Abstract
Background
Surgical approach to type A acute aortic dissection (AADA) is usually dictated by the presenting anatomy. We compared long-term outcomes of AADA repaired with a root replacement versus a supracoronary tube graft, regardless of the proximal extent of the intimal tear.
Methods
A single-centre, retrospective cohort of consecutive patients undergoing repair of AADA between December 1999 and March 2012 were stratified based on the proximal surgical procedure performed: supracoronary tube graft or root replacement. Imaging, chart reviews and clinical follow-ups were analyzed to identify the presenting anatomy and clinical outcomes.
Results
We included the cases of 75 patients in our analysis: 54 received a supracoronary tube graft and 21 received a root replacement. The proximal tear was identified below the sinotubular junction in all patients in the root group and in 61% of patients in the supracoronary group. We detected no differences between the groups for in-hospital mortality, length of stay, or complications. However, the root group had significantly increased renal failure (0% v. 9.5%, p = 0.018), cardiopulmonary bypass time (198.4 ± 80.0 min v. 316.5 ± 102.5 min, p < 0.001), cross-clamp time (91.6 ± 34.9 min v. 191.3 ± 52.8 min, p < 0.001), duration of surgery (457.5 ± 129.9 min v. 611.6 ± 197.8 min, p < 0.001), and platelet transfusions (8.1 ± 7.6 v. 12.8 ± 8.7 units, p = 0.021) than the supracoronary group. Long-term follow-up demonstrated a greater incidence of 2+ aortic regurgitation among patients in the supracoronary group than the root group (29.7% v. 0.0%, p = 0.006); however, there was no difference between the groups in symptoms or reoperation.
Conclusion
In AADA, aortic root replacement involves a longer procedure with increased risk of early renal impairment. Long-term follow-up identified significantly more aortic regurgitation and root dilation in the supracoronary group than the root group, with a trend toward worse long-term survival. However, we found no difference between the groups in mortality, reoperation or New York Heart Association class.
Abstract
Contexte
L’approche chirurgicale à la dissection aigüe de l’aorte de type A (DAAA) dépend habituellement de la présentation anatomique. Nous avons comparé les résultats à long terme d’une DAAA réparée par remplacement de la racine de l’aorte c. greffon supracoronarien artificiel, indépendamment de la portée proximale de la déchirure de l’intima.
Méthodes
Une cohorte rétrospective monocentrique de patients consécutifs soumis à une réparation de DAAA entre décembre 1999 et mars 2012 a été stratifiée en fonction de l’intervention chirurgicale proximale effectuée : greffon supracoronarien artificiel ou remplacement de la racine de l’aorte. Les épreuves d’imagerie, résumés de dossiers et suivis cliniques ont été analysés pour cerner la présentation anatomique et les résultats cliniques.
Résultats
Nous avons inclus 75 patients dans notre analyse : 54 ont reçu un greffon supracoronarien artificiel et 21 ont subi un remplacement de la racine de l’aorte. Une déchirure proximale a été identifiée sous la jonction sinotubulaire chez tous les patients du groupe racine de l’aorte et chez 61 % des patients du groupe greffon supracoronarien. Nous n’avons décelé aucune différence entre les groupes pour ce qui est de la mortalité en milieu hospitalier, de la durée de l’hospitalisation ou des complications. Mais, le groupe racine de l’aorte a présenté des augmentations significatives du nombre de cas d’insuffisance rénale (0 % c. 9,5 %, p = 0,018), de la durée de la circulation extracorporelle (198,4 ± 80,0 min c. 316,5 ± 102,5 min, p < 0,001), du clampage de l’aorte (91,6 ± 34,9 min c. 191,3 ± 52,8 min, p < 0,001) et de la chirurgie (457,5 ± 129,9 min c. 611,6 ± 197,8 min, p < 0,001), ainsi que du nombre de transfusions plaquettaires (8,1 ± 7,6 unités c. 12,8 ± 8,7 unités, p = 0,021) comparativement au groupe greffon supracoronarien. Le suivi à long terme a fait état d’une incidence plus élevée de régurgitation aortique 2+ chez les patients du groupe greffon supracoronarien comparativement au groupe racine de l’aorte (29,7 % c. 0,0 %, p = 0,006); toutefois, on n’a noté aucune différence entre les groupes pour ce qui est des symptômes ou du taux de réopération.
