Abstract
Objective
To describe guideline adherence for patients with suspected upper tract stones.
Methods
We performed a cross-sectional analysis of visits recorded by the National Hospital Ambulatory Medical Care Survey (ED component) in 2007–2010 (most recent data). We assessed adherence to clinical guidelines for diagnostic laboratory testing, imaging, and pharmacologic therapy. Multivariable regression models controlled for important covariates.
Results
An estimated 4,956,444 ED visits for patients with suspected kidney stones occurred during the study period. Guideline adherence was highest for diagnostic imaging, with 3,122,229 (63%) visits providing optimal imaging. Complete guideline-based laboratory testing occurred in only 2 of every 5 visits. Pharmacologic therapy to facilitate stone passage was prescribed during only 17% of eligible visits. In multivariable analysis of guideline adherence, we found little variation by patient, provider or facility characteristics.
Conclusions
Guideline-recommended care was absent from a substantial proportion of acute care visits for patients with suspected kidney stones. These failures of care delivery likely increase costs and temporary disability. Targeted interventions to improve guideline adherence should be designed and evaluated to improve care for patients with symptomatic kidney stones.
Keywords: kidney stones, quality of care, emergency care, guidelines
Introduction
Kidney stones impose a large and rising burden of disease in the United States: their prevalence has nearly doubled over the past 15 years, and stone disease now affects 1 of every 11 persons.1,2 Kidney stones occur primarily in a working age population, and up to 50% of patients experience a recurrence.3,4 Stones are among the most costly urologic conditions in terms of aggregate direct costs, in addition to the indirect costs of work loss and temporary disability from pain.4,5
Extreme pain often causes patients to seek care in the emergency department (ED). Coincident with the rising prevalence of stone disease, the rate of ED visits for kidney stones has increased by 91% over 1992–1994 baseline.6 Initial acute care is provided primarily by non-urologists.7 Given rising acute care visits by patients with symptomatic stones, and the gateway role for further intervention that the ED serves, understanding quality of this acute care is critical.
One potential measure of quality is adherence to published, evidence-based guidelines. Current guidelines suggest that patients should be assessed for signs of sepsis or renal failure, each of which is an indication for urgent intervention.8 Patients with bacteriuria should be empirically treated with antibiotics to prevent urosepsis.8 The most sensitive initial imaging modality for most patients is non-contrast computerized tomography (CT), which serves to confirm the clinical diagnosis and determine prognosis for passage of the stone.9,10 For appropriately selected patients, a trial of pharmacologic medical expulsive therapy (MET) is recommended; randomized controlled trials suggest that this will obviate 1 surgical intervention for every 4 patients treated.11
The few existing analyses of acute care for patients with suspected kidney stones focus primarily on broad utilization patterns, rather than guideline adherence.6,12–14 Prior analyses of MET utilization examined data collected prior to guideline endorsement,15 or did not explore factors associated with utilization of MET.6 Given this context, we sought to assess adherence to guidelines for acute care of patients with suspected kidney stones. Specifically, we sought to characterize guideline adherence in the areas of laboratory testing, imaging, and use of MET, and to describe variation in guideline-adherent care delivery.
Patients and Methods
Data Source
We used data from the Emergency Department component of the National Hospital Ambulatory Medical Care Survey (NHAMCS-ED). The NHAMCS is a multistage probability survey of outpatient and emergency department encounters at non-federal hospitals located in all 50 states and the District of Columbia.16 The survey is designed to produce nationally representative estimates of ED encounters in the United States; each observed (unweighted) visit (n=1341) is weighted according to National Center for Health Statistics (NCHS) procedures to generate national estimates.16 De-identified data for each sampled visit include patient demographics, diagnoses, services, medications prescribed, and disposition. The institutional review board determined that this study was exempt from review.
Study Population
The study population consisted of all visits for patients with suspected kidney stones between 2007 and 2010 (most recent data available). We used established claims algorithms based on International Classification of Disease 9th edition (ICD-9) diagnostic codes to identify patients with encounters for kidney stones.15,17 Patients younger than 18 years of age were excluded.
Outcomes
To assess guideline adherence, we examined three discrete outcomes implicit in current guidelines (see eMethods). We defined adherence with laboratory testing guidelines as an encounter where a patient underwent a complete blood count (assess for signs of sepsis8), measurement of serum creatinine (assess renal function8) and urinalysis (assess for bacteriuria).8 We measured adherence to imaging guidelines9 by the performance of a CT scan during the visit. As a pre-specified sensitivity analysis, we identified visits in which an ultrasound or plain x-ray was performed; guidelines suggest these may be appropriate in certain circumstances.9 We identified MET utilization as prescription of an alpha-blocker or a calcium channel blocker, using established algorithms for this dataset.6,15 We excluded ineligible patients using established algorithms.6,15 As a pre-specified sensitivity analysis, we repeated the analysis only among those with a highly specific ICD-9 code (592.1) for ureteral stones.18 No patients in the MET cohort were admitted to hospital or underwent procedural intervention.
