolization using coils previously reported in the literature
| First author and year | Number | Location | Feeder | Microcatheter | Outside diameter of microcatehter tip (mm) |
|---|---|---|---|---|---|
| Fukai, 200112) | 1 | SSS | MMA | Prowler-14 | 0.63 |
| Tokunaga, 200313) | 2 | TS-SS | MMA | Excel-14 | 0.63 |
| Kiyosue, 200414) | 3 | SSS | MMA | NA | NA |
| Layton, 200615) | 4 | Tentorium | MMA | Echelon 10 | 0.56 |
| 5 | Vein of Galen | MMA | Echelon 10 | 0.56 | |
| Shiragami, 200916) | 6 | TS-SS | MMA | Renegade | 0.83 |
| Ohara, 201217) | 7 | SSS | MMA | Marathon | 0.5 |
| Baik, 201418) | 8 | SSS | MMA | NA | 0.56–0.63 |
| 9 | CS | MMA | NA | 0.56–0.63 | |
| 10 | SS | MMA | NA | 0.56–0.63 | |
| 11 | SS | MHT | NA | 0.56–0.63 | |
| Yamauchi, 201519) | 12 | CS | AMA | Headway 17 | 0.43 |
| Present case | 13 | SLSW | AFR | Excelsior SL-10 | 0.56 |
AFR: artery of the foramen rotundum, AMA: accessory meningeal artery, CS: cavernous sinus, MHT: meningohypophyseal trunk, MMA: middle meningeal artery, SLSW: sinus of the lesser sphenoid wing, SS: sigmoid sinus, SSS: superior sagittal sinus, TS-SS: transverse-sigmoid sinus.
Conclusion
We have reported a case of SLSW DAVF treated with TASE. TASE might be an additional treatment option for a DAVF associated with a large and straight feeding artery.
Footnotes
Conflicts of Interest Disclosure
The authors declare that there are no conflicts of interest.
References
- 1). Shi ZS, Ziegler J, Feng L, Gonzalez NR, Tateshima S, Jahan R, Martin NA, Viñuela F, Duckwiler GR: Middle cranial fossa sphenoidal region dural arteriovenous fistulas: anatomic and treatment considerations. AJNR Am J Neuroradiol 34: 373– 380, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Kim MJ, Shin YS, Ihn YK, Kim BM, Yoon PH, Oh SY, Kim BS: Transvenous embolization of cavernous and paracavernous dural arteriovenous fistula through the facial vein: report of 12 cases. Neurointervention 8: 15– 22, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Luo CB, Chang FC, Teng MM: Update of embolization of intracranial dural arteriovenous fistula. J Chin Med Assoc 77: 610– 617, 2014. [DOI] [PubMed] [Google Scholar]
- 4). Vanlandingham M, Fox B, Hoit D, Elijovich L, Arthur AS: Endovascular treatment of intracranial dural arteriovenous fistulas. Neurosurgery 74 Suppl 1: S42– S49, 2014. [DOI] [PubMed] [Google Scholar]
- 5). San Millán Ruíz D, Fasel JH, Rüfenacht DA, Gailloud P: The sphenoparietal sinus of breschet: does it exist? An anatomic study. AJNR Am J Neuroradiol 25: 112– 120, 2004. [PMC free article] [PubMed] [Google Scholar]
- 6). Rezende MT, Piotin M, Mounayer C, Spelle L, Abud DG, Moret J: Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: technical note. Neuroradiology 48: 130– 134, 2006. [DOI] [PubMed] [Google Scholar]
- 7). Macdonald A, Plaha P, Byrne J: An unusual presentation of a dural arteriovenous fistula of the sphenoparietal sinus. J Neurointerv Surg 7: e12, 2015. [DOI] [PubMed] [Google Scholar]
- 8). Singh J, Morris P: Superficial temporal vein: route to embolization of cavernous dural arteriovenous fistula. J Neuroimaging 21: 251– 254, 2011. [DOI] [PubMed] [Google Scholar]
- 9). White JB, Layton KF, Evans AJ, Tong FC, Jensen ME, Kallmes DF, Dion JE, Cloft HJ: Transorbital puncture for the treatment of cavernous sinus dural arteriovenous fistulas. AJNR Am J Neuroradiol 28: 1415– 1417, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Hamada Y, Goto K, Inoue T, Iwaki T, Matsuno H, Suzuki S, Matsushima T, Fukui M, Miyake E: Histopathological aspects of dural arteriovenous fistulas in the transverse-sigmoid sinus region in nine patients. Neurosurgery 40: 452– 458, 1997. [DOI] [PubMed] [Google Scholar]
- 11). Nishijima M, Takaku A, Endo S, Kuwayama N, Koizumi F, Sato H, Owada K: Etiological evaluation of dural arteriovenous malformations of the lateral and sigmoid sinuses based on histopathological examinations. J Neurosurg 76: 600– 606, 1992. [DOI] [PubMed] [Google Scholar]
- 12). Fukai J, Terada J, Kuwata T, Hyotani G, Raimura M, Nakagawa M, Yabumoto M, Kamei I: Transarterial intravenous coil embolization of dural arteriovenous fistula involving the superior sagittal sinus. Surg Neurol 55: 353– 358, 2001. [DOI] [PubMed] [Google Scholar]
- 13). Tokunaga K, Barath K, Martin J, Rüfenacht DA: Transarterial approach for selective intravenous coil embolization of a benign dural arteriovenous fistula. Case report. J Neurosurg 99: 775– 778, 2003. [DOI] [PubMed] [Google Scholar]
- 14). Kiyosue H, Okahara M, Matsumoto S, Hori Y, Yamashita M, Nagatomi H, Mori H: Coil embolization of superior sagittal sinus dural arteriovenous fistula by transarterial intrasinus catheterization. Cardiovasc Intervent Radiol 27: 405– 407 2004. [DOI] [PubMed] [Google Scholar]
- 15). Layton KF, Nelson MD, Kallmes DF: Transarterial coil embolization of the venous component of aggressive type 4 dural arteriovenous fistulas. AJNR Am J Neuroradiol 27: 750– 752, 2006. [PMC free article] [PubMed] [Google Scholar]
- 16). Shiragami T, Takada H, Akai T, Yamamoto K, Iida T, Okamoto K, Iizuka H: Sinus coil embolization for dural arteriovenous fistula by trans-arterial approach: a case report. Nousotchu 32: 68– 73, 2010. (Japanese) [Google Scholar]
- 17). Ohara N, Toyota S, Kobayashi M, Wakayama A: Superior sagittal sinus dural arteriovenous fistula treated by stent placement for an occluded sinus and transarterial embolization: A case report. Intervent Neuroradiol 18: 333– 340, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18). Baik SK, Kim YW, Lee SW, Choi CH, Park J: A treatment option for nontraumatic adult-type dural arteriovenous fistulas: transarterial venous coil embolization. World Neurosurg 82, 417– 422, 2014. [DOI] [PubMed] [Google Scholar]
- 19). Yamauchi T, Koguchi Y, Matsuura I, Kijima Y, Aikawa M, Suzuki K, Miyata A, Kobayashi S: Transarterial embolization with coils via accessory meningeal artery for the cavernous sinus dual arteriovenous fistula: a case report. J Neuroendovasc Ther 9: 31– 36, 2015. (Japanese) [Google Scholar]