Conclusion
Dans la DAAA, le remplacement de la racine de l’aorte suppose une intervention de plus longue durée qui s’accompagne d’un risque accru d’insuffisance rénale précoce. Un suivi à long terme a révélé un nombre significativement plus élevé de cas de régurgitation aortique et de dilatation de la racine de l’aorte dans le groupe greffon supracoronarien que dans le groupe racine de l’aorte, avec une tendance moins favorable au plan de la survie à long terme. Toutefois, nous n’avons trouvé aucune différence entre les groupes pour ce qui est de la mortalité, du taux de réopération ou de la classe de la New York Heart Association.
Stanford type A acute aortic dissection (AADA) is a lethal condition with an early mortality of 1% per hour and 21% in first 24 hours with isolated medical therapy.1,2 Surgical considerations include deciding on the proximal and distal degree of the resection, excluding the intimal tear, removing diseased/aneurysmal tissue and preventing malperfusion.2,3 Proximal extension of an AADA into the aortic root (below the sinotubular junction) has important implications for the degree of complexity required for adequate repair.3,4 Aortic root procedures involving composite valve grafts or valve-sparing techniques while excluding the proximal intimal tear are presumed to be technically challenging because of the complexity of reimplanting coronary arteries, requirement of additional suture lines, and extended cardiopulmonary bypass and cross-clamp durations.4 Using a supracoronary tube graft (with or without commissural resuspension) to replace the ascending aorta and exclude the entry tear that is below the sinotubular junction but not involving the aortic annulus can be performed as a more conservative alternative.5 Restoration of the association between the size of the aortic root and ascending aorta along with resuspension of commissures has been demonstrated to be adequate to address the acute aortic insufficiency associated with AADA.6
Many factors, including patient comorbidities, presence or absence of connective tissue disorder, morphology of the aortic valve and the extent of the proximal tear into the aortic root, contribute to the surgical decision-making regarding the need for a total root replacement compared with a more conservative supracoronary graft.7 The purpose of the present study was to report patient demographic characteristics, operative outcomes (mortality and major adverse cardiac events), clinical follow-up (survival and freedom from reoperation) and imaging (echocardiography and computed tomography [CT]) results of patients presenting with AADA who were treated with root replacement procedures compared with a conservative approach for root intervention.
Methods
Patient population
We retorspectively reviewed the charts, imaging and operative reports of consecutive patients who underwent aortic surgery for AADA at the University Hospital of the London Health Sciences Centre in London, Ont., between December 1999 and March 2012 to identify the presenting anatomy (proximal/distal extent of dissection, previous aneurysm, bicuspid valve), presence of risk factors for aortic dissection (hypertension, family history, connective tissue disorder, cocaine use, pregnancy) and operative procedure performed. Approval for data collection for this study was granted by the research ethics board of Western University, which waived the requirement for individual patient consent. All patients underwent preoperative CT of the thorax, confirming diagnosis of type A dissection, and had intraoperative transesophageal echocardiograhpy.