Covariates
A number of factors could potentially be associated with provision of guideline-adherent care. Patient-level covariates included age and sex. The prevalence of kidney stones varies importantly by race and ethnicity.2 For this reason, and in accordance with National Center for Health Statistics (NCHS) analytic guidelines regarding sample size,16 we classified race and ethnicity as reported by NHAMCS into three groups: white non-Hispanic, Hispanic, and other. Payer type was recoded as private, Medicare, Medicaid, and self/other. We included arrival by ambulance transport. Quartiles of household income, percent of population in poverty, and percent of adults with a bachelor’s degree or higher in the patient’s ZIP code served as a proxy for socioeconomic status.
We created an indicator variable for whether the patient was seen by a non-physician provider (i.e., nurse practitioner). Facility-level covariates included teaching status and ownership. Given the known geographic variation in stone prevalence,1 we included region as a covariate. In addition, we used an indicator variable to identify hospitals located in metropolitan areas. To identify potential changes in guideline adherence over time, we included survey year as a covariate.
To examine potential associations between health information technology and care delivery, we included indicators for whether the ED had computerized systems to provide reminders about guideline-based interventions, as well as an indicator variable for a computerized lab ordering system. At the time of our analysis, these data elements for the 2010 survey were not yet publically available. Therefore, we limited this analysis to the 2007–2009 data and a priori designated this as a secondary analysis.
Statistical Analysis
Using NCHS-recommended design and weighting variables, we calculated nationally representative estimates of the percent of encounters that provided guideline-adherent care. All results are reported as nationally representative (weighted) estimates unless otherwise specified. We constructed logistic regression models for each of the three outcomes (laboratory testing, imaging and MET use) to identify associations between provision of guideline-adherent care and patient, provider, hospital and geographic area covariates, accounting for the complex survey sample design. Regression models for laboratory testing and imaging included age, sex, race, payer, arrival by ambulance, non-physician provider, teaching status, hospital ownership, region, year, education level, household income, poverty level, and metropolitan status. Due to the smaller number of eligible subjects and NCHS analytic guidelines regarding cell size, only patient age, sex, region household income and education were included in the MET guideline adherence regression model. We performed several sensitivity analyses to address potential selection bias from cohort identification (eMethods). In no case did the proportion of visits including guideline-adherent care differ substantively from the main analysis. We used SAS 9.2 (Cary, NC) for all analyses. Results were considered statistically significant with two-sided α = 0.05.
Results
An estimated 4,956,444 ED visits nationally occurred between 2007 and 2010. Visits for patients eligible for MET constituted 4,214,570 (85%) estimated national ED visits for kidney stones. The average age of the patients was 43.2 ± 0.58 years and males comprised 55% of the study population (Table 1).