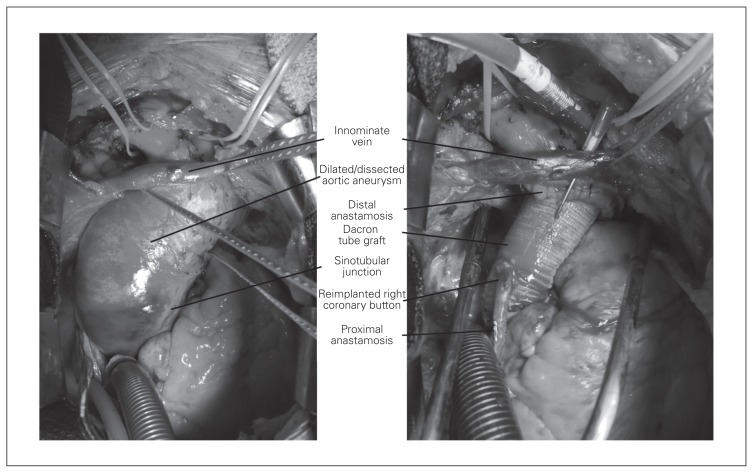
Patients were retrospectively classified into 2 groups based on the surgical details provided in the operative report. The surpracoronary group included all patients who underwent repair with a supracoronary tube graft, with or without resuspension of the aortic valve commissures (Fig. 1). The root group included patients who underwent either a composite valve graft replacement or aortic valve-sparing procedure (Fig. 1).
Fig. 1.
Intraoperative images of acute type A aortic dissection (left), with post-Bentall repair, involving complete replacement of the aortic root with reimplantation of coronary buttons and ascending aortic Dacron tube graft (right).
Surgical technique
All procedures occurred under the discretion of 1 of 8 participating surgeons, resulting in variations among cannulation site, degree of hypothermia, cardioplegia protection strategy and cerebral perfusion technique. Standard postoperative protocols were followed for immediate postsurgical care and ward convalescence.
In the supracoronary group, some patients had an aortic entry tear clearly identified distal to the sinotubular junction, and the aortic root and valve along with the coronary artery ostia were not involved. Most patients in this group, had dissections where the entry tear, or the dissection flap, extended below the sinotubular junction, but not into the annulus. For patients in the root group, the decision was made by the individual surgeon in the operating room to proceed with complete replacement of the root with reimplantation of the coronary arteries in order to address the competency of the valve and native architecture of the root as the entry tear was below the level of the sinotubular junction. One patient required conversion from a supracoronary tube graft to a composite valve graft because of severe postrepair aortic insufficiency (AI).
Clinical and imaging follow-up
We completed a retrospective chart review and assessment of outcomes according to our institutional database for all patients. Transthoracic echocardiography assessed postoperative aortic regurgitation, degree of aortic root dilation and ventricular function. Postoperative CT evaluated aortic root dilation, patency of distal false lumen and presence of sternal wound infection or dehiscence.
Statistical analysis
Continuous variables are expressed as means ± standard deviations, and categorical data are expressed as percentages. We compared categorical variables using χ2 tests and independent continuous variables using unpaired Student t tests. We considered results to be significant at p < 0.05.
Results
Preoperative demographic characteristics
Of the 75 patients undergoing surgical repair of an acute type A aortic root dissection during our study period, 54 were treated with a supracoronary tube graft with or without commissural resuspension of the aortic valve and 21 were treated with a root replacement procedure. The demographic characteristics and presenting anatomy are displayed in Table 1 and Table 2. There was no significant difference between the groups in age; sex; prevalence of clinically important comorbidities, such as hypertension; previous myocardial infarction (MI); previous cardiac surgery; or urgency of the procedure. The presenting anatomy of the aortic dissections is described in Table 2. Thirty-three of the 54 patients in the supracoronary group compared with all patients in the root group had dissections that were identified as proximal to the sinotubular junction (61.1% v. 100%, p < 0.001). There was no significant difference between the groups with respect to involvement of the aortic arch or descending aorta; presence of a bicuspid valve; or presence of hypertension, family history, current pregnancy, or illicit drug use. Presence of connective tissue disorder was significantly higher in the root group than the supracoronary group (1.9% v. 14.2%, p = 0.018).
Table 1.
Demographic and clinical characteristics of the study sample
| Characteristic | Group; mean ± SD or no. (%) | p value | ||
|---|---|---|---|---|
| Total (n = 75) | Supracoronary graft (n = 54) | Root procedure (n = 21) | ||
| Age, yr | 63.3 ± 13.7 | 63.9 ± 13.4 | 61.4 ± 14.8 | 0.48 |
| Male sex | 40 (53.3) | 37 (68.5) | 13 (61.9) | 0.58 |
| Hypertension | 43 (57.3) | 31 (57.4) | 12 (57.1) | 0.98 |
| Emergent procedure* | 57 (76.0) | 41 (75.9) | 16 (76.2) | 0.98 |
| Salvage procedure† | 12 (16.0) | 9 (16.7) | 3 (14.3) | 0.80 |
| Previous cardiac surgery | 8 (10.7) | 5 (9.3) | 3 (14.3) | 0.52 |
| Previous MI | 1 (1.9) | 1 (1.3) | 0 (0) | 0.53 |
MI = myocardial infarction; SD = standard deviation.
Emergent procedures refer to high-acuitiy surgical case taken to the operating room within 2 h of original presentation to hospital.
Salvage procedures occurred in patients in cardiogenic shock requiring inotropic or mechanical support.
Table 2.
Presenting anatomy
| Anatomy | Group; no. (%) | p value | ||
|---|---|---|---|---|
| Total (n = 75) | Supracoronary graft (n = 54) | Root procedure (n = 21) | ||
| Root involvement | 54 (72.0) | 33 (61.1) | 21 (100) | < 0.001 |
| Arch repaired* | 16 (21.3) | 10 (18.5) | 6 (28.6) | 0.34 |
| Bicuspid valve | 1 (1.3) | 0 (0) | 1 (4.7) | 0.11 |
| Tricuspid valve | 74 (98.7) | 54 (100) | 20 (95.3) | 0.11 |
| Connective tissue disorder | 4 (5.3) | 1 (1.9) | 3 (14.2) | 0.018 |
| Risk factors† | 50 (66.7) | 34 (63.0) | 16 (76.2) | 0.28 |
Any procedure involving replacement of aortic tissue distal to the innominate artery, including both hemiarch and total arch replacements.
Risk factors include hypertension, pregnancy, inflammatory disease, family history and cocaine use.
Operative results
There was no significant difference between the groups in 30-day mortality (20.4% in the supracoronary group v. 19.0% in the root group). Major adverse cardiac events, including postoperative infection, renal failure, ventilator dependence, need for reoperation for bleeding and dehiscence, did not differ significantly between the groups. Operative details and results are shown in Table 3. There was no significant difference between the groups in location of arterial cannulation (femoral, axillary or both). Cardiopulmonary bypass time (198.4 ± 80.0 min v. 316.5 ± 102.5 min, p < 0.001), cross-clamp time (91.6 ± 34.9 min v. 191.3 ± 52.8 min, p < 0.001) and total operating room time (457.5 ± 129.9 min v. 611.6 ± 197.8 min, p < 0.001), were all significantly increased for patients undergoing a root replacement procedure. Degree of hypothermia, presented as the average of the coolest operative temperatures, did not differ significantly between the groups (21.9 ± 4.7°C in the supracoronary group v. 21.0 ± 3.2°C in the root group, p = 0.42). There was no significant difference in the rates of packed red blood cell transfusion (9.2 ± 8.9 units v. 11.5 ± 8.4 units, p = 0.31) or fresh frozen plasma (10.7 ± 9.9 units v. 14.2 ± 10.4 units, p = 0.18) between the supracoronary and root groups; however, we found a significant difference in the rates of platelets transfused (8.1 ± 7.6 units v. 12.8 ± 8.7 units, p = 0.021).
Table 3.
Operative characteristics
| Characteristic | Group; no. (%) or mean ± SD | p value | ||
|---|---|---|---|---|
| Total (n = 75) | Supracoronary graft (n = 54) | Root procedure (n = 21) | ||
| Femoral cannulation | 38 (50.7) | 30 (55.6) | 8 (38.1) | 0.18 |
| Axillary cannulation | 16 (21.3) | 12 (22.2) | 4 (19.0) | 0.76 |
| Femoral and axillary cannulation | 13 (17.3) | 8 (14.8) | 5 (23.8) | 0.36 |
| Total operative duration | 494.6 ± 162.3 | 457.5 ± 129.9 | 611.6 ± 197.8 | < 0.001 |
| Cardiopulmonary bypass time, min | 229.2 ± 100.8 | 198.4 ± 80.0 | 316.5 ± 102.5 | < 0.001 |
| Aortic cross-clamp time, min | 118.8 ± 60.2 | 91.6 ± 34.9 | 191.3 ± 52.8 | < 0.001 |
| Lowest core temperature, °C | 21.7 ± 4.4 | 21.9 ± 4.7 | 21.0 ± 3.2 | 0.42 |
SD = standard deviation.