Table 1.
Characteristics of Study Population
| Characteristic | Unweighted N | Weighted N (%) |
|---|---|---|
| Age, mean (SD) | -- | 43.2 (0.58) |
| Sex | ||
| Male | 741 | 2733333 (55) |
| Female | 600 | 2223111 (44) |
| Race/ethnicity | ||
| White, Non-Hispanic | 1045 | 3910766 (79) |
| Hispanic | 153 | 501395 (10) |
| Black/Other, Non-Hispanic | 143 | 544283 (10) |
| Primary Payer | ||
| Private | 687 | 2655266 (56) |
| Medicare | 154 | 572476 (12) |
| Medicaid | 170 | 556907 (12) |
| Self-pay/other | 261 | 934213 (20) |
| Region | ||
| Northeast | 290 | 872739 (18) |
| Midwest | 310 | 1127245 (23) |
| South | 492 | 2001262 (40) |
| West | 249 | 955198 (19) |
| Year | ||
| 2007 | 355 | 1243701 (25) |
| 2008 | 310 | 1226116 (25) |
| 2009 | 339 | 1311817 (26) |
| 2010 | 337 | 1174810 (24) |
| Educationa | ||
| Quartile 1 | 371 | 1445058 (31) |
| Quartile 2 | 298 | 1127320 (24) |
| Quartile 3 | 316 | 1095093 (24) |
| Quartile 4 | 287 | 968250 (21) |
| Household Income | ||
| Quartile 1 | 300 | 1138142 (25) |
| Quartile 2 | 307 | 1094107 (24) |
| Quartile 3 | 347 | 1292451 (28) |
| Quartile 4 | 318 | 1111021 (24) |
| Poverty Level in ZIP | ||
| < 5% | 274 | 1001206 (22) |
| 5–9.99% | 400 | 1455914 (31) |
| 10–19.99% | 401 | 1413158 (30) |
| ≥ 20% | 197 | 765443 (17) |
| MSA | ||
| No | 187 | 852158 (17) |
| Yes | 1154 | 4104286 (83) |
% adults with Bachelor’s degree in patient’s ZIP code, quartile
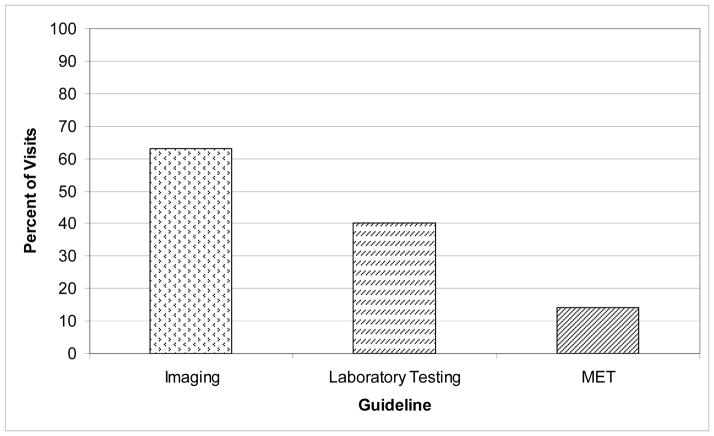
The degree to which clinical care was adherent to current guidelines varied widely depending on the guideline of interest (Figure, Table 2). Imaging guideline adherence was highest, with 63% of visits including a CT scan. Only 2 of every 5 visits included all guideline-based laboratory testing. MET utilization was very low, with only 14% of eligible visits resulting in prescription of MET to patients discharged from the ED. Similar results were obtained when restricting the analysis to only patients with a primary diagnosis of stone, as well as the subpopulation with only a diagnostic code for ureteral stone (eMethods).
Figure.
Nationally representative percentage of emergency department visits with documentation of guideline-adherent care, 2007–2010.
Table 2.
Nationally representative visits with provision of guideline-adherent care among patients with suspected kidney stone (univariate analysis).
| Characteristic | Laboratory Testing | P Value (Labs) | Imaging | P Value (Imaging) | Medical Expulsive Therapy | P Value (MET) |
|---|---|---|---|---|---|---|
| Overall | 1957851 (40) | -- | 3122229 (63) | -- | 570060 (14) | -- |
| Sex | ||||||
| Male | 1083744 (40) | 0.93 | 1796672 (66) | 0.04 | 413640 (17) | <0.001 |
| Female | 874107 (39) | 1325557 (60) | 156420 (9) | |||
| Race/ethnicity | ||||||
| White, Non-Hispanic | 1586552 (41) | 2502077 (64) | 468174(14) | |||
| Hispanic | 180062 (36) | 0.50 | 318810 (55) | 0.37 | a | -- |
| Black/Other, Non-Hispanic | 191237 (35) | 301342 (64) | a | |||
| Primary Payer | ||||||
| Private | 989881 (37) | 1723633 (65) | 376442 (17) | |||
| Medicare | 247181 (43) | 0.64 | 349162 (61) | 0.78 | a | -- |
| Medicaid | 236513 (42) | 335773 (60) | a | |||
| Self-pay/other | 374774 (40) | 590113 (63) | a | |||
| Arrived by EMS | ||||||
| No | 1722880 (39) | 0.68 | 2738400 (63) | 0.44 | 520305 (14) | -- |
| Yes | 165578 (42) | 268450 (68) | a | |||
| Physician Extender Seen | ||||||