Postoperative imaging follow-up results
Postoperative imaging data were available for 34 of 43 (79.1%) patients in the supracoronary group who survived beyond 30 days postoperatively; their mean duration of follow-up was 84.7 ± 55.1 months. These data were available for 16 of the 17 (94.1%) patients in the root group who survived beyond 30 days postoperatively; their mean duration of follow-up was 70.3 ± 34.0 months. The degree of aortic regurgitation was evaluated at follow-up, with yearly transthoracic echocardiography. Significant regurgitation was deemed to be greater than 2+ to account for any interevaluator bias, as different cardiologists were reviewing the patients’ charts. Patients in the supracoronary group had a greater incidence of 2+ aortic regurgitation than patients in the root group (29.7% v. 0.0%, p = 0.006; Table 4). Of the patients in the supracoronary group who had an intimal dissection flap proximal to the sinotubular junction, 25.0% were found to have significant 2+ aortic regurgitation at the most recent follow-up.
Table 4.
Surgical outcomes
| Outcome | Group; no. (%) or mean ± SD | p value | ||
|---|---|---|---|---|
| Total (n = 75) | Supracoronary graft (n = 54) | Root procedure (n = 21) | ||
| In-hospital 30-day mortality | 15 (20.0) | 11 (20.4) | 4 (19.0) | 0.90 |
| Stroke | 10 (13.2) | 9 (16.7) | 1 (4.8) | 0.17 |
| Length of hospitalization, d | 15.4 ± 10.4 | 15.9 ± 11.2 | 14.0 ± 6.8 | 0.47 |
| ICU stay, d | 7.9 ± 12.4 | 8.7 ± 13.6 | 4.8 ± 4.4 | 0.20 |
| Renal failure | 2 (2.7) | 0 (0) | 2 (9.5) | 0.018 |
| Postoperative infection | 2 (2.7) | 1 (1.9) | 1 (4.8) | 0.48 |
| Ventilator dependence | 11 (14.7) | 7 (13.0) | 4 (19.0) | 0.50 |
| Reoperation for bleeding | 9 (12.0) | 7 (13.0) | 2 (9.5) | 0.68 |
| Postoperative MI | 1 (1.3) | 0 (0) | 1 (4.8) | 0.11 |
| Sternal dehiscence | 2 (2.7) | 1 (1.9) | 1 (4.8) | 0.48 |
| Patent false lumen on CT | 14 (18.7) | 9 (16.7) | 5 (23.8) | 0.48 |
| Aortic root, mm | 38 ± 9 | 44 ± 6 | 30 ± 5 | < 0.001 |
| 2+ aortic regurgitation | 8 (20.0) | 8 (29.7) | 0 (0) | 0.006 |
| Transfusion outcomes | ||||
| Packed red blood cells | 9.8 ± 7.3 | 9.2 ± 8.9 | 11.5 ± 8.4 | 0.31 |
| Adult platelets | 9.3 ± 8.1 | 8.1 ± 7.6 | 12.8 ± 8.7 | 0.021 |
| Fresh frozen plasma | 11.6 ± 10.1 | 10.7 ± 9.9 | 14.2 ± 10.4 | 0.18 |
| Patients not requiring transfusion | 4 (5.4) | 3 (5.7) | 1 (4.8) | 0.68 |
| Cardiac-related deaths | 18 (88.9) | 13 (81.3) | 5 (100) | 0.35 |
| Reoperation | 0 (0) | 0 (0) | 0 (0) | > 0.99 |
| NYHA class in living patients | ||||
| I | 29 (67.4) | 22 (71.0) | 7 (58.3) | 0.56 |
| II | 9 (20.9) | 5 (16.1) | 4 (33.3) | 0.28 |
| III | 5 (11.6) | 4 (12.9) | 1 (8.3) | 0.60 |
| IV | 0 (0) | 0 (0) | 0 (0) | > 0.99 |
CT = computed tomography; ICU = intensive care unit; MI = myocardial infarction; NYHA = New York Heart Association; SD = standard deviation.