| No | 1738589 (39) | 0.33 | 2784148 (62) | 0.32 | 476270 (13) | -- |
| Yes | 219262 (44) | 338081 (68) | a | |||
| Teaching Status | ||||||
| No | 1776968 (39) | 0.42 | 2837503 (62) | 0.30 | 519321 (13) | -- |
| Yes | 180883 (44) | 284726 (69) | a | |||
| Ownership status | ||||||
| Voluntary non-profit | 1542097 (40) | 2435064 (64) | 448649 (14) | |||
| Government, non-federal | 222555 (42) | 0.31 | 326393 (61) | 0.81 | a | -- |
| Proprietary | 193199 (33) | 360772 (60) | a | |||
| Region | ||||||
| Northeast | 398652 (46) | 563439 (65) | 102389 (14) | |||
| Midwest | 486608 (43) | 0.03 | 769342 (68) | 0.40 | 152627 (17) | 0.57 |
| South | 797775 (40) | 1218130 (61) | 229834 (13) | |||
| West | 274816 (29) | 571318 (60) | 85210 (10) | |||
| Year | ||||||
| 2007 | 507584 (41) | 734217 (59) | a | |||
| 2008 | 478792 (39) | 0.53 | 789569 (64) | 0.39 | 129657 (13) | -- |
| 2009 | 463739 (35) | 804220 (61) | 175414 (16) | |||
| 2010 | 507736 (43) | 794223 (68) | 197120 (20) | |||
| Educationb | ||||||
| Quartile 1 | 504392 (35) | 870354 (60) | 139974 (11) | |||
| Quartile 2 | 503030 (45) | 0.23 | 714568 (63) | 0.72 | 129651 (14) | 0.82 |
| Quartile 3 | 412890 (38) | 726009 (66) | 121007 (13) | |||
| Quartile 4 | 412295 (43) | 625283 (65) | 123134 (15) | |||
| Household Income | ||||||
| Quartile 1 | 433027 (38) | 637187 (56) | 104273 (10) | |||
| Quartile 2 | 435424 (40) | 0.98 | 712343 (65) | 0.16 | 134708 (15) | 0.68 |
| Quartile 3 | 514344 (40) | 836659 (65) | 147288 (14) | |||
| Quartile 4 | 449812 (40) | 750025 (68) | 127497 (13) | |||
| Poverty Level in ZIP | ||||||
| < 5% | 439730 (44) | 667829 (67) | 127260 (15) | |||
| 5–9.99% | 551827 (38) | 0.60 | 987029 (68) | 0.12 | 163741 (13) | -- |
| 10–19.99% | 562922 (40) | 847981 (60) | 130764 (11) | |||
| ≥ 20% | 278128 (36) | 433375 (67) | a | |||
| MSA | ||||||
| No | 254588 (30) | 0.02 | 427876 (50) | 0.002 | 516492 (15) | -- |
| Yes | 1703263 (41) | 2694353 (66) | a |
Too few unweighted observations for reliable estimate per NCHS analytic guidelines. -- indicates no statistical hypothesis test performed due to NCHS guidelines.
% adults with Bachelor’s degree in patient’s ZIP code, quartile
Laboratory Testing
Overall, 40% of ED visits included the provision of all three guideline-recommended laboratory tests. For each individual test, utilization varied widely. Patients underwent urinalysis at 85% of visits. Renal function was assessed at 47% of visits, whereas a complete blood count was performed at 68% of visits. Guideline adherence was not substantially different in the sensitivity analyses.
On multivariable analysis, there was little variation in the odds of a patient undergoing guideline-adherent laboratory testing at a visit (Table 3). As age increased, the odds of undergoing laboratory testing increased (OR 1.01 per year, P = 0.04), but there were no statistically significant differences in testing by gender, race/ethnicity, payer, or measures of socioeconomic status (Table 3). Similarly, provider and facility characteristics were not associated with the receipt of guideline-adherent laboratory testing. Visits to hospitals within a metropolitan statistical area were more likely to include guideline-adherent testing (OR 1.82, P = 0.008).
Table 3.
Association between patient, provider and facility characteristics and receipt of guideline-adherent care at visit, multivariable model (nationally representative estimates).