Follow-up CT imaging identified a patent distal false lumen in 16.7% of patients in the supracoronary group and 23.8% in the root group (p = 0.48). Furthermore, echocardiography and CT reports showed a significant enlargement of the aortic root in the supracoronary group compared with the root group (44 ± 6 mm v. 30 ± 5 mm, p = 0.002; Table 4).
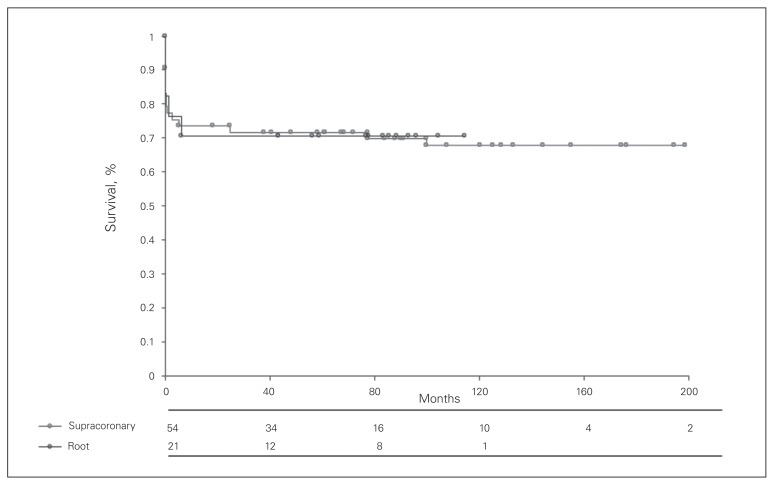
Clinical follow-up results
Long-term clinical follow-up data were available for 86% of patients who survived beyond 30 days postoperatively. Overall survival at 1 and 5 years was 71.7% and 67.9%, respectively, in the supracoronary group and 70.6% and 70.6%, respectively, in the root group. Kaplan–Meier survival curves are displayed in Figure 2. No significant difference between the groups was seen on follow-up with regards to cardiac-related deaths, functional (New York Heart Association) status or need for reoperation in patients surviving beyond the first 30 postoperative days (Table 4).
Fig. 2.
Kaplan-Meier survival curves.
Discussion
The results of our study suggest that in the setting of acute type A dissections, aortic root replacement procedures consisting of composite valve grafts or aortic valve-sparing techniques do not appear to expose patients to an increased risk of perioperative adverse outcomes, even given the significantly increased need for platelet transfusions, OR, total bypass and cross-clamp times, and resulted in long-term competency of the aortic valve.
Interestingly, more than 60% of the patients who received an isolated supracoronary tube graft still had a proximal tear identified below the sinotubular junction. This observation indicates that in reality the decision to address the aortic root at the time of surgery likely depends on other factors, including clinical status; tissue quality; and surgeon comfort with aortic root replacement procedures, such as composite valve grafts and aortic valve-sparing techniques, as they represent a far more technically demanding and lengthy procedure. However, we did not detect a significant difference in postoperative complications. Our series did not show any significant increase in major complications (death, stroke, bleeding requiring reoperation, MI, ventilator dependence, infection) among patients who underwent an aortic root replacement procedure. Furthermore, these procedures did not result in any significant increase in admissions to the intensive care unit or length of hospital stay. There was an increase in units of transfused platelets between the supracoronary and root groups (8.1 ± 7.6 units v. 12.8 ± 8.7 units, p = 0.021); however, we felt this increase was likely due to the increased pump times leading to an expected increase in postoperative platelet dysfunction.
The mortality and morbidity results achieved in this study for root replacement procedures are similar to those reported in other studies. Our 30-day mortality of 20.0% is similar to that described by multiple trials involving the International Registry of Acute Aortic Dissection (IRAD) database, which reported mortality between 16.2% and 27.4%.8,9 As seen in the Kaplan–Meier survival curve in our study (Fig. 1.), although early mortality was high, patients surviving the perioperative period did well in the long term.
An additional important outcome from our study was the echocardiographic findings demonstrating that 29.7% of patients with supracoronary tube grafts and commissural resuspension experienced moderate to severe AI at a mean follow-up of 84.7 ± 55.1 months. We demonstrated a significant reduction of more than 2+ aortic regurgitation in patients who underwent a root procedure compared with those who underwent a supracoronary tube graft with or without commissural resuspension (0% v. 29.7%, p = 0.006). Interestingly, there was no significant difference in development of aortic regurgitation within the supracoronary group between patients who had a proximal intimal tear within the root and those who did not (25.0% v. 29.7%). This finding may indicate that development of regurgitation in the future may be secondary only to the native tissue left behind if competency is restored to the aortic valve at the time of surgery. Our results differ from those of Rylski and colleagues, 10 who studied the longterm echocardiography and CT results of 119 patients who underwent a supracoronary tube graft for AADA. At median follow-up of 33.8 months, 26 (27%) patients had new-onset aortic root disease and 10 required aortic root reoperation.10 The data on patients in the root group in our study are more in line with the work of Leontyev and colleagues,11 who described a series of 179 patients undergoing root replacement procedures, none of whom had greater than 2+ AI at short-term follow-up and in whom 5-year freedom from reoperation was approximately 96%. Three patients in our cohort were identified on clinical follow-up to meet guidelines for reoperation owing to chronic aortic regurgitation or aortic root dilation. None of these patients received an aortic valve reoperation owing to advanced age or comorbidities; in these cases the surgeon deemed the operation too risky or the patient declined the operation. The survival curves and clinical outcome data presented here suggest that chronic AI in these patients, although clinically well tolerated, likely explains the decreased survival we observed when comparing the supracoronary with the root group over time. Rates of persistent false lumen flow in our study were comparable between the groups (16.7% in the supracoronary group v. 23.8% in the root group, p = 0.48); however, the rates were significantly lower than the 69% previously reported in the literature.12
Our results demonstrate that aortic root procedures, including remodelling/reimplantation techniques and composite valve grafts, have comparable perioperative outcomes to supracoronary procedures despite exposing individuals to longer bypass times, more transfusions and a greater risk of renal failure. The real benefit of replacing the entire aortic root seems to emerge with time as individuals are faced with far fewer complications, such as chronic AI and root dilation, leading to improved survival trends. Supracoronary tube grafts offer a technically less difficult operative approach with good perioperative outcomes, regardless of the proximal extent of the intimal tear, but expose the patient to worsening AI, root dilation and worse survival long-term.
Limitations
Limitations of our study include its retrospective design, lack of blinding and randomization owing to the nature of the disease, a small sample population at a single centre and the heterogeneity of the surgical approach among multiple surgeons. Regardless, we did not note any significant difference between the groups in baseline demographic characteristics, which would indicate a sampling error.
Conclusion
Our results suggest that in patients with an acute type A dissection, there is no significant difference in early perioperative outcomes between a root replacement procedure and a supracoronary tube graft, regardless of the proximal extent of the intimal tear. However, the more aggressive root techniques resulted in decreased rates of greater than 2+ AI, aortic root dilation and improved survival trends on long-term follow-up. We suggest that these techniques may be even more beneficial in younger patients or in the presence of connective tissue disorders when the surgeon feels that root replacement is technically feasible.