| Characteristic | Laboratory Testing Odds Ratio (95% CI) |
P Value | Imaging Odds Ratio (95% CI) |
P Value |
|---|---|---|---|---|
| Age | 1.01 (1.00—1.02) | 0.04 | 1.00 (0.99—1.01) | 0.93 |
| Sex | ||||
| Male | reference | 0.77 | reference | 0.093 |
| Female | 0.952 (0.68—1.32) | 0.778 (0.58—1.04) | ||
| Race/ethnicity | ||||
| White, Non-Hispanic | reference | reference | 0.45 | |
| Hispanic | 0.861 (0.50—1.49) | 0.69 | 0.710 (0.41—1.24) | |
| Black/Other, Non-Hispanic | 0.779 (0.42—1.43) | 0.870 (0.49—1.54) | ||
| Primary Payer | ||||
| Private | reference | reference | ||
| Medicare | 1.18 (0.71—1.96) | 0.23 | 1.05 (0.57—1.92) | 0.97 |
| Medicaid | 1.62 (0.99—2.66) | 0.914 (0.55—1.53) | ||
| Self-pay/other | 1.35 (0.87—2.10) | 0.982 (0.64—1.51) | ||
| Arrived by EMS | ||||
| No | reference | 0.83 | reference | 0.77 |
| Yes | 1.06 (0.64—1.74) | 1.10 (0.59—2.07) | ||
| Physician Extender Seen | ||||
| No | reference | 0.58 | reference | 0.31 |
| Yes | 1.13 (0.73—1.76) | 1.27 (0.80—2.03) | ||
| Teaching Status | ||||
| No | reference | 0.76 | reference | 0.092 |
| Yes | 1.09 (0.64—1.84) | 1.70 (0.92—3.15) | ||
| Ownership status | ||||
| Voluntary non-profit | reference | reference | ||
| Government, non-federal | 1.36 (0.90—2.05) | 0.32 | 1.17 (0.78—1.74) | 0.67 |
| Proprietary | 0.963 (0.55—1.67) | 0.911 (0.53—1.57) | ||
| Region | ||||
| Northeast | reference | reference | ||
| Midwest | 0.962 (0.55—1.68) | 0.05 | 1.34 (0.80—2.26) | 0.66 |
| South | 0.846 (0.49—1.46) | 1.16 (0.71—1.88) | ||
| West | 0.545 (0.33—0.89) | 1.00 (0.60—1.66) | ||
| Year | ||||
| 2007 | reference | reference | ||
| 2008 | 0.838 (0.47—1.49) | 0.94 | 1.28 (0.82—1.99) | 0.42 |
| 2009 | 0.868 (0.53—1.42) | 1.09 (0.72—1.67) | ||
| 2010 | 0.901 (0.44—1.48) | 1.40 (0.89—2.20) | ||
| Educationa | ||||
| Quartile 1 | reference | reference | ||
| Quartile 2 | 1.39 (0.87—2.21) | 0.38 | 0.828 (0.51—1.34) | 0.28 |
| Quartile 3 | 1.17 (0.74—1.85) | 0.966 (0.57—1.64) | ||
| Quartile 4 | 1.56 (0.86—2.84) | 0.671 (0.40—1.12) | ||
| Household Income | ||||
| Quartile 1 | reference | reference | ||
| Quartile 2 | 0.862 (0.49—1.52) | 0.71 | 1.26 (0.74—2.15) | 0.60 |
| Quartile 3 | 0.701 (0.38—1.28) | 1.08 (0.59—1.97) | ||
| Quartile 4 | 0.706 (0.30—1.66) | 1.46 (0.64—3.29) | ||
| Poverty Level in ZIP | ||||
| < 5% | reference | reference | ||
| 5–9.99% | 0.802 (0.51—1.26) | 0.61 | 1.06 (0.65—1.75) | 0.83 |
| 10–19.99% | 0.863 (0.48—1.55) | 0.897 (0.50—1.62) | ||
| ≥ 20% | 0.667 (0.31—1.44) | 0.770 (0.36—1.63) | ||
| MSA | ||||
| No | reference | 0.008 | reference | 0.009 |
| Yes | 1.82 (1.17—2.82) | 1.95 (1.17—3.23) |
% adults with Bachelor’s degree in patient’s ZIP code, quartile
Diagnostic Imaging
Overall, 63% of visits included a CT scan. The proportion of visits including imaging increased only slightly (66%) in sensitivity analyses. Because other imaging modalities, such as ultrasound, may be clinically appropriate in certain populations, we also performed a sensitivity analysis for any possible stone-directed imaging (i.e., CT scan, ultrasound, plain x-ray). In this analysis, the proportion of visits that included imaging was 72%.
Similar to the findings with laboratory testing, there was almost no statistically significant variation along patient, provider or facility characteristics in the odds of undergoing guideline-adherent imaging (Table 3). The odds of a CT scan were nearly twice as high at hospitals within a metropolitan statistical area (OR 1.95, P = 0.009). Similar results were noted when the model outcome was any stone-directed imaging (data not shown).
Medical Expulsive Therapy
Providers prescribed MET at only 14% of eligible visits on a nationally representative basis. Because randomized controlled trials supporting MET focus on ureteral stones, we performed a sensitivity analysis on the subpopulation of those visits that included a diagnostic code for ureteral stone, and otherwise fulfilled eligibility criteria for MET. Restricting our analysis to this highly selected group increased the proportion of guideline-adherent visits only to 16.8%. Due to the relatively small number of visits where MET was prescribed, the multivariable model included only age, gender, region and markers of socioeconomic status (Supplementary Table 1). The odds of females receiving MET was less than half that of men (OR 0.47, P <0.001).
Health Information Technology
A sensitivity analysis examined associations between delivery of guideline-adherent care and specific information technology systems. No statistically significant associations existed between laboratory testing, imaging or MET utilization endpoints and reminder systems for guideline-based interventions. Similarly, no statistically significant association was observed between laboratory testing adherence and the availability of a computerized lab ordering system.
Discussion
In this novel analysis of guideline adherence for the acute evaluation of patients with suspected kidney stones, we find that care fails to meet recommendations in a substantial proportion of cases. Only 2 in 5 patients undergo laboratory evaluation that indicates whether immediate surgical intervention is necessary, and only 1 in 7 receive therapy that has been shown to reduce the risk for future surgical intervention by 25%.11 These findings suggest substantial opportunities for improving quality of acute care for patients with kidney stones, a disease that afflicts nearly 1 in 11 persons in the United States.2
The potential consequences for patients of these apparent failures of care are significant. Laboratory testing provides crucial information to diagnose renal failure or early signs of sepsis. Renal failure and evidence of systemic infection in the presence of an obstructing stone are each indications for immediate procedural intervention.8 Lack of assessment for leukocytosis is associated with an increased risk of ED revisits,19 possibly due to missed sepsis.
Of particular concern is the apparent utilization of MET in only 1 of every 7 eligible patients, and the dramatically lower use of MET among women (9% vs 17% for men). We found that the guideline adherence rate was 14%, meaning that approximately 900,000 patients annually do not receive this highly effective therapy. Based on a number needed to treat of 4,11 this failure to deliver a well-tolerated, relatively inexpensive pill results in a projected 226,000 avoidable surgical procedures annually. The direct and indirect costs of these potentially unnecessary surgical interventions are likely substantial.20
That only 14% of eligible visits result in a prescription for MET is concerning, but this proportion represents a relatively sharp rise in utilization compared to prior analyses.6,15 Using similar methodology, Hollingsworth et al15 examined MET use between 2000 and 2006 in the NHAMCS-ED dataset, before this intervention received guideline endorsement.8 In 2006, after 11 randomized controlled trials had been published supporting the intervention, utilization of MET was estimated at only 3.9%.15 While overall utilization tripled between 2006 and 2010, the fact remains that a decade after the publication of the first randomized controlled trials of MET, only 1 in 7 eligible patients receive the intervention.
Patients with acute symptoms of kidney stones are primarily treated by physicians other than urologists,7 but urologists conducted the randomized controlled trials and developed guidelines supporting pharmacologic intervention. The existence of single-specialty guidelines often challenges the dissemination of practice into other specialties, such as emergency medicine; our results should be considered in this context. Lack of dissemination into the general medical literature for MET15 and other specialist-driven advances speaks to one of the challenges of providing high quality, coordinated care in a fragmented and highly specialized healthcare environment.
Use of health information technology could potentially improve care delivery. The results of our sensitivity analysis regarding clinical decision support showed no benefit of these systems in terms of increasing guideline adherence for patients with suspected kidney stones. The NHAMCS-ED dataset lacks information regarding the specific conditions supported by local health information technology systems. Therefore it remains unknown whether our findings imply a limitation of clinical-decision support technology, or simply failure to provide information regarding treatment of patients with suspected kidney stones. However, recent analyses suggest that one of the main consequences of widespread health information technology adoption has been an increase in costs without commensurate changes in the quality of care delivered.21 Thus it remains to be seen whether health information technology will fulfill the promise of helping providers deliver better care at lower cost.
Our findings must be considered in the context of several limitations. Classification bias could impact measurement of outcomes. However, the NHAMCS dataset specifically records performance of the laboratory tests recommended in evidence-based guidelines (e.g., urinalysis). We used previously validated algorithms15 to identify patients eligible for MET, and up to 8 medications prescribed by providers were specifically noted.
The NHAMCS dataset provides encounter level information, and therefore providers’ prior knowledge of a patient’s history or medical condition could confound our results. However, sensitivity analyses limited to first presentations for the stone and excluding patients with recent encounters for other reasons yielded no clinically important changes in our results. A related potential source of selection bias is the use of diagnostic codes that may identify only those with a confirmed stone, and thus miss those with a differential diagnosis much broader than a urinary stone. We believe it likely that any bias from this selection would be towards the appearance of greater adherence.
With respect to our findings regarding low utilization of MET, important clinical detail regarding stone size and location is lacking. The diagnostic code for renal stones is not specific (that is, in practice it is applied to patients with both renal and ureteral stones) and therefore the cohort may include patients with symptomatic renal stones, for whom MET may not be beneficial.18 However, even when limiting the analysis to a highly specific diagnostic codes for a ureteral stone,18 we did not find substantial improvement in MET use.