Footnotes
Competing interests: M. Chu has received speakers’ honoraria from Medtronic Canada, Edwards Life Sciences, Livanova, Symetis and Abbott. B. Kiaii is a consultant, speaker and proctor for Medtronic, Johnson & Johnson and Symetis. He has received honoraria and travel assistance from those companies for speaking at meetings and providing proctorship. No other competing interests declared.
Contributors: All authors designed the study. M. Valdis, C. Adams and L. Guo acquired and analyzed the data, which M. Chu also analyzed. M. Valdis, C. Adams and M. Chu wrote the article, which all authors reviewed and approved for publication.
References
- 1.Hirst AE, Johns VJ, Kime SW. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore) 1958;37:217–79. doi: 10.1097/00005792-195809000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Collins JS, Evangelista A, Nienaber CA, et al. Differences in clinical presentation, management, and outcomes of acute type a aortic dissection in patients with and without previous cardiac surgery. Circulation. 2004;110(Suppl 1):II237–42. doi: 10.1161/01.CIR.0000138219.67028.2a. [DOI] [PubMed] [Google Scholar]
- 3.El-Hamamsy I, Ouzounian M, Demers P, et al. Canadian Thoracic Aortic Collaborative (CTAC). State-of-the-art surgical management of acute type A aortic dissection. Can J Cardiol. 2016;32:100–9. doi: 10.1016/j.cjca.2015.07.736. [DOI] [PubMed] [Google Scholar]
- 4.Krüger T, Conzelmann LO, Bonser RS, et al. Acute aortic dissection type A. Br J Surg. 2012;99:1331–44. doi: 10.1002/bjs.8840. [DOI] [PubMed] [Google Scholar]
- 5.Subramanian S, Leontyev S, Borger MA, et al. Valve-sparing root reconstruction does not compromise survival in acute type A aortic dissection. Ann Thorac Surg. 2012;94:1230–4. doi: 10.1016/j.athoracsur.2012.04.094. [DOI] [PubMed] [Google Scholar]
- 6.Urbanski PP, Lenos A, Irimie V, et al. Acute aortic dissection involving the root: operative and long-term outcome after curative proximal repair. Interact Cardiovasc Thorac Surg. 2016;22:620–6. doi: 10.1093/icvts/ivw002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halstead JC, Meier M, Etz C, et al. The fate of the distal aorta after repair of acute type A aortic dissection. J Thorac Cardiovasc Surg. 2007;133:127–35. doi: 10.1016/j.jtcvs.2006.07.043. [DOI] [PubMed] [Google Scholar]
- 8.Hagan P, Nienaber C, Isselbacher E, et al. The International Registry of Acute Aortic Dissection (IRAD). New insights into an old disease. JAMA. 2000;283:897–903. doi: 10.1001/jama.283.7.897. [DOI] [PubMed] [Google Scholar]
- 9.Tsai T, Nienaber CA, Isselbacher EM, et al. Acute type A aortic dissection: Does a primary tear in the aortic arch affect management and outcomes? Insights from the International Registry of Acute Aortic Dissection (IRAD) Circulation. 2006;114:432–8. doi: 10.1161/CIRCULATIONAHA.106.681510. [DOI] [PubMed] [Google Scholar]
- 10.Rylski B, Beyersdorf F, Blanke P, et al. Supracoronary ascending aortic replacement in patients with acute aortic dissection type A: What happens to the aortic root in the long run? J Thorac Cardiovasc Surg. 2013;146:285–90. doi: 10.1016/j.jtcvs.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Leontyev S, Trommer C, Subramanian S, et al. The outcome after aortic valve-sparing (David) operation in 179 patients: a single-centre experience. Eur J Cardiothorac Surg. 2012;42:261–6. doi: 10.1093/ejcts/ezs011. discussion 266–7. [DOI] [PubMed] [Google Scholar]
- 12.Gariboldi V, Grisolia D, Kerbaula F, et al. Long-term outcomes after repaired acute type A aortic dissections. Interact Cardiovasc Thorac Surg. 2007;6:47–51. doi: 10.1510/icvts.2006.136606. [DOI] [PubMed] [Google Scholar]