We lacked important detail as to whether and to what extent these apparent failures in care delivery impact patient-relevant outcomes. In other datasets, lack of laboratory testing is associated with an increased risk of ED revisit, but other outcomes (i.e., sepsis) were not examined.19,22 Measurement of blood counts and serum creatinine are not explicit in current guidelines, but aside from exam findings (i.e., fever, hypotension), leukocytosis or renal failure detected through laboratory testing typically indicate the need for urgent procedural intervention. Given the magnitude of potential harms (i.e., severe sepsis, death) and the relatively low cost of the recommended laboratory tests suggest that focused efforts towards improvement are warranted. In the light of emerging evidence regarding potential iatrogenic harms of radiologic exams,23–26 it remains unclear whether our results represent ideal patterns of imaging use, or potential overutilization of computerized tomography. Finally, increasing use of a well-tolerated, low-cost pharmacologic intervention that can prevent costly surgical procedures in 1 out of 4 patients seems a straightforward opportunity to maximize value in healthcare delivery.
Conclusion
These limitations notwithstanding, our findings compel immediate action; at a minimum, individual institutions should examine their own guideline adherence in this dimension. The NHAMCS dataset is specifically designed to generate nationally representative estimates of ED care. Our results document apparent failures in care for an increasingly prevalent disease, with important consequences for healthcare spending and patient health. Physicians must engage in multidisciplinary partnerships to design and assess interventions to reliably deliver high quality, guideline-adherent care for patients with symptomatic kidney stones.
Supplementary Material
Acknowledgments
Grant Support: Drs. Scales and Bergman were supported by the Robert Wood Johnson Foundation Clinical Scholars program and the US Department of Veterans Affairs during conduct of this research. Drs. Saigal and Litwin were supported by the Urologic Diseases in America Project, through the National Institute of Diabetes and Digestive and Kidney Diseases and the National Library of Medicine (HHSN276201200016C).
Dr. Scales had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
FUNDING/SUPPORT
Drs. Scales and Bergman were supported by the Robert Wood Johnson Foundation and the VA Office of Academic Affiliations through the VA/Robert Wood Johnson Clinical Scholars Program.
The Urologic Diseases in America Project is supported by grant HHSN276201200016C from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Library of Medicine.
The views expressed in this article are those of the authors and do not necessarily reflect the position and policy of the United States Federal Government or the Department of Veterans Affairs. No official endorsement should be inferred.
Footnotes
AUTHOR CONTRIBUTIONS:
Study concept and design: Scales, Bergman, Carter, Jack, Saigal, Litwin
Acquisition of data: Scales
Analysis and interpretation of data: Scales, Bergman, Carter, Jack, Saigal, Litwin
Drafting of the manuscript: Scales
Critical revision of the manuscript for important intellectual content: Bergman, Carter, Jack, Saigal, Litwin
Statistical analysis: Scales
Obtained funding: Scales, Saigal, Litwin
Administrative, technical, or material support: Saigal, Litwin
Study supervision: Saigal, Litwin
ROLE OF THE SPONSORS:
The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation or review of the manuscript, or decision to submit for publication. The Robert Wood Johnson Foundation and US Department of Veterans Affairs had no role in approval of the manuscript. The Executive Committee of the Urologic Diseases in America Project includes representatives from the National Institute of Diabetes and Digestive and Kidney Diseases; the Executive Committee approves project manuscripts based on technical considerations alone but otherwise has no role in the study.
ETHICAL APPROVAL TO PERFORM THE STUDY:
The institutional review boards of the RAND Corporation determined that the study design was exempt from the requirement for review.
DISCLOSURE OF CONFLICTS OF INTEREST:
None of the authors have conflicts of interest to disclose.
GROUP INFORMATION:
The members of the Urologic Disease in America Project are: Mark S. Litwin, MD MPH, Department of Urology, David Geffen School of Medicine and Fielding School of Public Health, University of California, Los Angeles; Christopher S. Saigal, MD MPH, Department of Urology, David Geffen School of Medicine, UCLA and RAND Corporation; Paul Eggers, PhD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington, DC; Tamara Bavendam, MD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington DC; Ziya Kirkali, MD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington, DC.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003 May;63(5):1817–1823. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 2.Scales CD, Jr, Smith AC, Hanley JM, Saigal CS. Prevalence of Kidney Stones in the United States. Eur Urol. 2012 Mar 31; doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ljunghall S. Incidence of upper urinary tract stones. Miner Electrolyte Metab. 1987;13(4):220–227. [PubMed] [Google Scholar]
- 4.Saigal CS, Joyce G, Timilsina AR. Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int. 2005 Oct;68(4):1808–1814. doi: 10.1111/j.1523-1755.2005.00599.x. [DOI] [PubMed] [Google Scholar]
- 5.Litwin MS, Saigal C. US Department of Health and Human Services, editor. Urologic Diseases in America. Washington, DC: US Government Printing Office; 2012. [Google Scholar]
- 6.Fwu CW, Eggers PW, Kimmel PL, Kusek JW, Kirkali Z. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013 Mar;83(3):479–486. doi: 10.1038/ki.2012.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sterrett SP, Moore NW, Nakada SY. Emergency room follow-up trends in urolithiasis: single-center report. Urology. 2009 Jun;73(6):1195–1197. doi: 10.1016/j.urology.2008.07.057. [DOI] [PubMed] [Google Scholar]
- 8.Preminger GM, Tiselius HG, Assimos DG, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007 Dec;178(6):2418–2434. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 9.Coursey CA, Casalino DD, Remer EM, et al. Acute Onset Flank Pain - Suspicion of Stone Disease. Reston, VA: 2011. [Google Scholar]
- 10.Pearle MS. AUA Update Series. American Urological Association; 2008. Management of the Acute Stone Event. [Google Scholar]
- 11.Hollingsworth JM, Rogers MA, Kaufman SR, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006 Sep 30;368(9542):1171–1179. doi: 10.1016/S0140-6736(06)69474-9. [DOI] [PubMed] [Google Scholar]
- 12.Brown J. Diagnostic and treatment patterns for renal colic in US emergency departments. Int Urol Nephrol. 2006;38(1):87–92. doi: 10.1007/s11255-005-3622-6. [DOI] [PubMed] [Google Scholar]
- 13.Hyams ES, Korley FK, Pham JC, Matlaga BR. Trends in imaging use during the emergency department evaluation of flank pain. J Urol. 2011 Dec;186(6):2270–2274. doi: 10.1016/j.juro.2011.07.079. [DOI] [PubMed] [Google Scholar]
- 14.Hyams ES, Matlaga BR, Korley FK. Practice patterns in the emergency care of kidney stone patients: an analysis of the National Hospital Ambulatory Medical Care Survey (NHAMCS) Can J Urol. 2012 Aug;19(4):6351–6359. [PubMed] [Google Scholar]
- 15.Hollingsworth JM, Davis MM, West BT, Wolf JS, Jr, Hollenbeck BK. Trends in medical expulsive therapy use for urinary stone disease in U.S. emergency departments. Urology. 2009 Dec;74(6):1206–1209. doi: 10.1016/j.urology.2009.03.050. [DOI] [PubMed] [Google Scholar]
- 16.NHAMCS Micro-File Documentation. 2009.
- 17.Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America project: urolithiasis. J Urol. 2005 Mar;173(3):848–857. doi: 10.1097/01.ju.0000152082.14384.d7. [DOI] [PubMed] [Google Scholar]
- 18.Semins MJ, Trock BJ, Matlaga BR. Validity of administrative coding in identifying patients with upper urinary tract calculi. J Urol. 2010 Jul;184(1):190–192. doi: 10.1016/j.juro.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 19.Scales CD, Jr, Lin L, Saigal CS, et al. Emergency department revisits for patients with kidney stones in california. Acad Emerg Med. 2015 Apr;22(4):468–474. doi: 10.1111/acem.12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tosoian JJ, Ludwig W, Sopko N, Mullins JK, Matlaga BR. The effect of repair costs on the profitability of a ureteroscopy program. J Endourol. 2015 Apr;29(4):406–409. doi: 10.1089/end.2014.0435. [DOI] [PubMed] [Google Scholar]
- 21.Kellermann AL, Jones SS. What it will take to achieve the as-yet-unfulfilled promises of health information technology. Health Aff (Millwood) 2013 Jan;32(1):63–68. doi: 10.1377/hlthaff.2012.0693. [DOI] [PubMed] [Google Scholar]
- 22.Sfoungaristos S, Hidas G, Gofrit ON, et al. A Novel Model to Predict the Risk of Readmission in Patients with Renal Colic. Journal of Endourology. 2014;28(8):1011–1015. doi: 10.1089/end.2014.0082. [DOI] [PubMed] [Google Scholar]
- 23.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009 Dec 14;169(22):2078–2086. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrandino MN, Bagrodia A, Pierre SA, et al. Radiation exposure in the acute and short-term management of urolithiasis at 2 academic centers. J Urol. 2009 Feb;181(2):668–672. doi: 10.1016/j.juro.2008.10.012. discussion 673. [DOI] [PubMed] [Google Scholar]
- 25.Goodman DM. Initiatives focus on limiting radiation exposure to patients during CT scans. JAMA. 2013 Feb 20;309(7):647–648. doi: 10.1001/jama.2013.83. [DOI] [PubMed] [Google Scholar]
- 26.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012 Aug 4;380(9840):499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.